Back to Journals » Cancer Management and Research » Volume 14
Pretreatment Fibrinogen-Albumin Ratio (FAR) Associated with Treatment Response and Survival in Advanced Non-Small Cell Lung Cancer Patients Treated with First-Line Anti-PD-1 Therapy Plus Platinum-Based Combination Chemotherapy
Authors Yuan C, Huang M, Wang H, Jiang W, Su C, Zhou S
Received 3 November 2021
Accepted for publication 30 December 2021
Published 26 January 2022 Volume 2022:14 Pages 377—386
DOI https://doi.org/10.2147/CMAR.S347547
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eşkazan
Chengliang Yuan, Meifang Huang, Huilin Wang, Wei Jiang, Cuiyun Su, Shaozhang Zhou
Department of Respiratory Oncology, Guangxi Medical University Affiliated Tumor Hospital, Nanning City, Guangxi Zhuang Autonomous Region, 530021, People’s Republic of China
Correspondence: Shaozhang Zhou; Cuiyun Su,Department of Respiratory Oncology, Guangxi Medical University Affiliated Tumor Hospital, Nanning City, Guangxi Zhuang Autonomous Region, 530021, People’s Republic of China, Tel +86-0771-5320761; +86-0771-5334955, Fax +86-0771-5300613, Email [email protected]; [email protected]
Purpose: PD-1 inhibitors have been routinely used to treat advanced non-small cell lung cancer (NSCLC) and have significantly improved clinical outcomes. In this study, we aimed to explore the influence of pretreatment fibrinogen-albumin ratio (FAR) on treatment response and survival in advanced NSCLC patients treated with first-line anti-PD-1 therapy plus platinum-based combination chemotherapy.
Patients and Methods: A total of 91 patients with advanced NSCLC were included in the study. All patients received at least two cycles of systemic first-line anti-PD-1 therapy plus platinum-based combination chemotherapy. Receiver operating characteristics analysis was performed to determine the optimal cutoff values of FAR. Univariate and multivariate analyses were used to identify independent prognostic factors, and the Kaplan–Meier method was used to estimate survival curves.
Results: Multivariate logistic regression analysis showed that N stage (N2-3) and high FAR (≥ 0.175, optimal cutoff value) were independent predictors for objective response rate (P = 0.0002, P = 0.0005, respectively). Multivariate Cox regression analysis of progression-free survival and overall survival showed that high FAR (≥ 0.145) was independent prognostic factors (P = 0.0061, P = 0.0024, respectively). Progression-free survival and overall survival were significantly shorter in the high FAR (≥ 0.145) group than those in the low FAR (< 0.145) group (P = 0.0024, P = 0.0024, respectively).
Conclusion: Pretreatment FAR was an independent predictor for treatment response and independent prognostic factors in advanced NSCLC patients treated with first-line anti-PD-1 therapy plus platinum-based combination chemotherapy.
Keywords: non-small cell lung cancer, serum albumin, plasma fibrinogen, immunotherapy, prognosis
Introduction
In patients with advanced non-small cell lung cancer (NSCLC) and PD-L1 TPS ≥50%, immune checkpoint inhibitors (ICIs) monotherapy was associated with significantly longer progression-free survival (PFS) and overall survival (OS) than those treated with platinum-based chemotherapy. However, ICIs alone may not be the best option for patients with PD-L1 TPS between 1% and 49%.1,2 In addition, it was reported that ICIs combination chemotherapy has shown its significant benefits regardless of PD-L1 expression status, without inducing concomitant side effects and financial burden for the patients.3–7 Therefore, identifying novel reliable, economic, and easily accessible biomarkers for advanced NSCLC patients treated with ICIs combination chemotherapy is essential.
Fibrinogen is an extracellular matrix protein composed of three polypeptide chains with fibrinogen alpha, beta, and gamma. Alpha may play a suppressive role in lung adenocarcinoma cells to inhibit tumor growth and metastasis through induction of apoptosis and inhibition of epithelial-mesenchymal transition.8 Fibrinogen, as a molecule produced by the liver in response to cytokine stimulation, could also reflect the status of the tumor-associated inflammatory response.9 Many tumor-growth and metastasis-enhancing events always occur during the tumor-associated inflammatory response, such as the inhibition of apoptosis, the enactment of immunosuppressive effects, the increased release of cytokines and inflammatory mediators.10 Several studies have confirmed the relationship between high serum fibrinogen levels and poor outcomes in many kinds of solid malignancies, including NSCLC,11,12 bladder cancer,13 colorectal cancer,14 and prostate cancer.15
Albumin plays a key role in the transport of chemotherapeutic drugs, binding to and being delivered by albumin can significantly affect their efficacy. Meanwhile, albumin can also bind to fatty acids, which can affect tumor proliferation and metabolism.16 It was reported that albumin, which reflects nutritional status, was also closely related to the prognosis of many kinds of solid malignancies, including NSCLC,17–19 Laryngeal Carcinoma,20 prostate cancer,15 upper tract urothelial Carcinoma,21 gastric cancer.22
Several studies have confirmed the relationship between high fibrinogen-albumin ratio (FAR) and poor outcomes in many kinds of solid malignancies, including pancreatic neuroendocrine neoplasms,23 gastrointestinal stromal tumors,24 locally advanced rectal cancer,25 Glioblastoma.26 It was also reported that FAR was independently associated with PFS in EGFR-Mutant lung adenocarcinoma patients receiving first-line EGFR-TKIs treatment.27 However, the prognostic values of FAR in advanced NSCLC patients treated with first-line anti-PD-1 therapy plus platinum-based combination chemotherapy is still unknown.
Thus, we conducted this retrospective study to mainly discuss correlations of pretreatment FAR with treatment response and survival in advanced NSCLC patients treated with first-line anti-PD-1 therapy plus platinum-based combination chemotherapy.
Materials and Methods
Patients and Samples
A total of 91 patients with advanced NSCLC who could not receive radical surgery or radiotherapy at baseline and received systemic anti-PD-1 therapy (camrelizumab, sintilimab, pembrolizumab, tislelizumab or toripalimab) plus platinum-based combination chemotherapy as the first-line setting at Guangxi Medical University Affiliated Tumor Hospital between April 2019 and July 2021 were enrolled. Patients received 200mg camrelizumab, 200mg sintilimab, 200mg pembrolizumab, 200mg tislelizumab or 240mg toripalimab intravenously once every 3 weeks. Combination chemotherapy was all based on platinum doublet chemotherapy. The other chemotherapy drugs, including pemetrexed, paclitaxel/nab-paclitaxel, docetaxel, and gemcitabine, were chosen by physicians according to clinical treatment guidelines. Patients with histories of other malignant tumors, chronic inflammatory diseases, current steroid therapy, acute infection, or deep vein thrombosis were excluded.
Clinicopathological characteristics of the patients, including age at the time of treatment, sex, smoking history, Eastern Cooperative Oncology Group score (ECOG score), histology, TNM stage, and radiotherapy were collected through electronic medical records. Plasma fibrinogen and serum albumin were collected before treatment and FAR was defined as fibrinogen-albumin ratio. Whole-body computed tomography scans were performed every 6–8 weeks after two cycles of treatment to assess patients’ response to treatment according to The Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1). The last follow-up date was July 1, 2021. Objective response rate (ORR) was defined as complete remission + partial remission. Progression-free survival (PFS) was defined as the time from initial treatment to imaging progression, death, or the last follow-up. Overall survival (OS) was defined as the time from initial treatment to the last follow-up or death, whichever came first.
This study was conducted following the principles of the Declaration of Helsinki and approved by the Ethics Committee of Guangxi Medical University Affiliated Tumor Hospital (Approval number: LW2021102). The identifiable information of patients was unnamed or anonymous to protect patients’ privacy. The need for informed consent was waived owing to the retrospective nature of the study.
Statistical Analysis
The baseline characteristics and treatment response of the patients were reported as medians and interquartile ranges for continuous variables, or frequencies and percentages for categorical variables. Receiver operating characteristics analysis was performed to determine the optimal cutoff values of FAR. Univariate and multivariate logistic regression were used to identify independent predictors between clinical factors/FAR (0.175, optimal cutoff value) and ORR. For the survival outcomes, we used the Kaplan–Meier method to generate the PFS and OS survival curves and the Log rank test to compare survival outcomes among patients separated by FAR (0.145, optimal cutoff value). Univariate and multivariate Cox proportional hazards regression analysis used the backward elimination method to estimate hazard ratios for risk factors. Variables included in the multivariable analysis were selected based on the influence of introducing covariates in the basic model or eliminating covariates in the complete model on the regression coefficient >10% and statistical significance in the univariable analysis (P < 0.10). P < 0.05 was considered statistically significant. All tests were two-sided. All data were analyzed using the statistical package R version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria) and Empower (X&Y Solutions, Inc. Boston, Massachusetts).
Results
Patients’ Clinicopathological Characteristics and Treatment Response
The clinicopathological characteristics and treatment response of the 91 advanced NSCLC patients are listed in Table 1. Twenty-three (25.27%) female patients and 68 (74.73%) male patients were included. The age of patients ranged from 32 to 80 years, and the median was 61 years. Fifty-nine (64.84%) patients had a history of smoking. Eighty-four (92.31%) patients had the ECOG score of 0–1. Forty (43.96%) patients had the histologic type of squamous cell carcinoma (SCC), while 48 (56.04%) patients were diagnosed with Non-SCC (53.8%). Twenty-two (24.18%) patients had the T stage of T1-2, while 69 (75.82%) had the T stage of T3-4. 16 (17.58%) patients had the N stage of N0-1, while 75 (82.42%) had the N stage of T2-3. 24 (26.37%) patients had the TNM stage of III, while 67 (73.63%) had the TNM stage of IV. 14 (15.38%) patients had a history of radiotherapy. The FAR ranged from 0.04 to 0.35, and the median was 0.13. The treatment response, CR 0(0%), PR 50 (54.95%), SD 36 (39.56%), and PD 5 (5.49%).
 |
Table 1 Patients’ Clinicopathological Characteristics and Treatment Response |
The Optimal Cutoff Values of FAR
The optimal cutoff value of FAR to predict ORR was 0.175 (AUC: 0.6407, sensitivity: 0.9000, specificity: 0.3659) (Supplemental Figure 1). The optimal cutoff values of FAR to predict PFS was 0.145 (AUC: 0.7170, sensitivity: 0.6154, specificity: 0.8077) (Supplemental Figure 2). The optimal cutoff value of FAR to predict OS was 0.145 (AUC: 0.7251, sensitivity: 0.7407, specificity: 0.7812) (Supplemental Figure 3).
Univariate and Multivariate Logistic Regression Analysis for ORR
The results of the univariate and multivariate logistic regression analyses are shown in Table 2. In the univariate logistic regression models, N stage (N2–3), TNM stage IV and high FAR (≥0.175, optimal cutoff value) were significant predictors for ORR (odds ratio [95% CI]: 7.27 [1.91, 27.77], p = 0.0037; 0.30 [0.11, 0.86], P = 0.0253; 0.217 [0.077–0.573], p = 0.002; respectively). In the multivariate logistic regression model, N stage (N2–3) and high FAR (≥0.175, optimal cutoff value) were independent predictors for ORR (17.45[3.78, 80.54], P = 0.0002; 0.10 (0.03, 0.36), P = 0.0005, respectively).
 |
Table 2 Univariate and Multivariate Analyses for ORR in Patients with NSCLC |
Survival Analysis
Kaplan–Meier curves of PFS and OS stratified by FAR (≥0.145 or <0.145, optimal cutoff value) are shown in Figures 1 and 2. PFS and OS were significantly shorter in the high-FAR group than those in the low-FAR group (p = 0.0024, p = 0.0024, respectively).
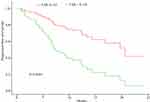 |
Figure 1 Kaplan–Meier survival curves for PFS stratified by different values of FAR. Abbreviations: PFS, progression-free survival; FAR, fibrinogen-albumin ratio. |
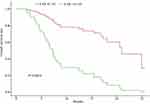 |
Figure 2 Kaplan–Meier survival curves for OS stratified by different values of FAR. Abbreviations: OS, overall survival; FAR, fibrinogen-albumin ratio. |
Univariate and Multivariate Analyses for PFS and OS
In the univariate Cox proportional hazards regression analyses, high FAR (≥0.145, optimal cutoff value) was significant prognostic factors for PFS (hazard ratio (HR) [95% Cl]: 2.60 [1.36, 4.98], P = 0.0038). In the multivariate Cox proportional hazards regression analysis, high FAR (≥0.145, optimal cutoff value) was also independent prognostic factors for PFS (hazard ratio (HR) [95% Cl]: 2.68 [1.33, 5.43], P = 0.0061) (Table 3).
 |
Table 3 Univariate and Multivariate Analyses for PFS in Patients with NSCLC |
Univariate Cox proportional hazards regression analysis showed that radiotherapy and high FAR (≥0.145, optimal cutoff value) were significant prognostic factors for OS (2.55 [1.11, 5.86], P = 0.0268; 3.74 [1.57, 8.90], P = 0.0028, respectively). Multivariate Cox proportional hazards regression analysis showed that high FAR (≥0.145, optimal cutoff value) also was significant prognostic factors for OS (4.95 [1.76, 13.89], P = 0.0024) (Table 4).
 |
Table 4 Univariate and Multivariate Analyses for OS in Patients with NSCLC |
Discussion
ICIs have become standard treatment options in patients with advanced NSCLC. It was reported that ICIs combination chemotherapy has shown significant benefits regardless of PD-L1 expression status.3–5,7,28 However, only a minority of patients benefit from this novel and costly method of treatment. PD-L1 expression, tumor mutation burden, and lymphocytic tumor infiltration might be closely related to immunotherapy outcomes.28–31 However, limited by cumbersome detection protocols and high costs, they are not considered to be perfect predictors. Therefore, easy, affordable, and efficient markers are needed to help characterize the patients who can potentially benefit from the ICIs treatment.
In recent years, it has been reported that peripheral blood biomarkers, including prognostic nutrition index, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and fibrinogen-to-lymphocyte ratio were suggestive indicators for the prognosis of advanced NSCLC patients treated with ICIs.32–34 In our study, a total of 91 advanced NSCLC patients treated with first-line anti-PD-1 therapy plus platinum-based combination chemotherapy were included retrospectively. We found that high FAR (≥0.145) was independent predictors for ORR and independent prognostic factors for PFS and OS. PFS and OS were significantly shorter in the high FAR group than those in the low FAR group. Lang et al found that decreasing leading serum tumor markers (STM) at first restaging predict longer PFS and OS among initial radiological non-responders in ICIs treated NSCLC patients.35 Tang et al found that the combination score based on the dynamics of early STM and neutrophil-to-lymphocyte ratio can accurately predict the clinical efficacy of PD-1/PD-L1 inhibitors and prognosis in advanced NSCLC patients.36 In our study, we found that FAR was independent predictors for ORR and independent prognostic factors for PFS and OS. The predictive role of STM dynamics, single or combination with FAR, further studies is needed in advanced NSCLC patients treated with first-line anti-PD-1 therapy plus platinum-based combination chemotherapy.
Fibrinogen, a molecule produced by the liver in response to cytokine stimulation, could reflect the status of the tumor-associated inflammatory response.9 A high level of fibrinogen was associated with poor prognosis in NSCLC patients.11,12 It was reported that nutrition as an important determinant of immune response and malnutrition was associated with impaired cell-mediated immunity against tumor progression and metastasis.37,38 Low serum albumin, which reflects nutritional status, could predict poor prognosis in NSCLC patients.11,18 As a composite indicator, FAR could represent the coagulation system, nutritional status, inflammation of a patient. Therefore, it is reasonable to adopt FAR as prognostic factors in advanced NSCLC patients treated with first-line anti-PD-1 therapy plus platinum-based combination chemotherapy.
In advanced NSCLC patients undergoing first-line platinum-based chemotherapy, Ying et al found that albumin-to-fibrinogen ratio (AFR) was independent risk factors for PFS and significant prognostic factors for OS. The PFS and OS in the high AFR group were significantly improved compared with those in the low AFR group.39 In our study, all patients received systemic first-line anti-PD-1 therapy plus platinum-based combination chemotherapy. The FAR was independent risk factors for PFS and significant prognostic factors for OS. PFS and OS were significantly shorter in the high FAR (≥0.145) group than those in the low FAR (<0.145) group, which was consistent with Ying et al. For patients undergoing first-generation EGFR-TKI (gefitinib, erlotinib, or icotinib) as the first-line treatment, Zhao et al found that FAR was independent prognostic factors for PFS, but not independently correlated with OS.27 In our study, the FAR was independent prognostic factors for PFS, consistent with Zhao et al. Our study also found that FAR was independently correlated with OS. In addition, our study also found that high FAR was independent predictors for ORR. To the best of our knowledge, this study has firstly investigated the relationship between FAR and clinical outcomes in advanced NSCLC patients treated with anti-PD-1 therapy combination chemotherapy regimens. Our study demonstrated that FAR was independent predictors for treatment response and independent prognostic factors for PFS and OS in advanced NSCLC patients treated with anti-PD-1 therapy plus platinum-based combination chemotherapy. Therefore, FAR is expected to become a new biomarker for prognosis evaluation and treatment response prediction for advanced NSCLC patients and is significant in the guidance they could provide for the development of individualized treatment strategies.
Our study still has several limitations. First, this study was a single-center retrospective analysis and included a small number of patients. Therefore, multicentric prospective studies with large samples need to be carried out in the future. Second, due to the lack of external data, we could not design a validation group to verify our findings. Third, due to the lack of external data, PD-L1 expression of tumors was not included in our study. All these may result in underestimating the association of PD-L1 expression with the antitumor effect using ICI treatment.
Conclusion
Pretreatment FAR was an independent predictor for treatment response and independent prognostic factors in advanced NSCLC patients treated with first-line anti-PD-1 therapy plus platinum-based combination chemotherapy.
Acknowledgments
The authors thank all the Guangxi Medical University Affiliated Tumor Hospital staff for their support in the work. In addition, we would like to thank Zhou S for the English language editing.
Funding
This study was supported by a “139 Talent Planning” granted by Guangxi Health Commission (grant number: 201903030) and a “Appropriate Technology Development, Promotion and Application Project” granted by Guangxi Health Commission (grant number: S2020102).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mok TSK, Wu Y, Kudaba I, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, Phase 3 trial. The Lancet. 2019;393(10183):1819–1830. doi:10.1016/S0140-6736(18)32409-7
2. Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. New Engl J Med. 2016;375(19):1823–1833. doi:10.1056/NEJMoa1606774
3. Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288–2301. doi:10.1056/NEJMoa1716948
4. Gandhi L, Rodriguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378(22):2078–2092. doi:10.1056/NEJMoa1801005
5. Peng TR, Lin HH, Tsai FP, Wu TW. Immune checkpoint inhibitors for first‐line treatment of advanced non‐small‐cell lung cancer: a systematic review and network meta‐analysis. Thorac Cancer. 2021;12(21):2873–2885. doi:10.1111/1759-7714.14148
6. Maung TZ, Ergin HE, Javed M, Inga EE, Khan S. Immune checkpoint inhibitors in lung cancer: role of biomarkers and combination therapies. Cureus. 2020;12(5):e8095. doi:10.7759/cureus.8095
7. Yang Y, Sun J, Wang Z, et al. Updated overall survival data and predictive biomarkers of sintilimab plus pemetrexed and platinum as first-line treatment for locally advanced or metastatic nonsquamous NSCLC in the Phase 3 ORIENT-11 study. J Thorac Oncol. 2021;16(12):2109–2120. doi:10.1016/j.jtho.2021.07.015
8. Tiscia G, Margaglione M. Human fibrinogen: molecular and genetic aspects of congenital disorders. Int J Mol Sci. 2018;19(6):1597. doi:10.3390/ijms19061597
9. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi:10.1038/nature01322
10. Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? The Lancet. 2001;357(9255):539–545. doi:10.1016/S0140-6736(00)04046-0
11. Chen P, Wang C, Cheng B, et al. Plasma fibrinogen and serum albumin levels (FA score) act as a promising prognostic indicator in non-small cell lung cancer. Onco Targets Ther. 2017;10:3107–3118. doi:10.2147/OTT.S138854
12. Ohara S, Suda K, Tomizawa K, et al. Prognostic value of plasma fibrinogen and d-dimer levels in patients with surgically resected non-small cell lung cancer. Surg Today. 2020;50(11):1427–1433. doi:10.1007/s00595-020-02019-1
13. Yang S, Guan H, Wang S, et al. Plasma fibrinogen predicts the prognosis of bladder cancer patients after radical cystectomy. Cancer Manag Res. 2020;12:9303–9314. doi:10.2147/CMAR.S269244
14. Sun Y, Han W, Song Y, et al. Prognostic value of preoperative fibrinogen for predicting clinical outcome in patients with nonmetastatic colorectal cancer. Cancer Manag Res. 2020;12:13301–13309. doi:10.2147/CMAR.S275498
15. Man Y, Chen Y. Systemic immune-inflammation index, serum albumin, and fibrinogen impact prognosis in castration-resistant prostate cancer patients treated with first-line docetaxel. Int Urol Nephrol. 2019;51(12):2189–2199. doi:10.1007/s11255-019-02265-4
16. Yu L, Hua Z, Luo X, Zhao T, Liu Y. Systematic interaction of plasma albumin with the efficacy of chemotherapeutic drugs. Biochimica Et Biophysica Acta (BBA)) Rev Cancer. 2022;1877(1):188655. doi:10.1016/j.bbcan.2021.188655
17. Miura K, Hamanaka K, Koizumi T, et al. Clinical significance of preoperative serum albumin level for prognosis in surgically resected patients with non-small cell lung cancer. Lung Cancer. 2017;111:88–95. doi:10.1016/j.lungcan.2017.07.003
18. Takada K, Takamori S, Yoneshima Y, et al. Serum markers associated with treatment response and survival in non-small cell lung cancer patients treated with anti-PD-1 therapy. Lung Cancer. 2020;145:18–26. doi:10.1016/j.lungcan.2020.04.034
19. Yang J, Xu J, Chen G, et al. Post-diagnostic C-reactive protein and albumin predict survival in Chinese patients with non-small cell lung cancer: a prospective cohort study. Sci Rep-UK. 2019;9(1):8143. doi:10.1038/s41598-019-44653-x
20. Shen L, Wang Q, Yu Q. The systemic immune-inflammation index and albumin as prognostic predictors in laryngeal carcinoma. Nutr Cancer. 2021;73(10):1916–1923. doi:10.1080/01635581.2020.1812677
21. Zhao Z, Xie S, Feng B, et al. Preoperative risk classification using neutrophil-to-lymphocyte ratio and albumin for upper tract urothelial carcinoma treated with radical nephroureterectomy. Cancer Manag Res. 2020;12:9023–9032. doi:10.2147/CMAR.S274332
22. Xiao S, Feng F, Liu N, et al. Preoperative albumin level is superior to albumin-globulin ratio as a predicting indicator in gastric cancer patients who underwent curative resection. Cancer Manag Res. 2019;11:9931–9938. doi:10.2147/CMAR.S230741
23. Deng S, Fan Z, Xia H, et al. Fibrinogen/albumin ratio as a promising marker for predicting survival in pancreatic neuroendocrine neoplasms. Cancer Manag Res. 2021;13:107–115. doi:10.2147/CMAR.S275173
24. Li R, Song S, He X, et al. Relationship between fibrinogen to albumin ratio and prognosis of gastrointestinal stromal tumors: a retrospective cohort study. Cancer Manag Res. 2020;12:8643–8651. doi:10.2147/CMAR.S271171
25. Lu S, Liu Z, Zhou X, et al. Preoperative Fibrinogen-Albumin Ratio Index (FARI) is a reliable prognosis and chemoradiotherapy sensitivity predictor in locally advanced rectal cancer patients undergoing radical surgery following neoadjuvant chemoradiotherapy. Cancer Manag Res. 2020;12:8555–8568. doi:10.2147/CMAR.S273065
26. Li J, Zhou X, Xiang Y, et al. Clinical significance of preoperative fibrinogen to albumin ratio in patients with glioblastoma: a single center experience. Cancer Manag Res. 2021;13:3259–3269. doi:10.2147/CMAR.S305025
27. Zhao X, Zhang N, Zhang H, et al. High fibrinogen-albumin ratio index predicts poor prognosis for lung adenocarcinoma patients undergoing epidermal growth factor receptor-tyrosine kinase inhibitor treatments. Medicine. 2020;99(46):e23150. doi:10.1097/MD.0000000000023150
28. Melosky B, Chu Q, Juergens RA, et al. Breaking the biomarker code: PD-L1 expression and checkpoint inhibition in advanced NSCLC. Cancer Treat Rev. 2018;65:65–77. doi:10.1016/j.ctrv.2018.02.005
29. Arak H, Aytekin A, Canoz O, Ozkan M. Prognostic and predictive significance of pd-l1 expression in non-small cell lung cancer patients: a single-center experience. Turkish J Pathol. 2021;37(3):239–248. doi:10.5146/tjpath.2021.01545
30. Negrao MV, Skoulidis F, Montesion M, et al. Oncogene-specific differences in tumor mutational burden, PD-L1 expression, and outcomes from immunotherapy in non-small cell lung cancer. J Immunother Cancer. 2021;9(8):e2891. doi:10.1136/jitc-2021-002891
31. Banna GL, Signorelli D, Metro G, et al. Neutrophil-to-lymphocyte ratio in combination with PD-L1 or lactate dehydrogenase as biomarkers for high PD-L1 non-small cell lung cancer treated with first-line pembrolizumab. Transl Lung Cancer Res. 2020;9(4):1533–1542. doi:10.21037/tlcr-19-583
32. Peng L, Wang Y, Liu F, et al. Peripheral blood markers predictive of outcome and immune-related adverse events in advanced non-small cell lung cancer treated with PD-1 inhibitors. Cancer Immunol Immunother. 2020;69(9):1813–1822. doi:10.1007/s00262-020-02585-w
33. Russo A, Russano M, Franchina T, et al. Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and outcomes with nivolumab in pretreated Non-Small Cell Lung Cancer (NSCLC): a large retrospective multicenter study. Adv Ther. 2020;37(3):1145–1155. doi:10.1007/s12325-020-01229-w
34. Liu M, Yang J, Wan L, Zhao R. Elevated pretreatment fibrinogen-to-lymphocyte percentage ratio predict tumor staging and poor survival in non-small cell lung cancer patients with chemotherapy or surgery combined with chemotherapy. Cancer Manag Res. 2021;13:4921–4933. doi:10.2147/CMAR.S308659
35. Lang D, Horner A, Brehm E, et al. Early serum tumor marker dynamics predict progression-free and overall survival in single PD-1/PD-L1 inhibitor treated advanced NSCLC—A retrospective cohort study. Lung Cancer. 2019;134:59–65. doi:10.1016/j.lungcan.2019.05.033
36. Tang Y, Cui Y, Li LL, et al. Dynamics of early serum tumour markers and neutrophil-to-lymphocyte ratio predict response to PD-1/PD-L1 inhibitors in advanced non-small-cell lung cancer. Cancer Manag Res. 2021;13:8241–8255. doi:10.2147/CMAR.S329963
37. Zitvogel L, Tesniere A, Kroemer G. Cancer despite immunosurveillance: immunoselection and immunosubversion. Nat Rev Immunol. 2006;6(10):715–727. doi:10.1038/nri1936
38. Tanriverdi O, Avci N, Oktay E, et al. Pretreatment serum albumin level is an independent prognostic factor in patients with Stage IIIB non-small cell lung cancer: a study of the Turkish Descriptive Oncological Researches Group. Asian Pac J Cancer Prev. 2015;16(14):5971–5976. doi:10.7314/APJCP.2015.16.14.5971
39. Ying J, Zhou D, Gu T, Huang J, Liu H. Pretreatment albumin/fibrinogen ratio as a promising predictor for the survival of advanced non small-cell lung cancer patients undergoing first-line platinum-based chemotherapy. BMC Cancer. 2019;19(1):288. doi:10.1186/s12885-019-5490-y
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
