Back to Journals » Clinical Interventions in Aging » Volume 9
Prevalence of dementia in Al-Quseir city, Red Sea Governorate, Egypt
Authors El Tallawy H, Farghly W , Badry R, Rageh T, Shehata G, Hakeen M NA, El Hamed EH, Sayd M, Hamed Y, Kandil M
Received 15 May 2013
Accepted for publication 1 August 2013
Published 6 December 2013 Volume 2014:9 Pages 9—14
DOI https://doi.org/10.2147/CIA.S48325
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Hamdy N El Tallawy,1 Wafaa M Farghly,1 Reda Badry,1 Tarek A Rageh,1 Ghaydaa A Shehata,1 N Abdel Hakeem M,2 Mohamed Abd El Hamed,1 Mohamed AM Sayd,3 Yasser Hamed,2 Mahmoud R Kandil1
1Department of Neurology, 2Department of Neurology Faculty of Medicine, Assiut University, Assiut Egypt; 3Department of Neurology, Faculty of Medicine, Sohag University, Sohag, Egypt
Abstract: Dementia is one of the most important public health problems as a result of the rapid increase in the number of elderly persons worldwide. Improvement of prevention strategies and caring for people with dementia should be undertaken. We performed a door-to-door study to screen all subjects aged 50 years and older (n=4,329 of 33,285 inhabitants) in Al-Quseir city. The screening was performed by 3 neuropsychiatrists, using a modified form of the Mini-Mental State Examination. Suspected cases were subjected to case ascertainment according to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, diagnostic criteria for dementia; full clinical assessment; psychometric assessment using Cognitive Abilities Screening Instruments, Hachinski Ischaemic Score, Instrumental Activities of Daily Living Scale and the Geriatric Depression Scale; neuroimaging (computed tomography and/or magnetic resonance imaging); and laboratory investigations for selected patients when indicated. The prevalence of dementia was 2.01% for participants aged 50 years or older and 3.83% for those aged 60 years or older. It increased steeply with increasing age to a maximum of 13.5% for those aged 80 years or older. Alzheimer's dementia (48.3%) was the most common subtype, followed by vascular dementia (36.8%), dementia resulting from general medical conditions (11.5%), and last, dementia resulting from multiple etiologies (3.4%).
Keywords: Alzheimer's dementia, epidemiology, vascular dementia, Egypt
Corrigendum for this paper has been published
Introduction
Due to rapidly growing numbers of elderly people, dementia has become a major public health problem among the elderly in developed countries and is also a growing problem in the developing world, with major implications for morbidity and mortality, quality of life, and health care costs.1 Evidence suggests that elderly people with dementia in developing countries do not often use health care services, and when they do, the health care system is often not well prepared to provide good-quality services for dementia.2 More than 5% of the population aged 65 years and older suffer from dementia, and its prevalence steadily increases with aging. Alzheimer’s disease (AD) is the most frequent form of dementia, accounting for 50%–60% of all cases.3 In 2001, a Delphi consensus study estimated that there were 24.3 million people with dementia worldwide and predicted that this number would increase to 42.3 million in 2020 and 81.1 million by 2040.4 Despite the utmost importance of population-based epidemiologic information on dementia for clinicians, health care providers, and researchers, there are only a few reports that provide prevalence rates of dementia, and most of them are from Western countries.5 The aim of this study is the determination of the prevalence of all types of dementia among the population of Al-Quseir city, Red Sea Governorate, Egypt, aged 50 years and older.
Population and methods
We report a population-based door-to-door study among the population of Al-Quseir city, Red Sea Governorate. The study was conducted from July 1, 2009, to January 31, 2012. The sampling unit was all persons of either nuclear or extended families who were aged 50 years or older in a door-to-door survey. The Red Sea Governorate is the longest governorate in Egypt, and all its cities and villages lie directly on the Red Sea. The study area, Al Quseir city, is the second most populous city. It lies on the west side of the Red Sea Governorate.6 The total screened population in Al-Quseir city was 33,285 participants, with the exception of 533 individuals (1.6%) who refused to participate in the study. The main cause of refusal to be involved in the study was illiteracy and lack of knowledge, which is common in such communities. Participants were reached at their homes. If they were not there at the time of the first visit, they were revisited at another time (the capture–recapture method). Of the total population, 4,329 participants were aged 50 years and older, and those were the subjects of the present study.
Inclusion criteria include all persons at or above the age of 50 years of both sexes. Exclusion criteria include the presence of psychiatric illness (schizophrenia and mood disorder) and severe sensory impairment (blindness, deafness). Informed written consent was obtained from each patient, caregiver, or responsible family member according to the ethics committee of the Faculty of Medicine, Assiut University, and consent was obtained from the Egyptian Ministry of Health for the whole project.
Methods
This study was conducted in 3 phases.
Phase 1: screening phase
Screening of all inhabitants (aged 50 years and more) was performed by three neuropsychiatrists, using standardized Arabic screening, including inquiry about any acquired cognitive, behavioral, or personality changes7 and the modified Mini-Mental State Examination (MMSE),8 to pick up suspected cases of dementia. The 2 points for testing reading and writing in MMSE were excluded if the subject was illiterate, and the full score was calculated as 28 instead of 30 points; hence, the cutoff for regarding a subject as someone with suspected dementia was 21 instead of 23 points.5
Phase 2: diagnostic phase
In phase 2, all participants who were suspected to be demented (MMSE ≤23 or <21 for illiterate subjects) were invited to attend at Al-Quseir General Hospital for case ascertainment and typing of dementia. A full clinical history was taken, and a meticulous examination was performed for each patient in a specialized sheet prepared specifically for this study. A psychometric assessment was also made, using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition,Text Revision, criteria to confirm the diagnosis and differentiate different types of dementia; Cognitive Abilities Screening Instruments (which is more comprehensive than most screening tests of cognitive abilities), which has a cutoff point of 67 or fewer points for dementia;9 the Instrumental Activities of Daily Living Scale, which provides a measure of social and occupational functioning that is used as a threshold for accepting a cognitively impaired subject as being demented;10 the Geriatric Depression Scale for diagnosis of comorbid depression;11 and the Hachinski Ischaemic Score to differentiate vascular dementia from other types of dementia (a score of 7 or higher indicates vascular dementia, a score of 5 or 6 indicates mixed dementia, and a score lower than 5 indicates AD).12 Staging of dementia was done according to the results of MMSE. We calculate a score of 17–21 for mild, 9–16 for moderate, and less than 9 for a severe degree of dementia. These values correspond to the values of 19–23, 11–18, and less than 11 for mild, moderate, and severe dementia on the full score of 30 points.5
Phase 3: investigatory phase
Specific investigations were carried out for patients in Al-Quseir General Hospital, such as electrocardiogram, complete blood picture, blood sugar curve, renal functions, liver functions, serum uric acid, lipid profile, thyroid functions, and serum level of heavy metals. A computed tomography scan and/or a magnetic resonance imaging scan of the brain was carried out for all patients in Safaga Hospital, North Safaga, Egypt.
Statistical analysis was done using an analysis of variance test for comparison between mild, moderate, and severe dementia, as well as different types of dementia. The chi square test was used to illustrate the relations or comparisons in nominal data. A P-value less than 0.05 was considered significant.
Results
The overall population involved in this study was 4,329 participants, of whom 2,426 (56%) were men and 1,903 (44%) were women. The age distribution of the studied sample shows that 51.3% were aged from 50 to less than 60 years, 32.6% were aged from 60 to less than 70 years, 12.4% were aged 70 to less than 80 years, and 3.7% were aged 80 years and older. The ratio of men to women in the total sample was 1.3:1. Educated participants made up 56% (n=2,418) of the population, and illiterate participants made up 44% (n=1,911). The steps that were carried out for detection of the prevalence of dementia and classification of its subtypes are demonstrated in Figure 1.
  | Figure 1 Flow chart for screening and diagnosis of dementia. |
Prevalence of dementia among this study and worldwide studies are reported in Table 1. Age- and sex-specific prevalence for dementia at different age groups is illustrated in Table 2. The prevalence of dementia was significantly higher among illiterate than educated participants, as shown in Table 3. Classification of dementia as a result of general medical condition is reported in Table 4. The degree of dementia and its subtypes is mentioned in Table 5.
  | Table 1 Worldwide prevalence of dementia in different studies |
  | Table 2 Age- and sex-specific prevalence ratios of dementia of all types |
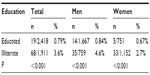  | Table 3 Prevalence ratio of dementia in relation to education |
  | Table 4 Classification of dementia resulting from general medical conditions according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision |
  | Table 5 Degree of dementia and its subtypes |
Discussion
The estimated prevalence rate of all types of dementia recorded in this study was 2.01% for those aged 50 years and more, 3.83% for those aged 60 years and more, 8.12% for those aged 70 years and more, and 13.5% for those aged 80 years and more. The prevalence rate of dementia doubles every decade. The results of this study are slightly lower than those recorded by El Tallawy et al in 20107 in Al Kharga District, Egypt, who reported that the prevalence rate of all types of dementia was 2.26% for patients aged 50 years and more and 4.45% for patients aged 60 years and more in a sample of 8,173 subjects, and Farrag et al in 19985 in Assiut, Egypt, who reported a prevalence rate of all types of dementia of 4.5% for patients aged 60 years and more in a sample of 2,000 subjects. The lower prevalence in this study could be attributed to carrying out this study on an urban population (Al Quseir city), whereas both previous studies were carried out on both urban and rural populations.
Farrag et al5 reported that the prevalence of dementia of all types is slightly more frequent in rural than urban populations but that this difference was insignificant. In a Swedish study, Rorsman et al13 found that the prevalence rate of dementia was higher in rural communities than in urban communities. The prevalence rates of dementia in different studies vary from very low (0.62%) in Kolkata, India, for those aged 50 years and more14 to very high in Israel (19.2%) in those aged 65 years and more.15 This geographical difference might come from several factors, such as a different culture and environment, including rather simple activities of daily living, low-technology environment, and underreported functional impairment by family members.16 In addition, a short life span and high mortality rates in developing countries might also influence the low prevalence of dementia. Third, a true racial difference might exist. For example, the APOE 4 allele, which is known as a genetic risk factor for AD in Caucasians and Asians, is not associated with a higher risk of dementia in Africans.17 However, this may be attributed to methodological factors such as differences in the sample sizes, age distribution of the population, case ascertainment, screening methods, and interpretation of diagnostic criteria, which greatly differed from one study to another.5
With regard to different types of dementia, AD was the most frequent type of dementia, followed by vascular dementia, dementia resulting from general medical condition, and last, dementia resulting from multiple etiologies (48%, 36%, 12%, and 3%, respectively). These results are in agreement with El Tallawy et al7 in Al Kharga District, Egypt, who reported that AD was the most frequent type of dementia, followed by vascular dementia (51% and 29% respectively), and by Farrag et al5 in Nile Valley, Assiut, who reported that the prevalence of AD was 53% and that of vascular dementia was 22.9%. Fratiglioni et al18 reported that the ratio between AD and vascular dementia was similar in most studies of the United States, Europe, and Africa. AD is the most common etiology of dementia and accounts for 50%–70% of total dementia cases, followed by vascular dementia, which accounted for 20%–30% of total dementia. The increase in the rate of vascular dementia in this study may be related to the increase in the prevalence of cerebrovascular stroke (CVS), over time, worldwide, and especially in developing countries.19 Unlike other studies, we did not report any cases of substance-induced dementia or alcoholic dementia because of the sociocultural attitude against alcohol consumption in our community. There also was no significant sex difference between men and women in the prevalence rate of AD, but there was significant difference between both sexes in vascular dementia in this study. These results are not in agreement with Gao et al20 in the United States and Ruitenberg et al21 in Rotterdam, who reported that AD is more common in women than men. The Latin America studies showed that slightly higher rates of dementia for women compared with men in all age groups.22 A similar finding was reported in the European pooled data analysis,23 as well as in a published study conducted in Latin America, India, and the People’s Republic of China.24 In the present study, the prevalence of dementia was significantly higher in illiterate subjects than in educated subjects. These results are in agreement with Herrera et al,25 who reported that illiteracy was associated with a significantly higher prevalence of dementia.
Dong et al26 in the People’s Republic of China found that the more years of education there were, the lower the prevalence rate of AD was, and Kalaria et al27 reported that illiteracy remains a risk factor for dementia in developing countries. The European Studies of Dementia (EURODEM) analysis revealed that a low level of education increased the risk of AD in women, but not in men.28 Education might be an indirect risk factor in which a lower number of educated people, acting as manual workers, are more frequently exposed to toxins or nutritional deficiency. Education also is related to intelligence. Some studies reported that higher premorbid intelligence is associated with a low risk of developing dementia.29,30 The rates of mild, moderate, and severe dementia were 33.3%, 48.3%, and 18.4%, respectively. These results are in agreement with Farrag et al,5 who reported that the degrees of dementia in his study were as follows: 36.7% of patients had a mild degree, 45.6% had a moderate degree, and 17.8% had a severe degree of dementia. Mild and moderate cases of dementia in this study represent the largest proportion of dementias, involving about 80% of the patients. These patients are the best candidates for treatment and are only recognizable through door-to-door, population-based studies.
Conclusion
The prevalence of all types of dementia was 2.01% for those aged 50 years and older and 3.83% for those aged 60 years and older. AD was the most common subtype, followed by vascular dementia. Age was the most important risk factor. Education affected the prevalence of dementia. Mild to moderate cases of dementia, who are the best candidates for treatment, represent the largest proportion of dementias.
Disclosure
The authors report no conflicts of interest in this work.
References
Perea-Bartolome MV, García-García R, Ladera-Fernández V, et al. Detection of mild cognitive impairment in people older than 65 years of age and its relationship to cardiovascular risk factors (DECRIVAM). BMC Public Health. 2011;11:504. doi: 10.1186/1471-2458-11-504. | |
Dias A, Patel V. Closing the treatment gap for dementia in India. Indian J Psychiatry. 2009;51 Suppl 1:S93–S97. | |
Blennow K, de Leon MJ, Zetterberg H. et al; Alzheimer’s Disease International. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–2117. | |
Ferri CP, Prince M, Brayne C, et al; Alzheimer’s Disease International. Global prevalence of dementia: a Delphi consensus study. Lancet; 2005;366:2112–2117. | |
Farrag A, Farwiz HM, Khedr EH, Mahfouz RM, Omran SM. Prevalence of Alzheimer’s disease and other dementing disorders: Assiut-Upper Egypt study. Dement Geriatr Cogn Disord. 1998;9(6):323–328. | |
Gaber SM, Aly SM, Masood KA. Center of information and decision on making, Red Sea Governorate achievement index (In Arabic). 2010. | |
El Tallawy HN, Farghaly WM, Rageh TA, et al. Epidemiology of major neurological disorders project in Al Kharga district, New Valley, Egypt. Neuroepidemiology. 2010;35(4):291–297. | |
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. | |
Ross GW, Petrovitch H, White LR, et al. Characterization of risk factors for vascular dementia: the Honolulu-Asia Aging Study. Neurology. 1999;53(2):337–343. | |
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. | |
Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982–1983;17(1):37–49. | |
Hachinski VC, Iliff LD, Zilhka E, et al. Cerebral blood flow in dementia. Arch Neurol. 1975;32(9):632–637. | |
Rorsman B, Hagnell O, Lanke J. Prevalence and incidence of senile and multi-infarct dementia in the Lundby Study: a comparison between the time periods 1947–1957 and 1957–1972. Neuropsychobiology. 1986;15(3–4):122–129. | |
Banerjee TK, Mukherjee CS, Dutt A, Shekhar A, Hazra A. Cognitive dysfunction in an urban Indian population – some observations. Neuroepidemiology. 2008;31(2):109–114. | |
Wertman E, Brodsky J, King Y, Bentur N, Chekhmir S. An estimate of the prevalence of dementia among community-dwelling elderly in Israel. Dement Geriatr Cogn Disord. 2007;24(4):294–299. | |
Chandra V, Pandav R, Dodge HH, et al. Incidence of Alzheimer’s disease in a rural community in India: the Indo-US study. Neurology. 2001;57(6):985–989. | |
Kalaria RN, Ogeng’o JA, Patel NB, et al. Evaluation of risk factors for Alzheimer’s disease in elderly east Africans. Brain Res Bull. 1997;44(5):573–577. | |
Fratiglioni L, De Ronchi D, Agüero-Torres H. Worldwide prevalence and incidence of dementia. Drugs Aging. 1999;15(5):365–375. | |
Truelsen T, Heuschmann PU, Bonita R, et al. Standard method for developing stroke registers in low-income and middle-income countries: experiences from a feasibility study of a stepwise approach to stroke surveillance (STEPS Stroke). Lancet Neurol. 2007;6(2):134–139. | |
Gao S, Hendrie HC, Hall KS, Hui S. The relationships between age, sex, and the incidence of dementia and Alzheimer disease: a meta-analysis. Arch Gen Psychiatry. 1998;55(9):809–815. | |
Ruitenberg A, Ott A, van Swieten JC, Hofman A, Breteler MM. Incidence of dementia: does gender make a difference? Neurobiol Aging. 2001;22(4):575–580. | |
Nitrini R, Bottino CM, Albala C, et al. Prevalence of dementia in Latin America: a collaborative study of population-based cohorts. Int Psychogeriatr. 2009;21(4):622–630. | |
Lobo A, Launer LJ, Fratiglioni L, et al. Prevalence of dementia and major subtypes in Europe: A collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology. 2000;54(11 Suppl 5):S4–S9. | |
Llibre Rodriguez JJ, Ferri CP, Acosta D, et al; 10/66 Dementia Research Group. Prevalence of dementia in Latin America, India, and China: a population-based cross-sectional survey. Lancet. 2008;372(9637):464–474. | |
Herrera E Jr, Caramelli P, Silveira AS, Nitrini R. Epidemiologic survey of dementia in a community-dwelling Brazilian population. Alzheimer Dis Assoc Disord. 2002;16(2):103–108. | |
Dong MJ, Peng B, Lin XT, Zhao J, Zhou YR, Wang RH. The prevalence of dementia in the People’s Republic of China: a systematic analysis of 1980–2004 studies. Age Ageing. 2007;36(6):619–624. | |
Kalaria RN, Maestre GE, Arizaga R, et al; World Federation of Neurology Dementia Research Group. Alzheimer’s disease and vascular dementia in developing countries: prevalence, management, and risk factors. Lancet Neurol. 2008;7(9):812–826. | |
Letenneur L, Launer LJ, Andersen K, et al. Education and the risk for Alzheimer’s disease: sex makes a difference. EURODEM pooled analyses. EURODEM Incidence Research Group. Am J Epidemiol. 2000;151(11):1064–1071. | |
Schmand B, Smit JH, Geerlings MI, Lindeboom J. The effects of intelligence and education on the development of dementia. A test of the brain reserve hypothesis. Psychol Med. 1997;27(6):1337–1344. | |
Alexander GE, Furey ML, Grady CL, et al. Association of premorbid intellectual function with cerebral metabolism in Alzheimer’s disease: implications for the cognitive reserve hypothesis. Am J Psychiatry. 1997;154(2):165–172. | |
Mura T, Dartigues JF, Berr C. How many dementia cases in France and Europe? Alternative projections and scenarios 2010–2050. Eur J Neurol. 2010;17(2):252–259. | |
Bottino CM, Azevedo D Jr, Tatsch M, et al. Estimate of dementia prevalence in a community sample from São Paulo, Brazil. Dement Geriatr Cogn Disord. 2008;26(4):291–299. | |
Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1–2):125–132. | |
Custodio N, et al. Prevalencia de demencia en una comunidad urbana de Lima: Un estudio puerta a puerta. [Prevalence of dementia in an urban community of Lima: A door to door survey.] XII Pan American Congress of Neurology, Santo Domingo, Dominican Republic, 15. 2007. | |
Shaji S, Bose S, Verghese A. Prevalence of dementia in an urban population in Kerala, India. Br J Psychiatry. 2005;186:136–140. | |
Berr C, Wancata J, Ritchie K. Prevalence of dementia in the elderly in Europe. Eur Neuropsychopharmacol. 2005;15(4):463–471. | |
Rahkonen T, Eloniemi-Sulkava U, Rissanen S, Vatanen A, Viramo P, Sulkava R. Dementia with Lewy bodies according to the consensus criteria in a general population aged 75 years or older. J Neurol Neurosurg Psychiatry. 2003;74(6):720–724. | |
El-Tallawy H, Farghaly W, Metwally N, et al. Prevalence of neurological disorders in Al Quseir, Egypt: methodological aspects. Neuropsychiatr Dis Treat. 2013; 9:1295–1300. Available from: http://www.msdiscovery.org/papers/biblio/7623-prevalence-neurological-disorders-al-quseir-egypt-methodological-aspects. Accessed November 20, 2013. |
 © 2013 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2013 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
