Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Prevalence and Risk Factors of Osteoporosis in Patients with Type 2 Diabetes Mellitus in Nanchang (China): A Retrospective Cohort Study
Authors Li T, Hu L, Yin XL, Zou Y, Fu HY, Li HL
Received 26 April 2022
Accepted for publication 14 August 2022
Published 28 September 2022 Volume 2022:15 Pages 3039—3048
DOI https://doi.org/10.2147/DMSO.S372348
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Ting Li,1,* Ling Hu,1,* Xiao-Ling Yin,1 Yi Zou,1 Hai-Yan Fu,1 Hong-Lin Li2
1Department of Endocrinology, The First Hospital of Nanchang (The Third Affiliated Hospital of Nanchang University), Nanchang, Jiangxi, People’s Republic of China; 2Department of Biochemistry, Medical College of Georgia, Augusta, GA, USA
*These authors contributed equally to this work
Correspondence: Ling Hu, Department of Endocrinology, The First Hospital of Nanchang (The Third Affiliated Hospital of Nanchang University), No.128 of Xiangshan North Road, Donghu District, Nanchang, Jiangxi, 330008, People’s Republic of China, Tel +86 0791-88862350, Fax +86 0791-6782945, Email [email protected]
Objective: To retrospectively review the clinical data of type 2 diabetes mellitus (T2DM) patients hospitalized in Nanchang, China, summarized the prevalence of osteoporosis (OP) in T2DM patients in this area, and analyzed related influencing factors.
Methods: The clinical data of hospitalized patients with T2DM were collected retrospectively. According to the results of bone mineral density test, the subjects were divided into the normal bone mass group, the osteopenia group, and the OP group. Age, gender, educational background, body mass index (BMI), waist-to-hip ratio (WHR), duration of T2DM, glycosylated hemoglobin, serum lipids, and complications of T2DM in the three groups were analyzed and compared.
Results: The prevalence of OP in patients with T2DM was 35.77%. There were statistically significant differences in age, gender, BMI, WHR, duration of T2DM, educational background, the level of high-density lipoprotein cholesterol (HDL-C), the prevalence of diabetic retinopathy (DR), and diabetic peripheral neuropathy among the three groups (P < 0.05). Logistic regression analysis showed that increasing age, prolonged duration of T2DM, low BMI, high levels of HDL-C, and complicated DR were risk factors for osteopenia and OP.
Conclusion: The prevalence of OP in T2DM was high. Risk factors for abnormal bone mass in T2DM might be females, advanced age, long duration of T2DM, low BMI, high levels of HDL-C, and diabetic microangiopathy.
Keywords: type 2 diabetes mellitus, osteoporosis, risk-factors, prevalence
Introduction
Type 2 diabetes mellitus (T2DM) is a common metabolic disease and its prevalence has been increasing with the aging population. The current prevalence rate of T2DM in China is 11.2%.1 Osteoporosis (OP) is also a commonly diagnosed metabolic disease in Chinese population over 50 years old, with a prevalence of 20.7% in females and 14.4% in males. The prevalence of OP is significantly increased in people over 60 years old, especially in females.2 Many studies have shown that patients with T2DM have a higher risk of fracture than non-diabetic population and are more prone to OP.3–9 Moreover, after fracture, diabetic patients with OP are prone to develop a series of complications such as pneumonia and bed sores, and even death. In the present study, we retrospectively reviewed the clinical data of T2DM patients hospitalized in Nanchang, China, aiming to summarize the prevalence of OP in T2DM patients in this area and analyze related influencing factors.
Materials and Methods
General Data
This study was approved by the Ethics Committee of the Nanchang First Hospital, China (Approval code: KY2021072). Patients with T2DM hospitalized at the Department of Endocrinology, Nanchang First Hospital, from June 2018 to September 2021 were selected as study subjects. The inclusion criteria were: 1. enrolled subjects met the diagnostic criteria for T2DM formulated by the World Health Organization (WHO) in 1999: (1) present with diabetes symptoms (ie polyuria, polydipsia, polyphagia, and unexplained weight loss caused by hyperglycemia) plus any one or more of the following criteria: (a) Random blood sugar ≥ 11.1 mmol/L or (b) fasting Blood glucose ≥ 7.0 mmol/L or (c) blood glucose ≥ 11.1 mmol/L 2 hours after glucose load; 2. aged > or equal to 18–75 years old. The exclusion criteria were patients: (1) with type 1 diabetes mellitus (T1DM) and other types of diabetes mellitus; (2) in critical condition or with abnormal mental conditions who could not cooperate with the medical history and relevant physical examinations; (3) patients that were bedridden, or with serious long-term infections, severe heart, lung, liver, and kidney diseases; (4) long-term administration of immunosuppressants or glucocorticoids; (3) bone tumors, hyper- or hypothyroidism, diseases of the adrenal glands, gonads, and other diseases affecting bone metabolism.
Research Methods
The subjects were retrospectively investigated, and the actual data (clinical and laboratory) of the subjects were obtained from electronic medical records. The following clinical data were collected on the subjects: gender, age, body mass index (BMI), duration of T2DM, glycated hemoglobin (HbA1c) (Huizhong MQ-2000PT), serum lipids, fundus photography, results of neurogram of both lower limbs, and so on.
According to the diagnostic criteria for OP issued by the WHO in 1994, bone mineral density (BMD) levels in premenopausal women and men under 50 years of age were represented by the Z-value. Normal bone mass was defined as a Z score of >–2.0, and osteopenia as a Z score of ≤–2.0. BMD levels in postmenopausal women and men over 50 years of age were expressed as T-values. Normal bone mass was defined as a T score of ≥–1.0, osteopenia as –2.5 < T score <–1.0, and OP as a T score of ≤–2.5.10 Fragility fracture was also included in the diagnosis of osteoporosis. In this study, both hip and lumbar were used for T/Z score measurements. The same DEXA machine (Hologic Explorer, USA) was used to measure BMD for all patients. Subjects were divided into the normal bone mass, osteopenia, and OP groups. The Research Ethics Committee of Nanchang First Hospital approved the present study.
Statistical Analysis
SPSS 22.0 software was used for statistical analysis. All continuous variables satisfying the normal distribution were expressed as mean ± standard deviation (X ± SD). The t-test was used to compare parameters between two groups, and analysis of variance was used to compare parameters among multiple groups. The categorical variables were compared by the chi-square test. Risk factors of abnormal bone mass were analyzed by logistic regression. P < 0.05 was considered statistically significant.
Results
General Clinical Data
A total of 1697 patients with T2DM were included this study. There were 733 females and 964 males, with an age range of 25–75 years. The prevalence of OP was 35.77%, the prevalence of osteopenia was 44.67%, and the prevalence of normal bone mass was 19.56%. There existed statistically significant differences in age, gender, BMI, waist-to-hip ratio (WHR), duration of T2DM, and educational backgrounds among the three groups (P < 0.05) (Table 1). There were statistically significant differences in age, BMI, and WHR among the three groups of female patients (P<0.05) (Table 2). There were statistically significant differences in age, BMI, course of disease, and education level among the three groups of male patients (P<0.05) (Table 3).
 |
Table 1 Comparison of Clinical Data Among All Patients |
 |
Table 2 Comparison of Clinical Data Among Female Patients |
 |
Table 3 Comparison of Clinical Data Among Male Patients |
Glucose and Lipid Metabolism in Patients with Different Bone Mass
There were no significant differences in HbA1c, total cholesterol (TC), triglyceride (TG), and low-density lipoprotein cholesterol (LDL-C) among patients with different bone mass (P > 0.05). The differences in the levels of high-density lipoprotein cholesterol (HDL-C) were statistically significant among the three groups (P < 0.05) (Table 4). There was a statistically significant difference in high-density lipoprotein cholesterol (HDL-C) among the three groups in male patients (P<0.05) (Table 5), but not in female patients (Table 6).
 |
Table 4 Comparison of Glucose and Lipid Metabolism Among All Patients |
 |
Table 5 Comparison of Glucose and Lipid Metabolism Among Male Patients |
 |
Table 6 Comparison of Glucose and Lipid Metabolism Among Female Patients |
Diabetic Complications in Patients with Different Bone Mass
The comparison of diabetic complications among patients with different bone mass groups showed that the prevalence of diabetic retinopathy (DR) and diabetic peripheral neuropathy (DPN) were statistically different among the three groups of all patients (P < 0.05) (Table 7), male patients (P < 0.05) (Table 8), and female patients (P < 0.05) (Table 9).
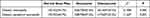 |
Table 7 Comparison of Diabetic Complications Among All Patients |
 |
Table 8 Comparison of Diabetic Complications Among Male Patients |
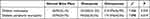 |
Table 9 Comparison of Diabetic Complications Among Female Patients |
Factors Influencing Bone Mineral Density in Patients with T2DM
Age, gender, education, duration of T2DM, BMI, HDL-C, the prevalence of DR and DPN were taken as variables and introduced into the multiple regression equation. In all patients, compared with those in the normal bone mass group, age, educational background, BMI, duration of T2DM, levels of HDL-C, and prevalence of DR were the influencing factors of osteopenia. Compared with those in the normal bone mass group, gender, age, BMI, duration of T2DM, levels of HDL-C, and prevalence of DR and DPN were the influencing factors of OP (Table 10).
 |
Table 10 Influencing Factors of Abnormal Bone Mass in All Patients with T2DM |
In male patients, compared with those in the normal bone mass group, educational background (below high school), age, BMI, HDL-C, and diabetic retinopathy were the influencing factors of osteopenia in male patients. Compared with those in the normal bone mass group, age, BMI, HDL-C, diabetic retinopathy, and diabetic peripheral neuropathy were the influencing factors of OP (Table 11). In female patients, compared with in the normal bone mass group, age and BMI are the influencing factors of osteopenia. Compared with those in the normal bone mass group, age, BMI, and the presence of diabetic retinopathy were the influencing factors of OP (Table 12).
 |
Table 11 Influencing Factors of Abnormal Bone Mass in Male Patients with T2DM |
 |
Table 12 Influencing Factors of Abnormal Bone Mass in Female Patients with T2DM |
In patients younger than 45 years, compared with those in normal bone mass group, age, BMI, TG, gender are the influencing factors of osteopenia (Table 13). In patients between 45 and 60 years, compared with those in the normal bone mass group, age, BMI, HDL-C, educational background (below high school), and diabetic peripheral neuropathy were the influencing factors of osteopenia. Compared with those in the normal bone mass group, age, BMI, male gender, diabetic retinopathy, and diabetic peripheral neuropathy were the influencing factors of OP (Table 14). In patients above 60 years, compared with the normal bone mass group, BMI, duration of T2DM, gender (male), HDL-C, and diabetic retinopathy were the influencing factors of osteopenia. Compared with the normal bone mass group, duration of T2DM, gender (male), and diabetic retinopathy were the influencing factors of OP (Table 15).
 |
Table 13 Influencing Factors of Abnormal Bone Mass in T2DM Patients Younger Than 45 Years |
 |
Table 14 Influencing Factors of Abnormal Bone Mass in T2DM Patients Between 45 and 60 Years |
 |
Table 15 Influencing Factors of Abnormal Bone Mass in T2DM Patients Above 60 Years |
Discussion
T2DM and OP are the most common metabolic diseases in middle-aged and older adults, and the prevalence of OP in patients with T2DM is significantly higher than in those without T2DM.11 In the present study, the prevalence of OP in patients with T2DM was 35.77%, which was slightly lower than 37.8% in the meta-analysis by Si.12
Age and gender were risk factors for OP, which was consistent with previous studies.13–17 This might be due to the decreased physical activity with age, decreased calcium absorption in the gut, and decreased synthesis of 1.25-(OH)2D3 in the kidneys.18 The relative and secondary increase in parathyroid hormones may result in a decreased bone turnover rate. Meanwhile, bone absorption will be affected due to the depletion of ovarian follicles in postmenopausal women and the decline in levels of sex hormones. Increased microRNA-151a-3p levels in postmenopausal women promote osteoclast differentiation and affect BMD through targeting SOCS5 and activating the JAK2/STAT3 signaling pathways.19,20
With a longer duration of T2DM, patients are at an increased risk of developing bone mass abnormalities. In patients with T2DM, insulin function gradually declines with prolonged disease duration, and long-term insulin deficiency can lead to continuous hyperglycemia and decreased bone turnover, affecting osteoclast activity and promoting bone resorption.21,22
It was suggested in the present study that BMI might be a protective factor of bone tissue. Several studies23 suggest that bone mineral density increases with increased BMI, which correlates with fracture risk reduction.24 On the one hand, when BMI increases, it can increase the bearing capacity of bone, increase the mechanical stress on bones, and promote bone formation. On the other hand, people with high BMI have higher body fat content, which may be converted into fat-related hormones, such as vitamin D, estrogen, androgen, etc. through the secretion of adipokines, such as leptin, adiponectin, and Tumor Necrosis Factor (TNF), and affect bone metabolism by inflammatory factors that increase bone resorption.13,23
High HDL-C levels are correlated with abnormal bone mass. Ahmed et al25 found that low HDL-C levels had a protective effect on bone mass. A meta-analysis of 12,395 subjects26 also showed that HDL-C could be used as an indicator to predict osteopenia, OP, and even fractures. With the increase of HDL-C, the risk of OP also increases. A study on the differentiation of mesenchymal stem cells showed27 that specific hydroxyl sterols could stimulate the osteogenic differentiation of mesenchymal stem cells, while HDL-C could clear the hydroxyl sterols from peripheral tissues, suggesting that high HDL-C levels might not be conducive to osteogenic differentiation, but the specific mechanism is still unclear.
At present, many studies consider diabetic microangiopathy as a risk factor for OP.28,29 Diabetic microangiopathy (ie diabetic retinopathy and diabetic peripheral neuropathy) is also considered a risk factor for abnormal bone mass. Chronic hyperglycemia and oxidative stress in diabetic patients lead to the accumulation of advanced glycation end products (AGEs), stimulation of the production of inflammatory factors, changes of the vascular endothelial growth factor signal transduction, and affect bone metabolism.30,31 It has been reported that the peripheral nervous system in patients with T2DM regulates bone metabolism through the influence of local neurotransmitters on bone cells and neuromodulation supplied by bone vessels.32 Since DPN may result in loss of coordination, balance, and walking problems,33 low physical activity or lack of activity is common in patients with DPN, especially in those with painful DPN,34 which ultimately leads to decreased bone mass and bone mineral density.
In this study, we presented the analysis results of related risk factors for male and female patients, respectively, and for patients at different ages, respectively. This is the strengths of the present study. However, there were still some limitations in this study. First, we did not analyze the correlations between various metabolic indicators and bone mass in these patients. Future investigations are needed to explore the potential relationships between these parameters. Secondly, no further analysis considering post-menopausal status as a confounding factor was performed when analyzing the gender difference among different groups. Thirdly, as this was a retrospective study, other T2DM- and OP-related parameters (ie fasting blood glucose levels, insulin levels, insulin sensitivity, glucose tolerance, and vitamin D), socioeconomic data (ie calcium consumption status, exercise habits, smoking status, and daily alcohol consumption), and complications (ie diabetic nephropathy, diabetic foot, and diabetic peripheral vascular disease) were not available for all patients. Lastly, all patients included in this study were hospitalized T2dM patients and most of them were admitted due to poor blood sugar control. It might explain why there was no significant difference in the HbA1c levels among groups with different bone mass.
In conclusion, the prevalence of OP in T2DM was high. Risk factors for abnormal bone mass in T2DM were females, advanced age, long duration of T2DM, low BMI, high levels of HDL-C, and diabetic microangiopathy. Therefore, in the clinical treatment of patients with the above risk factors, it might be necessary to strengthen BMD screening, with early bone mass screening and intervention.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of The First Hospital of Nanchang. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes. 2021;13(04):315–409.
2. Chinese Medical Association. Guideline for primary care of primary osteoporosis (2019). Chin J Gen Pract. 2020;19(04):304–315.
3. Jiang N, Xia W. Assessment of bone quality in patients with diabetes mellitus. Osteoporos Int. 2018;29(8):1721–1736.
4. Poiana C, Capatina C. Fracture risk assessment in patients with diabetes mellitus. J Clin Densitom. 2017;20(3):432–443.
5. Thong EP, Herath M, Weber DR, et al. Fracture risk in young and middle-aged adults with type 1 diabetes mellitus: a systematic review and meta-analysis. Clin Endocrinol. 2018;89(3):314–323.
6. Wang H, Ba Y, Xing Q, Du JL. Diabetes mellitus and the risk of fractures at specific sites: a meta-analysis. BMJ Open. 2019;9(1):e024067.
7. Sato M, Ye W, Sugihara T, Isaka Y. Fracture risk and healthcare resource utilization and costs among osteoporosis patients with type 2 diabetes mellitus and without diabetes mellitus in Japan: retrospective analysis of a hospital claims database. BMC Musculoskelet Disord. 2016;17(1):489.
8. Heilmeier U, Hackl M, Schroeder F, et al. Circulating serum microRNAs including senescent miR-31-5p are associated with incident fragility fractures in older postmenopausal women with type 2 diabetes mellitus. Bone. 2022;158:116308.
9. Kara Z, Güneş M, Bolayırlı İM, et al. The effects of diabetic polyneuropathy and autonomic neuropathy on bone turnover. Metab Syndr Relat Disord. 2022;20:11–19.
10. Zhang Z, Jin X, Xia W. Key points of diagnosis and treatment guidelines for primary osteoporosis (2017 Edition). Chin J Osteopor Bone Mineral Res. 2017;5:8.
11. Jawhar DS, Hassan NA, Shamssain MH. Dual-energy x-ray absorptiometry scan (DXA) findings in diabetic and non-diabetic female: a retrospective cohort study. Med J Malaysia. 2020;75(1):47–51.
12. Si Y, Wang C, Guo Y, Xu G, Ma Y. Prevalence of osteoporosis in patients with type 2 diabetes mellitus in the Chinese mainland: a systematic review and meta-analysis. Iran J Public Health. 2019;48(7):1203–1214.
13. Palermo A, Tuccinardi D, Defeudis G, et al. BMI and BMD: the Potential Interplay between Obesity and Bone Fragility. Int J Environ Res Public Health. 2016;13(6):544.
14. Chen P, Li Z, Hu Y. Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health. 2016;16(1):1039.
15. Tian L, Yang R, Wei L, et al. Prevalence of osteoporosis and related lifestyle and metabolic factors of postmenopausal women and elderly men: a cross-sectional study in Gansu province, Northwestern of China. Medicine. 2017;96(43):e8294.
16. Cui L, Chen L, Xia W, et al. Vertebral fracture in postmenopausal Chinese women: a population-based study. Osteoporos Int. 2017;28(9):2583–2590.
17. Jepsen KJ, Schlecht SH. Biomechanical mechanisms: resolving the apparent conundrum of why individuals with type II diabetes show increased fracture incidence despite having normal BMD. J Bone Miner Res. 2014;29(4):784–786.
18. Groenendijk I, Chan R, Woo J, et al. A combined nutrition and exercise intervention influences serum vitamin B-12 and 25-hydroxyvitamin D and bone turnover of healthy Chinese middle-aged and older adults. J Nutr. 2020;150(8):2112–2119.
19. Fu Y, Xu Y, Chen S, Ouyang Y, Sun G. MiR-151a-3p promotes postmenopausal osteoporosis by targeting SOCS5 and activating JAK2/STAT3 signaling. Rejuvenation Res. 2020;23(4):313–323.
20. He Y, Chen D, Guo Q, Shi P, You C, Feng Y. MicroRNA-151a-3p functions in the regulation of osteoclast differentiation: significance to postmenopausal osteoporosis. Clin Interv Aging. 2021;16:1357–1366.
21. Conway BN, Long DM, Figaro MK, May ME. Glycemic control and fracture risk in elderly patients with diabetes. Diabetes Res Clin Pract. 2016;115:47–53.
22. Maycas M, Portolés MT, Matesanz MC, et al. High glucose alters the secretome of mechanically stimulated osteocyte-like cells affecting osteoclast precursor recruitment and differentiation. J Cell Physiol. 2017;232(12):3611–3621.
23. Głogowska-Szeląg J, Kos-Kudła B, Marek B, Nowak M, Siemińska L. Assessment of selected adipocytokines in obese women with postmenopausal osteoporosis. Endokrynol Pol. 2019;70(6):478–483.
24. Johansson H, Kanis JA, Odén A, et al. A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res. 2014;29(1):223–233.
25. Ahmed LA, Schirmer H, Berntsen GK, Fønnebø V, Joakimsen RM. Features of the metabolic syndrome and the risk of non-vertebral fractures: the Tromsø study. Osteoporos Int. 2006;17(3):426–432.
26. Zhao H, Li Y, Zhang M, Qi L, Tang Y. Blood lipid levels in patients with osteopenia and osteoporosis: asystematic review and meta-analysis. J Bone Miner Metab. 2021;39(3):510–520.
27. Kha HT, Basseri B, Shouhed D, et al. Oxysterols regulate differentiation of mesenchymal stem cells: pro-bone and anti-fat. J Bone Miner Res. 2004;19(5):830–840.
28. Avogaro A, Fadini GP. Microvascular complications in diabetes: a growing concern for cardiologists. Int J Cardiol. 2019;15(291):29–35.
29. Shanbhogue VV, Hansen S, Frost M, et al. Compromised cortical bone compartment in type 2 diabetes mellitus patients with microvascular disease. Eur J Endocrinol. 2016;174(2):115–124.
30. Chen H, Liu W, Wu X, Gou M, Shen J, Wang H. Advanced glycation end products induced IL-6 and VEGF-A production and apoptosis in osteocyte-like MLO-Y4 cells by activating RAGE and ERK1/2, P38 and STAT3 signalling pathways. Int Immunopharmacol. 2017;52:143–149.
31. Sanguineti R, Puddu A, Mach F, Montecucco F, Viviani GL. Advanced glycation end products play adverse proinflammatory activities in osteoporosis. Mediators Inflamm. 2014;2014:975872.
32. Beeve AT, Brazill JM, Scheller EL. Peripheral neuropathy as a component of skeletal disease in diabetes. Curr Osteoporos Rep. 2019;17(5):256–269.
33. Kluding PM, Bareiss SK, Hastings M, Marcus RL, Sinacore DR, Mueller MJ. Physical training and activity in people with diabetic peripheral neuropathy: paradigm shift. Phys Ther. 2017;97(1):31–43.
34. Börekci E, Kara A, Kılıç M, et al. The increase of neuropathic symptoms in diabetic patients is related with osteopenia. Neurol Sci. 2021;42(7):2873–2880.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
