Back to Journals » International Journal of Women's Health » Volume 12
Prevalence and Associated Factors of Early Postnatal Care Service Use Among Mothers Who Had Given Birth Within the Last 12 Months in Adigrat Town, Tigray, Northern Ethiopia, 2018
Authors Gebreslassie Gebrehiwot T , Mekonen HH , Hailu Gebru T , Kiros KG, Gebresilassie B , Teklu G , Tesfay Tadese H , Haileslassie Y
Received 30 July 2020
Accepted for publication 12 October 2020
Published 19 October 2020 Volume 2020:12 Pages 869—879
DOI https://doi.org/10.2147/IJWH.S266248
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Tesfay Gebreslassie Gebrehiwot,1 Haftea Hagos Mekonen,1 Tsegu Hailu Gebru,1 Kbrom Gmechu Kiros,1 Berhanu Gebresilassie,2 Guesh Teklu,1 Haileslassie Tesfay Tadese,1 Yared Haileslassie1
1Nursing Department, College of Medicine and Health Science, Adigrat University, Adigrat, Ethiopia; 2Midwifery Department, College of Medicine and Health Science, Adigrat University, Adigrat, Ethiopia
Correspondence: Tesfay Gebreslassie Gebrehiwot Tel +251-945-807-481
Email [email protected]
Background: The care given for the first hours, days, and weeks after childbirth is life-threatening. So far, this period receives less attention from health-care providers than the care given to pregnancy and delivery. This study aimed to determine the prevalence and associated factors of early postnatal care service use among mothers who had given birth in the last 12 months in Adigrat Town, Tigray, Ethiopia.
Methods: A community-based cross-sectional study was conducted from March to April 2018 among 481mothers who had given birth in the last 12 months. A systematic random sampling technique was used to select study participants. A pre-tested and structured questionnaire was used to collect the data. Data analysis was computed using SPSS version 20. An adjusted odds ratio with a 95% confidence interval and p-value less than 0.05 was used to determine the level of significance.
Results: The proportion of early postnatal care service utilization was 34.3% (95% CI: 29.9%– 38.5%). Mothers’ use of early postnatal care service was predicted by previous early postnatal care use (AOR=2.60, 95% CI: 1.41– 4.77), ANC visit (AOR=0.122, 95% CI:0.059– 0.251), delivery complication (AOR=5.57, 95% CI: 2.85– 10.89), distance (AOR =5.05, 95% CI: 2.45– 10.42), postnatal home visit (AOR=0.21, 95% CI: 0.11– 0.40), awareness on early postnatal care (AOR=16.38 95% CI: 6.23– 43.07), age (AOR=9.34, 95% CI: 1.73– 50.27), (AOR=6.50, 95% CI: 2.29– 18.41), (AOR= 6.23, 95% CI: 2.38– 16.33) and income (AOR=7.97 95% CI: 2.42– 26.26, AOR=3.30 95% CI:1.42– 7.67).
Conclusion: Our study’s finding revealed that the prevalence of early postnatal care service use was low. Early postnatal care service use was significantly associated with previous early postnatal care use, delivery complication, distance, postnatal home visit, number of ANC visits, awareness on early postnatal care use, age, and income.
Keywords: early postnatal care, factors, mothers, Adigrat, Ethiopia
Background
Postnatal care (PNC) is referred to as care given to the mother and her newborn baby immediately after the baby’s birth and for the first 42 days of life. The period from the first 24 hours after birth is referred to as the immediate postnatal period. The period from Days 2 through 7 is defined as the early postnatal care (EPNC), and the period from Days 8 through 42 is the late postnatal period.1
The care given for the first hours, days, and weeks after childbirth is a life-threatening not only for survival but also to the future of mothers and newborn babies because those periods are a critical time for both the mother and the newborn infant. So far, this period receives less attention from health-care providers than the care given to pregnancy and delivery.1,2 Bleeding and infection pose the most significant risk to the mother’s life directly following birth. Whereas preterm birth, asphyxia, and severe infections pose the most significant threat to the newborn.1 Therefore, the Postnatal period needs follow up using the world health organization (WHO) standard contact times.2 Amplified deaths of mothers and newborns in the globe are becoming a persistent public health problem. Half of the postnatal maternal and three-quarters of the newborn deaths occur within the first seven days after childbirth.1,3 Sub-Saharan Africa contributed to more than half of those deaths.4 Ethiopia’s maternal mortality ratio is also high, which is currently estimated at 412 maternal deaths per 100,000 live births.5
Worldwide, only 30% of mothers follow postnatal care, and 13% follow postnatal care in sub-Saharan Africa.6 A study in China shows, 8% of mothers received timely early postnatal care.7 Studies in Uganda and South Sudan also showed that 15.4% and 11.4% of mothers use early postnatal care.8,9 The Ethiopian demographic health survey revealed that 17% of mothers received PNC within the first two days after childbirth.5 Findings from postnatal care studies in North West Ethiopia showed that 30.8% of mothers use postnatal care at 3–7days.10 Different Studies point ed out that, education of mother, occupation of mothers, education of husband, place of delivery, the person conducting delivery and level of knowledge of mother about the need of a postnatal check-up, distance, number of antenatal care visit, household income, awareness of early postnatal care service, length of hospitalization after delivery, the experience of PNC utilization, an appointment given for PNC, delivery complication, mode of delivery were the factors that affect the early postnatal care service use.8,9,11–15 The health of the mother, newborn, and children are among the priorities placed in Ethiopia’s National Health-Care Quality Strategy for 2016–2020 with the motivating goals to reduce the maternal mortality ratio (MMR) from 412 to 199 per 100,000 live births, the neonatal mortality rate (NMR) from 28 to 10 per 1,000 live births and stillbirth rate from 18 to 10 per 1000 births by 2020.16 Hence, this study’s findings, along with other research findings, would contribute to designing effective plans to alleviate determinant factors of postnatal care service utilization. Different stakeholders possibly will also be benefited from this study to give the necessary support to improve the health of childbearing women by the timely use of early postnatal care. It is also intended to assist policy-makers, program managers, educators, and providers in caring for women and newborns after birth. Despite the fact, early PNC service use plays a critical role in reducing maternal and newborn mortality, little is known about its determinants in the region. Our study aimed to determine the prevalence of early postnatal care service use and associated factors among mothers who had given birth in the last 12 months.
Method
Study Design and Area
A community-based cross-sectional study was conducted from March to April 2018 in Adigrat Town Eastern zone of Tigray among 481 mothers who had given birth in the last 12 months. Adigrat town is found 903 km far from the capital of the country Addis Ababa. Adigrat town has 6 Kebeles, 14,443 households. According to the 2007 census population projection, the total population of Adigrat town is 63,548. Out of which 50.8% are females, and 23.5% of them are reproductive-age females. There are one district hospital, two governmental health centers, two private higher clinics, and 351 women development armies. There are about 992 total lists of birth in the town 12 months before the survey.
Sample Size Determination and Sampling Procedure
All Mothers who were randomly selected and who has given birth in the last 12 months before our study was considered source populations. All mothers who gave birth in the previous 12 months preceding the survey and resided in the town for at least six months were included in the study. Mothers who had a mental problem and critically ill during data collection were excluded from this study.
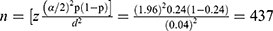
A single population proportion formula was used to get the required sample size based on the following assumption.
Prevalence of early postnatal care (P=0.24).17
Level of confidence=95%.
The margin of error=4.
By adding a 10% non-response rate, the total sample size was becoming 481 mothers.
To get the study participants, first four kebeles were selected by lottery method from the six kebeles in Adigrat town. The number of mothers who gave birth in the past 12 months in each kebele was; kebele 01 (200), kebele 02 (170), kebele 04 (220), kebele06 (150). The total sample size of 481 was distributed proportionate allocation to size to each kebele. Finally, the participants were selected by simple random sampling (Figure 1).
The dependent variable for our study was early postnatal care use. The Independent variables for our study were: Socio-demographic factors include Age, Religion, Ethnicity, Monthly income, marital status, Family size, Occupation, Educational status, partner education, and partner’s occupation; Maternal factors include: Knowledge of mother on the danger sign of post-partumpost-partum, experience on the utilization of early postnatal care, place of delivery, Pregnancy plan, parity, ANC follow up and the number of visits, mode of delivery, and delivery attendant; Health institution related factors include: Access to transportation, distance from the health facility, length of stay at a health facility after delivery, advice by a health professional on early postnatal care after discharge, awareness of postnatal care service.
Operational Definition
Early Postnatal Care
Is defined as healthcare services given after delivery to the end of the first week of delivery for the mothers and newborn babies by health workers.
Early Postnatal Care Use
In this study, mothers who had at least one postnatal care check-up for the current delivery within 2–7 days after delivery in a health facility. The coverage of early postnatal care use was defined as the percentage of mothers and newborns that were visited the health facilities at any time within seven days after delivery and after discharged. The visits were measured by mothers/caretakers words.i.e.by yes or no options for a visit (yes = 1, no = 0).
Knowledge
Knowledge was measured concerning; Knowledge of the mothers about postnatal maternal danger signs, knowledge of the mothers about newborn danger signs, and knowledge of mothers about early postnatal services provided. Knowledge of mothers about obstetric danger signs was measured by the total number of correct answers to 7 items. And knowledge of mothers on the early postnatal service provided was measured by the total number of correct answers to 8 items. Accordingly, two categories were developed for each item. A mother who answers at least two danger signs of post-partum and early postnatal service was labeled as having Good knowledge. A mother who did not answer at least two danger signs of post-partum and early postnatal service provided was labeled as having no knowledge.17,24
Data Collection Procedure and Quality Control
An interviewer-based structured questionnaire was used to collect the data. The questionnaire was developed in English, then translated into the Tigrigna language (the local language of the area), and back to English to ensure its consistency. Additionally, training was given to data collectors and supervisors. A pre-test was conducted on (5%) of the total sample size, then after, a necessary adjustment was made before the questionnaires were used for actual data collection. The data collection procedure was closely supervised, and the collected data were checked for completeness, consistency, and reliability.
Data Processing and Analysis
Data were entered and analyzed using SPSS version 20.0 statistical software package. Descriptive statistics such as frequencies, percentages, means, standard deviations, and crosstabs were computed. In the bivariate logistic regression analysis model, variables with a p-value of less than 0.2526 at binary were taken into multivariable logistic regression. Those variables with a P-value of <0.05 at the final model were considered independent predictors of early postnatal care use. To determine the association between dependent and independent variables, OR with 95% confidence intervals were used. Finally, results were presented using text, tables, and figures.
Result
Socio-Demographic Characteristics versus Early Post Natal Care Service Utilization
From the total 481 study participants, the complete response rate was obtained for 478 (99.4%). The mean age of mothers was 27.9±5.6 years. One hundred sixty-seven mothers (34.9%) were in the age group of 25–29. Out of these, 37.7% of mothers were used early postnatal care services. The majority of the respondents were from the Tigray region and orthodox Christian’s followers; 340 (92%) and 338 (70.7%). According to the study, 83 (17.3%) mothers and 38 (8.1%) husbands were with no formal education, whereas 124 (25.9%) of mothers and 200 (41.8%) of husbands were educated with college and above. Out of those, 15 (18.1%) and 8 (20.5%) of the mothers and husbands with no formal education were used early postnatal care services, whereas 25 (20.2%) and 66 (33.0%) of the mothers and husbands with college and above were used early postnatal care services (Table 1).
 |
Table 1 Socio-Demographic Characteristics versus Early Post Natal Care Service Utilization Among Mothers Who Gave Birth in Adigrat Town, Tigray, Ethiopia, 2018 |
Obstetrics and Reproductive Characters of Mothers versus Utilization of Early Postnatal Care Services
From the interviewed mothers, more than half, 311 (65.1%) of the mothers had no history of abortion. Out of those, 106 (34.1%) of them use early postnatal care service. Three hundred forty-six (72.8%) has more than four antenatal visits, and the rest 129 (27.2%) has less than four times ANC visits. Twenty-four (5%) mothers delivered at home for the current baby, and the rest were offered at the institution. Three hundred fifty-nine (75.1%) of pregnancy conditions were planned and supported for the current baby, and 31 (6.5%) of mothers were unplanned and did not support pregnancy. From those mothers with unplanned an unsupported pregnancy, 16.1% use early postnatal care, whereas 83.9% did not use the service (Table 2).
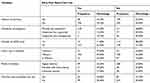 |
Table 2 Obstetrics and Reproductive Characteristics of Mothers versus Early Post Natal Care Service Utilization Among Mothers Who Gave Birth in Adigrat Town, Tigray, Ethiopia, 2018 |
Among the mothers who had complications during pregnancy, 128 (26.8%), (30.2%), 50 (22.3%), 30 (13.3%), 12 (5.3%), 34 (15.1%), 31 (13.8%) complaining of vaginal Bleeding, severe headache, severe abdominal pain, blurred vision, poor fetal movement, and high-grade fever, respectively. From mothers who develop complications after delivery (29.1%), 79 (50%), 39 (24.7%), 40 (25.3%) complained of prolonged labor, fetal distress, pregnancy-induced hypertension, respectively. Ninety-four (19.7%) mothers develop complications following delivery. Among mothers who develop complications majority of 60 (56.6%) immediately went to the health-care facility. And the rest 14 (13.2%), 13 (12.3%), and 19 (17.9%) discuss with traditional birth attendants, consult with traditional healers, and left with no measure, respectively.
Health Institution and Provider-Related Characteristics of Mothers versus Early Postnatal Care Service Utilization
Four hundred forty (92.1%) mothers respond that they have access to transportation from the interviewed mothers. On the other hand, 326 (68.2%) of mothers travel <1-hour distance on foot. Out of those, one hundred eighty (55.2%) were used early postnatal care services. And 152 (31.8%) travel for more than one hour. Out of those, 18 (11.8%) used early postnatal care and the rest 134 (88.2%) did not used the service. Three hundred forty-six (72.4%) and 132 (27.6%) of mothers ever heard and never heard about early postnatal care service, respectively. Out of those who had awareness on EPNC services, majority (29.5%) have information about immunization. The rest 11.5%, 12.8%, 15.1%, 6%, 3.4%, 6.7%, 15% were aware of physical exam for the mother, physical exam for baby, family planning, advice on danger sign of baby and mother, advice on nutrition, advice on hygiene, advice on breast feeding, respectively. From those mothers who have awareness about the service, 155 (44.8%) and 191 (55.2%) mothers were used early postnatal care service, respectively. Four hundred and nineteen (87.7%) of Mothers were appointed for EPNC after discharge. From those appointed mothers majority 231 (48.3%) were appointed six to seven days of post-delivery (Table 3).
 |
Table 3 Health Institution and Provider-Related Characteristics Among Mothers Who Gave Birth in Adigrat Town, Tigray, Ethiopia, 2018 |
Prevalence of Early Post Natal Care
From all the respondents about one hundred sixty four (34.3%) with 95% CI (29.9%-38.5%) of respondents had utilized early postnatal care after discharge from health facilities.
Out of the respondents who did not visit PNC within one week of delivery (21.6%) and (15.9%) were not utilized PNC within one week because of secularism and health-care provider not in good manner, respectively (Figure 2).
Factors to the Use of Early Postnatal Care
In the Bivariate analysis: the number of antenatal care visits, delivery complication, distance, postnatal home visit, previous EPNC, awareness on EPNC, age and income were significantly associated with early postnatal care use at a p-value of <0.25 level. The above variables were taken to multivariable logistic regression analysis.
Accordingly, women who had less than four antenatal care visit were 88% less likely to use early postnatal care than those who had more than four antenatal care visits (AOR (95% CI) 0.122 (0.059–0.251)). Besides, mothers who travel less than one hour distance on foot were five times more likely to use early postnatal care service than those who travel more than one hour (AOR (95% CI) 5.05 (2.45–10.42)). Mothers who have 500–1999 and 4000–6999 monthly household income were seven times and three times more likely to use early postnatal care service than those who had less than 500 monthly income ((AOR=7.97 95% CI (2.42–26.26 and AOR=3.30 95% CI (1.42–7.67)). Those mothers with age group 15–19, 20–24 and 25–29 were 9 and 6 times more likely to use EPNC those mothers with age group of ≥35 years old (AOR=9.34, 95% CI (1.73–50.27), AOR=6.50, 95% CI (2.29–18.41), and AOR= 6.23 95% CI (2.38–16.33)). Moreover, those who had aware of the early postnatal care were sixteen times more likely to use the service than those who had never heard about the service (AOR=16.38 95% CI (6.23–43.07)). Mothers who had previous exposure to EPNC were two times more likely to use EPNC service than those with no previous use (AOR=2.60, 95% CI (1.41–4.77)). Those mothers with postnatal home visits by health-care provider were 79% less likely to use early postnatal care service than those who have no postnatal care home visit (AOR=0.21, 95% CI (0.11–0.40)). Mothers who faced complications during delivery were five times more likely to use EPNC than with no complication (AOR=5.57, 95% CI (2.85–10.89)) (Table 4).
 |
Table 4 Factors Associated with Early Post Natal Care Service Utilization Among Mothers Who Gave Birth in Adigrat Town, Tigray, Ethiopia, 2018 |
Discussion
Our study showed a low coverage of 164 (34.3%) (95% CI; 29.9%–38.5%) of mothers and newborns used early postnatal care service after discharge from health facilities. This confirms that EPNC remains highly neglected and is the weakest of all reproductive, maternal, and child health interventions.1,3
Evidence showed that early postnatal care service use reduces maternal and newborn morbidity and mortality, especially at higher coverage.6 However, our finding showed low percentage of mothers who received EPNC service. Though, Ethiopia’s National Health-Care Quality Strategy for 2016–2020 has motivated goals to reduce the maternal mortality ratio (MMR) from 412 to 199 per 100,000 live births, neonatal mortality rate (NMR) from 28 to 10 per 1,000 live births and stillbirth rate from 18 to 10 per 1000 births by 2020.16 Our study can be an input to policymakers and health-care providers to schedule mothers based on the national postnatal care follow-up protocol to increase postnatal care service utilization.
The number of ANC visits, previous EPNC, delivery complication, distance, postnatal home visit, awareness on EPNC, age, and income had a statistically significant association with the use of early postnatal care service. So, our finding gave emphasis the need to strengthen the use of EPNC by recognizing and addressing the barriers to utilization of the service.
The result of the present study was higher than a finding from EDHS 2016 (17%), a study carried out in South East Ethiopia (23.4%), Studies conducted in northern Ethiopia (19.4%), Addis Ababa Ethiopia and studies conducted in Southwest Ethiopia (5.1%).5,17–19 This difference might be explained by the study time difference that there could be improvement in accessing and utilizing health-care service through time. In addition to the above, Studies conducted in Uganda, Sudan, India and revealed that early postnatal care utilization was 11.4%, 15.4%, 10.1%, and 4.3%, respectively; which were lower as compared to our study.8,9,11,12 The difference in the above might be due to difference in geographical barriers, study setting difference where it was institutional based in where mothers may represent a fearful way of expressing their interest at the health institution in front of care providers where as being community-based study in our study.
The current study is also lower than a study conducted in Debretabour town, North West Ethiopia (30.8%).10 The difference might be due to sample size determination difference. The other suggestion might be due to lack of information about postnatal care and low attention of health-care professionals in counseling the women to come back for postnatal care.
Overall, these findings confirm previous reports9,12,13,23 that health workers in Africa largely advise mothers to return for postnatal care at 6 weeks, a period when maternal and newborn deaths are lower compared to the first 7 days after delivery.25 This study can be implicated to the MOH, regional health bureau and other health-care organizations to create opportunities; suggest practical actions to strengthen PNC at the health facility, through outreach, and in the community, during the early postnatal period.
In our study, respondents were not visited PNC within one week of delivery, majorly because of the practices that keep mothers and babies indoors for the first 7 days – a period of seclusion. This is supported by previous studies.17–21 this might be because of worrying of the mothers about the visitors coming in close contact with newborns. Societies from this study can be therefore, benefited from Understanding of the beliefs and cultural practices that can hinder utilizing early postnatal care service.
In this study, Mothers’ experience of early postnatal care for their previous child had a significant positive association with the use of EPNC service. Similar findings were reported from different studies.11,20 This may be explained by experienced mothers may had a better opportunity to get information and/or advice on the importance of early postnatal care service follow up during previous childbirth from health-care providers. Thus, rigorous efforts are necessary by health-care providers on information and/or advice provision during childbirth of mothers on the importance of early postnatal care service follow up.
We found mothers that accessed the nearest health facility at less than one hour distance on foot had increased use of EPNC. This finding is consistent with previous studies in Ethiopia, Asseco Dembecha, Gondar, and Postnatal care study in China.7,17,20,21 The reason behind may be mothers getting tired and the cultural influence to walk long distances on daytime to health facility. In addition, when health facilities are distant, access to routine maternal health services and emergency care is reduced due to relatively high costs in paying for transport system (when available) and lengthy travel time.8
Early postnatal care service use was also more likely if a mother had awareness about EPNC service. Similar findings were noticed as increased use of EPNC service if a mother had awareness about EPNC service.14,22 This might be due to the reason that awareness can increases the demand for PNC early. Accordingly, it is important to provide health education to post-partumpost-partum mothers before health facility discharge for creating awareness so as to enhance and sustain the use of EPNC services.
Mothers who attended less than four or more ANC visits were less likely to attend early postnatal care service; results are similar to those reported in a study of postnatal care attendance in Nepal.13 Additionally, use of early postnatal care service was higher among women who had experienced problems during their delivery, similar to a prior study in China, Bangladesh and Nepal.7,13,23 This was probably the mothers who had complication at a time of delivery will be consulted by health-care providers’ immediately after delivery and advised on the necessity of EPNC.
Mothers who have between 500–1999 and 4000–6999 monthly household income were more likely to use early postnatal care service. This is supported by a study conducted in Nepal and Debretawer by which mothers from rich families were more likely to report attending postnatal care early.10,13 This might be due to the reason that as economic status of mothers increased mother’s expectation to have early care after delivery increased with their monthly income increment.
Even though it was not stated in other studies, the mother’s age was found to have statistically significant association with utilization of EPNC in our study. Those young mothers (15–19, 20–24, 25–29) were more likely to use EPNC.
Limitation of the Study
The short-term interpersonal relationship that developed between interviewer and interviewee could have created some response bias. Since this is a 1-time measurement of exposure and outcome, it is difficult to derive causal relationships from cross-sectional analysis. Also, as the survey asked the information retrospectively, this may have yielded some recall bias.
Conclusion
The finding of our study revealed that prevalence of early postnatal care service use was low. Number of ANC visit, Previous EPNC, delivery complication, distance, postnatal home visit, awareness on EPNC, age, and income were significantly associated with the use of early PNC. It is better for the MOH and other health development stalk holders to mentor and supervise the health centers activities on MNCH especially PNC service to be provided timely at health institutions as well as at home. Having health education session for those come to MNCH services and educating the community at household level to increase the awareness of community on the important factors that affect mothers to attend timely postnatalpostnatal care especially on secularism. In addition, the District level administrative office should give strong attention to improve transportation service in the study area by connecting kebeles of the district through road construction. Moreover, it is better if The Health professionals and Health extension worker take the opportunities to encourage mothers who attend delivery and ANC on the importance and availability of early PNC services. Additionally, strengthening the service through home visit for those travelling more hours on foot to the nearest health facility, by providing client-oriented service and provide information or advise to the use of early postnatal care service at discharge. Finally, for the Researchers, it will be more valuable if studies will be conducted on this subject matter with alternative study design to find more factors associated with PNC within one-week utilization.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; OR, crude odds ratio; SPSS, Statistical Package for Social Sciences; WHO, World Health Organization; EDHS, Ethiopian Demographic and Health survey; FMOH, Federal Ministry of Health; HEWs, health extension workers; HSDP, health sector development program; IMR, infant mortality rate; LMICs, low and middle income countries; MDGs, millennium development goals; MNCH, maternal, newborn and child health; SBA, skilled birth attendant; SVD, spontaneous vaginal delivery; ANC, antenatal care; PNC, postnatal care; EPNC, early postnatal care.
Data Sharing Statement
The datasets used and analyzed during this study are available from the corresponding author on reasonable request. Data will be available at [email protected].
Ethics Approval and Consent to Participate
An Official letters of cooperation were obtained from Tigray Regional health Bureau and permissions for collection of data were obtained from the local administrators and district health office of Adigrat Town.
The study protocol and Participants under the age of 18 years were approved by the ethics committee of Adigrat University college of Medicine and health sciences (ethics number: AGU/CMHS/091/11). All participants were informed about the purpose of the study, and this study was conducted in accordance with the Declaration of Helsinki.
Before conducting the interviews, information was given to the participants and participants’ voluntary participation, confidentiality, anonymity and freedom to withdraw from the study at any time was assured. As a result consent was obtained from the participants. Finally, written informed consent was obtained from all the participants.
Acknowledgment
First and foremost we thank to almighty God. Second our heartfelt thanks to Adigrat University, for giving us this golden opportunity. Our recognition also goes to data collectors, supervisors, and administrators of Adigrat town who were facilitating the data collection. Finally, we would like to thank the study participants who were willing to take part in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
We have not received any funding for the conducting, manuscript development and publication of this manuscript.
Disclosure
The authors report no conflicts of interest for this work.
References
1. World Health Organization. Technical consultation on postpartum and postnatal care. Swizerland; 2010.
2. World Health Organization. Recommendations on postnatal care of the mother and newborn. 2014.
3. Charlotte W, Pat D, Lalla T, Pyande M Opportunities for Africa’s newborns, postnatal care. 2010.
4. World Health Organization, UNFPA, and The World Bank estimate, Trends in maternal mortality: 1990 to 2010. Swizerland; 2012.
5. Centeral statstics agency. Ethiopia demographic and health survey. Addis Ababa, Ethiopia; 2016.
6. Hailemariam A, Huruy A, Yohannes A. Prevalence and factors associated with post natal care utilization in Abi-Adi Town, Tigray, Ethiopia. Int J Pharma Bio Sci. 2014;8:23–35.
7. Chen L, Qiong W, Van Velthoven MH, et al. Coverage, quality of and barriers to postnatal care in rural Hebei, China: a mixed method study. BMC Pregnancy Childbirth. 2014;14(1):31. doi:10.1186/1471-2393-14-31
8. Izudi J, Akwang GD, Amongin D. Early postnatal care use by post-partumpost-partum mothers in Mundri East County, South Sudan. BMC Health Serv Res. 2017;17(1):442.
9. Nankwanga A. Factors influencing utilisation of postnatal services in Mulago and Mengo hospitals Kampala. Uganda: University of the Western Cape; 2004:10.
10. Wudineh KG, Nigusie AA, Gesese SS, et al. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):508. doi:10.1186/s12884-018-2138-x
11. Berhanu S Assessment of prevalence of postnatal care utilization and associated factors among women who gave birth and attending immunization clinic in selected government health centers in Addis Ababa, Ethiopia, 2015: Addis Ababa University. 2015.
12. Bhaisare KA, Khakase GM. Study of utilization of postnatal care services in tribal area, Maharashtra. Int J Med Sci Public Health. 2014;3(12):1487–1492. doi:10.5455/ijmsph.2014.170920142
13. Dhakal S, Chapman GN, Simkhada PP, et al. Utilisation of postnatal care among rural women in Nepal. BMC Pregnancy Childbirth. 2007;7(1):19. doi:10.1186/1471-2393-7-19
14. Limenih MA, Endale ZM, Dachew BA. Postnatal care service utilization and associated factors among women who gave birth in the last 12 months prior to the study in Debre Markos town, northwestern Ethiopia: a community-based cross-sectional study. Int J Reprod Med. 2016;2016. doi:10.1155/2016/7095352
15. Tumbure A, Argaw D, Fantahun E, et al. Assessment of postnatal care service utilization and associated factors in Asella Town, Arsi Zone, Oromiya Regional State, Ethiopia.
16. World Health Organization. Fewer maternal deaths and stillbirths in Ethiopia: improving quality of care is paying off. Available from: https://www.afro.who.int/news/fewer-maternal-deaths-and-stillbirths-ethiopia-improving-quality-care-paying off 2020: ethiopia.
17. Teklehaymanot A, Niguse D, Tesfay A. Early postnatal care service utilization and associated factors among mothers who gave birth in the last 12 months in Aseko district, Arsi zone, south East Ethiopia in 2016. J Women’s Heal Care. 2017;6:1–12.
18. Gebrehiwot G, Medhanyie AA, Gidey G, Abrha K. Postnatal care utilization among urban women in northern Ethiopia: cross-sectional survey. BMC Women’s Health. 2018;18(1):78. doi:10.1186/s12905-018-0557-5
19. Yarinbab TE, Tona WC. Utilization of postnatal care and its determinants in Loma District, Southwest Ethiopia: a community based cross sectional study. 2017.
20. Tesfahun F, Worku W, Mazengiya F, et al. Knowledge, perception and utilization of postnatal care of mothers in Gondar Zuria District, Ethiopia: a cross-sectional study. Matern Child Health J. 2014;18(10):2341–2351. doi:10.1007/s10995-014-1474-3
21. Hordofa MA, Almaw SS, Berhanu MG, et al. Postnatal care service utilization and associated factors among women in Dembecha District, Northwest Ethiopia. Sci J Public Health. 2015;3(5):686–692. doi:10.11648/j.sjph.20150305.24
22. Mrisho M, Obrist B, Schellenberg D. The use of antenatal and postnatal care: perspectives and experiences of women and health care providers in rural southern Tanzania. BMC Pregnancy Childbirth. 2009;9(1):10. doi:10.1186/1471-2393-9-10
23. Chakraborty N, Islam MA, Chowdhury RI, et al. Utilisation of postnatal care in Bangladesh: evidence from a longitudinal study. Health Soc Care Community. 2002;10(6):492–502. doi:10.1046/j.1365-2524.2002.00389.x
24. Hailu D, Berhe H. Knowledge about obstetric danger signs and associated factors among mothers in Tsegedie District, Tigray Region, Ethiopia: community based cross-sectional study. PLoS One. 2014;9(2):e83459. doi:10.1371/journal.pone.0083459
25. Kerber KJ, de Graft-johnson JE, Bhutta ZA, et al. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007;370(9595):1358–1369. doi:10.1016/S0140-6736(07)61578-5
26. Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3(1):17. doi:10.1186/1751-0473-3-17
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.