Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Prevalence and Associated Factors of Carpal Tunnel Syndrome Among Diabetic Patients in Arba Minch General Hospital, South West Ethiopia, 2021
Authors Bekele A , Abebe G , Hailu T, Fekadu T , Gebremickael A , Getachew T , Churko C , Alelign D , Wassihun B , Teshome D , Bukala Z
Received 3 January 2022
Accepted for publication 12 March 2022
Published 31 March 2022 Volume 2022:15 Pages 983—993
DOI https://doi.org/10.2147/DMSO.S356484
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ming-Hui Zou
Alehegn Bekele,1 Getachew Abebe,1 Tadiwos Hailu,2 Teshale Fekadu,3 Abinet Gebremickael,1 Tamiru Getachew,1 Chuchu Churko,3 Dagninet Alelign,4 Biresaw Wassihun,5 Daniel Teshome,6 Zekarias Bukala1
1Department of Anatomy, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 2Department of Internal Medicine, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 3Department of Public Health, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 4Department of Medical Laboratory, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 5Department of Midwifery, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 6Department of Anatomy, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Alehegn Bekele, Department of Anatomy, Arba Minch University, P.O Box: 21, Arba Minch, Southern Nations, Nationalities and Peoples, Ethiopia, Tel +251921575427, Email [email protected]
Purpose of the Study: This study aimed to assess the prevalence of carpal tunnel syndrome and associated factors among diabetic patients in Arba Minch General Hospital, Southwest Ethiopia. Carpal tunnel syndrome (CTS) is the second most common cause of absence from work which causes functional loss of the hands and leads to disability. However, it is understudied among diabetic patients in Ethiopia.
Patients and Materials: An institution-based cross-sectional study was conducted from May 1 to October 1, 2021. Systematic random sampling method was used to select 353 study participants. CTS-6 Evaluation tool was applied to assess carpal tunnel syndrome. The data was coded and entered into Epi-Data version 3.1 statistical packages and exported to SPSS version 25 for analysis. Binary logistic regression model was applied to assess the association between outcome variable and independent variables. Odds ratio (OR) with 95% CI and p-values < 0.05 were used to identify significantly associated factors with an outcome variable.
Results: The study was conducted among 353 diabetic patients. The cumulative prevalence of carpal tunnel syndrome among diabetes was 3.1%. CTS was statistically significantly associated with high body mass index; AOR=0.34 (0.12, 0.97, 95% CI) (p=0.04. Majority of participants 322 (91.2%) had type 2 DM. Mean fasting blood sugar level ± standard error of study participants was 157.52 ± 1.91 mg/dl.
Conclusion: The prevalence of carpal tunnel syndrome was relatively low. High body mass index (BMI) was significantly but negatively associated with carpal tunnel syndrome compared to diabetic patients with normal BMI. Diabetic patients with normal BMI should be screened for CTS for early management of the disease and prevention of further complications. Further investigations are recommended.
Keywords: diabetes, carpal tunnel syndrome, body mass index, musculoskeletal disorder
Introduction
Diabetes mellitus describes a group of metabolic disorders characterised by high blood glucose levels. Diabetes mellitus is a major public health problem worldwide which is resulting in higher medical care costs, reduced quality of life and increased mortality. The major driver of diabetes costs is the treatment of the related complications. Musculoskeletal complications have been reported in about 36–75% of diabetic patients.1,2
Carpal tunnel syndrome is one of musculoskeletal disorder associated with diabetes next to shoulder capsulitis, Dupuytren’s contracture and limited joint mobility.3 Carpal tunnel syndrome (CTS) is a constellation of symptoms and signs resulting from the compression of the median nerve inside the carpal tunnel at the wrist, which results in functional impairment and local ischemia of the nerve within the tunnel. It is common condition in patients with type 1 and type 2 diabetic patients.4,5
The origin of CTS is often unknown in many cases. Symptoms of CTS include pain, paraesthesia and weakness in the hand, especially in the first three fingers at nights which may travel up the arm toward the shoulder.6
According to the US Bureau of Labor Statistics, there were 16,440 cases of CTS involving lost work days in 2005. It comprised the second most common cause of absence from work.7 A study conducted by Rochester in Minnesota on Conditions associated with carpal tunnel syndrome had estimated that standardized morbidity ratio of Carpal Tunnel Syndrome was 2.3 for diabetes mellitus.8
Studies conducted in United Kingdom, Dhaka, India, Saudi, Moroccan and Gondar, Ethiopia showed the prevalence of carpal tunnel syndrome among diabetes was 20%, 26%, 19.8%. 6.7%, 8.8% and 29.2% respectively.9–14
A study conducted in Turkey on Carpal tunnel syndrome and metabolic syndrome had shown that CTS was commonly associated with conditions such as obesity, diabetes mellitus, smoking, overuse-type injuries caused by repetitive motion, pregnancy, hormonal replacement therapy and corticosteroid use.15,16 According to a cross-sectional study conducted at the National Center for Diabetes, Endocrinology and Genetics in Amman, Jordan, female gender, old age, duration of diabetes, hypertension were significantly associated with hand disorders in T2DM (2).
But the issue of CTS is understudied in Ethiopia particularly regarding the prevalence of carpal tunnel syndrome among diabetes and its determinants. So, this study aimed to assess the prevalence of carpal tunnel syndrome and its associated factors among diabetic patients.
Methods
Study Area and Period
This study was conducted at Arba Minch General Hospital, Southern Ethiopia. Arba Minch town is the capital city of Gamo zone. The town is located at a distance of 275 Km and 505 km from the regional city, Hawassa and the country capital city, Addis Ababa respectively.
Arba Minch General Hospital serves approximately two million people and provides services such as outpatient treatment, inpatient, emergency, ophthalmic, dental, obstetrics and gynecology with different diagnostic modalities. It also provides chronic disease follow-up services, which include routine diabetics and hypertension case follow up. This study was conducted from May 1 to October 1, 2021.
Study Design
Institutional based cross-sectional study design was applied.
Population
The source populations of the study were all diabetic patients who have follow up at diabetic clinic of Arba Minch General Hospital and the study populations were all selected diabetics patient who have follow up at diabetic clinic during data collection period and met inclusion criteria. All diabetic patients who have had routine follow up for 6 months and above at Diabetes Clinic of Arba Minch General Hospital were included in the study. However, DM patients whose age was less than 18 years, patients with a history of hand trauma, epilepsy, chronic liver disease, family history of DC, recent fracture or injuries, patients who had comorbidities that can cause similar symptoms with CTS, like lesion in the CNS, cervical region, ulnar nerve, or radial nerve and patients previously undergone surgery to the shoulder and non-conscious subjects were excluded.
Sample Size Determination and Sampling Procedure
Sample Size Determination
The sample size was determined using single population proportion statistical formula at 95% of confidence interval with prevalence of carpal tunnel syndrome, (p= 29.2%) and d=5%.14 After adding 10% non-response rate; the final sample size was 353.
Sampling Technique and Procedure
Study subjects were selected by using systematic random sampling technique. Initially, there were 800 diabetic patients who have had chronic diseases follow up of 6 months and above at Arba Minch Hospital. Fortunately, all of (800) diabetic patients fulfilled the inclusion criteria of the study. Due to budget or resource constraint we have been facing, we randomly selected 353 study subjects using systematic random sampling interval formula;
K=N/n=800/353 =2.3 =2, where “K” is an interval of random selection of study samples; “N” is source of population, which the study samples drawn from and “n” is the calculated sample size for this study. As a result, study subjects were selected at every second interval of patients coming to diabetic clinic for follow up. The first study participant was selected randomly by lottery method.
Variables
Dependent Variable
Carpal tunnel syndrome (yes or no)
Independent Variables
- Socio demographic: Age, sex, occupation, residence, religion, education.
- Diabetic related factors: Type of diabetes, duration of DM, FBS, type of medication/therapy.
- Other factors: Cardiovascular illness, body mass index (BMI), physical exercise.
Data collection tools and procedures
Semi-structured questionnaire, checklist and CTS-6 Evaluation tool were used to collect data. CTS-6 Evaluation tool was used to assess carpal tunnel syndrome which was confirmed by a trained physician. The CTS tool contains two components such as symptoms and history of CTS and physical examination sections. These were scored out of 26 total points. Patients with total score >12/26 without comorbidities that can cause similar symptoms with CTS were considered as positive for carpal tunnel syndrome.22 Socio-demographic data and physical exercise status of all study participants were collected using interviewer administered questionnaire Document review of every study participant was also done to collect data related to concomitant disease and diabetic related conditions like medication type, duration of DM and type of DM. One BSC nurses, two laboratory technicians, one health officer, and a physician were recruited for data collection.
After we got consent from study participants for laboratory measurements, the laboratory technician has drawn three rounds of 5mL blood after overnight fasting of 8–10 hour for determination of FBS; then average FBS was taken. Lipid panel (Total cholesterol, HDL-c and Triglyceride) was also determined. Sample was collected by an experienced laboratory technician. Laboratory analysis was carried out by senior laboratory technician.
Measurement
Weight was measured using WHO standard weighing scale at precision of 0.1 kg with study subjects dressed light clothes. Height was measured using stadiometer in centimeters in erect position at precision of 0.1 cm without shoe. Then BMI was calculated by the formula; mass (kg)/height2 (m).
Data Quality Control
Two day intensive training was given for data collectors on the data collection tool and how to review documents. An internist was assigned as a supervisor. The collected data was repeatedly entered into Epi data software version 3.1. With two data clerks independently and the investigator checked consistency between the two data sets. Pretest was done among 5% sample size at Jinka hospital to test the consistency of the questionnaire and checklist.
Operational Definitions
Carpal tunnel syndrome positive; are patients who scored >12/26 for CTS-6 evaluation tool and without comorbidities that can cause similar symptoms with CTS.22
- Body Mass Index –was assessed according to WHO (2020) standard that describe underweight (when BMI is <18.49 kg/m2), normal body weight (when BMI is 18.5–24.9 kg/m2), Pre-obesity (when BMI of 25–30 kg/m 2), and obesity (when BMI ≥30 kg/m 2).
Data Processing Analysis Procedures
The collected data was checked for its completeness, coded and entered into Epi-Data version 3.1 statistical packages then exported to SPSS version 20 for further analysis. Inconsistent values were double checked against the filled data extract format and corrected as necessary. Bivariate logistic regression analysis was applied to determine independent variables associated with CTS. Independent variables which were found to have association with CTS with p-value <0.25 and/or variables showed association with CTS in previous studies were transferred to multivariable logistic regression to control for the effect of confounders. Finally, significantly associated independent variables at p-values < 0.05 were identified based on the adjusted odds ratio (AOR), with 95% CI.
Ethical Consideration
Ethical clearance was obtained from Institutional Ethics Review Board of college of medicine and health sciences; Arba Minch University. This ethical clearance and support letter was submitted to selected hospitals.
Study participants were informed about the purpose of the study. Verbal consent was obtained from each study subjects before collection of blood samples and other relevant clinical information. Study participants were recruited only based on their consent and the inclusion and exclusion criteria apart from any form of discrimination. Security and confidentiality of detail clinical and laboratory finding data was kept carefully by using code for identification. The study complies with the Declaration of Helsinki.
The participants were ensured to be free from any coercion, under inducement, influence or intimidation. The only potential risk was a little pain due to vein puncture and consumption of time of participant during the data collection. The participants have had the right to withdraw from the study whenever they feel inconveniences.
The results of participants with CTS were linked to the attending physician for appropriate treatment and management. The leftover sample of the participants was decontaminated and disposed according to waste disposal protocol of respective laboratories immediately after investigation of the research parameters.
Result
Socio-Demographic Characteristics
Data was collected from 353 study subjects; of which 195 (55.2%) were female. The mean age (± standard deviation) of study subjects was 51.34 (± 14.07) years. Most of the participants; 227 (64.3%) were urban dwellers and 113 (32.0%) of participants did not have completed formal education. The majority of the study subjects; 146 (41.4%) were house wives (Table 1).
DM Related and BMI Characteristics of Study Participants
Almost majority of study participants; 322 (91.2%) had type 2 DM. The mean duration of diagnosis for diabetes was 4 (± 4.95) years. 289 (81.9%) of these study participants have less than 10 years of duration since diagnosed with DM. The mean fasting blood sugar (FBS) (± standard error) of study participants was 157.52 (± 1.91) mg/dl; 276 (78.2%) of subjects have FBS leve l ≥130 mm/dl, which implies that more than two-third of subjects have uncontrolled serum glucose (Table 2).
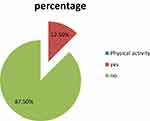
More than two-third; (75.9%) of the study subjects were using oral hypoglycemic medications followed by insulin; 59 (16.7%) and combined (oral hypoglycemic medications and insulin) 25 (7.1%). Out of the total study subjects; 82 (23.2%) had diagnosed with cardiovascular complications. More than half of study participants 187 (53.0%) were overweight (Figure 1).
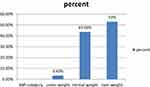 |
Figure 1 BMI category of study subjects for prevalence and associated factors of carpel tunnel syndrome among diabetic patients on follow-up in Arba Minch General Hospital, Southwest, Ethiopia, 2021. |
Most of study participants 309 (87.5%) have not physical exercise of 15 minute or more a day per one week (Figure 2). Approximately all subjects 349 (98.9%) were right hand dominant.
Prevalence of Carpal Tunnel Syndrome in the Study Participants
The overall cumulative prevalence of carpal tunnel syndrome among study participants was 3.1%. CTS was prevalent among type 2 diabetic patients 11 (3.1%). The age specific prevalence of CTS was noted in age group of forty five years and above 7 (1.9%).
The prevalence of CTS was 2.5%, 2.2%, 1.9% and 1.6% among study participants with less than 10 year duration of DM diagnosis, female, serum FBS level greater than 130mg/dl and house wives respectively (Table 2).
All independent variables in this study were included in a bivariate logistic regression analysis model and they were tested for their crude association with CTS. Sex, age, educational status, duration of diabetes illness and FBS level were associated with Carpal tunnel syndrome in the previous studies and high BMI showed crude association with Carpal tunnel syndrome at (p<0.25). However, among these variables included into multivariate logistic regression analysis, high BMI was statistically significantly associated with CTS; (p<0.04); AOR=0.34 (0.12, 0.97, 95% CI) (Table 3).
Discussion
Diabetes mellitus has been linked to a variety of musculoskeletal disorders. These disorders have paid less attention mostly, yet they could be marker of severe micro vascular complications.2
The carpal tunnel syndrome is one of the major problems in diabetes mellitus characterized by paresthesia, pain, and burning sensation over the median nerve cutaneous distribution of the thumb, index, middle, and lateral half of the ring fingers, which is often worse at night and relieved by hanging the arm down or shaking the hand.17 Swelling within the carpal tunnel can cause compression of the median nerve and resultant inflammation causes further nerve compression. Carpal tunnel syndrome is one of the most frequent entrapment neuropathies of the upper limb.10 The clinical carpal tunnel syndrome-6 (CTS-6) diagnostic tool was used in this study.
According to this study, the prevalence of carpal tunnel syndrome among diabetic patients was 3.1%. This result is lower than studies conducted in Amman, Jordan and Iran which included 1000 patients with T2DM (5.5%) (2) and 432 diabetic patients (8.56%)18 respectively. These variations might be due to large number of sample sizes used in the previous study could increase the prevalence of CTS as compared to the current one which has included 352 diabetic patients.
Similarly other studies conducted in United Kingdom, Saudi Arabia, India, Bangladesh and Ethiopia among 96,252,106,354 and 301 diabetic patients respectively, the prevalence of CTS was (20%),(6.7%),((19.8%),(26%) and (29.2%) respectively9–12,14. All these results showed a higher prevalence than the current study prevalence. These variations might be due to the CTS evaluation tools or diagnostic criteria used in this study might underestimate the prevalence of CTS. The genetic variations and life style differences among peoples of Ethiopia and these nations might be also the possible cause of variation.
In contrast, the prevalence of CTS in this study was higher than studies conducted in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia (1%).3 This variation might be due to use of the less specific diagnostic tests (Tinel’s or Phalen’s sign) of CTS in the previous study may under estimate the prevalence of CTS.
According to the current study finding, high BMI was significantly but negatively associated with carpal tunnel syndrome among diabetes. This finding is in contrast with a study conducted in Bangladesh among 354 diabetes which showed that BMI was significantly (p < 0.05) positively associated with CTS10 and a study conducted in Italy among 117 CTS cases found a close positive association between BMI and CTS (p = 0.005).19 These differences possibly might be due the clinical diagnostic tool used in the current study may fail to diagnose CTS cases among subjects with normal BMI might results this associations. Moreover, study subjects of this study lies in the age range of 45 years and above, who might be vulnerable to degeneration of carpal ligaments; this may causes compression and entrapments of median nerve. This might cause the CTS among patients with normal BMI. However, it needs further investigations.
In contrast to the present study finding, another case control study conducted on 514 patients who underwent a carpal tunnel release procedure also showed that CTS was significantly high among patients who were obese (p = 0.02; odds ratio, 1.77).20 This might be due to the fact that the previous study might have included large number of obese patients with CTS. Moreover, this association might occur due to diagnosis tool used in this study might underestimate CTS cases among obese patients.
Another large scale study in UK showed that obesity (OR = 2.06) was a risk factor associated with CTS21 which contradicts the present study. These might be due to the previous study has included 3391 confirmed CTS cases of which 72% were women this might increase the frequency of obese subjects with CTS. In contrast to present study, a study in India among 106 DM patients also showed that BMI was not associated with CTS.11 This difference might be due to small sample sizes used in the previous study, which may alter the frequency of occurrence of the case (CTS) with respect to predictor variable (BMI).
The present study finding does not showed any association between CTS and age, sex and duration of DM. In contrast to this finding, a study conducted in Iran among 432 diabetic patients showed that CTS was significantly associated with advanced age (p<0.032, female sex (p<0.002) and duration of DM (p<0.007)18. These differences might be due to high sample sizes used in the previous study.
Besides, a similar study showed that CTS was significantly associated with poor glycemic control at p<0.0003,18 which opposes the current study, which might be due to large sample size used in the previous study compared to the current.
However, in line with the present study, a study conducted in India showed that duration of DM was not associated with CTS (p=0.13).11 These similarities might be due to average duration of DM among most of the study subjects in both studies ranges from 5 to 10 years; when the CTS might be at its asymptomatic stage in these study subjects.
According to studies conducted in Gondar, Ethiopia among 301 subjects with DM and Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia, sex of male (p<0.05), type 1 DM (p=0.009), and greater than 10 years duration of diabetes showed significant association with musculoskeletal disorders among diabetic patients3,14 which contradicts the current study finding showing that all these variables did not show any association with CTS. All of the variations might be due to the fact that the previous studies have included all musculoskeletal disorders as outcome variables so that the association between CTS and risk factors may be affected by other outcome variables.
Besides almost all study subjects in the current study were type 2 diabetes unlike the two previous studies and the proportion of study subjects who have greater than 10 years duration of diabetes were low in the current study.
Limitations of the Study
- This study was limited to use clinical diagnosis method of CTS which did not included electrophysiological confirmatory diagnosis method of CTS due to unavailability of the test in the study area.
- This study does not show cause-and-effect relationship between BMI and CTS.
- Resource or budget constraints.
- Diagnostic tool related bias.
Conclusion
The prevalence of carpal tunnel syndrome among diabetic patients was low. High body mass index (BMI) was significantly but negatively associated with Carpal tunnel syndrome compared to diabetic patients with normal BMI. So, high BMI was associated with a less likelihood of developing carpal tunnel syndrome among diabetic patients in this study. This implies diabetic patients with normal BMI are likely to be affected by CTS. So that they should be screened for CTS in routine diabetic follow ups to identify patients at high risk of developing CTS for early management and prevention of further complications. Further investigations are needed to see the relationship between CTS and BMI.
Ethical Approval
The study complies with the Declaration of Helsinki and it was approved by the Institutional Ethics Review Board of Arba Minch University. The study participants were informed about the purpose of the study and informed verbal consent for participation and blood sample donation was obtained from study subjects before commencement of the study.
Acknowledgments
The authors highly appreciate Arba Minch University for funding. All co-investigators are deserved great thanks for their valuable and critical revision of the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Arba Minch University.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Cho N, Shaw JE, Karuranga S, et al. Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi:10.1016/j.diabres.2018.02.023
2. Mustafa KN, Khader YS, Bsoul AK, Ajlouni K. Musculoskeletal disorders of the hand in type 2 diabetes mellitus: prevalence and its associated factors. Int J Rheum Dis. 2016;19(7):730–735. doi:10.1111/1756-185X.12617
3. Wamisho BL, Feleke Y. Epidemiology and clinical profile of common musculoskeletal diseases in patients with diabetes mellitus at Tikur Anbessa Specialized Hospital in Addis Ababa, Ethiopia. East Cent Afr J Surg. 2017;22(2):49–62. doi:10.4314/ecajs.v22i2.6
4. Alotaibi SN, Alqahtani SS, Alammar RM, et al. The prevalence and patterns of carpal tunnel syndrome and their associated risk factors among diabetic population in South-West of Kingdom of Saudi Arabia. Egypt J Hosp Med. 2018;7(70):1152–1158. doi:10.12816/0044542
5. Perkins BA, Olaleye D, Bril V. Carpal tunnel syndrome in patients with diabetic polyneuropathy. Diabetes Care. 2002;25(3):565–569. doi:10.2337/diacare.25.3.565
6. Oktayoglu P, Nas K, Kilinç F, Tasdemir N, Bozkurt M, Yildiz I. Assessment of the presence of carpal tunnel syndrome in patients with diabetes mellitus, hypothyroidism and acromegaly. J Clin Diagnostic Res. 2015;9(6):OC14. doi:10.7860/JCDR/2015/13149.6101
7. Sharief F, Kanmani J, Kumar S. Risk factors, symptom severity and functional status among patients with carpel tunnel syndrome. Neurol India. 2018;66(3):743. doi:10.4103/0028-3886.232351
8. Stevens J, Beard C, O’fallon W, Kurland L. Conditions associated with carpal tunnel syndrome. Mayo Clin Proc. 1992;67(6):541–548. doi:10.1016/S0025-6196(12)60461-3
9. Ramchurn N, Mashamba C, Leitch E, et al. Upper limb musculoskeletal abnormalities and poor metabolic control in diabetes. Eur J Intern Med. 2009;20(7):718–721. doi:10.1016/j.ejim.2009.08.001
10. Islam MR, Rahman T, Islam RN, et al. Frequency of carpal tunnel syndrome in patients having diabetes mellitus with neuropathy in a tertiary care hospital of Bangladesh. BIRDEM Med J. 2018;8(3):240. doi:10.3329/birdem.v8i3.38131
11. Paranthakan C, Govindarajan P. A study on carpal tunnel syndrome among diabetes patients in tertiary care hospital. Int J Community Med Public Health. 2016;3:805–807.
12. Attar SM. Musculoskeletal manifestations in diabetic patients at a tertiary center. Libyan J Med. 2012;7(1):19162. doi:10.3402/ljm.v7i0.19162
13. Majjad A, Errahali Y, Toufik H, et al. Musculoskeletal disorders in patients with diabetes mellitus: a cross-sectional study. Int J Rheumatol. 2018;2018. doi:10.1155/2018/3839872
14. Fasika S, Abebe SM, Kebede AG. The prevalence of shoulder and hand complications and associated factors among diabetic patients at University of Gondar Teaching Referral Hospital in Northwest Ethiopia. Age. 2013;4(12):13–14.
15. Yurdakul FG, Bodur H, Çakmak ÖÖ, et al. On the severity of carpal tunnel syndrome: diabetes or metabolic syndrome. J Clin Neurol. 2015;11(3):234–240. doi:10.3988/jcn.2015.11.3.234
16. Balci K, Utku U. Carpal tunnel syndrome and metabolic syndrome. Acta Neurol Scand. 2007;116(2):113–117. doi:10.1111/j.1600-0404.2007.00797.x
17. Papanas N, Maltezos E. The diabetic hand: a forgotten complication? J Diabetes Complications. 2010;24(3):154–162. doi:10.1016/j.jdiacomp.2008.12.009
18. Kiani J, Goharifar H, Moghimbeigi A, Azizkhani H. Prevalence and risk factors of five most common upper extremity disorders in diabetics. J Res Health Sci. 2014;14(1):93–96.
19. Plastino M, Fava A, Carmela C, et al. Insulin resistance increases risk of carpal tunnel syndrome: a case‐control study. J Peripher Nerv Syst. 2011;16(3):186–190. doi:10.1111/j.1529-8027.2011.00344.x
20. Karpitskaya Y, Novak CB, Mackinnon SE. Prevalence of smoking, obesity, diabetes mellitus, and thyroid disease in patients with carpal tunnel syndrome. Ann Plast Surg. 2002;48(3):269–273. doi:10.1097/00000637-200203000-00007
21. Geoghegan JM, Clark DI, Bainbridge LC, Smith C, Hubbard R. Risk factors in carpal tunnel syndrome. J Hand Surg. 2004;29(4):315–320. doi:10.1016/J.JHSB.2004.02.009
22. Powar RS, Mahapure KS. Accuracy of quick-DASH tool versus CTS-6 tool in evaluating the outcome of carpal tunnel release. Eur J Plast Surg. 2021;16:1–6.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.