Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Prevalence and Impact of Metabolic Syndrome on Short-Term Prognosis in Patients with Acute Coronary Syndrome: Prospective Cohort Study
Authors Fanta K , Daba FB , Asefa ET, Chelkeba L , Melaku T
Received 14 May 2021
Accepted for publication 24 June 2021
Published 15 July 2021 Volume 2021:14 Pages 3253—3262
DOI https://doi.org/10.2147/DMSO.S320203
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ming-Hui Zou
Korinan Fanta,1 Fekede Bekele Daba,1 Elsah Tegene Asefa,2 Legese Chelkeba,3 Tsegaye Melaku1
1Department of Clinical Pharmacy, Institute of Health, Jimma University, Jimma, Oromia, Ethiopia; 2Department of Internal Medicine, Institute of Health, Jimma University, Jimma, Oromia, Ethiopia; 3Department of Pharmacology and Clinical Pharmacy, College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Korinan Fanta
Department of Clinical Pharmacy, Institute of Health, Jimma University, P.O.Box: 378, Jimma, Ethiopia
Tel +251 911598485
Fax +251 476617980
Email [email protected]
Purpose: Despite the increasing burden of metabolic syndrome (MS) and ischemic heart disease in sub-Saharan Africa, data on the prevalence of MS among patients with acute coronary syndrome (ACS) from the regions are limited. Hence, this study is aimed to evaluate the prevalence and impact of MS on 30-day all-cause mortality in patients hospitalized with ACS.
Patients and Methods: We prospectively assessed 176 ACS patients, who were admitted to two tertiary hospitals in Ethiopia. MS was diagnosed based on a harmonized definition of MS. In-hospital major adverse cardiovascular events (MACE) and 30-day mortality were recorded. Multivariable cox-regression was used to identify predictors of 30-day mortality.
Results: Among 176 ACS patients enrolled, 62 (35.2%) had MS. Majority of the patients (62.5%) were male with the mean age of 56± 11.9 years. ACS patients with MS were older, presented with atypical symptoms, and they had history of hypertension, diabetes, dyslipidemia and coronary artery disease compared to those without MS. MS was also significantly associated with in-hospital MACE (30.6% vs 17.5%; p= 0.046) and 30-day mortality [adjusted hazard ratio (AHR) = 3.25, 95% CI=1.72– 6.15]. The other significant predictors of 30-day mortality were pre-hospital delay > 12h (HR= 4.32, 95% CI=1.68– 11.100), killip class ≥ 2 (HR=10.7, 95% CI= 2.54– 44.95), and ejection fraction < 40 (HR= 2.59 95% CI=1.39– 4.84).
Conclusion: The prevalence of MS among patients with ACS in Ethiopia is high. MS was significantly associated with high in-hospital MACE and it was an independent predictor of 30-day mortality. Initiating appropriate strategies on MS prevention and timely diagnosis of MS components could decrease the burden of ACS and improve patient’s outcome.
Keywords: metabolic syndrome, myocardial infarction, mortality, sub-Saharan Africa
Introduction
The metabolic syndrome (MS) represents a group of correlated metabolic disorders that have a synergic effect on atherosclerotic cardiovascular disease risk.1,2 According to the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III), MS is defined by the presence of any three of the following metabolic abnormalities: abdominal obesity, dyslipidemia, hypertension or treated hypertension, and elevated fasting plasma glucose levels.3
About one-quarter of the world population is currently affected by MS.4 Contrary to the prior thought, MS are no longer rare in sub-Saharan Africa (SSA). Recent meta-analysis of a community-based study reported that the overall prevalence of MS in SSA was 17.1% and 18% according to the NCEP/ATP III and international diabetes federation (IDF) diagnostic criteria, respectively.5 Furthermore, the burden of non-communicable disease in SSA regions is exceeding the global average.6 Historically, rheumatic heart disease from infections source has been the leading cause of cardiovascular disease, while other causes were comparatively rare.6,7 However, recent studies show that stroke and ischemic heart disease are the leading cause of cardiovascular disease burden in the regions.5,6,8 These findings reflect that MS, a common precursor of these cardiovascular diseases is common in the continent. However, data on the prevalence of MS among ischemic heart disease particularly, ACS patients in the region are limited and the available data on MS are mainly done in diabetic, HIV/AIDS and hypertensive patients.9
Many studies have shown that MS has a negative impact on the prognosis of patients who survived ACS.10–12 These studies were predominantly conducted in developed countries among ACS patients managed in different ways which undoubtedly influenced prognosis and the occurrence of new adverse outcomes among these patients. However, an association of MS with risk of cardiovascular disease and mortality outcomes varies according to race/ethnicity, geographical area, age, and access to medical care.13 Despite these pieces of evidences, data on the association between MS and the outcome of ACS patients from SSA is rare. Therefore, we evaluated the prevalence and impact of MS 30-day all-cause mortality among patients hospitalized with ACS managed medically in tertiary hospitals in Ethiopia.
Methods
Study Design and Study Population
A prospective cohort study was conducted at two tertiary hospitals in Ethiopia (Saint Peter’s Specialized Hospital and Jimma University Medical Center) from March 2018 to November 2018. In the present study, ACS was diagnosed according to the third universal definition of myocardial infarction.14 Consecutive patients with confirmed ACS diagnosis admitted to selected hospitals who fulfilled the following eligibility criteria were enrolled: (1) age ≥ 18 years; (2) willing to provide written or oral informed consent; (3) type I myocardial infarction. Patients who died before clinical assessment or anthropometric and biochemical measurements were excluded. Additionally, readmitted patients (if enrolled previously), and patients with initial ACS diagnosis changed were excluded from the present study (see Supplementary Figure 1). The study protocol was approved by Institutional Review Board (IRB) of Jimma University, the Institute of Health before initiating data collection with a reference number of IHRPGD/193/18.
Metabolic Syndrome Diagnosis and Scores
Metabolic syndrome was assessed based on the harmonized definition of MS outlined by the IDF Task Force on Epidemiology and Prevention, NHLBI, AHA, World Heart Federation, International Atherosclerosis Society, and International Association for the Study of Obesity15 and ethnic-based waist circumference as defined by IDF16 was used. According to this criterion patient with ACS were diagnosed to have MS if they have at least three of the following components: (1) Elevated waist circumference (≥ 94 cm for men or ≥ 80 cm for women); (2) elevated fasting plasma glucose (FPG) ≥100 mg/dl or on drug treatment for raised glucose; (3) elevated blood pressure ≥130/85 mmHg or on antihypertensive treatment for a patient with a history of hypertension (4) reduced high-density lipoprotein cholesterol (HDL-C) [< 40 mg/dL (1.03 mmol/L) in males and < 50 mg/dL (1.29 mmol/L) in females] or and (5) Raised triglycerides ≥ 150 mg/dL (1.7 mmol/L). We did not consider treatment with lipid-lowering drugs as a criterion for patients on lipid-lowering agents for the sole purpose of cardiovascular disease prevention.
Waist circumference was measured at the midway between the lower margin of the ribs and the upper margin of the iliac crest in a horizontal plane using plastic metric tape.16 Brachial blood pressure was measured twice by appropriate sized-cuffs in a sitting position and a mean of the two recordings was used in the analyses. Fasting venous blood sample was collected for biochemical measurement in the morning after 8–12 fasting overnight. Accordingly, fasting plasma glucose, high-density lipoprotein, triglyceride low-density lipoprotein, and total cholesterol were measured using Cobas® 6000 analyzer.
Data Collection
Data collection was undertaken by trained health professionals who interviewed the study participants using pre-tested structured questionnaires and examined using standardized instruments and methods. Data collectors also abstracted relevant information (presenting symptoms, clinical data at admissions, cardiovascular risk factors and treatment) from active patient’s medical records prospectively.
The primary end-points of the study were 30-day all-cause mortality and in-hospital MACE. The data on primary end-points were collected by checking medical documentation on a daily basis from admission to discharge or death prospectively. For patients who died during hospitalization, physician’s death summary notes were reviewed. For those who died after hospital discharge, telephone contact with family members or caregivers and a death certificate review was used to confirm death. The definitions of clinical endpoints used in the present study are available in (Supplementary Material)
Operational Definitions
Major adverse cardiovascular events (MACE): defined as a composite of in-hospital cardiovascular death, stroke, and non-fatal acute myocardial infarction (re-infarction).
Typical chest pain: defined as a retrosternal sensation of pain/discomfort (“angina”) radiating to either or both arm, neck, or jaw, which may be intermittent (usually lasting ≥10 minutes) or persistent. It might be accompanied by additional symptoms such as nausea, abdominal pain, sweating, and syncope.
Atypical presentation: was defined as a non-classic symptoms, including epigastric pain, indigestion-like symptoms, stabbing or pleuritic pain, and isolated dyspnea in the absence of typical chest pain.
Statistical Analysis
Data were entered into Epidata version 4.2 and analyzed using statistical package for social science, version 23 (IBM, Armonk, NY, USA). Categorical variables were presented as proportion and compared between ACS with and without MS using the chi-square test. Continuous variables were presented as mean ± standard deviation when normally distributed and median (interquartile range) when skewed. Continuous variables were compared using the Student’s t-test or Mann–Whitney test as appropriate. The 30-day mortality rate among ACS patients with and without MS was compared by using Kaplan–Meier survival curve and Log rank test. Cox regression was used to identify independent predictors of time to 30-day mortality. P-value <0.25 was used as a cutoff point to select candidate variables on binary cox-regression. Multivariable cox-regression with backward step-wise methods was used to identify the independent predictors of 30-day mortality of ACS patients. Two-tailed p-values < 0.05 were considered as a statistically significant difference.
Results
Baseline Clinical Characteristics and Metabolic Syndrome Components
Among 176 ACS patients studied, 62 (35.2%) had MS. Patients with MS were older (58.5±11.0 vs 54.6±12.2, p= 0.035) compared to those without MS. Similarly, ACS patients with MS were more likely to have a prior history of hypertension, diabetes, dyslipidemia, chronic kidney disease, and coronary artery disease (p=0.001). Overall, there was no a statistically significant difference between ACS patients with MS and those without MS regarding sex, residence, and behavioral measures such as smoking and alcohol use (Table 1). The most common components of MS identified were abdominal obesity (46%) and a history of hypertension or blood pressure >130/85 mmHg (45.5%) (Figure 1).
 |
Table 1 Demographics and Baseline Characteristics in Patients with and without MS Presented with ACS |
 |
Figure 1 |
Clinical Presentation, Biochemical Data and Key Diagnostics
Patients with MS were more likely to present with atypical symptoms (p=0.026) and high admission systolic blood pressure (p= 0.007) compared to those without MS. Likewise, patients with MS were also present with high admission fasting plasma glucose, triglyceride, low-density lipoprotein cholesterol, and total cholesterol compared to those without MS (p-value <0.001). There was no significant difference between ACS patients with MS and without MS in ACS subtypes and other clinical findings (Table 2).
 |
Table 2 Clinical Presentation, Laboratory Measures, and Key Diagnostics in Patients with ACS, Stratified According to Presence or Absence of MS |
Treatment and In-Hospital Outcomes
Overall, aspirin, dual antiplatelet (aspirin and clopidogrel), and statins were used in more than 90% of ACS patients. Patients with MS were more likely to receive dual antiplatelet therapy compared to those without MS (p=0.015). The use of beta-blockers, ACEI/ARB, and any heparin was sub-optimal (70–80%), and no significant difference between the two groups (Table 3). Patients with MS were more likely to develop MACE during their hospital stay (p=0.026). In particular, patients with MS were more likely to develop heart failure (p=0.017) and cardiogenic shock (p=0.015) compared to those without MS. However, there was no difference regarding cardiovascular death, non-fatal stroke and re-infarction between the two groups (Table 3). Discharge medications follow similar patterns to in-hospital medications and comparable between both groups (Table 3).
 |
Table 3 Managements and In-Hospital Complications in Patients Presented with ACS with and without MS |
Predictors of 30-Day Mortality
From the total the total of 176 ACS patients, 46 (26.1%) patients were died during the 30-day follow-up. Twelve variables (age, residence, pre-hospital delay, presentation symptoms, systolic blood pressure, heart rate, serum creatinine, hemoglobin, Killip class, ACS subtypes, MS, and ejection fraction) with p-value <0.25 on bivariate cox-regression were included in the final model of multivariable cox-regression. On multivariable Cox proportional hazard model analysis, pre-hospital delay >12h, systolic blood pressure, Killip class ≥2, presence of MS, and low ejection fraction were significantly associated with 30-day mortality (Table 4).
 |
Table 4 Predictors of 30-Day Mortality in Patients Presented with ACS |
In this study patients who were presented to hospital after 12 h of symptom onset were about four times more likely to have 30-day mortality compared to those presented within 12 h of symptom onset [hazard ratio (HR)=4.32 95% confidence interval (CI)=1.68–11.10]. Patients presented with killip class ≥2 had about 11-fold increased hazard of 30-day mortality compared to those patients presented with Killip class 1(HR=10.7, 95% CI= 2.54–44.95). Similarly, ACS patients with MS were about 3 times more likely to have 30-day mortality than ACS patients without MS (HR =3.25, 95% CI = 1.72–6.15). Likewise, patient who had low ejection fraction (<40%) had three-fold increase in 30-day mortality compared to those who had preserved ejection fraction (HR= 2.59 95% CI= 1.39–4.84). High admission systolic blood pressure was associated with good prognosis (HR = 0.98, 95% CI= 0.96–0.99) (Table 4). Kaplan Meier cumulative 30-day survival curve was compared between ACS patients with MS and without MS using Log rank test (p=0.004) (Figure 2).
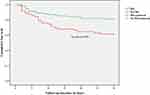 |
Figure 2 Kaplan Meier survival analysis of ACS patients with MetS and without MetS. |
Discussion
This study, the first in Ethiopia, showed a high prevalence of MS among patients with ACS. Overall, individuals with MS were more likely to be older, present with atypical symptoms, and have a history of hypertension, diabetes dyslipidemia, chronic kidney disease, and coronary artery disease before the index event. In the present study, MS is associated with in-hospital MACE and 30-day all-cause mortality. Even after adjusting for confounders, MS was still an independent predictor of 30-day all-cause mortality.
The prevalence of MS (35.2%) among the patients with ACS in the present study is significantly higher than 11–24% observed in general populations of sub-Saharan Africa.5 However, the prevalence of MS recorded in our study participants was low compared to previous studies done among patients with ACS from six Middle East countries that reported 46% of hospitalized ACS patients had MS.17 Likewise, a study conducted among ACS patients who received coronary intervention in China showed 46% of ACS patients had MS.18 Another study done by Cavalari et al19 indicated that more than half (62%) of ACS patients had MS. This difference might be due to differences in population-level risk factors, difference in MS diagnostic criteria used, and relatively low prevalence of MS in sub-Saharan Africa compared to other regions such as the Middle East and China.20,21
One of the major findings of the present study is that MS is significantly associated with in-hospital MACE. This finding is in line with the Analysis of the Gulf Registry of Acute Coronary Events (Gulf RACE), which demonstrated a significant association between MS and non-fatal MACE (heart failure and recurrent myocardial infarction).17 In addition, the report of a prior study done by Zeller et al22 showed a significant association between MS and severe in-hospital heart failure among patients hospitalized with acute myocardial infarction. Furthermore, the association between MS and MACE sustained even on long-term follow-up.18,19,23 This claim could be elucidated in view of the fact that inflammation caused by this syndrome plays a critical role in the process of atherosclerosis, which causes more severe coronary artery disease, restenosis and severe angiographic stenosis based on objective finding such as Syntax and modified Gensini.24,25
The other finding and most probably the main finding of this study is that MS is an independent predictor of 30-day mortality. A significant association between MS and a range of adverse cardiovascular events including mortality were noted in previous studies. Study conducted by Al-Rasadi et al26 which enrolled 1392 ACS patients, reported increased odds of in-hospital death among MS patients with ACS (OR, 4.42; 95% CI: 1.25–15.5; P = 0.020). Similarly, analysis of the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL)27 trial showed that, ACS patients with MS had around 1.5-fold increased risk of adverse cardiovascular events (non-fatal myocardial infarction, recurrent MI and cardiac arrest) including mortality. Moreover, a meta-analysis of 87 cohort studies confirmed that MS was associated with a two-fold increase in cardiovascular mortality and 1.5 fold increase in overall mortality.28 On the other hand, further studies with different duration of follow-up did not demonstrate a significant association between MS and cardiovascular or all-cause mortality particularly in ACS patients managed with PCI.29,30
The high risk of 30-day mortality (HR=3.25, 95% CI=1.72–6.15) observed among ACS patients with MS in the present study could be explained by higher prevalence of prior history of coronary artery disease and chronic kidney disease among patients with this syndrome which might influence mortality.31 Additionally, prolonged pre-hospital delay and sub-optimal treatment (lack of reperfusion therapy in our setup) and small sample size might also contribute to the high mortality rate observed among ACS with MS in the present study.
The present study has several limitations. First, it included a relatively small number of ACS patients from two tertiary hospitals in Ethiopia. Second, some important predictors (, Syntax score, uric acid, and white blood cell) were missed since the data were collected from an observational study (routine clinical practice). Third, the prevalence of MS might be underestimated since the use of statin for primary prevention of cardiovascular disease is not considered as MS criteria and patients who died before biochemical measurement and confirmation of ACS diagnosis were excluded. Fourth, the findings of this study are based on data collected from two tertiary hospitals in Ethiopia and cannot be generalized for other sub-Saharan African countries. Therefore, the results of the present study should be used as a hypothesis-generating and large-scale registry data needed to confirm the results.
Conclusions
The prevalence of MS among ACS patients in Ethiopia is high. MS is associated with in-hospital MACE particularly, heart failure and cardiogenic shock with a significant increase in 30-day mortality. Timely diagnosis, prevention, and management of different components of MS could improve the outcome of patients with ACS.
Abbreviations
ACEI, Angiotensin Converting Enzyme Inhibitors; ACS, Acute Coronary Syndromes; ARB, Angiotensin Receptor Blockers; DAPT, Dual Antiplatelet Therapy; FPG, Fasting plasma glucose; HDL-C, High density lipoprotein cholesterol; LDL, Low density lipoprotein cholesterol; MACE, Major Adverse cardiovascular Events; MS, Metabolic syndrome; NSTE-ACS, No-ST-elevations Acute Coronary Syndromes; STEMI, ST-elevations Myocardial infarction; PCI, Percutaneous coronary intervention.
Data Sharing Statement
The data used for this study will be made available by the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study protocol was approved by the Institutional Review Board (IRB) of Jimma University, Institute of Health before initiating data collection with a reference number of IHRPGD/193/18. In addition, permission was obtained from responsible bodies of both hospitals before extracting data from active patient’s case records. All the study protocols were conducted in line with the ethical principle of the declaration of Helsinki.32 Written and verbal informed consent was obtained from all study participants. The confidentiality and privacy of study participant’s data were maintained by using different codes throughout the data collection tools.
Acknowledgments
We would like to thank Jimma University Institute of health for financially supporting this study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Institute of Health, Jimma University [JUIH/193/10, 2018]. The funding body had no involvement in study design, data collection, analysis, interpretation, manuscript writing, and in the decision to submit the article for publication.
Disclosure
The authors declare that there is no conflict of interest regarding this work.
References
1. Kelli HM, Kassas I. Cardio metabolic syndrome: a global epidemic. J Diabetes Metab. 2016;6(3). doi:10.4172/2155-6156.1000513
2. Ritchie SA, Connell JMC. The link between abdominal obesity, metabolic syndrome and cardiovascular disease. Nutr Metab Cardiovasc Dis. 2007;17(4):319–326. doi:10.1016/j.numecd.2006.07.005
3. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112(17):2735–2752. doi:10.1161/CIRCULATIONAHA.105.169404
4. Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20(2):12. doi:10.1007/s11906-018-0812-z
5. Jaspers Faijer-Westerink H, Kengne AP, Meeks KAC, Agyemang C. Prevalence of metabolic syndrome in sub-Saharan Africa: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. 2020;30(4):547–565. doi:10.1016/j.numecd.2019.12.012
6. Gouda HN, Charlson F, Sorsdahl K, et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: results from the Global Burden of Disease Study 2017. Lancet Glob Heallth. 2019;7(10):e1375–87. doi:10.1016/S2214-109X(19)30374-2
7. Cappuccio FP, Miller MA. Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern Emerg Med. 2016;11(3):299–305. doi:10.1007/s11739-016-1423-9
8. Yuyun MF, Sliwa K, Kengne AP, Mocumbi AO, Bukhman G. Cardiovascular diseases in sub-saharan Africa compared to high-income countries: an epidemiological perspective. Glob Heart. 2020;15(1):15. doi:10.5334/gh.403
9. Ambachew S, Endalamaw A, Worede A, Tegegne Y, Melku M, Biadgo B. The prevalence of metabolic syndrome in ethiopian population: a systematic review and meta-analysis. J Obes. 2020;2020:2020. doi:10.1155/2020/2701309
10. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005;28(7):1769–1778. doi:10.2337/diacare.28.7.1769
11. Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006;119(10):812–819. doi:10.1016/j.amjmed.2006.02.031
12. Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death. A systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49(4):403–414. doi:10.1016/j.jacc.2006.09.032
13. Gurka MJ, Filipp SL, Deboer MD. Geographical variation in the prevalence of obesity, metabolic syndrome, and diabetes among US adults article. Nutr Diabetes. 2018;8(1). doi:10.1038/s41387-018-0024-2
14. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60(16):1581–1598. doi:10.1016/j.jacc.2012.08.001
15. Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; American heart association; World heart federation; International. Circulation. 2009;120(16):1640–1645. doi:10.1161/CIRCULATIONAHA.109.192644
16. Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome - A new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469–480. doi:10.1111/j.1464-5491.2006.01858.x
17. Al Suwaidi J, Zubaid M, El-Menyar AA, et al. Prevalence of the metabolic syndrome in patients with acute coronary syndrome in six middle eastern countries. J Clin Hypertens. 2010;12(11):890–899. doi:10.1111/j.1751-7176.2010.00371.x
18. Wang HH, Jia SD, Liu Y, et al. [The impact of metabolic syndrome and its individual components on long-term prognosis of patients undergoing percutaneous coronary intervention]. Zhonghua Yi Xue Za Zhi. 2020;100(21):1623–1628. doi:10.3760/cma.j.cn112137-20190920-02077. [Chinese]
19. Cavallari I, Cannon CP, Braunwald E, et al. Metabolic syndrome and the risk of adverse cardiovascular events after an acute coronary syndrome. Eur J Prev Cardiol. 2018;25(8):830–838. doi:10.1177/2047487318763897
20. Ansarimoghaddam A, Adineh HA, Zareban I, Iranpour S, HosseinZadeh A, Kh F. Prevalence of metabolic syndrome in Middle-East countries: meta-analysis of cross-sectional studies. Diabetes Metab Syndr Clin Res Rev. 2018;12(2):195–201. doi:10.1016/j.dsx.2017.11.004
21. Li R, Li W, Lun Z, et al. Prevalence of metabolic syndrome in mainland China: a meta-analysis of published studies. BMC Public Health. 2016;16(1):1–10. doi:10.1186/s12889-016-2870-y
22. Zeller M, Steg PG, Ravisy J, et al. Prevalence and impact of metabolic syndrome on hospital outcomes in acute myocardial infarction. Arch Intern Med. 2005;165(10):1192–1198. doi:10.1001/archinte.165.10.1192
23. Lovic MB, Djordjevic DB, Tasic IS, Nedeljkovic IP. Impact of metabolic syndrome on clinical severity and long-term prognosis in patients with myocardial infarction with ST-segment elevation. Hell J Cardiol. 2018;59(4):226–231. doi:10.1016/j.hjc.2018.02.002
24. Widecka K, Safranow K, Lewandowski M, Przybycień K, Gorący J, Kornacewicz-Jach Z. Angiographic severity of coronary artery disease and cardiovascular risk in acute coronary syndrome in patients with metabolic syndrome. Kardiol Pol. 2018;76(3):662–668. doi:10.5603/KP.a2017.0259
25. Miri R, Sajjadieh A, Parsamahjoob M, et al. Relationship between metabolic syndrome and angiographic severity of coronary artery disease. ARYA Atheroscler. 2016;12(5):220–225.
26. Al-Rasadi K, Sulaiman K, Panduranga P, Al-Zakwani I. Prevalence, characteristics, and in-hospital outcomes of metabolic syndrome among acute coronary syndrome patients from Oman. Angiology. 2011;62(5):381–389. doi:10.1177/0003319710382419
27. Schwartz GG, Olsson AG, Szarek M, Sasiela WJ. Relation of characteristics of metabolic syndrome to short-term prognosis and effects of intensive statin therapy after acute coronary syndrome: an analysis of the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) trial. Diabetes Care. 2005;28(10):2508–2513. doi:10.2337/diacare.28.10.2508
28. Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–1132. doi:10.1016/j.jacc.2010.05.034
29. Won KB, Kim BK, Chang HJ, et al. Metabolic syndrome does not impact long-term survival in patients with acute myocardial infarction after successful percutaneous coronary intervention with drug-eluting stents. Catheter Cardiovasc Interv. 2014;83(5):713–720. doi:10.1002/ccd.25150
30. Lee Y, Lim YH, Shin JH, Park J, Shin J, Kim KS. The impact of metabolic syndrome on clinical outcomes after everolimus-eluting stent implantation. Am J Cardiol. 2015;116(5):717–724. doi:10.1016/j.amjcard.2015.05.041
31. Liu L, Miura K, Fujiyoshi A, et al. Impact of metabolic syndrome on the risk of cardiovascular disease mortality in the United States and in Japan. Am J Cardiol. 2014;113(1):84–89. doi:10.1016/j.amjcard.2013.08.042
32. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
