Back to Journals » Patient Preference and Adherence » Volume 15
Prevalence and Influencing Factors of Medical Dissatisfaction Experiences in Chinese Hospitals: A Cross-Sectional Study
Authors Lv H, Wang J , Xing X, Ren W
Received 13 November 2020
Accepted for publication 22 January 2021
Published 3 March 2021 Volume 2021:15 Pages 523—532
DOI https://doi.org/10.2147/PPA.S290651
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Naifeng Liu
Hui Lv,1,2 Jingjing Wang,3 Xiaolin Xing,3 Wenjie Ren1
1Institutes of Health Central Plains, Xinxiang Medical University, Xinxiang, 453000, People’s Republic of China; 2Management Institute, Xinxiang Medical University, Xinxiang, 453000, People’s Republic of China; 3School of Public Health, Xinxiang Medical University, Xinxiang, 453000, People’s Republic of China
Correspondence: Wenjie Ren Email [email protected]
Purpose: To explore the influencing factors of medical dissatisfaction experiences from the perspectives of patients, and provide corresponding strategies for its prevention.
Patients and Methods: Using multistage random sampling, 43 hospitals in three provinces of China were surveyed using a self-designed questionnaire. There were 2065 valid questionnaires analyzed in our study.
Results: 46.9% (n = 934) of participants had experienced medical dissatisfaction in the past year, mainly due to poor service quality, cumbersome procedures and high medical costs. There were statistically significant differences in the medical dissatisfaction experiences for these patients with different ages, marital status and levels of education (P< 0.05). According to structural equation modelling, health education and media reports had a positive and indirect influence (standardized coefficient = 0.046) on medical dissatisfaction experiences, while there was a negative correlation (standardized coefficient = − 0.399) between patients’ social recognition and medical dissatisfaction experiences. Also, our results also found that social relationships had a negative and indirect impact (standardized coefficient = − 0.166) on medical dissatisfaction experiences. Besides, health education and media reports had a negative impact (standardized coefficient = − 0.115) on patients’ social recognition, while social relationships have a positive effect (standardized coefficient = 0.416) on patients’ social recognition.
Conclusion: Health education and media reports and social relationships, as antecedent variables, have an indirect effect on inducing the medical dissatisfaction experiences of patients. In addition, patients’ social recognition was an intermediate variable in inducing the medical dissatisfaction of patients.
Keywords: social cognition, health care workers, HCWs, mistrust, patients satisfaction
Introduction
There is increasing incidence of aggressive behavior by patients against health care workers (HCWs) in many countries,1,2 especially in China,3–5 which is considered to be an occupational hazard.3 It is not considered an accidental event but to be caused by a combination of various factors, such as failed doctor-patient relationships (DPR),6 a low-level of risk perception,7 flawed medical systems, patients’ increasing mistrust of hospitals and physicians,8 dissatisfaction with staff attitude,2 and media orientation.9 Several researches have pointed out there is a direct relationship between the violence and the patients’ medical experience.10,11 Recent research has discovered that those who had ever had an unpleasant experience expressed the highest degree of mistrusting HCWs8 and were more likely to initiate defensive medical practices,12 resulting in doctor-patient conflict, even violence.12 Therefore, it is necessary to study the influencing factors leading to patients’ dissatisfaction so as to provide intervention strategies to prevent violence.
The media plays an important role in communicating information about health and health services.13 Biased and unfavorable media reporting could contribute to deteriorating DPR especially when patients may have a negative experience within the healthcare system.3,9,13 Meanwhile, the reputation of the hospital in China is impaired, partly because of the sensationalized depiction of medical incidents and conflicts by the public media.12 In addition, the massive expansion of the media sector leads to an increase in health awareness among people, making them gain more medical knowledge in all kinds of ways.14,15 Literature has found that HCWs with poor communication skills negatively impact the relationship in situations where patients do have healthcare information they bring with them to the visit, which may lead to a dissatisfied medical experience.14 An existing study has mentioned that those patients with higher educational attainment were considered to have low trust.16
Social relationships (SR) are universal predictors of the mental and physical health of adults,17 which includes family relationship, degree of social support and social status cognition in the present study. Although a previous study has indicated HCWs should realize the subjectivity of the patients (ie, family relationship, emotions) instead of just focusing on their disease.18 Similarly, what characteristics of the patients (ie, emotional intelligence, self-confidence and personality traits) influence patients’ ratings of the relationships with the doctor.19 Besides, related studies have manifested that poor social relationships may result in emotion problems,20 while doctors’ respect to patients could relieve their anxious emotions,21 which may be regarded as a friendly signal to express their respect and concern to their patients. However, there have rarely been investigations involving the correlation between patients’ social relationships and their evaluation of HCWs and medical systems.
Social cognition refers to the cognitive processes involved in how individuals think about other people, social situations and interactions, which also mean the perception, interpretation and processing of social information.21 Similarly, patients’ social cognition (PSC) mainly involves how patients evaluate the HCWs, the DPR and medical systems. There are two aspects to reflect PSC, including cognition for the HCWs and hospitals and industry, which play an important intermediate role in the process of a patient's experiences. Enhancing patients’ cognitive and emotional reactions can be a great way to gain their trust,19 then, to improve their medical experience. In this paper, the aim of our study is to build the theoretical model of medical dissatisfaction experience to verify the correlation among variables.
Patients and Methods
Sampling and Setting
A cross-sectional study with multistage random sampling was used in our study. First, hospitals were selected in three different provinces (Shandong, Henan and Guizhou) as sample provinces, which stood for eastern, central and western regions of China. Second, according to the level of economic development, there were two prefecture-level cities being selected in each province, then randomly selecting 3 tertiary hospitals, 2 county-level hospitals and 2 town-level hospitals (1 community health service center and 1 town and township hospital) in each prefecture-level city. There were 50 outpatients and inpatients randomly selected in each tertiary or county-level hospital, and 30 outpatients and inpatients were randomly selected in each town-level hospital. Besides this, all surveyors were divided into three teams to set out for the corresponding provinces to carry out the survey, and there was a related lead teacher to manage the investigators in each team and deal with possible problems in the process of our survey.
Measurements
The dimensions of the initial questionnaire were formed based on social cognitive theory,21 the relevant literature and group discussion. Then there were five professors, including three health management and health systems experts and two public health experts, being consulted to revise the questions for content validity and suitability for use in China. Cronbach’s α coefficient refers to the consistency between the scores of various items in the scale, reflecting whether it is consistent or not.22 After analyzing the data, its result indicates that the Cronbach’s alpha is 0.73, which meets the acceptable standard of more than 0.6 recommended by Chang.23
According to the factor analysis, varimax rotation was used to extract four factors. The validity of data was analyzed by Kaiser-Meyer-Olkin (KMO) = 0.845, which was more than 0.8. The value of Chi-square was 7869.227, and the significant P-value was less than 0.001. These indexes reflect the fact that it is suitable for factor analysis. In addition, the total variance explained rate of four extracted factors was 62.90%, representing most of the information from the items. Meanwhile, social relationships, health education and media reports were regarded as antecedent variables in inducing medical dissatisfaction experiences, which was represented by X1-X5. Patients’ social cognition, covering patients’ cognition on health care workers (PCHCWs) and patients’ cognition on hospitals and Industry (PCHI), was considered as a mediating variable in inducing medical dissatisfaction experiences, which was displayed by Y1-Y8. All of these items can be seen in Table 1.
 |
Table 1 The Classification of Influencing Factors of Medical Dissatisfaction Experiences |
In addition, medical dissatisfaction experiences (MDE) are described in frequency of medical dissatisfaction experiences (FMDE), which was used as a single item of evaluation by asking the patients “Have you ever been dissatisfied with hospitals or hospital staff in your medical experience in the last year?” with five choices: (1) Almost never, (2) Seldom, (3) Generally, (4) Often, (5) Almost always. As well as asking for patients’ sociodemographic information, including sex (1 = Male, 2 = Female), age (1 = less than 30 to 5 = 60 or more), marital status (1 = Never married, 2 = Married, 3 = Divorced, 4 = Widowed), level of education (1 = Primary school to 5 = Bachelor or more), job types (1 = farmer, 2 = civil servant to 8 = others), and income (1 = Very low to 5 = Very high).
Data Collection
For the inpatients, they had stayed in hospital for more than three days and were able to respond to the survey, the outpatients must have been treated and agreed to participate in the waiting room. The trained surveyors provided the questionnaires to these patients. Only patients were included in our study if they consented to participate and had finished filling out the questionnaires. After finishing the investigation, patients would receive a small gift as gratitude for their cooperation. Data was entered by using Epidata software, which was exported into Excel form. There were 43 Chinese hospitals participating in this study between 1 July 2018 and 25 August 2018. After deleting the missing data from the survey responses there were 2065 valid questionnaires being analyzed in our study.
Statistical Analysis
SPSS statistic (IBM) version 24.0 was used for descriptive analysis and factor analysis. Analysis of Moment Structure (AMOS) version 22.0 was used for the Structural Equation (SEM), which mainly refers to test the relationships between different constructs. There are four variables in the SEM, which are named the exogenous variables and endogenous variables, the latent variables (unobserved variables) and manifest variables (observed variables). The latent variables were labeled in the ellipse, while the manifest variables will be labeled in the rectangle in SEM graphs. This study also used several indices, including goodness of fit index (GFI > 0.9), adjusted goodness of fit index (AGFI > 0.8), normal fit index (NFI > 0.9) and root mean square of standardized residual (RMSR < 0.08) to evaluate overall model fitness. Descriptive statistics, including frequency distribution and percentages were made for some variables. Structural Equation Modeling was used to verify the theoretical model.
Ethical Considerations
The study was approved by the Ethical Review Board of Xinxiang Medical University (XYLL-2018191), Xinxiang, China, and was in accordance with the World Medical Association of Helsinki. Our study also received oral permission from the directors of all the health care settings. Data was collected in anonymous form. By using the written consent form made by ourselves, we would interpret the above contents in detail to each participant before starting the investigation. Then if we gained their consent, we would start our investigation. The written consent form was also approved by the Ethical Review Board of Xinxiang Medical University.
Results
Difference of Medical Dissatisfaction Experiences of Patients on Demographic Characteristics
There were 2065 valid questionnaires being analyzed in our study. All of the participant's demographic information is shown in Table 2 in detail. About 49.5% (n = 1023) were male, and 50.5% (n = 1042) were female. The average age of participants was 42.9 years (SD = 16.834; Range = 18–90 years). Among participants, those who had married reported the highest frequency (80.5%, n = 1662), followed by those who had never married (16.2%, n = 335). With regard to education, the most common education level was junior high school (26.2%, n = 542), and only 14.9% (n = 307) had ended in primary school or below.
 |
Table 2 Difference of Medical Dissatisfaction Experiences of Patients on Demographic Characteristics |
According to the nonparametric test, we have found that there were statistically significant differences in the medical dissatisfaction experiences for these patients with different age, marital status and level of education (P<0.05). In addition, the distribution of demographic data in terms of the state of being exposed to medical dissatisfaction experiences is shown in Table 2.
Medical Dissatisfaction Experiences
Our results indicate that 46.9% (n=934) of participants experienced medical dissatisfaction, among which 24.9% (n=506) had occasionally experienced medical dissatisfaction in the past year. About 6.8% (n=139) and 1.3% (n=27) of participants had often or frequently experienced medical dissatisfaction, respectively (Figure 1). There were nine reasons for medical dissatisfaction experiences in Figure 1, among which the highest frequency was for poor service attitude, followed by cumbersome procedures, high medical bills and long waiting time. Inferior equipment condition was the lowest reason for medical dissatisfaction (Figure 2).
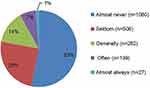 |
Figure 1 Frequency of medical dissatisfaction experiences. |
 |
Figure 2 Reasons for medical dissatisfaction experiences. |
The Structural Equation Modelling Analysis
Model Fitness Indices
AMOS statistical analysis software was used to test the conceptual model, and the goodness-of-fit indicators and all path coefficients are presented in Figure 1.The results indicated that all path coefficients reached statistical significance. In addition, the chi-square value was 474.415, and the degree of freedom was 72, and P value was 0.000. According to the goodness-of-fit indicators, CFI = 0.952 (>0.90 is good); GFI = 0.968 (>0.90 is good); AGFI = 0.953 (>0.90 is good); TLI = 0.939 (>0.90 is good); and RMSEA = 0.052 (<0.08 is reasonable, <0.10 is acceptable), all of which have meant that the model we built can be accepted as a whole.
Relationship Among HEMR, SR, PSC and MDE
The relationships among HEMR, SR, PSC and MDE are presented in Figure 3 and Table 3. Health education and media reports (HEMR) and its indicators were shown to exert both direct and indirect effects on medical dissatisfaction experiences (MDE), which were 0.250 and 0.046, respectively. Moreover, patients’ social cognition (PSC) had a negative impact on MDE, which was −0.399 for the standardized direct effect. Also, a negative and indirect effect of social relationships (SR) on medical dissatisfaction experiences (MDE) was found in the SEM, which was −0.166 for the standardized indirect effect. In addition, HEMR was shown to affect PSC negatively (standardized direct effect = −0.115), while SR had a positive and direct influence on PSC (standardized direct effect = 0.416).
 |
Table 3 Standardized Effects Between SR, HEMR, PSC and MDE |
Discussion
In this study, our result has shown that 46.9% (n=954) of participants experienced medical dissatisfaction, among which 6.8% (n=141) and 1.3% (n=27) of participants had often or frequently experienced medical dissatisfaction in the past year, respectively. A study conducted in China testified that patients who are younger and with higher educational attainment are prone to be less satisfied with their physicians.6 Similarly, the results of this study also display that patients with these characteristics are more likely to have medical dissatisfaction experiences. Besides this, our findings also concluded the reasons which brought about the dissatisfaction, among which the top three were poor service quality, cumbersome procedures and high medical costs, respectively. This is different from the finding of an existing study that the long waiting time was the first reason for causing medical dissatisfaction.24 Meanwhile, many researches have also indicated that service quality and medical costs were still important factors affecting medical experiences,12,20 which were consistent with our study.
Health education and media reports (HEMR) had a positive effect on medical dissatisfaction experiences (MDE) in the SEM, implying that the more patients get media reports involving medical behaviors and DPR, the worse their perception of the HCWs, hospitals and industry will be, probably leading to MDE. Several previous studies have also indicated the similar conclusion that the more the public comes to understand the doctor–patient relationship (DPR) then the more it can be influenced by media coverage of relevant news,25 and especially those adverse news reports without in-depth analysis which can deteriorate the public perception of the DPR,26 reflecting that patient cognition can be effected by media orientation.27,28 Also, a study related to public perception on healthcare services in China has found that 47.4% provided negative feedback for healthcare services in social media platforms, having the highest proportion of negative contents (74.9%) in the DPR category.29 In the present study, we got a finding that media reports can be an antecedent variable in inducing medical experiences, leading to generating a vicious circle between negative patients’ social cognition and medical dissatisfaction, continually worsening DPR. Therefore, relevant departments should launch some management measures to regulate media reports, making sure to provide clear, unbiased and educational messages to the public13 to increase positive public opinion.25 It is essential to establish disciplinary mechanisms to punish those who report unreal information to achieve standardized management.
The convenience brought by the information age makes it more convenient for people to get the health knowledge they need to make judgments and take decisions in everyday life in terms of healthcare.30 It has found that health education negatively associates with patients’ social cognition in this study. Such a result has been due to several reasons, such as the lack of reliability or accuracy of some online information,14 high expectation for HCWs,20 and negative feedback.29 On the one hand, patients’ lack of medical knowledge31 may be eager to gain more related knowledge through media sources.32 But mistrust would appear between patients and HCWs when this information was inconsistent with what the physicians delivered, reflecting asymmetric information may lower their trust in doctors.31 On the other hand, those gaining more health knowledge tend to have higher education levels, and they are more likely to know about more questions of medical systems so as to lead to negative cognition on hospitals and the industry. In the training for HCWs, it should attach importance to improve communication skills and cultivate their empathy to transfer patients’ negative cognition. Holding more health education lectures in the community to spread the knowledge of common diseases and frequently-occurring diseases by the explanation of clinical experts to eliminate patients’ misunderstanding.
Social cognition reflected domains of emotion and social perception.11 As for patients’ social cognition (PSC), it means how patients assess their opinions on HCWs, hospital and industry in this study. We made an important finding in the present study that patients’ negative cognition on HCWs can lead to patients having more frequent medical dissatisfaction experiences. Similarly, previous studies have found that patient perceptions of injustice within the healthcare system can have an impact on medical experiences.33 Indeed, excessive emphasis on the tension of DPR has been increasing the antagonism of patients towards doctors,25 resulting in unpleasant medical experiences and even conflicts or violence.
On the contrary, trust in physicians has been found to positively affect the patient experience,14 which is in line with our study. Patients may feel more satisfied with their medical experience when they have received care conforming to their specific needs and values.34 Others have shown that patients are likely to trust HCWs when they feel respected and perceive medical staff as attentive and honest,7 which is helpful to relieve the patients’ anxiety due to bad treatment outcomes. Although there is uncertainty and high risk in medical treatment, patients believe they will have a good clinical outcome once admitted to the hospital, regardless of the severity of the disease.9 As a result, the risk of medical dissatisfaction will be increased if there is a bad medical outcome. Besides, public hospitals with insufficient financial support from the state are lead to run like private hospitals and treat patients as medical consumers,8 making them probably over-supply unnecessary medical services to increase financial revenue, which deepens patients’ negative impressions of hospitals and the industry and leading to medical dissatisfaction. Therefore, it is essential to rebuild a trusting DPR from the bottom up to solve the problem of patient dissatisfaction with medical staff.11,15 Related research has shown that trust in medical providers and the healthcare system may motivate patients to utilize health information, which may subsequently improve patients’ health behavior.35
Social relationships refer to the social network of the patient, which includes family relationships, social support and social status cognition in this study. The present study has confirmed the finding that social relationships had an indirect effect (though PSC) on medical dissatisfaction experiences (MDE), implying that patients with negative social relationships would be more likely to represent negative social cognition to lead to medical dissatisfaction. One of the most important reasons is that most HCWs pay more attention to identifying patients’ disease information than their background information (eg, social relationships) so that they probably ignore providing the humanistic care with those patients leading to negative SR in the process of medical practices, which worsens patients’ impression on HCWs to lead to more dissatisfied experiences even conflict. Therefore, it is essential to attach importance to identifying patients’ information, such as family relationship and social support, making sure to accurately acquire their personality characteristics, and providing personalized services to patients with different needs to improve their medical experience. Meanwhile, hospitals should strengthen the training of humanistic knowledge to promote the harmonious doctor-patient interaction and enhance the doctor-patient relationship.
Conclusion
The analysis leads to the following conclusions. Firstly, there was generally a high frequency of medical dissatisfaction, mainly due to poor service quality, cumbersome procedures and high medical costs. Secondly, health education and media reports (HEMR) have a negative effect on patients’ social recognition, implying that it is an antecedent variable in inducing medical dissatisfaction. Therefore, it is necessary to regulate media reports by rebuilding the admittance threshold of reporting medical-related events for the media practitioners. Thirdly, social relationships had an indirect effect (though PSC) on medical dissatisfaction experiences (MDE), suggesting that health care workers should know about the background information of patients so that they can provide personalized service to decrease patients’ medical dissatisfaction. Also, these findings provide a reference for further research on the mechanism of medical dissatisfaction of patients.
Acknowledgments
The authors would like to acknowledge the time and efforts that participants have given to this survey. This study was funded by the National Natural Science Foundation of China (71503226); and the Postgraduate Research Innovation Support Program of Xinxiang Medical University (YJSCX201928Z).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Singh M. Communication as a bridge to build a sound doctor-patient/parent relationship. Indian J Pediatr. 2016;83(1):33–37. doi:10.1007/s12098-015-1853-9
2. Cai R, Tang J, Deng C, et al. Violence against health care workers in China, 2013–2016: evidence from the national judgment documents. Hum Resour Health. 2019;17(1):103. doi:10.1186/s12960-019-0440-y
3. Du Y, Wang W, Washburn DJ, et al. Violence against healthcare workers and other serious responses to medical disputes in China: surveys of patients at 12 public hospitals. BMC Health Serv Res. 2020;20(1):253. doi:10.1186/s12913-020-05104-w
4. Jiao M, Ning N, Li Y, Gao L, Hao Y. Workplace violence against nurses in Chinese hospitals: a cross-sectional survey. BMJ Open. 2015;5(3):e006719. doi:10.1136/bmjopen-2014-006719
5. Zhao S, Qu L, Liu H, et al. Coping with workplace violence against general practitioners and nurses in Heilongjiang Province, China: social supports and prevention strategies. PLoS One. 2016;11(6):e0157897. doi:10.1371/journal.pone.0157897
6. Wang W, Zhang H, Washburn DJ, et al. Factors influencing trust towards physicians among patients from 12 hospitals in China. Am J Health Behav. 2018;42(6):19–30. doi:10.5993/AJHB.42.6.3
7. Wei D, Xu A, Wu X. The mediating effect of trust on the relationship between doctor-patient communication and patients’ risk perception during treatment. Psych J. 2020;9(3):383–391. doi:10.1002/pchj.327
8. Chan CS-C. Mistrust of physicians in China: society, institution, and interaction as root causes. Dev World Bioeth. 2018;18(1):16–25. doi:10.1111/dewb.12162
9. Lancet T, Anon. Chinese doctors are under threat. Lancet. 2010;376(9742):657. doi:10.1016/S0140-6736(10)61315-3
10. Zhou C, Mou H, Xu W, et al. Study on factors inducing workplace violence in Chinese hospitals based on the broken window theory: a cross-sectional study. BMJ Open. 2017;7(7):e016290. doi:10.1136/bmjopen-2017-016290
11. Xiong NN, Wei J, Fritzsche K, et al. Psychological and somatic distress in Chinese outpatients at general hospitals: a cross-sectional study. Ann Gen Psychiatry. 2017;16(35). doi:10.1186/s12991-017-0158-y.
12. Ding D, Li Y, Ding D. Patient satisfaction with hospital inpatient care: effects of trust, medical insurance and perceived quality of care. PLoS One. 2016;11(10):e0164366. doi:10.1371/journal.pone.0164366
13. Hoyle LP, Kyle RG, Mahoney C. Nurses’ views on the impact of mass media on the public perception of nursing and nurse-service user interactions. J Res Nurs. 2017;22(8):586–596. doi:10.1177/1744987117736363
14. Hoff T, Collinson GE. How do we talk about the physician-patient relationship? What the nonempirical literature tells us. Med Care Res Rev. 2017;74(3):251–285. doi:10.1177/1077558716646685
15. Shrivastava SR, Shrivastava PS, Ramasamy J. Exploring the dimensions of doctor-patient relationship in clinical practice in hospital settings. Int J Health Policy Manag. 2014;2(4):159–160. doi:10.15171/ijhpm.2014.40
16. Zhao D, Zhang Z. Changes in public trust in physicians: empirical evidence from China. Front Med. 2018;13(4):504–510. doi:10.1007/s11684-018-0666-4
17. McCauley JB, Pickles A, Huerta M, Lord C. Defining positive outcomes in more and less cognitively able autistic adults. Autism Res. 2020;1–13.
18. Zhou P, Grady SC. Three modes of power operation: understanding doctor-patient conflicts in China’s hospital therapeutic landscapes. Health Place. 2016;42:137–147. doi:10.1016/j.healthplace.2016.09.005
19. Petrocchi S, Iannello P, Lecciso F, et al. Interpersonal trust in doctor-patient relation: evidence from dyadic analysis and association with quality of dyadic communication. Soc Sci Med. 2019;235:112391. doi:10.1016/j.socscimed.2019.112391
20. Chang CS, Chen SY, Lan YT. Service quality, trust, and patient satisfaction in interpersonal-based medical service encounters. BMC Health Serv Res. 2013;13(1):22. doi:10.1186/1472-6963-13-22
21. Addington J, Girard TA, Christensen BK, et al. Social cognition mediates illness-related and cognitive influences on social function in patients with schizophrenia-spectrum disorders. J Psychiatry Neurosci. 2010;35(1):49–54. doi:10.1503/jpn.080039
22. Yang T, Wu Y. A study on the influence of patient participation on patient trust-based on sample survey in China. Front Psychol. 2018;9:2189. doi:10.3389/fpsyg.2018.02189
23. Chang CS, Chang HC. Perceptions of internal marketing and organizational commitment by nurses. J Adv Nurs. 2010;65(1):92–100. doi:10.1111/j.1365-2648.2008.04844.x
24. Fafliora E, Bampalis VG, Zarlas G, et al. Workplace violence against nurses in three different Greek healthcare settings. Work. 2016;53(3):551–560. doi:10.3233/WOR-152225
25. Sun J, Liu S, Liu Q, et al. Impact of adverse media reporting on public perceptions of the doctor-patient relationship in China: an analysis with propensity score matching method. BMJ Open. 2018;8(8):e022455. doi:10.1136/bmjopen-2018-022455
26. Sun J, Liu S, Liu Q, et al. Impact of physician-doctor relationship media report on clinical medical students. Chin Med Ethics. 2016;29:864–867.
27. Gao HD, Chen H, Feng J. Balanced scorecard-based performance evaluation of Chinese county hospitals in underdeveloped areas. J Int Med Res. 2018;46(5):1947–1962. doi:10.1177/0300060518757606
28. Bustamante S. CSR,trust and the employer brand. Working Papers. 2018.
29. Guangyu H, Han X, Zhou H, et al. Public perception on healthcare services: evidence from social media platforms in China. Int J Environ Res Public Health. 2019;16(7):1273. doi:10.3390/ijerph16071273
30. Samerski S. Health literacy as a social practice: social and empirical dimensions of knowledge on health and healthcare. Soc Sci Med. 2019;226:1–8. doi:10.1016/j.socscimed.2019.02.024
31. Xu Y, He W. More information = less aggression? Impact of information asymmetry on chinese patients’ aggression. Front Public Health. 2019;7:118. doi:10.3389/fpubh.2019.00118
32. Freidson E. The reorganization of the medical profession. Med Care Rev. 1985;42(1):11. doi:10.1177/107755878504200103
33. Yao M, Finnikin S, Cheng KK. Call for shared decision making in China: challenges and opportunities. Z Evid Fortbild Qual Gesundhwes. 2017;123–124:32–35. doi:10.1016/j.zefq.2017.05.004
34. Jiang S. Pathway linking patient-centered communication to emotional well-being: taking into account patient satisfaction and emotion management. J Health Commun. 2017;22(3):234–242. doi:10.1080/10810730.2016.1276986
35. Tsai TI, Yu WR, Lee SD. Is health literacy associated with greater medical care trust? Int J Qual Health Care. 2018;30(7):514–519. doi:10.1093/intqhc/mzy043
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

