Back to Journals » International Journal of General Medicine » Volume 15
Prevalence and Associated Factors of Anemia Among Newborns at Tibebe Ghion Specialized Hospital, Northwest Ethiopia
Authors Alamneh TT, Tilahun SF, Beyne MB, Fekadu SA , Assem AS , Kassa SF
Received 15 March 2022
Accepted for publication 2 August 2022
Published 6 August 2022 Volume 2022:15 Pages 6465—6474
DOI https://doi.org/10.2147/IJGM.S365817
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Tazebew Tilahun Alamneh,1 Shitahun Fente Tilahun,2 Melkamu Bedimo Beyne,3 Sofonias Addis Fekadu,4 Abel Sinshaw Assem,4 Selam Fisiha Kassa5
1Department of Pediatrics and Child Health, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Pediatrics and Child Health, School of Medicine, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia; 3Department of Biostatistics and Epidemiology, Bahir Dar University, Bahir Dar, Ethiopia; 4Department of Optometry, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 5Department of Pediatrics and Child Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Abel Sinshaw Assem, Email [email protected]
Introduction: Anemia is a common hematological problem in neonatal admissions. Poor detection rate and inappropriate treatment adversely affect the growing infant. Data on the magnitude and risk factors of anemia in sick newborns are lacking in Ethiopia, so knowing the prevalence and risk factors may reduce the long-term untreated complications of anemia.
Objective: The overall aim of this study was to assess the prevalence and associated factors of anemia among newborns admitted to Tibebe Ghion specialized hospital.
Methods: A hospital-based cross-sectional study was conducted among 272 newborns admitted to Tibebe Ghion Specialized Hospital from February 1 to May 30, 2021. A pretested structured questionnaire containing socio-demographic, clinical, and laboratory parameters was used for the data collection. Data were collected by trained nurses and residents after obtaining ethical clearance. The data were entered through Epi-data version 4.6 and analyzed using SPSS version 23.0 computer software. Descriptive statistics were performed using frequency, mean and standard deviation. Bivariable and multivariable binary logistic regressions were done to identify risk factors of anemia. Adjusted odds ratio with 95% confidence interval at a p-value < 0.05 was declared as a statistically significant variable in the multivariable logistic regression.
Results: About two-thirds 177 (65.1%) of the newborn babies were male and 152 (55.9%) of the newborn had a birth weight of ≥ 2500 grams. The most commonly diagnosed medical conditions were sepsis 218 (80.1%) and prematurity of birth 78 (28.7%). The prevalence of anemia among newborns in this study was 63 (23.2%) [19.1– 28.7%]. Gestational age of 33– 36 weeks (AOR=0.36: 95% CI=0.17– 0.96) and maternal anemia (AOR=3.81: 95% CI=1.29– 11.23) were significantly associated with newborn anemia.
Conclusion: The prevalence of anemia among newborns in Tibebe Ghion specialized hospital was high. Gestational age and maternal anemia were significantly associated with newborn anemia. So, it is better to properly educate and advise women about newborn anemia during antenatal care follow-up.
Keywords: newborns, anemia, associated factors, Tibebe Gion
Introduction
Anemia is defined as the level of hematocrit (HCT) below 2 standard deviations measured for the respective age and sex of a child.1,2 In the newborn period, it has different pictures based on the gestational age and postnatal age variations of blood counts.3 During the newborn period, the top three causes of anemia are blood loss, decreased red blood cell production, and increased destruction of red blood cells.4–6 These mechanisms can be compounded by the birth weight and gestational age of the newborn.7,8 Clinical manifestations of anemia include poor feeding, fast breathing, paleness, and change in mental status to the extent of poor systemic tissue perfusion.1,3,9,10 The complication of untreated anemia in newborns involves tissue hypoxia, stunted growth, chronic heart failure, infectious diseases including HIV AIDS, and hepatitis secondary to repeated blood product transfusions.11
The global prevalence of anemia in under-five children was 41.7%, whereas in the Africa region was 59%.12 In sub-Saharan Africa, including Ethiopia, the national prevalence of anemia among children under five was above 40%.13 According to the Ethiopian Demographic Health Survey 2016 the prevalence of anemia among 6–59 months of children was 56%.13
Neonatal anemia is a common problem in developing countries whereby there are poor antenatal care and also due to different factors. The practice of antenatal follow-up in developing countries is not well established which may result in maternal anemia and finally end up with possible neonatal anemia. Possible contributing factors of neonatal anemia are prematurity, low birth weight, maternal anemia, and other neonatal medical problems including external blood loss.10,14,15 Newborn anemia is a serious public health issue which causes infant mortality and morbidity in early neonatal life.2 Unless identified earlier and treated properly, anemia can cause physical, mental, and other public health problems in developing infants or can cause death in newborns.
While anemia is a common neonatal problem encountered among newborns, there are limited studies regarding the prevalence and associated factors of newborn anemia generally in Ethiopia and specifically in the study area. Therefore, this study aimed to assess the prevalence and associated factors of anemia among newborns at Tibebe Ghion Specialized Hospital, Northwest Ethiopia.
Methods and Material
Study Design and Period
A hospital-based cross-sectional study was conducted on newborns admitted to Tibebe Ghion Specialized Hospital (TGSH) from February 1 to May 30, 2021.
Study Area
The study was conducted at TGSH, which is located in the northwest part of Ethiopia, 560 km away from Addis Ababa in Amhara Regional State Government capital city of Bahir Dar. It is a tertiary referral hospital and one of the biggest health institutions in Ethiopia providing different health care services including pediatrics and child health. The neonatal intensive care unit ward in TGSH has separate compartments for preterm and term newborns. The ward is equipped with phototherapy machines and incubators. The health care for the newborn at the hospital is provided with structured services involving interns, residents, and senior physicians along with the nursing staff.
Source and Study Population
All newborns admitted to Tibebe Ghion Specialized Hospital were the source population, whereas newborns admitted to TGSH during the data collection period were the study population of this study.
Inclusion and Exclusion Criteria
All newborns were born after ≥28 weeks gestational age and neonates ≤28 days and who were admitted to TGSH during the study period. However, those newborns who have lethal congenital anomalies were excluded from the study.
Sample Size and Sampling Technique
Sample Size Determination
The required minimum sample size was calculated using the single population proportion formula. By taking the prevalence of anemia among newborns 50%, 5% margin of error, and 95% confidence interval (CI)=1.96; the sample size was determined to be 384. Since the source population is <10,000, we used a correction formula calculation. After adjusted with correction formula and adding 5% non-response rate, the final sample size becomes 272.
Sampling Technique and Procedure
In the 4 months of admissions, a systematic random sampling technique based on registration numbers was used to select the study participants. A systematic random sampling technique based on Medical Registration Number (MRN) is employed to select the study participants. The estimated number of admissions was about 175 per month, which was about 700 newborns over the study period. The sampling interval (K) was determined by dividing the total admissions over 4 months for the sample size resulting in every 3rd newborn, and when the selected newborn was excluded the next order MRN was substituted.
Study Variables
Dependent Variable
Anemia
Independent Variables
Socio-demographic characteristics: Postnatal age, maternal age, sex, gestational age, residence, educational status; Medical conditions: Sepsis, asphyxia, jaundice, HDM, birth weight, blood loss, DIC; Obstetrical variables: Parity, BG/RH, ANC follow-up, iron supplement, bleeding, mode of delivery, hypertension, any current illness.
Data Collection Tools and Procedure
The data were collected by using a structured interviewer-administered questionnaire prepared in English and translated to the local language (Amharic) and back to English to check for consistency. The data were collected by pediatrics residents and ward nurses after taking training about the purpose of the study and data collection instruments. Neonatal HCT and hemoglobin were obtained from the first complete blood count ordered by the treating physician and nurses. A maternal chart was also used to collect information regarding the mother’s medical and socio-demographic history. The data were collected using a systematic random method based on the order in which they get registered every third interval. It was collected with a pretested questionnaire having four parts, newborn characteristics, and the second on maternal socio-demographic characteristics, the third on maternal obstetric and medical complications, and the last on newborn’s medical conditions.
Data Quality Control
The training was given to the data collector and supervisor for one day. Pretest was done among 5% of the sample size at Felege Hiwot referral hospital, and necessary modifications were made accordingly. The principal investigator also supervises the data collection throughout the data collection period.
Data Analysis
The collected data were coded and checked for completeness and entered into epi-data version 4.6 and exported to SPSS version 23.0 for analysis. Descriptive statistics like frequency, mean and median were used to describe the data. The binary logistic regression method was fitted to identify factors associated with newborn anemia among newborns admitted to TGSH.
The effect of independent variables on the outcome variable was analyzed using binary logistic regression analysis. Multivariable logistic regression was done on all variables that had a p-value <0.2 in the bivariable logistic regression by using the enter method. Hosmer–Lemeshow goodness-of-fit tests was used to check model fitness. The strength and direction of association were determined by using an adjusted odds ratio (AOR) with a 95% level of significance. Variables that had a p-value of <0.05 in the multivariable logistic regression were taken as a significant risk factor for newborn anemia.
Ethical Considerations
Ethical clearance was obtained from Bahir Dar University School of Medicine's ethical review committee with a protocol number of 005/2020 following the declaration of Helsinki. Letter of the permission was also obtained from the Department of Pediatrics and Child Health. Written informed consent was obtained from the newborn mothers after clearly explaining the purpose of the research and participation was based on willingness, and the name was not mentioned to maintain confidentiality.
Result
Socio-Demographic and Clinical Characteristics of the Study Participants
A total of 272 newborns were included in this study with an average age of 14 hours. Nearly two-thirds 177 (65.1%) of the study subjects were males and more than half 155 (57.0%) of them had a gestational age of ≥37 weeks. The mean pulse rate and respiratory rate of the newborns were 145.45± 14.13 and 54.08± 13.6, respectively. The median HCT value of the newborn was 46.1% with IQR of [37.9–51.0%] whereas the median value of Platelet and MCV were 178.5 and 103 with IQR of [117–248] and [97–108], respectively (Table 1).
 |
Table 1 Socio-Demographic and Clinical Parameters of the Study Participants in TGSH, Northwest Ethiopia, 2021 |
Maternal Socio-Demographic and Clinical Characteristics
The mean age of the mothers in this study was 27.35 ± 5.05 years. The majority of the mothers 158 (58.1%) of the study participants were housewives in occupation and only 79 (29%) of them were in the age group of greater than 30 years. On the other side, 92 (33.9%) of the mothers had developed an obstetrical complication. The mean maternal hematocrit value was 37.26% ±3.85% (Table 2).
 |
Table 2 Maternal Socio-Demographic and Clinical Characteristics of the Study Participants in TGSH, Northwest Ethiopia, 2021 |
Physical Examination and Medical Diagnosis of the Newborns
The most commonly encountered clinical findings were gross pale and gross jaundice, which were encountered in 49 (18%) and 50 (18.4%) study subjects, respectively. The most widely diagnosed medical conditions were sepsis and prematurity of birth which accounts for 218 (80.1%) and 78 (28.7%) study subjects, respectively.
Prevalence of Anemia Among Newborns
The mean hemoglobin value of the neonate was 15.75g/dl ± 3.54 with a minimum and maximum value of 3.3g/dl and 22.5g/dl, respectively. The prevalence of anemia among newborns in this study was 63 (23.2%) with a Confidence interval of [19.1–28.7%] (Figure 1).
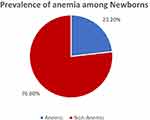 |
Figure 1 Prevalence of anemia among Newborns in TGSH, Northwest Ethiopia, 2021. |
Factors Associated with Anemia Among Newborns
In the multivariable binary regression, gestational age and maternal anemia were significantly associated with anemia in newborn babies.
Newborn babies with a gestational age of 33–36 weeks are 64% less likely to develop anemia as compared to newborns with a gestational age of ≤32 weeks. The odds of being anemic among neonates born from anemic mothers are 3.81 times higher as compared to those newborns born from a non-anemic mother (Table 3).
 |
Table 3 Bivariable and Multivariable Binary Logistic Regression Analysis for Factors of Anemia Among Newborns at TGSH, Northwest Ethiopia, 2021 |
Discussion
In the neonatal period anemia is a complex problem owing to the unique blood picture. Therefore, the present study aimed to assess the prevalence and associated factors of anemia among newborn babies at Tibebe Ghion Specialized Hospital. The prevalence of anemia among newborns in TGSH, northwest Ethiopia was 63 (23.2%) with a confidence interval of [19.1–28.7%].
The finding of the present study is similar to a study done in Gondar Ethiopia,16 New York,17 and Netherland18 which was reported as 25%, 21%, and 21%, respectively. This similarity might be due to the consistency of operationalizing the anemic level of the neonates and the cutoff point of the hemoglobin level of the newborn babies. Like in our study, the study mentioned in the above categorized newborn anemia is below the level of hemoglobin finding of 13g/dl.
However, the prevalence of anemia among newborns in this study is higher as compared to studies done in the USA,15 Nepal,19 Iran,20 and Addis Ababa Ethiopia21 which was reported as 14%, 5.7%, 11.7%, and 9%, respectively. These differences could be attributed to the differentials in socioeconomic conditions and variations in the clinical characteristics of the study participants. Another possible reason for this discrepancy might be due to sample size variations. In this study, 272 study participants were included, whereas a study from Addis Ababa was conducted among 89 study participants.
On the contrary, the prevalence of newborn anemia in this study is lower as compared to studies done in Brazil 32.6%,22 India 39%,11 79.3%,23 Iran 53%,24 Ghana 57.3%,25 Benin 61.1%,26 Ethiopia 29.1%.27 The possible difference from the Benin study might be attributed to the Benin study included newborns delivered from malaria-infected mothers only, whereas in the present study newborns delivered from malaria-free mothers were also included in the study. Malaria parasites are transmitted to the fetus through congenital and destroy the fetal RBC intracellular. This leads to lower hemoglobin values and subsequently increases the prevalence of newborn anemia. The possible reason for this discrepancy from the Iran study might be attributed to variation in study participants based on the mode of delivery between these studies. In Iran, all study participants were born through cesarean section, whereas about two-thirds (66.9%) of our study participants were born through spontaneous vaginal delivery. During the cesarean section, there may be an accidental incision of the placenta, resulting in bleeding leading to anemia as compared to normal vaginal delivery.
Another explanation for the discrepancy in the present study findings from the Addis Ababa, Ethiopia, study is that it includes small babies with a low birth weight, whereas the present study includes both low birth weight and normal weight newborns.
The mean hemoglobin value among newborn babies in the present study was 15.75 g/dl with a standard deviation of 3.54g/dl. This finding is supported by a study done in Turkey, which showed mean hemoglobin of 17 ± 3g/dl. This similarity might be explained by the consistency of the inclusion criteria for both preterm and term newborns and underweight and normal-weight newborn babies who participated in the studies.
Newborn babies with a gestational age of 33–36 weeks are 64% less likely to develop anemia as compared to newborns having a gestational age of 32 weeks and below. This finding is supported by various studies done in different countries.28–30 This might be explained by the relationship between gestational age and the hemoglobin concentration rising from about 10 g/dl at 16 weeks gestation to reach a value of approximately 15 g/dl at 32 to 34 weeks and an average value of 16.8 g/dl is seen in full-term infants.3
The odds of being anemic among neonates born from anemic mothers are 3.81 times higher as compared to those newborns born from non-anemic mothers. This finding is supported by similar previous studies.31,32 This is because the fetus obtains iron from maternal transferrin. When maternal iron stores are depleted, the fetus cannot accumulate as much iron and there is a decrease in fetal iron stores.
The limitation of the present study was that since the iron test was not incorporated, iron deficiency anemia may be the cause of newborn anemia. Another limitation of this study was the narrow literature to compare the findings from other studies adequately because there is a scarcity of studies regarding anemia among newborn babies.
Conclusion
The overall prevalence of anemia among newborns in TGSH was high. So, this finding showed a moderate public health problem in the study area. The independent, significantly associated risk factors for newborn anemia in this study were gestational age and maternal anemia. Efforts should be given to decrease the burden of newborn anemia by creating and enhancing awareness for the public and women about newborn anemia and the strategies to reduce preterm deliveries.
Abbreviations
AOR, Adjusted Odds Ratio; CBC, Complete Blood Count; COD, Crude Odds Ratio; GA, Gestational Age; HCT, Hematocrit; Hg, Hemoglobin; IQR, Inter Quartile Range; SPSS, Statistical Package for Social Science; TGSH, Tibebe Ghion Specialized Hospital; WHO, World Health Organization.
Data Sharing Statement
The data will be available upon request from the corresponding author.
Acknowledgment
We would like to thank Bahir Dar University College of Medicine and Health Science's Department of Pediatrics and Child Health, Tibebe Ghion Specialized Hospital staff, and mothers of newborns for their support and willingness while conducting this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
The authors did not receive any specific funding for this work.
Disclosure
We, the authors, declare that we have no competing interests.
References
1. Kligman SG, Shah B. Nelson Textbook for Pediatrics.
2. Von Lindern JS, Lopriore E. Management and prevention of neonatal anemia: current evidence and guidelines. Expert Rev Hematol. 2014;7(2):195–202. doi:10.1586/17474086.2014.878225
3. Lokeshwar MR, Dalal R, Manglani M, Shah N. Anemia in newborn. Indian J Pediatr. 1998;65(5):651–661. doi:10.1007/BF02731037
4. Javert CT. Hemorrhagic disease of the newborn. Am J Obstet Gynecol. 1938;35(2):200–214. doi:10.1016/S0002-9378(38)90112-7
5. Suzuki S, Iwata G, Sutor AH. Vitamin K deficiency during the perinatal and infantile period. InSemin Thromb Hemost. 2001;27(2):93–98. doi:10.1055/s-2001-14066
6. Kenet G, Chan A, Soucie J, Kulkarni R. Bleeding disorders in neonates. Haemophilia. 2010;16:168–175. doi:10.1111/j.1365-2516.2010.02316.x
7. Rao R, Georgieff MK. Iron therapy for preterm infants. Clin Perinatol. 2009;36(1):27–42. doi:10.1016/j.clp.2008.09.013
8. Sanjay Aher KM, Kadam S. Neonatal Anemia. KEM Hospital, Pune, Maharashtra, India: KEM Hospital; 2008.
9. John A, Widness M. Pathophysiology of anemia during the neonatal period, including anemia of prematurity. Neoreviews. 2008;9:e520–e525. doi:10.1542/neo.9-11-e520
10. Arakhita Swain SM, Trilochan M, Satpathy SK, Saiprasanna B. Aetiopathological and clinical study of anemia in newborns admitted to a tertiary care centre. Shock. 2017;4:3–77.
11. Christensen RD, Ohls RK. Anemia in the neonatal period. Neonatology. 2018;1489–1514. doi:10.1007/978-88-470-1405-3_103
12. Jember TA, Teshome DF, Gezie LD, Agegnehu CD. Spatial variation and determinants of childhood anemia among children aged 6 to 59 months in Ethiopia: further analysis of Ethiopian demographic and health survey 2016. BMC Pediatr. 2021;21(1):1–4. doi:10.1186/s12887-021-02901-y
13. Agency CS. Ethiopian Demographic and Health Survey 2016. Addis Ababa. Ethiopia, and Rockville, Maryland, USA: CSA and ICF: Key Indicators Report; 2016.
14. Sandhya V, Patil S, Rau A. Iron store status in newborns born to anemic and non-anemic mothers. J Pediatr Sci. 2012;4(1):1–4.
15. Lee S, Guillet R, Cooper EM, et al. Prevalence of anemia and associations between neonatal iron status, hepcidin, and maternal iron status among neonates born to pregnant adolescents. Pediatr Res. 2016;79(1–1):42. doi:10.1038/pr.2015.183
16. Tiruneh T, Shiferaw E, Enawgaw B. Prevalence and associated factors of anemia among full-term newborn babies at University of Gondar comprehensive specialized hospital, Northwest Ethiopia: a cross-sectional study. Ital J Pediatr. 2020;46(1):1–7. doi:10.1186/s13052-019-0764-1
17. Lee S, Guillet R, Cooper EM, et al. Prevalence of anemia and associations between neonatal iron status, hepcidin, and maternal iron status among neonates born to pregnant adolescents. Pediatr Res. 2016;79(1):42–48.
18. Kalteren WS, Horst HJH, de Vetten L, Kooi EM, Bos AF, Bos A. Perinatal anemia is associated with neonatal and neurodevelopmental outcomes in infants with moderate to severe perinatal asphyxia. Neonatology. 2018;114(4):315–322. doi:10.1159/000490369
19. Timilsina S, Karki S, Gautam A, Bhusal P, Paudel G, Sharma D. Correlation between maternal and umbilical cord blood in pregnant women of Pokhara Valley: a cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):70. doi:10.1186/s12884-018-1697-1
20. Mamoury G, Hamedy A, Akhlaghi F. Cord hemoglobin in newborns in correlation with maternal hemoglobin in northeastern Iran. Iranian J Med Sci. 2015;28(4):166–168.
21. Terefe B, Birhanu A, Nigussie P, Tsegaye A. Effect of maternal iron deficiency anemia on the iron store of newborns in Ethiopia. Anemia. 2015;2015(1):3–5. doi:10.1155/2015/808204
22. Augusta de SS, Willner E, Aguiar Duraes Pereira T, Rosse de Souza V, Teles Boaventura G, Blondet de Azeredo V. Anemia in pregnancy: impact on weight and in the development of anemia in newborn. Nutr Hosp. 2015;32(5):103–105.
23. Lone F, Qureshi R, Emmanuel F. Maternal anaemia and its impact on perinatal outcome in a tertiary care hospital in Pakistan. East Mediterr Health J. 2004;10(6):801–807. doi:10.26719/2004.10.6.801
24. Baharvand P, Fathi M, Eliyasy H, Abdolkarimi B, Kiani AA. The effect of delivery type on neonatal blood indices in an Iranian population. Biomed Res Therapy. 2018;5(10):2768–2775. doi:10.15419/bmrat.v5i10.492
25. Laar AK, Grant FE, Addo Y, et al. Predictors of fetal anemia and cord blood malaria parasitemia among newborns of HIVpositive mothers. BMC Res Notes. 2013;6(1):350. doi:10.1186/1756-0500-6-350
26. Koura GK, Ouedraogo S, Le Port A, et al. Anaemia during pregnancy: impact on birth outcome and infant hemoglobin level during the first 18 months of life. Tropical Med Int Health. 2012;17(3):283–291.
27. Alemu T, Umeta M. Prevalence and predictors of “small size” babies in Ethiopia: in-depth analysis of the Ethiopian demographic and health survey, 2011. Ethiop J Health Sci. 2016;26(3):243–250. doi:10.4314/ejhs.v26i3.7
28. Ree IM, Lopriore E. Updates in neonatal hematology: causes, risk factors, and management of anemia and thrombocytopenia. Hematol Oncol Clin. 2019;33(3):521–532.
29. Duley L, Batey N. Optimal timing of umbilical cord clamping for term and preterm babies. Early Hum Dev. 2013;89(11):905–908. doi:10.1016/j.earlhumdev.2013.09.002
30. Widness JA. Pathophysiology of anemia during the neonatal period, including anemia of prematurity. Neoreviews. 2008;9(11):e520–5.
31. Debbarma R, Debbarma B, Devi MA. Effect of maternal anaemia on cord haemoglobin and birth weight of newborn. IOSR. 2015;14(7):19–21.
32. Adam I, Babiker S, Mohammed AA, et al. Low body mass index, anaemia and poor perinatal outcome in a rural hospital in eastern Sudan. J of Tropical Pediatrics. 2008;54(3):202–204. doi:10.1093/tropej/fmm110
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
