Back to Journals » Research and Reports in Urology » Volume 11
Prevalence and awareness of varicocele among athletes in Riyadh, Saudi Arabia
Authors Hariri A , Abbarh S , Ameen A , Sabra A , Salman A , Alhulaimi Y , Aabed M , Habous M, Madbouly K, Binsaleh S
Received 22 November 2018
Accepted for publication 15 January 2019
Published 13 February 2019 Volume 2019:11 Pages 21—27
DOI https://doi.org/10.2147/RRU.S195582
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Albara Hariri,1 Shahem Abbarh,1 Aref Ameen,1 Ahmad Sabra,1 Ahmad Salman,1 Yaser Alhulaimi,1 Mahmoud Aabed,1 Mohamad Habous,2 Khaled Madbouly,3 Saleh Binsaleh4
1Faculty of Medicine, Al-Maarefa University, Riyadh, Saudi Arabia; 2Department of Urology and Andrology, Elaj Medical Centers, Jeddah, Saudi Arabia; 3Department of Urology, Prince Mohammed Bin Abdulaziz Hospital, Riyadh, Saudi Arabia; 4Division of Urology, Department of Surgery, Faculty of Medicine, King Saud University, Riyadh, Saudi Arabia
Purpose: To evaluate the prevalence and awareness about symptoms, and complications of varicocele among athletes (bodybuilding and aerobics exercises) in Riyadh, Saudi Arabia.
Patients and methods: A cross-sectional study of male athletes aged between 18 and 48 years old was carried out in multiple branches of fitness centers over a period of 13 months in Riyadh, Saudi Arabia. A total of 382 face-to-face interviews using a predesigned questionnaire were conducted to identify the levels of knowledge, attitude, and practice. A randomly selected 48 subjects were examined. Varicocele was diagnosed and graded based on clinical examination and Doppler ultrasonography.
Results: Of the participants, 157 (41%) lacked knowledge and awareness regarding varicocele, its symptoms and complications. Of the examined participants, 22 (46%) were found to have varicocele. No difference in varicocele was found among bodybuilders and aerobic athletes (P=0.249). Similarly, no difference was related to duration of exercise session whether for 1 hour or more (P=0.131). However, our study revealed a higher rate of varicocele among athletes who exercised more than three times per week (P=0.009). Testicular volume was neither significantly different among respondents with and without varicocele nor between the left or right sides within each group.
Conclusion: Knowledge about varicocele, its symptoms and complications is poor among male athletes in Riyadh, Saudi Arabia. Varicocele is more common in athletic men who are frequently exercising. Efforts to increase knowledge and enhance awareness of varicocele in young males, in general, are strongly warranted.
Keywords: athletes, varicocele, testis, awareness, knowledge
Introduction
Varicocele is an abnormal tortuous dilatation of the pampiniform plexus in the scrotal portion of spermatic veins that drains blood from the testis.1 The pathogenesis of varicocele formation, although somewhat unclear, is thought to be related to various factors resulting in an increase in pressure in the veins of the pampiniform plexus and its venous drainage. Varicocele is more common in the left side.1
Based on physical examination, varicocele is graded according to the system of Dubin and Amelar as grade 1, 2, or 3.2 Subclinical varicocele is not palpable or visible at rest or during the Valsalva maneuver but is demonstrable by special tests. The diagnosis of subclinical should be confirmed by additional investigations.2,3
Varicocele is found in 15% of all men worldwide.4 It is reported in 19–41% of men presenting with primary infertility and in 45–81% of men with secondary infertility and remains the most common cause of male infertility.4 In the Gulf region (Qatar), 43% of infertile men were confirmed to have varicocele.5 It has been reported in 24% of healthy young population in Turkey,6 as a similar community to Saudi Arabia.
Varicocele-related pain increases during exercise suggesting a role of exercise in its pathophysiology.7 Up to 30% of athletes are diagnosed with varicocele, representing a significantly higher incidence than in the general population, and up to 60–80% of bodybuilders are recorded as being affected.8 In a study of over 1,000 males, Radojevic et al9 showed that varicocele prevalence was higher in males playing basketball, football, handball, and volleyball than in sport-inactive controls (17.05% vs 12.35%). Some studies suggested that exercise (bodybuilding and aerobic) might be an aggravating factor of varicocele.7,10,11 Athletes were found to have significantly worse varicocele than nonathletes.11 Furthermore, it has been reported that subclinical varicocele will progress to clinically palpable varicocele over years of forced physical activity in athletes.12
Very few studies explored athletes’ awareness of this condition. Half of young athlete participants of two studies were unaware why the genitals were examined on sports physical examination.13,14
This study aims to evaluate the prevalence and awareness regarding symptoms and complications of varicocele among athletes in Riyadh, Saudi Arabia. To our knowledge, no similar studies were locally conducted.
Patients and methods
A cross-sectional study, community-based survey of male athletes (exercising for fitness and good health) was carried out over a period of 13 months (from July 2017 to August 2018). The study included five branches of fitness centers covering a population of 14,000 in Riyadh, Saudi Arabia. There were 382 questionnaire respondents, while there were only 48 examination respondents.
The study’s sample population included all male athletes, aged 18–48 years old, practicing bodybuilding and/or aerobic exercises. Athletes below the age of 18 years were not included due to difficulty in obtaining legal consent. Athletes above 48 years of age were also excluded as their few numbers were not enough to be used as a representative data for this age group. Other exclusion criteria included subjects who were training for <6 months, diagnosed before they began exercising, had a previous surgery for varicocele, or having heavy-labor occupations that may affect validity of the study.
College of Medicine, King Saud University Institutional Review Board clearance was obtained prior to the initiation of the study. All participants provided a written informed consent, and the study was conducted in accordance with the Declaration of Helsinki. During these sport center visits, the aims of the study were explained to the eligible members and data were collected by personal, face-to-face interviews, using a predesigned questionnaire. The questionnaire included details on awareness of participants regarding symptoms and complications of varicocele, type and frequency of exercise, previous diagnosis and surgery for varicocele, and presence of family history of varicocele (Supplementary material S1).
Forty-eight subjects were randomly selected from the five fitness centers in proportion to their population sizes and were examined in the urology clinic in King Khalid University Hospital. Varicocele was diagnosed clinically using a predesigned form (Supplementary material S2). Subjects were requested to stand upright relaxed for inspection of visible enlargement and while applying Valsalva maneuvers (eg, cough) for palpable enlargement of pampiniform plexus. Varicocele was graded based on clinical examination and application of the Dubin and Amelar grading system.2 A person was considered to have grade 1 if the varicocele is palpable during Valsalva maneuver but not otherwise, grade 2 if palpable at rest, grade 3 if visible and palpable at rest. Abnormal findings during physical examination were further evaluated by high-resolution, color-flow Doppler ultrasonography to assess maximum vein diameter, blood flow direction, grade of varicocele (if present), testicular size, and any other pathology. Testicular size was measured in three dimensions. The volume of the testicles was calculated by multiplying the dimensions with the standard coefficient of 0.71. Vein diameter of 3 mm or larger while patient was at rest was considered diagnostic for varicocele. Respondents with bilateral varicoceles were assigned the grade of the most advanced side.
Data analysis
Descriptive statistics are presented as the mean ± SD and percent. For comparative statistics, chi-squared/Fisher’s exact tests and independent/paired t-test were used as appropriate. A P-value <0.05 was considered significant for all tests performed. All statistical analysis was performed using IBM SPSS Statistics version 21.0 (IBM Corporation, Armonk, NY, USA).
Results
Out of 382 athlete participants, 157 (41%) have never heard about varicocele. Among the 225 athletes who reported knowledge about varicocele, 172 (76.4%) correctly defined varicocele as dilatation of the testicular veins. Others (53, 23.6%) incorrectly defined it as a testicular inflammation, absence of one testis or testicular torsion. Similarly, 177/225 (78.7%) properly reported dull testicular pain as the most common symptom of varicocele while 157/225 (69.8%) appreciated the relation of varicocele to male infertility (Table 1).
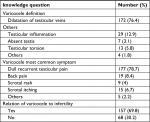  | Table 1 Knowledge regarding varicocele definition, most common symptom, and relation to infertility |
Out of the 48 examined respondents, 26 (54.2%) had no varicocele. Left varicocele was diagnosed in 17 (35.4%) and bilateral varicocele in 5 (10.4%). Prevalence and grades of varicocele detected are shown in Figure 1.
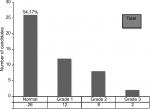  | Figure 1 Prevalence and grade of varicocele. |
We tested the association of varicocele prevalence and grade with the frequency of exercising (3, 4, or 5 days/week), duration of the exercise session (1 hour vs >1 hour), as well as the type of exercise, whether, mainly aerobics (jogging, cycling, swimming, etc), bodybuilding or both (Table 2). Prevalence and grade of varicocele were found to be significantly related to the number of days they exercise/week (P=0.009). Of the examined athletes with varicocele, 2/22 (9.1%) were exercising for 3 days/week and the remaining 20 (90.9%) were exercising for >3 days. Furthermore, 75% of the examined athletes with grade 2 varicocele exercise 4 days/week while 100% of the examined athletes with grade 3 varicocele exercise 5 days/week (Table 2). No significant differences were found between varicocele prevalence and grade with the duration of exercise sessions (P=0.131) or with the type of exercise (P=0.249).
  | Table 2 Varicocele grades and relation to type, frequency and duration of exercise Note: aFisher’s exact test. |
Testicular volume showed no significant difference among respondents with and without varicocele both on the left (P=0.589) and the right (P=0.497) sides (Table 3). Similarly, the right testicular volume was slightly and insignificantly more than on the left side within each group (Table 3).
  | Table 3 Volume of the right and left testes in the examined respondents group Notes: aPaired t-test. bIndependent t-test. |
Discussion
A large percentage of our athlete participants (41%) lacked the knowledge and awareness regarding varicocele, its symptoms and complications. Furthermore, a good portion of the respondents who had heard about varicocele incorrectly identified its definition (53/225, 23.7%), symptoms (38/225, 21.3%), and relation to infertility (68/225, 30.2%). Similar results were reported about knowledge regarding benign testicular disorders (BTDs) in Pakistan, where more than half of the participants had little knowledge about BTDs (including varicocele).15
The lack of studies regarding the knowledge and awareness about varicocele in the general population as well as in athletes in Saudi Arabia is due to the taboo nature of this topic as considered by the majority of participants. Both social and religious restrictions are placed in the Saudi society when discussing such sensitive topics. Other developing countries such as Pakistan and Nigeria also showed similar trends.15,16 Thus, the level of knowledge and awareness remains excessively inadequate in such areas of the world.
Varicocele has been reported in ~40% of men presenting with infertility and has been associated with a progressive decline in fertility.1,4 Relation of varicocele to infertility has been appreciated by more than half (69.8%) of our respondents who had heard about varicocele. Similar results were reported.15
Our results showed that 46% of examined athletes have varicocele. Gulino et al8 reported a high incidence (up to 30%) of varicocele in a population of athletes and up to 60–80% in the subgroup of bodybuilders. Conversely, we did not find any relation between bodybuilding and varicocele in particular. The same rate of varicocele was encountered among bodybuilders and aerobic athletes (P=0.249). Others reported a similar prevalence of varicocele in the different sports practiced.10
Our findings revealed a higher rate of varicocele among athletes who exercised more than three times per week (P=0.009) but no relation has been found to the duration of exercise/session (P=0.131). Others reported an increasing number of athletes with higher grade of varicocele in the group with 7–12 hours training per week compared to the group of 6 hours/week.10 It is obviously clear that increasing the number of sessions/week, as in our findings, will increase the total exercise duration with more varicocele development and/or higher varicocele grade.
Although our findings had shown a smaller ipsilateral testicular volume in the respondents with varicocele compared to those without varicocele, the difference was not found to be statistically significant. Similarly, no difference was found in the testicular volume between both sides within each group. Di Luigi et al11 reported a significantly lower left testis volume than contralateral testis. This may be explained by the small sample number of the examined respondents which did not allow obtaining a statistical difference.
Exercise increases the spermatic vein diameter and reflux time in patients with varicoceles.7 Athletes with varicocele had significantly lower spermatozoa progressive forward motility (P<0.5). Moreover, 6 months after restriction of sport activities, Radojevic et al9 reported complete healing of the varicocele in 18 of the basketball, football, volleyball, or handball (BFVH) group and reduction of varicocele by one grade in 19 out of the other 31 participants of the same group. Furthermore, all the parameters of the seminal fluid analysis measured were shown to have improved in the BFVH group. This further underscores the significance of awareness regarding varicocele, particularly in athletes who have delayed fertility issues. Awareness must be raised that exercise may be a potential cause for male fertility problems.
There is a strong need for a more effective role to enhance knowledge and awareness of varicocele and BTD. Various methods concerning spreading awareness including visual and print media, social media, and campaigns are warranted.
Our study is limited by the small number of examined respondents which limits generalization of conclusions over athletes as well as the general population in Saudi Arabia. However, our study added new information about varicocele among athletes in Saudi Arabia. We recommend that the knowledge regarding BTD be made more readily available to the general population.
Conclusion
The rate of knowledge regarding varicocele among athletes in Saudi Arabia is low.
We demonstrated a high rate of varicocele among them. We are calling for more efforts to improve knowledge and awareness of varicocele and benign testicular orders among athletes as well as the general population. More studies of larger sample size are still warranted.
Acknowledgment
This study was supported by a grant from the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors report no conflict of interest in this work.
References
Practice Committee of the American Society for Reproductive Medicine, Society for Male Reproduction and Urology. Report on varicocele and infertility: a committee opinion. Fertil Steril. 2014;102(6):1556–1560. | ||
Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril. 1970;21(8):606–609. | ||
Belay RE, Huang GO, Shen JK, Ko EY. Diagnosis of clinical and subclinical varicocele: how has it evolved? Asian J Androl. 2016;18(2):182–185. | ||
Pastuszak AW, Wang R. Varicocele and testicular function. Asian J Androl. 2015;17(4):659–667. | ||
Elbardisi H, Arafa M, Rengan AK, et al. Varicocele among infertile men in Qatar. Andrologia. 2017;49(4):e12637. | ||
Soylemez H, Atar M, Ali Sancaktutar A, Bozkurt Y, Penbegul N. Varicocele among healthy young men in Turkey; prevalence and relationship with body mass index. Int Braz J Urol. 2012;38(1):116–121. | ||
Atar M, Söylemez H, Oguz F, et al. Effects of acute exercise on the diameter of the spermatic vein, and duration of reflux in patients with varicocele. Scand J Urol. 2013;47(3):206–210. | ||
Gulino G, Sasso F, D’Onofrio A, et al. [Sport, infertility and erectile dysfunction]. Urologia. 2010;77(2):100–106. Italian. | ||
Radojevic N, Radunovic M, Pajovic B. Restricting sports activity in reducing the rate of varicocele and related infertility parameters in athletes. Arch Med Sci. 2015;11(1):169–173. | ||
Rigano E, Santoro G, Impellizzeri P, et al. Varicocele and sport in the adolescent age. Preliminary report on the effects of physical training. J Endocrinol Invest. 2004;27(2):130–132. | ||
Di Luigi L, Gentile V, Pigozzi F, Parisi A, Giannetti D, Romanelli F. Physical activity as a possible aggravating factor for athletes with varicocele: impact on the semen profile. Hum Reprod. 2001;16(6):1180–1184. | ||
Zampieri N, Dall’Agnola A. Subclinical varicocele and sports: a longitudinal study. Urology. 2011;77(5):1199–1202. | ||
Nasrallah P, Nair G, Congeni J, Bennett CL, McMahon D. Testicular health awareness in pubertal males. J Urol. 2000;164(3 Pt 2):1115–1117. | ||
Congeni J, Miller SF, Bennett CL. Awareness of genital health in young male athletes. Clin J Sport Med. 2005;15(1):22–26. | ||
Saleem D, Muneer S, Younus Khan RF, et al. Knowledge, attitude and practices regarding benign testicular disorders in the educated young men of Pakistan. Cureus. 2017;9(8):e1563. | ||
Onyiriuka AN, Imoebe FE. Testicular-self examination among Nigerian adolescent secondary school boys: knowledge, attitudes and practices. J Prev Med Hyg. 2013;54(3):163–166. |
Supplementary materials
S1 Questionnaire
Thank you for participating in our questionnaire. We assure you that the information taken from you is for study and research purposes only, that will lead to better understanding of varicocele effect on healthy male athletes in Saudi Arabia.
  |
S2 Examination Form
  |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
