Back to Journals » Journal of Pain Research » Volume 10
Prevalence of chronic pain with neuropathic characteristics: a randomized telephone survey among medical center patients in Kuwait
Authors Zghoul N , Ross EL, Edwards RR, Ahmed A, Jamison RN
Received 5 October 2016
Accepted for publication 14 November 2016
Published 4 April 2017 Volume 2017:10 Pages 679—687
DOI https://doi.org/10.2147/JPR.S123966
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Nadia Zghoul,1 Edgar L Ross,2 Robert R Edwards,2 Adel Ahmed,1,3 Robert N Jamison2
1Clinical Research Department, Dasman Diabetes Institute, Kuwait City, Kuwait; 2Department of Anesthesiology, Pain Management Center, Brigham and Women’s Hospital, Harvard Medical School, Chestnut Hill, MA, USA; 3Faculty of Medicine, Kuwait University, Safat, Kuwait
Background: Chronic pain with neuropathic characteristics is considered to be an international health problem. However, surveys on the actual incidence of neuropathic pain have not been conducted in many Middle East countries, including Kuwait. The aim of this study was to examine the incidence of pain and medical comorbidities among a random sample of patients treated at a large medical center in Kuwait.
Methods: A list of 1,000 patients was created from the hospital medical record system, and a telephone survey was conducted on 759 patients who responded to the phone call, of which 67.2% (N=510) participated. Those who stated that they had pain every day for the past 3 months were invited to answer additional questions about their pain.
Results: Fifty-six percentage of those surveyed (N=283) reported experiencing chronic pain. Total average age was 49.2 years (SD=14.5), 45.5% were female, and 70.5% were Kuwaiti nationals. Most (74.3%) reported having diabetes and one-third (32.2%) showed evidence of neuropathic pain characteristics (mean DN4=2.8, SD=1.7). Other comorbid medical conditions were prevalent (48.4% hypertension, 30.4% arthritis, 22.6% heart disease, and 20.4% asthma) with an average of 2.3 (SD=1.3) medical problems per person. Those with pain tended to be older, female, unemployed, and overweight (p<0.01). The pain was mostly located in the lower extremities and those with neuropathic pain tended to report a higher intensity of pain and a higher frequency of seeking treatment for their pain in a clinic or hospital (p<0.05). Most relied on over-the-counter medications for their pain (38.1%). Very few were taking prescription medication for their pain.
Conclusion: This survey suggests that chronic pain is more prevalent in a medical population in Kuwait than previously anticipated. Health care services and behavioral interventions to improve lifestyle changes in Kuwait and other Arab countries are needed to positively impact pain and reduce other comorbidities.
Keywords: chronic pain, medical comorbidities, gender differences, Kuwait, weight, diabetes mellitus, health behavior
Introduction
Many studies have documented that chronic pain is an international widespread problem.1–3 Pain is the primary motivating factor that encourages individuals to seek medical attention, and chronic pain is known to significantly interfere with sleep, employment, mood, energy level, and overall quality of life.4 There has been a gradual increase in the number of older people as a percentage of the global population, and with age comes many chronic health conditions that have chronic pain as a component of their disorder. These include arthritis, diabetes, and heart disease as well as the residual effect of treatment for other conditions (e.g., cancer and back pain).3
The incidence of chronic pain has not been determined in many regions of the world. Although the World Health Organization (WHO) has estimated that the incidence of chronic pain is significant in most countries, they also note that it is variable across countries with an up to 6-fold estimated variation.5 There have been few published surveys of the incidence of chronic pain among the Arabian Peninsula states in the Middle East, which consist of Saudi Arabia, Qatar, Bahrain, United Arab Emirates, Oman, and Kuwait. Some studies suggest that chronic pain associated with medical comorbidities in the Middle East may be as high as 25% and may be associated with gender and behavioral differences, but this has not been confirmed.6 Over the past decade, there has been a reported increase in back pain in the Middle East,7 and in clinic-based studies of small samples in Kuwait, persistent pain was found to be reported among adolescents,8 pregnant women,9 patients treated for cancer,10 health care providers,11 and children with inflammatory bowel disease.12 Recently, an extensive survey among attendees evaluated at a rehabilitation center in Kuwait found female Kuwaitis to have a higher incidence of pain and medical comorbidities than males and non-Kuwaitis, highlighting the role of gender and cultural factors in contributing to pain and comorbid medical conditions.13
Neuropathic pain, as defined by the International Association for the Study of Pain, is pain initiated or caused by a primary lesion or dysfunction in the nervous system.14 Neuropathic pain afflicts millions of people worldwide and has been estimated to occur in as much as 7% of the general population.15 Many common diseases, injuries, and interventions that produce lesions in the somatosensory pathways in the periphery or central nervous system can cause neuropathic pain.16 While numerous studies have reported on the incidence of diabetic neuropathy (which is a microvascular condition resulting in numbness in the extremities and can affect as many as 50% of those with diabetes),17 there has been less emphasis on reporting the incidence of painful diabetic neuropathy. This is an important area of work, as many studies have indicated that neuropathic pain is associated with reduced quality of life and physical functioning.18,19 Such findings were obtained even within groups of chronic pain patients; frequently, patients who describe their pain as having neuropathic features report a greater intensity and impact of their pain, worse emotional functioning, and greater disability than patients with nonneuropathic pain.20,21 Some relatively small studies in diabetic patients have suggested that diabetes-related pain with neuropathic features has a disproportionately negative impact in such diverse regions of the world as Croatia,22 France,23 South Africa,24 Israel,25 and portions of Asia and Latin America.26 To date, however, there has been minimal research on neuropathic diabetic pain in Kuwait.
In the State of Kuwait, all nationals enjoy health care benefits, yet, despite access to these benefits, there remains an elevated incidence of medical problems, including diabetes, that can contribute to increased pain.27 Diabetic patients often underreport symptoms associated with their condition, including pain, particularly among patients with type II diabetes, leading them to being inadequately treated.28 There has been a call for greater attention to understanding the effect weight and behavioral lifestyle have on general health and medical comorbidities in Kuwait and other Middle East countries.6
This study was designed to assess the incidence of neuropathic pain and medical comorbidities among a random sample of patients treated at a large medical center in Kuwait. We intended to examine differences based on age, gender, weight, and presence and type of medical comorbidities. Based on the literature, it was anticipated that between 25% and 35% of respondents would report having chronic pain and 30% of these would have neuropathic characteristics. An additional goal of this survey study was to identify those subgroups of individuals who would be at greatest risk for chronic pain and medical comorbidities and to help determine how these medical issues might further influence lifestyle and behavioral change and affect treatment strategies.
Methods
This study was approved by the Dasman Institute Ethics Committee. A research assistant was hired and trained to conduct phone surveys on a random list of patients who had been seen at the Dasman Institute in Kuwait City. The investigators met to review a list of possible survey items, and forward and backward translation was conducted. During the pilot phase of the study, 15 subjects were surveyed in order to train the interviewer and to identify any perceived difficulties by the participants in responding to the questionnaire items. The interviews could be conducted in Arabic or English, whichever was preferred. The preliminary surveys were recorded with permission and evaluated by independent medical specialists who were fluent in both English and Arabic. Suggestions for change in language and follow-up questions were added and revised based on consensus of the study group.
We obtained a list of patients through the hospital electronic medical record system who were aged 21 years or older, living in Kuwait, and having either a home phone or cell phone. A list of random names and phone numbers was generated from >6,000 telephone numbers of registered patients who received medical care at the institute. No recorded information was available about the incidence of pain among these patients. Phone calls were made during morning, afternoon, and early evening hours on weekdays from 9 a.m. to 7 p.m. If no contact was made with the first call, that same number was called three more times at different times of the day. All surveys were conducted by the same interviewer. Password-protected phone interview data were entered into a deidentified database utilizing a web-based electronic data capture program (REDCap) to record the interview data of the participants. All calls were recorded with permission of the subjects using a CISCO phone call recording program (CallREC) and software by Zoom International (http://www.zoomint.com).
Most interviews were conducted in Arabic, and the data were entered in English directly onto a spreadsheet by the research assistant who was fluent in both English and Arabic. Body mass index (BMI; height/weight) was obtained for each of the participants through the electronic medical record system after obtaining verbal consent and ethics committee approval.
Survey questions
All respondents were told that their participation was voluntary and that their responses were confidential. Verbal consent was obtained at the beginning of the interview and participants were informed that the interview would be brief and not require >10 minutes. After consenting, all respondents were asked if they currently suffered from pain every day that had lasted for >3 months. If they answered “no” then they were asked to provide demographic information of age, gender, nationality, how long they had lived in Kuwait, employment status, and smoking behavior.
Those who responded “yes” to having pain every day lasting >3 months were asked additional questions about their pain. Pain description items were adapted from the Brief Pain Inventory.29,30 The questions included pain site, pain intensity, pain interference, pain medication, other types of pain treatments, medical comorbidities, and frequency of clinic and hospital visits over the past month.
In order to identify neuropathic characteristics of the pain, the participants were asked 10 questions from the Arabic version of the DN4.31 The DN4 was originally developed and used to identify and classify neuropathic pain.32 For the first seven symptom items, the respondents answered yes or no to whether their pain could be described as burning, painful cold, electric shocks, tingling, pins and needles, numbness, and itching. The subject was also asked if their pain area was sensitive to touch, sensitive to pin prick, and sensitive to light brushing, similar to a clinical examination. A score of 1 was given for each “yes” answer and 0 for each “no” answer. A score of 4 or higher has a >90% specificity for a neuropathic pain diagnosis. A score of <4 suggests that the pain is unlikely to be neuropathic. The DN4-interview questionnaire has been shown to have 83% sensitivity and 90% specificity when compared to clinical diagnosis.31 In persons with diabetes, the DN4 showed a high diagnostic accuracy for neuropathic pain. At the cutoff of 4, DN4 displayed a sensitivity of 80%, specificity of 92%, positive predictive value of 82%, negative predictive value of 91%, and a likelihood ratio for a positive result of 9.6.33 It has been translated into many languages, including Arabic.34
Statistical analyses
Data were analyzed using SPSS (v. 21; IBM Inc., Armonk, NY, USA) employing both parametric and nonparametric analyses. Categorical variables were analyzed using Kappa for determining agreement between dichotomous variables (such as yes/no) with 95% confidence intervals. Continuous variables were evaluated using intraclass correlation coefficients and Student’s t-test. Specific comparisons were made between groups based on gender and whether the subjects had evidence of neuropathic pain or not using regression models (Logistic and Poisson) and stepwise discriminant function analyses using Wilks’s lambda with canonical correlations and classification results based on predicted group membership. We also conducted one-way analysis of variance (ANOVA) with Bonferroni analysis to control for multiple comparisons on interview items based on weight (BMI) classification.
Results
We obtained a randomly generated list of 1,000 patients who had been evaluated and treated at the Dasman Institute and conducted a phone survey between November, 2014, and September, 2015. Although patients were often referred to the Institute for evaluation and treatment of diabetes, patients with medical comorbidities other than diabetes, including stroke, asthma, cardiac and respiratory problems, and multiple sclerosis, had also been treated at this center.
Of the 1,000 names who were identified and called, 759 (75.9%) responded to the call, while 241 (24.1%) did not answer despite frequent attempts. Of those who answered the call, 512 (67.5%) agreed to participate in the interview and, of these, 283 (55.3%) reported having chronic pain every day that had reportedly lasted longer than 3 months. Two of the subjects who agreed to participate and who stated that they were without pain were not included in the analyses due to missing demographic data. Of the participants who were included in the analyses (N=510), the majority were male (54.6%) and ranged in age between 21 and 98 years (average age 49.3, SD=14.3; Table 1). Almost 74% were of Kuwaiti nationality. The other subjects came mostly from Middle East countries and reported that they were Egyptian (6.5%), Iranian (3.1%), Syrian (2.4%), Jordanian (2.4%), or represented another country as their original nationality (9.2%). Less than 3% did not indicate their nationality. Most of the non-Kuwaitis reported either living in Kuwait since birth or for most of their lives. Over half of the subjects (54.3%) were employed. BMI (weight/height) data were obtained through the hospital medical record system and of those with BMI data (N=400), 12.3% were classified as healthy normal (N=49; BMI <25.0 kg/m2), 29.0% were classified as overweight (N=116; BMI ≥25.0 and <30.0 kg/m2), 49.8% were classified as obese (N=199; BMI ≥30.0 and <40.0 kg/m2), and 9.0% were classified as morbidly obese (N=36; BMI ≥40.0 kg/m2) according to obesity classification guidelines.35 Significant differences were found between those who reported having pain and those without pain on age, gender, employment status, and BMI classification; those with pain were older, more often female, unemployed, and overweight (p<0.001).
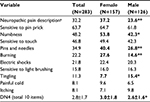
Table 2 presents the incidence of neuropathic pain descriptors and the comparison of these descriptors between men and women. Overall, except for “tingling”, women tended to endorse more neuropathic pain descriptors than men, and women had a higher average “yes” response among these descriptors compared with men (p<0.05).
Table 3 presents data among those who reported having a chronic pain problem that has lasted >3 months (N=283). Overall, their pain intensity ratings averaged 6.8 on a 0–10 numeric rating scale, and most reported lower extremity, lower back, or multiple joint pain as their primary pain problem. Most of them reported some interference with overall activity due to their pain (average 4.7, SD=2.5, on a 0–10 scale) and also that their pain mostly interfered with routine daily activities, sleep, ability to work, and contributed negatively to their mood. Ninety-one percentage reported taking pain medication, although most of these were over-the-counter aspirin or acetaminophen. Twenty percentage were prescribed anticonvulsants. Very few reported taking prescription opioids, muscle relaxants, benzodiazepines, antidepressants, or antipsychotics (range 7.0% and 0.4%). Seventeen percentage reported smoking cigarettes. Seventy-four percent stated that they had diabetes, of which only 19% were insulin dependent. The vast majority of the responders (87.2%) reported having a chronic medical condition of either diabetes, heart disease, high blood pressure, asthma, cancer, or arthritis and more than half (56.9%) of the participants reported having more than one chronic medical condition (mean=2.0, SD=1.3). Despite the high frequency of pain and medical problems, <40% reported seeing their doctor or going to a clinic in the past month.
Comparisons were made between those who showed a positive response on the DN4 (4 out of 10 items) and those who did not endorse items commonly associated with neuropathic pain. Those who were positive on the DN4 tended to significantly more often be women (p<0.01), report pain in their extremities (p<0.01), have higher rates of pain with more activity interference (p<0.01), and tended to have significantly more medical comorbidities (p<0.001), including heart disease and hypertension (p<0.05), compared to those lower on the DN4 scale. No differences were found between groups on age, nationality, or employment status. Stepwise discriminant function analyses were performed on the significant survey variables relating to neuropathic pain. Three items were shown to best predict differences between groups. These included total pain interference (Wilks’s lambda =0.94), presence of diabetes (Wilks’s lambda =0.90), and being female (Wilks’s lambda =0.89; p<0.001). The canonical correlation was 0.34 and these three items alone correctly classified 71.1% of the cases.
Differences were also examined between those who reported having chronic pain and diabetes (N=207) and those with chronic pain without diabetes (N=72). Those with pain and diabetes were older (54.2 vs 43.1 years; p<0.001), more often female (55.8% vs 44.2%; p<0.05), more often Kuwaiti (78.6% vs 21.4%; p<0.05), unemployed (60.2% vs 39.8%; p<0.05), had more medical problems (2.5 vs 0.6 problems; p<0.001), were more often overweight (BMI =33.1 vs 30.7 kg/m2; p<0.05), and had a higher percentage of pain with neuropathic characteristics (83.9% vs 16.1%; p<0.01) compared with those with chronic pain and who were not diabetic. Using stepwise discriminant function analyses, the total number of self-reported medical problems was best in differentiating diabetics from nondiabetics (Wilks’s lambda =0.68). This number was able to correctly classify 86.7% of the cases.
Results also revealed gender differences among this sample population. In general, compared with men, women were more often unemployed (p<0.05), had higher pain ratings (p>0.001), reported more activity interference (p<0.05) and more mood disorder (p>0.001), took more pain-related medication (p<0.05), and had a higher incidence of neuropathic pain (p<0.01). Women also reported significantly more arthritis and cancer (p<0.05) compared with men even though men tended to report smoking cigarettes much more often than women (p<0.001) and more often reported having diabetes (p<0.05) and heart disease (p<0.001) compared with women. Stepwise discriminant function analyses were performed on the significant survey variables relating to gender. Five items were shown to best predict differences between men and women. These included smoking (Wilks’s lambda =0.87), pain intensity average (0.79), heart disease (0.76), diabetes (0.74), and being unemployed (0.73). The combined canonical correlation was 0.52 and these five items were able to correctly classify 76.1% of the cases. Combined analyses of the survey variables revealed that women with neuropathic pain related to diabetes more often reported higher pain ratings and more activity interference than those without these descriptive qualities (p<0.001).
ANOVAs were conducted between the four classes of BMI groups (healthy normal, overweight, obese, and morbidly obese) on the interview items using Bonferroni analyses to control for multiple comparisons. Overall, BMI index was positively related to age (F=5.5, p<0.01) and having diabetes (F=5.2, p<0.01). Those who were overweight also tended to have more medical problems (F=6.6, p<0.001), including hypertension (F=3.6, p<0.01) and arthritis (F=3.3, p<0.01), spent more days in the hospital (F=4.5, p<0.05), and reported more depression, anxiety, and irritability associated with their pain (F=2.8, p<0.05).
Discussion
The results of this randomized telephone survey showed that over half of the individuals treated at a medical institute in Kuwait reported having chronic pain and one-third of these endorsed symptoms are suggestive of neuropathic pain. These results shed light on the need for further investigation on the incidence of persistent neuropathic pain within the wider Middle East population. Women in particular were found to have a higher incidence of neuropathic pain symptoms and reported significantly higher ratings of pain intensity, had a greater number of pain sites, and took more medication compared with men. Also, those who were classified as being overweight, which was associated with a higher incidence of pain, reported more medical problems, received more medical treatments, and had more of a mood disorder than those who were within a healthy weight range.
There are a number of points that can be drawn from a limited survey study of this nature. First, the long-known link between obesity and chronic pain is evident, and obesity is a major risk factor for diabetes, osteoarthritis, and heart disease among this population.36 Thus, strategies to target obesity would likely have a positive effect on pain and comorbid medical conditions. Second, even though all residents of Kuwait have access to low cost, state-supported health care, there remains a high incidence of medical problems and chronic pain. Further understanding of the influence of regional and cultural factors may help to clarify those contributing variables that increase the incidence of chronic pain and related comorbid medical conditions associated with pain.37 The results of this and other studies should encourage further research into investigating behaviors associated with obesity and resulting chronic pain. Although there has been a recent emphasis on eating behavior and obesity-related research in Kuwait, it still lags behind most other countries.38 For many, there has also been an emphasis on more medical solutions to problems, such as bariatric surgery for obesity, rather than strict adherence to diet and exercise. Third, although not significant, those who had evidence of neuropathic pain also reported a higher incidence of arthritis. This unexpected result should be explored further in future studies.
The results of this study offer an interesting contrast to the US and other western societies where there is a tendency to overrely on prescription medication to manage pain. The findings of this study and others10,13,37,39 suggest that very few individuals in Kuwait take prescription medication to manage their pain, including muscle relaxants, anticonvulsants, tranquilizers, antidepressants, and opioids. Evidence-based recommendations from systematic literature reviews and existing guidelines have strongly supported the use of tricyclic antidepressants, serotonin–noradrenaline inhibitors, pregabalin, and gabapentin for treating pain with neuropathic characteristics.40 Weaker support was found for lidocaine patches, capsaicin patches, and tramadol, and less support was found for strong opioids and botulinum injections.41,42 Interestingly, based on the results of this survey, the recommended types of medications for neuropathic pain are not frequently taken by many with pain in Kuwait.40 This is consistent with some epidemiologic evidence that neuropathic pain is likely undertreated, despite evidence for some effective interventions.43
Behavioral interventions for neuropathic pain are also likely both underutilized and understudied; a recent Cochrane review of nonpharmacological treatments for neuropathic pain found only a few randomized controlled trials of empirically supported treatments such as cognitive behavioral therapy for adults with chronic neuropathic pain conditions.44 It is also known that there has been a rapid increase in use of polypharmacy in many Western countries to treat chronic pain resulting in increased misuse and overdose of certain prescription medications, specifically benzodiazepines and opioids.45 This has contributed to what has been described as “an epidemic” of misuse in the US and elsewhere.46 In contrast, few individuals in Kuwait are prescribed opioids unless they are treated for terminal cancer and medications are used sparingly. Although problems associated with overuse of prescription medications may be avoided, it would seem that some individuals in Arab countries might benefit from increased use of certain medications (eg, anticonvulsants) that are not regularly being made available. Future comparative studies could help to identify outcome differences based on prescription medication and other treatments for neuropathic pain.
There are a number of limitations in this study that should be highlighted. First, although we were pleased at the high number of responders who participated in the telephone survey, a number of potential subjects were not contacted or did not wish to participate. As a result, these data are affected by a potential selection bias based on availability and response to the phone survey. Also, this phone survey collected data at one time point, and individuals were not followed over time. An enhanced general population survey of individuals who are monitored multiple times would be very valuable in accurately documenting the prevalence of chronic pain and comorbid medical conditions. Second, the majority of the data was obtained through self-report and was not verified through external measures. Most of the participants treated at the Dasman Institute were Kuwaiti citizens, and this study did not include those treated in other centers or those who did not have access to a telephone. Many of the patients who participated in this survey also admitted to having diabetes, which is highly prevalent in Kuwait. Given the comorbidities between diabetes and neuropathic pain, this makes it more likely that those surveyed would endorse pain. We did not specifically ask about the presence of fibromyalgia, which can have a lot of overlap with neuropathic-like symptoms. Furthermore, this study did not gather information on the Kuwaiti population as a whole, since the phone numbers were obtained from a list of those who had had access to treatment for a medical condition. It could also be assumed that other subgroups in Kuwait were not included among these subjects. Thus, these findings may not generalize to the country as a whole and selection bias should be considered. Third, there is a risk of underreporting of health behavior and medical conditions. For instance, smoking among women in Kuwait is considered culturally unacceptable, which may account for the large differences in reported smoking behavior between men and women. Others may not admit to chronic disabilities and mental health issues. Few also seem to seek psychological treatment despite a high incidence of pain negatively affecting mood. Because of a need among certain individuals to underreport information, the association between depression, obesity, and medical health, strongly supported elsewhere,47 may not be as strong in this study. Finally, we chose to translate the survey data from Arabic into English. Subtle differences due to translation may exist. A nationwide epidemiologic survey which included more individuals and captured multiple constructs of pain, mood, activity interference, and overall quality of life using mobile technology would be valuable in documenting a more accurate incidence of pain and associated medical conditions in Kuwait and other Arab countries.
Despite these limitations, this survey study suggests that there is a high incidence of chronic pain among a sample of adults who received care at a medical center in Kuwait and that this may represent an underreported and undertreated condition in this country and in the Gulf Cooperation Council (GCC) region. In particular, women reported a higher incidence of pain and pain intensity than men, and obesity and diabetes can be considered as risk factors for neuropathic pain. Strategies to introduce behavioral lifestyle changes targeted among those individuals with neuropathic pain characteristics should be encouraged in order to improve future health in Kuwait. Successful pain detection and eventual treatment are considered important to improve quality of life of patients and reduce the distress frequently associated with chronic pain. Furthermore, detection of neuropathic pain in diabetic patients specifically can help to prevent potential progressive sensory loss and long-term health-related complications.
Acknowledgments
The authors would like to recognize Hidaya Abdalla, who completed the surveys for this study, and Mohammed Issa and Salman Alharbi for their assistance with the study design. Thanks are also extended to the Information Technology Department at the Dasman Diabetes Institute for their assistance in setting up the call recording system. A portion of this study was presented at the 35th Annual Meeting of the American Pain Society in May 12, 2016, and the abstract was published in the Journal of Pain Research, April 2016, Volume 17, Issue 4, Supplement page S11. Also a portion of this study was presented at the 16th World Congress on Pain, September 27, 2016; Yokohama, Japan.. This study was funded by a grant through the Kuwait Foundation for the Advancement of Science and the Dasman Diabetes Institute (RA 2014-039).
Disclosure
The authors report no conflicts of interest in this work.
References
Ehrlich GE. Back pain. J Rheumatol Suppl. 2003;67:26–31. | ||
Garofalo JP, Polatin P. Low back pain: an epidemic in industrialized countries. In: Gatchel RJ, Turk DC, editors. Psychosocial Factors in Pain: Clinical Perspectives. New York, NY: The Guilford Press; 1999:164–174. | ||
Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011. | ||
Leadley RM, Armstrong N, Lee YC, Allen A, Kleijnen J. Chronic diseases in the European Union: the prevalence and health cost implications of chronic pain. J Pain Palliat Care Pharmacother. 2012;26(4):310–325. | ||
Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: a World Health Organization study in primary care. JAMA. 1998;280(2):147–151. | ||
Al-Abbadi I [webpage on the Internet]. Health care equality issues in the Middle East. International Society for Pharmacoeconomics and Outcome Research; 2008. Available from: http://www.ispor.org/news/articles/July09/HCE.asp. Accessed October 4, 2016. | ||
Mokdad AH, Jaber S, Aziz MI, et al. The state of health in the Arab world, 1990-2010: an analysis of the burden of diseases, injuries, and risk factors. Lancet. 2014;383(9914):309–320. | ||
Shehab DK, Al-Jarallah KF. Nonspecific low-back pain in Kuwaiti children and adolescents: associated factors. J Adolesc Health. 2005;36(1):32–35. | ||
Al-Sayegh NA, Salem M, Dashti LF, Al-Sharrah S, Kalakh S, Al-Rashidi R. Pregnancy-related lumbopelvic pain: prevalence, risk factors, and profile in Kuwait. Pain Med. 2012;13(8):1081–1087. | ||
Alshemmari S, Ezzat H, Samir Z, Sajnani K, Alsirafy S. Symptom burden in hospitalized patients with cancer in Kuwait and the need for palliative care. Am J Hosp Palliat Care. 2010;27(7):446–449. | ||
Landry MD, Raman SR, Sulway C, Golightly YM, Hamdan E. Prevalence and risk factors associated with low back pain among health care providers in a Kuwait hospital. Spine. 2008;33(5):539–545. | ||
Al-Qabandi WA, Buhamrah EK, Hamadi KA, Al-Osaimi SA, Al-Ruwayeh AA, Madda J. Inflammatory bowel disease in children, an evolving problem in Kuwait. Saudi J Gastroenterol. 2011;17(5):323–327. | ||
Deeny MC, Al Hamdan E, Ross EL, Edwards RR, Huang CC, Jamison RN. Chronic pain, comorbid medical conditions, and associated risk factors in Kuwait: gender and nationality differences. Pain Med. 2015;16(11):2204–2211. | ||
Merskey H, Bogduk N. Classification of Chronic Pain. 2nd ed. Seattle, WA: IASP Press; 1994. | ||
Bouhassira D, Lanteri-Minet M, Attal N, Laurent B, Touboul C. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain. 2008;136(3):380–387. | ||
Treede RD, Jensen TS, Campbell JN, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 2008;70(18):1630–1635. | ||
Schmader KE. Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clin J Pain. 2002;18(6):350–354. | ||
Torrance N, Lawson KD, Afolabi E, et al. Estimating the burden of disease in chronic pain with and without neuropathic characteristics: does the choice between the EQ-5D and SF-6D matter? Pain. 2014;155(10):1996–2004. | ||
Smith BH, Torrance N. Epidemiology of neuropathic pain and its impact on quality of life. Curr Pain Headache Rep. 2012;16(3):191–198. | ||
Duale C, Ouchchanel L, Schoeffler P, EDONIS Investigating Group; Dubray C. Neuropathic aspects of persistent postsurgical pain: a French multicenter survey with a 6-month prospective follow-up. J Pain. 2014;15(1):e1–e24. | ||
Attal N, Lanteri-Minet M, Laurent B, Fermanian J, Bouhassira D. The specific disease burden of neuropathic pain: results of a French nationwide survey. Pain. 2011;152(12):2836–2843. | ||
Dermanovic DC, Hrabac P, Skegro D, et al. The impact of neuropathic pain and other comorbidities on the quality of life in patients with diabetes. Health Qual Life Outcomes. 2014;12:170–171. | ||
Bouhassira D, Letanoux M, Hartemann A. Chronic pain with neuropathic characteristics in diabetic patients: a French cross-sectional study. PLoS One. 2013;8(9):e74195. | ||
Jacovides A, Bogoshi M, Distiller LA, et al. An epidemiological study to assess the prevalence of diabetic peripheral neuropathic pain among adults with diabetes attending private and institutional outpatient clinics in South Africa. J Int Med Res. 2014;42(4):1018–1028. | ||
Liberman O, Peleg R, Shvartzman P. Chronic pain in type 2 diabetic patients: a cross-sectional study in primary care setting. Eur J Gen Pract. 2014;20(4):260–267. | ||
Hoffman DL, Sadosky A, Alvir J. Cross-national burden of painful diabetic peripheral neuropathy in Asia, Latin America, and the Middle East. Pain Pract. 2009;9(1):35–42. | ||
Almutairi B. A Strategic Roadmap for Achieving the Potential Benefits of Electronic Health Record System in the State of Kuwait. London: University College; 2011. | ||
Daousi C, MacFarlane IA, Woodward A, Nurmikko TJ, Bundred PE, Benbow SJ. Chronic painful peripheral neuropathy in an urban community: a controlled comparison of people with and without diabetes. Diabet Med. 2004;21(9):976–982. | ||
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. | ||
Daut RL, Cleeland CS, Flanery RC. Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain. 1993;17(2):197–210. | ||
Harifi G, Ouilki I, El Bouchti I, et al. Validity and reliability of the Arabic adapted version of the DN4 questionnaire (Douleur Neuropathique 4 questions) for differential diagnosis of pain syndromes with a neuropathic or somatic component. Pain Pract. 2011;11(2):139–147. | ||
Bouhassira D, Attal N, Alchaar H, et al. Comparison of pain syndromes with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005;114(1–2):29–36. | ||
Spallone V, Morganti R, D’Amato C, Greco C, Cacciotti L, Marfia GA. Validation of DN4 as a screening tool for neuropathic pain in painful diabetic polyneuropathy. Diabet Med. 2012;29(5):578–585. | ||
Harifi G, Amine M, Ait Ouazar M, et al. Prevalence of chronic pain with neuropathic characteristics in the Moroccan general population: a national survey. Pain Med. 2013;14(2):287–292. | ||
Seidell JC, Flegal KM. Assessing obesity: classification and epidemiology. Br Med Bull. 1997;53(2):238–252. | ||
Messier SP, Milhalko SWL, Legault C, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: The IDEA randomized clinical trial. JAMA. 2013;310(12):1263–1273. | ||
Mosaad AT, Younis MA. Health policies and intervention strategies: a description of current issues and approaches to care of the public health and health care system in the United Arab Emirates. J Health Care Finance. 2014;40(3):86–100. | ||
Sweileh WM, Zyoud SH, Al-Jabi SW, Sawalha AF. Quantity and quality of obesity-related research in Arab countries: assessment and comparative analysis. Health Res Policy Syst. 2014;12:33. | ||
Davis JA, Robinson RL, Le TK, Xie J. Incidence impact of pain conditions and comorbid illness. J Pain Res. 2001;4:331–345. | ||
Dworkin RH, O’Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132(3):237–251. | ||
Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–173. | ||
Dworkin RH, O’Connor AB, Kent J, et al; International Association for the Study of Pain Neuropathic Pain Special Interest Group. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain. 2013;154(11):2249–2261. | ||
Torrance N, Ferguson JA, Afolabi E, et al. Neuropathic pain in the community: more under-treated than refractory? Pain. 2013;154(5):690–699. | ||
Eccleston C, Hearn L, Williams AC. Psychological therapies for the management of chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2015;(10):CD011259. | ||
Schofferman J, Fishman SM, Harden RN, Kirschner KL. Did we reach too far? The opioid epidemic and chronic pain. PM R. 2014;6:78–84. | ||
Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012;308:749–750. | ||
Abou Abbas L, Salameh P, Nasser W, Nasser Z, Godin I. Obesity and symptoms of depression among adults in selected countries of the Middle East: a systematic review and meta-analysis. Clin Obes. 2015;5(1):2–11. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.