Back to Journals » Research and Reports in Neonatology » Volume 11
Prevalence and Determinants of Appropriate Child Feeding Practice Among Mothers Having Children with and without Diarrhea Aged 6–23 Months in Debre Berhan Town, Ethiopia
Authors Asfaw T
Received 11 December 2020
Accepted for publication 15 February 2021
Published 1 March 2021 Volume 2021:11 Pages 35—42
DOI https://doi.org/10.2147/RRN.S289640
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Schelonka
Tsegahun Asfaw
Department of Medical Laboratory Science, Debre Berhan University, Debre Berhan, North Shoa, Ethiopia
Correspondence: Tsegahun Asfaw P. Box: 445 Email [email protected]
Background: In Ethiopia, data related to the appropriate child feeding (ACF) practice is limited. Complementary foods are not introduced in a timely fashion for many children, and most mothers do not follow the established recommended national child feeding strategy. Therefore, this study was designed to evaluate the prevalence, and determinants of ACF practice among mothers having children with and without diarrhea aged 6– 23 months.
Methods: A comparative cross-sectional study design was performed from January to May 2020. A sample size of 261 mothers of a child with diarrhea and 500 mothers of a child without diarrhea was recruited. The data were conducted by using a pretested and structured questionnaire. Data were clean-code and enter into EPI-data, version 3.1 and exported to IBM SPSS, version 21 for analysis. Multivariable binary logistic regression analysis was conducted. P-value less than or equal to 0.05 was considered as statistically significant.
Results: The overall prevalence of ACF practice was 70.3%. Sufficient maternal knowledge [AOR = 4.3 (95% CI; 2.1– 8.8)] and post natal care (PNC) visit [AOR = 2.2 (95% CI; 1.1– 4.5)] were factors associated with ACF practice among mothers having children with diarrhea. However, maternal knowledge [AOR = 4.98 (95% CI; 3.0– 8.3)] was the only significant associated factor with ACF practice for mothers having children without diarrhea.
Conclusion: The prevalence of ACF practice among mothers having children with diarrhea is lower than mothers having children without diarrhea. Maternal knowledge was a significantly associated factor of ACF practice for mothers having children both with and without diarrhea.
Keywords: children, feeding practice, mothers, diarrhea
Introduction
The appropriate child feeding (ACF) practice is vital for the survival, growth, development, health, and nutrition of children; but only a few children obtain nutritionally sufficient and safe complementary food worldwide.1 Preferably, infants should be breastfed within one hour of birth. Starting at 6 months, breastfeeding should be combined with safe, age-appropriate feeding of solid, semi-solid and soft foods. An infant that is not exclusively breastfed could be at a significantly higher risk of death from diarrhea or pneumonia.2
Globally in 2016, 155, 52, and 41 million children under five were estimated to be stunted, wasted, and overweight, respectively.3 Only two-fifths of infants aged 0–6 months were exclusively breastfed, fewer children received sufficient and safe complementary food, and less than one-fourth of children aged 6–23 months met minimum dietary frequency and minimum meal frequency.3 Children are susceptible to malnutrition and infectious disease at 6–23 months of age. Hence, infant diet should be nutrient dense with ACF practice. A poor child feeding practice has significant association with childhood diarrhea; in which, children who had diarrhea have greater odds of developing acute malnutrition.4,5 Malnutrition reduces the immune system and causes frequent illnesses in children. It is a major problem in developing countries.
In Ethiopia, the prevalence of exclusive breastfeeding until six months is 58%, while only 76% of children continued breastfeeding until 18–23 months of age.6 In Ethiopia, the incidence of consumption of vitamin A-rich and iron-rich foods, were 4.6% and 1.9% respectively.7 Optimum children feeding practice is protective against childhood diarrheal and other causes of morbidity, but adherence to scientifically recommended ACF practice remains poor in developing countries, including Ethiopia.8 The study in Ethiopia showed the low prevalence of ACF practice is associated with maternal educational status, place of delivery, socioeconomic status, maternal employment status, and access to mass media.
One of the sustainable development goals in Ethiopia is reduction of child mortality. This can be achieved by ACF practice so that infant and child deaths related to diarrheal disease is significantly reduced. However, there has been an information gap regarding prevalence and determinants of ACF practice in Ethiopia among mothers who have children with and without diarrhea among governmental and nongovernmental organizations, health care providers, and other respective stakeholders. Therefore, this study was designed to evaluate the prevalence, and determinants of ACF practice among mothers having children, with and without diarrhea, aged 6–23 months.
Materials and Methods
Study Area Period
This study was conducted at Debre Berhan town, located 130 kilometers northeast of Addis Ababa, Ethiopia. Debre Berhan town has three health centers, one referral hospital, and forty health posts. A comparative cross-sectional study design was conducted from January to May 2020.
Sample Size
The sample size required was calculated by using double population proportion formula by assuming; 95% confidence level, 10% nonresponse rate, ratio of exposed to unexposed 1:2, prevalence of introduction of complementary feeding at 6 months among children without diarrhea (p1 = 68.8%) and introduction of complementary feeding at 6 months among children with diarrhea (p2 = 56.5%).9 Finally, a total sample size of 783 was obtained.
Sampling Technique and Procedures
The number of mothers/caregivers selected in this study were allocated proportionally by dividing the number of mothers having children who visited each health facility by the total number of mothers having children who visited a health facility in the town to obtain a total sample size of 783 with a ratio of 1:2 for exposed and unexposed groups and recruited consecutively.
Data Collection
Data were collected by interviewing mothers/caregivers by using a pretested structured questionnaire (supplemental material 1). Pretest was conducted at the Debre Berhan referral hospital among 39 mothers of children with and without diarrhea (5% of the sample size).
Data Quality Control
Data collectors were trained before data collection started. Data collection was performed by 2 nurses and 2 midwives. The consistency and completeness of data were checked by investigators and supervisors. All data were cleaned and checked before coding and handled carefully.
Data Processing and Analysis
Data were analyzed using SPSS, version 21 software. Descriptive statistics were summarized in the tables. Binary logistic regression method was used to find variables associated with ACF practice. All explanatory variables associated with outcome variables with P < 0.2 were entered into multivariable logistic regression analysis. The variables and their significant association were identified by AOR, 95% CI, and P-value (<0.05).
Ethical Considerations
Ethical clearance was obtained from Debre Berhan University Ethical Review Committee. The official letter of co-operation was gained from each health institution. The aim of the study was explained by sample collector for participants. Informed consent was obtained from each child's mother/caregiver, after explaining about the research work, its confidentiality, protection, and anonymity of data. Finally, mothers/caregivers were advised on the child feeding practice. This study was conducted in accordance with the Declaration of Helsinki.
Operational Definitions
Appropriate Child Feeding Practice
The exclusive breastfeeding of children until 6 months, timely initiation of breastfeeding, non-use of bottle feeding, minimum meal frequency, minimum dietary diversity and timely introduction of solid, semi-solid and soft foods at 6–8 months. A practice that was appropriate for a specific age group obtained a score of 1, and a practice that was inappropriate obtained a score of 0. If the summed score of the indicators is ≥4, it was considered as ACF practice.9
Sufficient Knowledge of Appropriate Child Feeding Practice
When the participants correctly answer above 60% of the knowledge questionnaires about ACF practice.9
Sufficient Attitude of Appropriate Child Feeding Practice
When the participants agree and strongly agree to median and above favorable questions on ACF practice.9
Minimum Dietary Diversity
Proportion of children at 6–23 months of age who obtain foods from four or more food groups during the previous day (supplemental material 1).9
Minimum Meal Frequency
Proportion of breastfed and non-breastfed children at 6–23 months of age who receive solid, semi-solid, or soft foods the minimum number of times or more (minimum is defined as: two times for breastfed infants, 6–8 months; three times for breastfed children, 9–23 months; and four times for non-breastfed children, 6–23 months) in the previous day.9
Results
Socio-Demographic Characteristics
A total of 783 mothers having children aged 6–23 months participated, with a response rate of 97.2%. Among the 761 mothers/caregivers, 261 (34.3%) respondents were mothers of children with diarrhea and 500 (65.7%) respondents were mothers of children without diarrhea. The mean (± SD) age of mothers of children with diarrhea and without diarrhea was 32(±6) and 30.6(±5.6) years respectively. Two-fifths 102 (39.1%) and 177 (35.4%) of children with and without diarrheal episodes were at the age of 6 and 11 months, respectively (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Mothers of Children Aged 6–23 Months in Debre Berhan Town, Ethiopia, 2020 |
Health Service Utilization and Child Feeding Information
The majority of mothers of the children with diarrhea (90%) and the mothers of the children without diarrhea (92.2%) attended at least one antenatal care (ANC) visit. Among mothers of children who had ANC visits, the majority had 3 ANC visits (Table 2).
 |
Table 2 Maternal Health Service Utilization and Feeding Information in Debre Berhan Town, Ethiopia, 2020 |
Breast and Complementary Feeding Practice
The majority of mothers of the children with diarrhea (65.1%) and the mothers of the children without diarrhea (76.4%) initiated breastfeeding within the first hour of delivery. The prevalence of exclusive breastfeeding among mothers having a child with diarrheal episodes and not having diarrheal episodes was 177 (67.8%) and 353 (70.6%) respectively (Table 3).
 |
Table 3 Child Feeding Practices of Mothers of Children Aged 6–23 Months in Debre Berhan Town, Ethiopia, 2020 |
Knowledge and Attitude of Mothers on ACF
Only half of mothers of children with diarrhea (49.8%) and two-thirds mothers of children without diarrhea (67.4%) had sufficient knowledge about ACF practice. Nearly half of mothers of children with diarrhea (46.4%) and two-thirds mothers of children without diarrhea (61.4) had a favorable attitude to ACF practice.
Magnitude of ACF Practice
The overall prevalence of ACF practice in this study was 70.3%. Pearson chi-square test showed, there was statistically significant difference in ACF practice between mothers of children with diarrhea and without diarrhea (Pr = 0.024) (Figure 1).
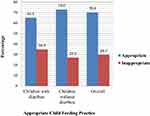 |
Figure 1 Prevalence of ACF practice among mothers of children with diarrhea and without diarrhea in Debre Berhan town, Ethiopia, 2020. |
Factors Associated with ACF Practice
The output of multivariable analysis revealed, the maternal knowledge and PNC visits were significantly associated with ACF practice for mothers of children with diarrhea (Table 4). However, maternal knowledge was the only significant associated factor with ACF practice for mothers of children without diarrhea (Table 5).
 |
Table 4 Factors Associated with ACF Practice Among Mothers of Children Aged 6–23 Months with Diarrhea in Debre Berhan Town, Ethiopia, 2020 |
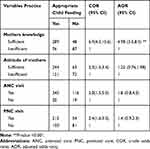 |
Table 5 Factors Associated with ACF Practice Among Mothers of Children Aged 6–23 Months without Diarrhea in Debre Berhan Town, Ethiopia, 2020 |
Discussion
This study was designed to compare the prevalence and associated factors of ACF practice among mothers of children with diarrhea and without diarrhea. Diarrheal episodes are commonly reported as key determinants of sub-optimal child feeding practice. This study also tried to identify determinants of ACF practice separately for both children with diarrhea and without diarrhea.
The majority of mothers of the children with diarrhea (65.1%) and the mothers of the children without diarrhea (76.4%) initiated breastfeeding within the first hour of delivery. The prevalence of exclusive breastfeeding among mothers having a child with diarrheal episodes and not having diarrheal episodes was 177 (67.8%) and 353 (70.6%) respectively. The overall prevalence of ACF practice was 70.3% which is comparable to a study done in the Amibara district, northeast Ethiopia (69.2%)10 and Assela town, southeast Ethiopia (70%).11 However, it is higher than studies conducted in the Burao district, Somaliland among 464 randomly selected mothers with children 6–24 months of age (20.47%),12 Dilla Zuria district, Gedeo Zone, southern Ethiopia (57.6%),13 northern Ethiopia (15%),14 Pawe District, northwest Ethiopia (61.8%),15 Axum (52.8%),16 Kamba (54.4%),17 Lasta district, northeast Ethiopia (56.5%)18 and Damot Sore district, southern Ethiopia (11.4%)19 The possible reason might be due to this study being conducted at health facility level; the fact that those mothers who had visited health facilities had better knowledge as compared to those who had not visited health facilities. This difference also might be due to behavioral characteristics of study participants, the existence of a nutrition intervention program by a nongovernmental organization, and the efforts of health extension workers, health professionals, nutrition animators, and practices changing with time.
The overall prevalence of ACF among mothers in our study is higher than studies done in other African countries like, from a study done in Ghana (64%)20 and Uganda (46.5% to 55.2%).21 These differences might be due to the socioeconomic status of the participants and/or access to health institutions, sample sizes and study setting difference. Age differences between the studies participants might be also a reason because children less than 6 months of age were included in the study from Ghana.20 However, this study showed a lower prevalence than from a study done in Nigeria (85.4%).22 This could be due to the age difference of study participants; the study done in Nigeria includes children only between 6–8 months.
The finding of this study was lower than the WHO recommendation for good practice of complimentary feeding (≥80%)23 and the study reports of other developing countries, such as India (77.5%)24 and Nepal (87.3%).25 This difference might be due to higher maternal literacy rates and utilization of institutional delivery in the latter study areas,25 which are the main fertile grounds to step-up mothers’ attitude towards ACF practices and the previous researches also illustrated that mother’s education was positively associated with timely initiation of complimentary feeding.23
Pearson chi-square test showed that there was a statistically significant difference in ACF practice between mothers of children with diarrhea and without diarrhea (Pr = 0.024). Accordingly, a lower proportion of ACF practice was observed among children with diarrhea 170 (65.1%) than those without diarrhea 365 (73%). This is supported by a study done in West Gojjam Zone, Achefer district which depicts there is a significant difference in an exclusive breastfeeding practice among children with diarrhea and without diarrhea 12.3% and 83%, respectively.26
In this study maternal knowledge and PNC visit was significantly associated with ACF practice for children with diarrhea. The result was similar to other studies of Ethiopia in different districts. In general, a PNC visit is important to increase mothers’ knowledge and attitude about ACF practices through providing child feeding counseling and behavioral change and communication interventions.27 Other studies in Africa also acknowledged promising encouragement of mothers’ knowledge for proper implementation of ACF practices.28–30 In this study, maternal knowledge had also showed significant association with ACF practice of mothers having children without diarrhea. In general, this is the result of the current national nutrition program and national nutrition strategy and community based nutrition implementation through health extension workers which are currently implemented in the study area, in which mothers of children who had been able to read and write can receive better information on the child feeding practice than others.
This study has shown that the prevalence of ACF practice was lower among mothers of children with diarrhea than mothers of children without diarrhea. Factors like maternal knowledge and PNC visit were significantly associated with ACF practice among mothers of children with diarrhea. While, maternal knowledge was significantly associated with ACF practice among mothers of children without diarrhea. Therefore, it is better to give due attention to the improvement of knowledge of mothers on ACF practice through advising and counseling during prenatal care, ANC visit, PNC visit, and immunization services.
Since this study included only mothers having a child and attending health facilities, the findings may not be generalizable to those who had not sought care at the time of data collection. Recall bias might also be committed since the measurement of some variables rely on the mother's recall.
Data Sharing Statement
All raw data are available upon request from the corresponding author.
Disclosure
The author reports no conflicts of interest in this work.
References
1. WHO, and, UNICEF. Global Strategy for Infant and Young Child Feeding:WHO, and, UNICEF; 2001.
2. UNICEF. Adoption optimal feeding practices is fundamental to a child’s survival, growth and development, but too few children benefit. https://datauniceforg/topic/nutrition/infant-and-young-child-feeding/. 2018.
3. Abuka T, Jember D, Tsegaw D. Determinants for acute malnutrition among under-five children at public health facilities in Gedeo Zone, Ethiopia: a case-control study. Pediatr Ther. 2017;7(317):2161–2665.
4. Asfaha KF, Tesfamichael FA, Fisseha GK, et al. Determinants of childhood diarrhea in Medebay Zana District, Northwest Tigray, Ethiopia: a community based unmatched case-control study. BMC Pediatr. 2018;18(1):120.
5. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
6. Roba KT, O’Connor TP, Belache T, O’Brien NM. Infant and young child feeding practices among mothers of children aged 6–23 months in two agro-ecological Zones of Rural Ethiopia. Int J Food Sci Nutr. 2016;5(3):185–194.
7. Demilew YM. Factors associated with mothers’ knowledge on infant and young child feeding recommendation in slum areas of Bahir Dar City, Ethiopia: cross sectional study. BMC Res Notes. 2017;10:191.
8. Solomon D, Aderaw Z, Tegegne TK. Minimum dietary diversity and associated factors among children aged 6–23 months in Addis Ababa, Ethiopia. Int J Equity Health. 2017;16(1):181. doi:10.1186/s12939-017-0680-1
9. WHO/UNICEF/USAID/FANTA/IFPRI. Indicators for Assessing Infant and Young Child Feeding Practices: Part 1: Definitions. Geneva: World Health Organization; 2008.
10. Wagris M, Seid A, Kahssay M, Ahmed O. Minimum meal frequency practice and its associated factors among children aged 6–23 months in Amibara District, North East Ethiopia. J Environ Public Health. 2019;7.
11. Sasie SD, Oljira L, Demena M. Infant and young child feeding practice and associated factors among mothers/caretakers of children aged 0–23 months in Asella Town, South East Ethiopia. J Fam Med. 2017;4(5):1122.
12. Jama A, Gebreyesus H, Wubayehu T, et al. Exclusive breastfeeding for the first six months of life and its associated factors among children age 6-24 months in Burao district, Somaliland. Int Breastfeed J. 2020;15:5. doi:10.1186/s13006-020-0252-7
13. Reddy S, Abuka T. Determinants of exclusive breastfeeding practice among mothers of children under two years old in dilla Zuria District, Gedeo Zone, Snnpr, Ethiopia, 2014. J Preg Child Health. 2016;3:224. doi:10.4172/2376-127X.1000224
14. Belete Y, Awraris W, Muleta M. Appropriate complementary feeding practice was relatively low and associated with mother’s education, family income, and mother’s age: a community based cross-sectional study in Northern Ethiopia. J Nutr Health Food Eng. 2017;6(2):29–35.
15. Ayana D, Tariku A. Feleke A and Woldie H. Complementary feeding practices among children in Benishangul Gumuz Region, Ethiopia. BMC Res Notes. 2017;10:335.
16. Yemane S, Awoke T, Gebreslassie M. Timely initiation of complementary feeding practice and associated factors among mothers of children aged from 6 to 24 months in Axum Town, North Ethiopia. Int J Nutr Food Sci. 2014;3(5):438–442.
17. Agedew E, Demissie M, Misker D, Haftu D. Early initiation of complementary feeding and associated factors among 6 months to 2 years young children, in Kamba Woreda, South West Ethiopia: a community-based cross-sectional Study. J Nutr Food Sci. 2014;4:314.
18. Molla M, Tadese Ejigu T, Nega G. Complementary feeding practice and associated factors among mothers having children 6–23 months of age, Lasta District, Amhara Region, Northeast Ethiopia. Adv Public Health. 2017;8.
19. Areja A, Dereje Yohannes D, Yohannis M. Determinants of appropriate complementary feeding practice among mothers having children 6–23 months of age in rural Damot sore district, Southern Ethiopia; a community-based cross-sectional study. BMC Nutr. 2017;3:82.
20. Tampah-Naah AM, Kumi-Kyereme A. Determinants of exclusive breastfeeding among mothers in Ghana: a cross-sectional study. Int Breastfeed J. 2013;8:13.
21. Mokori A, Schonfeldt H, Sheryl L. Hendriks. Child factors associated with complementary feeding practices in Uganda. S Afr J Clin Nutr. 2017;30(1):7–14.
22. Udoh EE, Amodu OK. Complementary feeding practices among mothers and nutritional status of infants in Akpabuyo Area, Cross River State Nigeria. Springer Plus. 2016;5:2073.
23. World Health Organization. Infant and Young Child Feeding. A Tool for Assessing National Practices: Policies and Programs. Geneva; 2003.
24. Rao S, Swathi PM, Unnkrishanan B, Hegade A. study of complementary feeding practice on mothers of child aged two to two years from coastal south India. Australas Med J. 2011;4:252.
25. Joshi N, Agho KE, Dibley MJ. Determinants of inappropriate complementary feeding practices in young children in Nepal. Secondary data analysis of demographic and health survey. Mater child nutr. 2006;8:45.
26. Girma M, Gobena T, Medhin G, Gasana J, Roba KT. Determinants of childhood diarrhea in West Gojjam, Northwest Ethiopia: a case control study. Pan Afr Med J. 2018;30:234.
27. Muluye D, Woldeyohannes D, Gizachew M, Tiruneh M. Infant feeding practice and associated factors of HIV positive mothers attending prevention of mother to child transmission and antiretroviral therapy clinics in Gondar Town health institutions, Northwest Ethiopia. BMC Public Health. 2012;12:240.
28. Arusei R, Ettyang G, Esamai F. Feeding patterns and growth of term infants in Eldoret Kenya. Food Nutr Dietetics. 2011;32:307–314.
29. Onuoha NO, Ibeanu VN, Chiekwu IM. Knowledge and practice of infant feeding by nursing mothers living with HIV/AIDS attending University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, Enugu, Nigeria. Niger J Nutr Sci. 2011;32(2):51–55.
30. Fjeld E, Siziya S, Katepa-Bwalya M, Kankasa C, Moland K, Tylleskär T. ‘No sister, the breast alone is not enough for my baby’ a qualitative assessment of potentials and barriers in the promotion of exclusive breastfeeding in southern Zambia. Int Breastfeed J. 2008;3:26.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
