Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 14
Prevalence, Clinical Manifestations, and Treatment Pattern of Patients with Rheumatoid Arthritis Attending the Rheumatology Clinic at Tikur Anbessa Specialized Hospital, Ethiopia: A Cross-Sectional Study
Received 27 July 2022
Accepted for publication 27 September 2022
Published 14 October 2022 Volume 2022:14 Pages 221—229
DOI https://doi.org/10.2147/OARRR.S383778
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Chuan-Ju Liu
Zerihun Bogale,1 Yeweyenhareg Feleke2
1Department of Internal Medicine, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 2Endocrinology and Metabolism Unit, Department of Internal Medicine, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Zerihun Bogale, Tel +251-913-83-31-57, Email [email protected]
Background: Rheumatoid arthritis (RA) is an a chronic inflammatory disease characterized by symmetric polyarticular inflammation that can lead to progressive joint damage. It is said to be rare among black Africans, even though there have been limited reports from some African countries and no study has been done on RA in Ethiopia. This study determined the prevalence, clinical features, and treatment of rheumatoid arthritis in Tikur Anbessa Specialized Hospital (TASH).
Methods: A cross-sectional study design was conducted on diagnosed patients with RA attending the rheumatology clinic at TASH from November 2018 to February 2019. Data was collected through patient interviews and chart reviews. The dataset was subjected to descriptive statistical analysis using the Statistical Package for Social Sciences (SPSS) version 25.
Results: A total of 1116 patients attended a rheumatologic clinic with rheumatologic complaints. The prevalence of rheumatoid arthritis was 18.5% (206/1116). Females were mostly affected (F:M 4.6:1). One hundred nineteen (57.8%) were between 35 and 64 years of age. The seropositivity for rheumatoid factor was 47.1%. Almost all patients had morning stiffness (89.8%) and joint pain (97.1%), with the majority (74.8%) having both small and large joint involvement. Nearly half of the patients, 99 (48.1%), had a joint deformity. Comorbid conditions seen in this study were hypertension (17%), overweight in 43 (20.9%), and obesity in 8 (3.9%). Methotrexate was the most prescribed agent (82.5%), both as monotherapy and along with other medications, but 139 (67.5%) of them were on prednisolone, which 2/3 (122) of patients took for 6 months in duration.
Conclusion: RA accounted for nearly one-fifth of the patients coming to the rheumatology clinics, with females affected more, which is similar to reports from some African countries. Disease-modifying anti-rheumatic drugs are the most prescribed agents, but most patients are on a prolonged dose of prednisolone.
Keywords: rheumatoid arthritis, rheumatology clinic, Tikur Anbessa Specialized Hospital, Ethiopia
Introduction
Rheumatoid arthritis (RA) is an a systemic autoimmune condition with protean manifestations. The primary expression of the disease occurs in the synovial tissues and is characterized by symmetric polyarticular inflammation, which can lead to progressive joint damage. The global burden of RA is estimated to be around 0.24%, and females are affected more than males.1 The prevalence of RA in low- or middle-income countries (without including Africa) is in the range of 0.37% to 1.25%.2 Likewise, in Africa, the prevalence of RA is 0.1% to 2.5% in urban settings and 0.07% to 0.4% in rural settings.3 However, the hospital-based study done in Africa shows varying results on the prevalence of RA, with as low as 2.2% and as high as 33%.Patients with RA are likely to have an increased risk of subclinical atherosclerosis and cardiovascular disease, and chronic inflammation in RA leads to impaired glucose metabolism due to insulin resistance and impaired beta-cell function.7
Comorbid conditions play an important role in the management and treatment outcomes of rheumatoid arthritis patients. COMORA (COMOrbidities in Rheumatoid Arthritis) study found that comorbid conditions with RA were depression (15%), cardiovascular events (6%), elevated blood pressure (1.2%), and hyperglycemia (3.3%).8 Similarly, a cross-sectional study done in Saudi Arabia found that the comorbidity conditions associated with RA were hypertension (35.9%), diabetes (30.9%), osteoporosis (25.8%), and dyslipidemia (19.4%).9 But, a recent prospective study done in India showed metabolic syndrome was found to be in 45% of the RA group compared to 22.7% of the control group according to joint consensus 2009 criteria, and the RA group was also significantly more likely to have low high-density lipoprotein (65%), elevated blood pressure (60%) levels and abnormal sugar (28%).10 Smoking is the major known environmental risk factor for RA, with an increased tendency of seropositivity for rheumatoid factor and a higher risk of anti-citrullinated protein antibody (ACPA)-positive RA.11,12
The main treatments for RA are disease-modifying anti-rheumatic drugs (DMARDS) and oral glucocorticoids (GC), which are still widely used nearly 73 years after they were introduced. 13,14 GCs have beneficial effects on improving symptoms of active RA by reducing joint pain, swelling, and stiffness. They are used mostly as a short-term measure to induce a rapid reduction in disease activity till the effects of slower-acting DMARDs come into the picture.13
Even though RA is frequently reported from western countries, it is said to be rare among black Africans, with limited reports from some African countries, particularly no reports from Ethiopia. To our knowledge, this is the first study on rheumatoid arthritis patients attending an a rheumatology clinic in Tikur Anbessa Specialized Hospital, Ethiopia. Therefore, this study assessed the magnitude, clinical manifestations, and pattern of medication for patients with rheumatoid arthritis.
Methods and Materials
Study Area and Study Population
A cross-sectional study was conducted among adult patients attending the rheumatology clinic at Tikur Anbessa specialized, one of the oldest teaching hospitals in our country. The hospital has various specialty clinics, including this rheumatology clinic, one of which runs once per week and appoints patients at intervals of one to four months for regular follow-up. The service is mostly provided by internal medicine residents with support from consultants. This study was conducted from November 2018 to February 2019.
Inclusion and Exclusion Criteria
Patients with RA diagnosed according to the 2010 ACR/EULAR (American College of Rheumatology/European League Against Rheumatism) with those aged greater than 18 years were included in this study, while other rheumatologic diseases based on history and patient chart review were excluded.
Sample Techniques and Procedures
The sample size was calculated using the single population (p) formula N=Z2P(1-p)/W2 taking the 8.5% prevalence of RA among rheumatologic patients from a previous study conducted in the Democratic Republic of Congo and 4% marginal error (w), and a confidence interval (CI) of 95%. Based on this formula, the calculated sample size was 187. Because there were non-responses (with an acceptable level of 10%), 10% of the calculated sample size was added to the estimated sample size, making the final sample size 206. Patients with rheumatoid arthritis fulfilling the ACR/EULAR criteria that were seen in the rheumatology clinic during the study period were selected by lottery method for every 4th patient from the logbook.
The data was collected by trained nurses. A structured questionnaire was used, and patients were interviewed by trained nurses at the TASH Rheumatology follow-up clinic during the study period to fill in the data collection format with relevant information about patient socio-demographic characteristics, the duration of illness, symptoms, related risk factors, and patient drug history.
Laboratory data, details of patient medications, and some of the clinical characteristics of the patient were obtained from the patient’s medical record.
Bodyweight and height were measured to calculate body mass index (BMI) (Bodyweight (kg) / Body height/(m2)). Waist circumference was measured by placing an a tape measure around the bare abdomen at the midpoint between the lower margin of the last palpable rib and the top of the iliac crest of the hip bone. Abdominal obesity was defined as a waist circumference of ≥94 cm for men and ≥80 cm for women.15
Blood pressure was taken three times on the left arm of the rested study participants for 5 minutes in a sitting position, using a mercury sphygmomanometer. Raised blood pressure was defined as systolic blood pressure (SBP) of 140 mmHg and/or diastolic blood pressure (DBP) of 90 mmHg, and the mean of the three measurements was taken for analysis.16,17
During the preparatory stage, the questionnaires were carefully designed and pretested on 5% of the study population to minimize errors. The collected data was checked for consistency, completeness, and odd answers immediately at the end of the interview with the investigators.
Operational Definition
- Rheumatoid arthritis – Already diagnosed with RA and on follow-up based on 2010 ACR/EULAR (a score of ≥6/10 is needed for classification of a patient as having definite RA).18
Data Analysis
The collected data was checked for completeness, organized, coded, cleaned, entered, and analyzed using SPSS version 25.
Results
Socio-Demographic Characteristics of Patients with RA
During this study, patients with rheumatologic disease (n = 1116) were seen at the rheumatology clinic. Out of those, 206 patients with an established diagnosis of rheumatoid arthritis on follow-up with those on treatment between 6 months and ten years were included in the study, making the proportion of rheumatoid arthritis about 18.5%.
Out of the 206 adult patients who participated in the study, 169 (82%) of them were females, making Females (F):Males (M) = 4.6:1. Regarding the age majority, 119 (57.8%) were between 35 and 64 years of age. The majority (131, or 63.6%) of the study were married, and 174, or 84.5%) were Christian in religion. Most of the 151 (73.3%) were in urban areas, and more than half the 123 (59.7%) had primary and secondary education. For forty-two (20.4%) salaried employees, almost all had (98.5%) no history of smoking, and 20 (9.7%) had a family history of diabetes (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Rheumatoid Arthritis Patients (N = 206) |
Clinical Features of RA and Comorbid Conditions
As shown in Table 2, almost all patients had morning stiffness (89.8%) and joint pain (97.1%), with the majority (74.8%) having both small and large joint involvement. Nearly half of the patients (48.1%) had a joint deformity. Thirty-five (17%) patients had a history of hypertension, and almost all were on treatment. Three (1.5%) patients had heart disease (1 ischemic heart disease, 1 rheumatic valvular heart disease, and 1 peripheral vascular disease with right above knee amputation), and 2 patients had a history of thyroid disease (1 hyperthyroidism on methimazole and 1 post-thyroidectomy hypothyroidism on levothyroxine).
 |
Table 2 Pattern of Joint Involvement and Comorbid Conditions of Rheumatoid Arthritis Patients (N = 206) |
Frequency of Blood Pressure, Anthropometric and Laboratory Measurements of RA
In 23 (11.2%) study participants of patients with rheumatoid arthritis had elevated blood pressure, 16 (7.8%) had abnormal sugar, 127 (61.7%) of the study participants had elevated waist circumference, 43 (20.9%) had overweight and 8(3.9%) had obesity. In our study, we found that rheumatoid factor tests were positive in 97 (47.1%) (Figure 1). Those with seronegative RA on treatment were also included in this study. Anti-CCP was not done because the test was not available in the country during the study period.
 |
Figure 1 Frequency of blood pressure, anthropometric, and rheumatoid factor of rheumatoid arthritis patients (N = 206). |
A Pattern of Medication Ordered for Patients with RA
Regarding ordered medication, both prednisolone and methotrexate concomitantly were the most prescribed medication 65 (31.6%), followed by triple medication (prednisolone, methotrexate, and chloroquine) 45 (21.8%). Prednisone alone was prescribed only for 19 (9.2%) patients, in the same way, methotrexate alone was prescribed for 24 (11.7%) and chloroquine alone for 7(3.4%) patients (Figure 2), but one hundred thirty-nine (67.5%) of two hundred six study participants were on oral prednisolone alone and along with other medications. More than 2/3 (122) out of one hundred thirty-nine patients took steroids for greater than six months. Methotrexate alone and other medications were prescribed for 170 (82.5%) of the study participants. Most study subjects were on low doses (≤7.5mg) of both prednisolone (43.7%) and methotrexate (41.3%) (Table 3).
 |
Table 3 Frequency and Percentage of Dosage of Commonly Prescribed Medications for Rheumatoid Arthritis Patients (N = 206) |
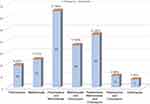 |
Figure 2 Frequency and percentage of drug prescribed for Rheumatoid Arthritis patients (N = 206). |
Discussion
Our results indicate that 18.5% of outpatients affected by rheumatic diseases attending the rheumatology clinic of Tikur Anbessa Specialized hospital were diagnosed with RA. The frequency of patients with RA seen in our rheumatology clinic is higher than that reported in Burkina Faso (2.2%), the Democratic Republic of Congo (8.5%), and Nigeria (10.6%) but significantly less than reported in Kenya (33%).4–6,19
The female-to-male ratio of 4.6:1 was recorded in this study, higher than the 4.25:1 by Singbo et al4 but less than 6.1:1 by Obagwu et al,5 the 6.5:1 by OWINO et al6 and the 8:1 by Malemba et al.19 Predominant age-affected ranges were between 35 and 64 years, which almost corresponded to those reported in Africa.4,6 About 89.8% of our study subjects had morning joint stiffness, and nearly half (48.1%) had joint deformities. Nearly 2/3 of the study participants had both small and large joint involvement almost similar to reports from Africa.5,6 There is the strongest connection between cigarette smoking and seropositive RA.11,12 Most of our study participants had no history of active cigarette smoking, and only 3 patients had a history of past smoking similar to what was reported by Malemba et al19 and Ohagwu et al.5 The percentage of seropositive patients for rheumatoid factor in our study (47.1%) was nearly similar to those reported from Congo (48.6%)19 and lower than what was reported in other African countries.4–6
The most common comorbid condition seen in our study participants was cardiovascular diseases (hypertension, ischemic heart disease, valvular heart disease, and peripheral vascular disease), and endocrine diseases like thyrotoxicosis and hypothyroidism were rare findings in this group of patients.7–9,20 The tendency of elevated blood pressure, overweight, and elevated waist circumference were appreciated in our study that was similar to those reported by Naik et al10 and Ozmen et al21 with some variation. Impaired glucose metabolism was also seen in our study participants but lower than what was reported in other studies.22,23
The ordered medication of RA in this study showed that methotrexate is the most prescribed agent, both as monotherapy and along with other medications, which was similar to a report from Burkina Faso, Nigeria, and Kenya.4–6 even-though it goes with the EUALAR guidelines recommendation for RA management, but 67.5% of our study participants were on prednisolone more than two-thirds of patients took for greater than 6 months in duration in contrast to the current established practice of using prednisolone duration as a bridge therapy.13 During the study period, despite the above medications, other DMARDs or biologicals and anti-B-cell therapy were not used because the drugs are not available in the country.
The limitation of the current study is that it is a single-center study and a short period, which showed no information on the long-term effects of treatment and risk factors to treatment, because the majority of patients are taking methotrexate and steroids for a long duration.
Conclusions
In this study, we found out that RA occurring is more common in patients with rheumatic diseases and females are affected more than males, and articular symptoms are classical and with significant joint deformity. DMARDS are the most prescribed agents, but most of the patients are on the prolonged duration of prednisolone.
Recommendations
We recommended conducting a multicenter study to look for the effects of long-term treatment and to follow EULAR recommendations during medication initiation and management of patients with rheumatoid arthritis.
Authors’ Information
The corresponding author was graduated with a specialty certificate of internal medicine (MD, Internist) from the Department of Internal Medicine, School of Medicine, College of Health Sciences, Addis Ababa University and currently working at Negele Arsi General Hospital and medical college, Ethiopia. The second author is a professor, researcher, and lecturer (MD, CSIM, MPhil) at the Endocrinology and Metabolism Unit, Department of Internal Medicine, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia.
Human and Animal Rights
No human or animal was used in this study.
Abbreviations
ACPA, Anti-citrullinated protein antibody; ACR, American College of Rheumatology; BMI, Body mass index; cm, centimeter; COMORA, COMOrbidities in Rheumatoid Arthritis; D, Day; DBP, Diastolic blood pressure; DMARDS, Disease-modifying anti-rheumatic drugs; EULAR, European League Against Rheumatism; F, Female; GC, Glucocorticoid; Kg, kilogram; M, Male; M, meter; Mg, milligram; mmHg, millimeters of mercury; N, Number; PO, by mouth, orally (from the Latin ”per os”); RA, Rheumatoid arthritis; RF, Rheumatoid factor; SBP, Systolic blood pressure; SPSS, Statistical Package for Social Sciences; TASH, Tikur Anbessa Specialized Hospital.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Statement
The study was conducted following the Helsinki Declaration. Ethical clearance was obtained from Internal Medicine Department Research and Ethical Review Committee, Department of Internal Medicine, School of Medicine, College of Health Sciences, Addis Ababa University, with approval number (Ref no IMD/350/10). Then, permission was obtained from the Rheumatology unit before data collection.
Consent for Publication
The purpose and significance of the study were explained, and informed written consent was received from each study subject. Patients’ confidentiality, equity of services, and the interests of patients were ensured during the study period by informing the data collectors of ethical issues. The interview scripts were coded.
Acknowledgments
We would like to acknowledge Addis Ababa University, College of Health Science, and School of Medicine for their financial support. We would also acknowledge those individuals (Nurses, Residents, and Senior Consultants) involved in the care of rheumatology patients. We are also grateful to the participants of the study for their willingness and cooperation during the data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is, in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors report no funding for this study.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Cross M, Smith E, Hoy D, et al. The global burden of rheumatoid arthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(7):1316–1322. doi:10.1136/annrheumdis-2013-204627
2. Rudan I, Sidhu S, Papana A, et al. Prevalence of rheumatoid arthritis in low- and middle-income countries: a systematic review and analysis. J Glob Health. 2015;5(1):010409. doi:10.7189/jogh.05.010409
3. Usenbo A, Kramer V, Young T, Musekiwa A. Prevalence of arthritis in Africa: a systematic review and meta-analysis. PLoS One. 2015;10(8):e0133858. doi:10.1371/journal.pone.0133858
4. Ouédraogo DD, Singbo J, Diallo O, Sawadogo SA, Tiéno H, Drabo YJ. Rheumatoid arthritis in Burkina Faso: clinical and serological profiles. Clin Rheumatol. 2011;30(12):1617–1621. doi:10.1007/s10067-011-1831-1
5. Ohagwu KA, Centre FM, Adelowo OO. Pattern of rheumatoid arthritis in Nigeria; study of patients pattern of rheumatoid arthritis in Nigeria; Study of; 2017.
6. Owino BO, Oyoo GO, Otieno CF. Socio-demographic and clinical aspects of rheumatoid arthritis. East Afr Med J. 2009;86:204–211. doi:10.4314/eamj.v86i5.54190
7. Avina-Zubieta JA, Thomas J, Sadatsafavi M, Lehman AJ, Lacaille D. Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. 2012;71(9):1524–1529. doi:10.1136/annrheumdis-2011-200726
8. Dougados M, Soubrier M, Antunez A, et al. Prevalence of comorbidities in rheumatoid arthritis and evaluation of their monitoring: results of an international, cross-sectional study (COMORA). Ann Rheum Dis. 2014;73(1):62–68. doi:10.1136/annrheumdis-2013-204223
9. Al-Bishri J, Attar S, Bassuni N, et al. Comorbidity profile among patients with rheumatoid arthritis and the impact on prescriptions trend. Clin Med Insights Arthritis Musculoskelet Disord. 2013;6:S11481. doi:10.4137/CMAMD.S11481
10. Naik M, Bhat T, Jalalie U, Ganayie MT, Waseem M, Bhat A. Prevalence and predictors of metabolic syndrome in rheumatoid arthritis. Int J Res Med Sci. 2017;5(8):3322. doi:10.18203/2320-6012.ijrms20173179
11. Baka Z, Buzás E, Nagy G. Rheumatoid arthritis and smoking: putting the pieces together. Arthritis Res Ther. 2009;11(4):238. doi:10.1186/ar2751
12. Bang S, KH Lee, Kyung CS, Lee HS, Lee KW, Bae S. Smoking increases rheumatoid arthritis susceptibility in individuals carrying the HLA-DRB1 shared epitope, regardless of RF and ACPA. Arthritis Rheum. 2010;62(2). doi:10.1002/art.27272
13. Smolen JS, Landewé R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76(6):960–977. doi:10.1136/annrheumdis-2016-210715
14. Philip S, Charles H, Howard F, Edward C. Effect of cortisone and pituitary adrenocorticotropic hormone (ACTH) on rheumatic diseases. J Am Medicat. 1950;144(16):1327–1335.
15. Zimmet P, Alberti KGMM, Serrano Ríos M. Una nueva definición mundial del síndrome metabólico propuesta por la Federación Internacional de Diabetes: fundamento y resultados. Rev Española Cardiol. 2005;58(12):1371–1376. doi:10.1016/S0300-8932(05)74065-3
16. Whelton PK, Carey RM, Aronow WS, et al. High blood pressure clinical practice guideline: executive summary 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults exec Hypertension; 2017.
17. Unger T, Borghi C, Charchar F, et al. International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–1357. doi:10.1161/HYPERTENSIONAHA.120.15026
18. Aletaha D, Neogi T, Silman AJ, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–2581. doi:10.1002/art.27584
19. Malemba J, Mbuyi-Muamba J, Mukaya J, et al. The phenotype and genotype of rheumatoid arthritis in the Democratic Republic of Congo. Arthritis Res Ther. 2013;15(4):R89. doi:10.1186/ar4269
20. Mccoy SS, Crowson C, Gabriel SE, Matteson EL. Hypothyroidism as a risk factor for development of cardiovascular disease in patients with rheumatoid arthritis. J Rheumatol. 2012;39(5):954–958. doi:10.3899/jrheum.111076
21. Ozmen M, Yersal O, Ozturk S, Solmaz D, Koseeoglu MH. Prevalence of the metabolic syndrome in rheumatoid arthritis. Eur J Rheumatol. 2014;1(1):1–4. doi:10.5152/eurjrheum.2014.001
22. Hoes JN, van der Goes MC, van Raalte DH, et al. Glucose tolerance, insulin sensitivity and -cell function in patients with rheumatoid arthritis treated with or without low-to-medium dose glucocorticoids. Ann Rheum Dis. 2011;70(11):1887–1894. doi:10.1136/ard.2011.151464
23. Thirumal DG, Rajapandian DSS, Rajkumar DM, Dharmaraj DC. A study of the association of impaired glucose metabolism in patients with newly detected rheumatoid arthritis. IOSR J Dent Med Sci. 2016;15(09):108–134. doi:10.9790/0853-150907108134
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
