Back to Journals » Clinical Interventions in Aging » Volume 14
Preserved physical fitness is associated with lower 1-year mortality in frail elderly patients with a severe comorbidity burden
Authors Åhlund K , Ekerstad N , Bäck M , Karlson BW, Öberg B
Received 17 December 2018
Accepted for publication 14 February 2019
Published 18 March 2019 Volume 2019:14 Pages 577—586
DOI https://doi.org/10.2147/CIA.S198591
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Kristina Åhlund,1,2 Niklas Ekerstad,3,4 Maria Bäck,2,5 Björn W Karlson,6,7 Birgitta Öberg2
1Department of Physiotherapy, NU Hospital Group, Trollhättan, Sweden; 2Department of Medical and Health Sciences, Division of Physiotherapy, Linköping University, Linköping, Sweden; 3Department of Research and Development, NU Hospital Group, Trollhättan, Sweden; 4Department of Medical and Health Sciences, Division of Health Care Analysis, Linköping University, Linköping, Sweden; 5Department of Occupational Therapy and Physiotherapy, Sahlgrenska University Hospital, Gothenburg, Sweden; 6Department of Molecular and Clinical Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 7Department of Internal and Acute Medicine, NU Hospital Group, Trollhättan-Uddevalla, Sweden
Introduction: Physical deterioration in connection with a care episode is common. The aim of this study was, in frail elderly patients with a severe comorbidity burden, to analyze 1) the association between physical fitness measurements and 1-year mortality and 2) the association between preserved physical fitness during the first three months after discharge from emergency hospital care and 1-year prognosis.
Methods: Frail elderly patients (≥75 years) in need of inpatient emergency medical care were included. Aerobic capacity (six-minute walk test, 6MWT) and muscle strength (handgrip strength test, HS) were assessed during the hospital stay and at a three-month follow-up. The results were analyzed using multivariate Cox regression; 1) 0–12-month analysis and 2) 0–3-month change in physical fitness in relation to 1-year mortality. The analyses were adjusted for age, gender, comorbidity and frailty.
Results: This study comprised 408 frail elderly hospitalized patients of whom 390 were evaluable (mean age 85.7 years, Charlson’s index mean 6.8). The three-month mortality was 11.5% and the 1-year mortality was 37.9%. After adjustments, the Cox-regression analysis showed that both 6MWT and HS were associated with 1-year mortality, HR6MWT 3.31 (95% CI 1.89–5.78, p<0.001) and HRHS 2.39 (95% CI 1.33–4.27, p=0.003). The 0–3-month change in the 6MWT and the HS were associated with 1-year mortality, where patients who deteriorated had a poorer prognosis than those with improved fitness, HR6MWT 3.80 (95% CI 1.42–10.06, p=0.007) and HRHS 2.21 (95% CI 1.07–4.58, p=0.032).
Conclusion: In frail elderly patients with a severe comorbidity burden, physical fitness in connection with emergency hospital care was independently associated with 1-year mortality. Moreover, a change in physical fitness during the first months after hospital care was important for the long-term prognosis. These results emphasize the importance of providing hospital care designed to prevent physical deterioration in frail elderly patients.
Keywords: frail elderly, mortality, physical fitness, six-minute walk test, handgrip strength test, in-hospital rehabilitation
Introduction
Society faces a major challenge in designing healthcare to provide good care for an increasing number of frail elderly patients. When people age, multimorbidity, disability and cognitive impairment become more common, which places substantial demands on healthcare systems.1,2
Frailty is a dynamic syndrome with known negative health outcomes, which can improve and worsen over time.3 A frail person is often characterized by a reduced physiological reserve and increased vulnerability, which poses a high risk of a recurrent need for hospitalization, institutionalization and death.4 In this condition, critical illness requiring hospitalization and prolonged bed rest are associated with physical deterioration and functional impairment persisting for a long time after hospital discharge.5–8 It has been reported that among old, independently walking patients, almost 20% require assistance after discharge from a period of medical inpatient care.9 Suboptimal post-hospital recovery leads to a negative spiral in physical function, which in turn affects the ability to maintain independence and is strongly associated with a reduced ability to benefit from medical interventions and an even poorer prognosis.10–13
There is no consensus definition of frailty, but most researchers agree that there are two types of frailty; physical and psychological, where the occurrence of sarcopenia and diminished muscle strength is one important discriminatory characteristic.14,15 One commonly used definition is The accumulation of deficits model, which adds together a person’s different diseases and disabilities to produce an index.16 Fried’s definition17 of physical frailty includes the following components: unintended weight loss, muscle weakness, self-reported exhaustion, slow gait speed and reduced physical activity. It identifies a frail person if three or more of these are fulfilled.
In frail elderly patients, hospital care is often acute and necessarily has a medical focus.1,18 The association between physical deterioration and hospital care is well known, but, despite this, interventions to counteract progressive disability are unusual.5,19 It has been shown that frail patients benefit from an interdisciplinary and holistic perspective of care, where well-structured rehabilitation is routinely part of the hospital treatment.20–22 Comprehensive Geriatric Assessment (CGA) is one care model with documented beneficial effects in terms of mortality, disability and cognitive functions.23 Recently, CGA was found to be superior to conventional medical care in preserving aerobic capacity, muscle strength and mobility three months after discharge from hospital in frail, acutely ill elderly patients.24 The multi-professional approach, comprising early assessment, interdisciplinary care, including regular team meetings, educational efforts and good access to assistive devices, is regarded as crucial for the prevention of functional decline. This means that there is still rehabilitation potential, even in frail elderly patients.
The aim of this study was, in frail elderly patients with a severe comorbidity burden, to analyze 1) the association between physical fitness measurements and 1-year mortality and 2) the association between a preserved physical fitness during the first three months after discharge from emergency hospital care and 1-year prognosis.
Materials and methods
This study is a sub-study from the project entitled “Is the Treatment of Frail Elderly Patients Effective in an Elderly Care Unit” (TREEE), which is a prospective controlled clinical trial carried out at the NU (NÄL-Uddevalla) Hospital Group, in western Sweden. This sub-study focuses on how physical fitness-related variables are associated with mortality and uses a different main outcome (1-year mortality in comparison to previously reported 3-month mortality). All the participants in the study gave their written informed consent, by themselves or by proxy. The study was conducted in accordance with the Declaration of Helsinki and approved by the regional ethical review board in Gothenburg (Entry no: 8883-12, December 12, 2012) and registered at the Swedish National Database of Research and Development; identifier 113021 (http://www.researchweb.org/is/vgr/project/113021), November 4, 2012.
Data collection and procedure
The original study design, inclusion-and exclusion criteria, methods and characteristics of the cohort have already been reported.25
Between March 2013 and July 2015, patients aged 75 years or more, frail according to the FRail Elderly Support researcH group (FRESH) screening instrument26,27 and in need of inpatient emergency medical care were included in the study. Patients with severe acute illness suitable for specialized hospital units, eg, acute myocardial infarction or stroke, were excluded from the study, as were patients whose informed consent could not be obtained.
Patients were identified by a general practitioner at the health care center or by the ambulance staff. When they found a person aged 75 years or more and in need of medical inpatient care, they called the geriatric emergency department (ED) and the patient was screened for frailty. If the patient was considered frail, he or she became eligible for the study. The patient could be allocated to a general medical ward, or to a ward using a CGA working model. After the patient was admitted to the ward, oral and written information was given and consent was obtained from the patient, or, if necessary, from the patient’s next of kin. Clinical and demographic characteristics were collected from medical records. All the participants performed tests of physical fitness during the index hospital stay. In connection with a follow-up visit to the hospital or in the patient’s home three months later, the same variables were registered. After one year, information on date of death was obtained through the medical records or the National Registry of Records.
Both tests of physical fitness were performed by experienced physical therapists, except in a few cases where they were performed by a specifically trained physician. In order to maintain good inter-rater reliability, the test procedure was repeated and calibrated several times before the study began and again during the study period, with the aim of ensuring that all the assessors would perform the test procedure in the most similar manner possible.
Because of the participants’ often severe condition and sometimes due to organizational difficulties, it was not possible to standardize the day of the first test. The aim was to perform tests when the participant was medically stabilized, in most cases toward the end of the hospital stay. Missing could be due to discharge before the tests were performed, the patient chose to renounce the test, the patient did not understand the instructions, (eg, due to severe dementia), or in a few cases due to the hand-dynamometer was missing. Some follow-up visits were made in the patients’ homes. When there was no access to a 30-meter straight stretch, the six-minute walk test (6MWT) was reported as missing.
Measurements
Physical fitness
The 6MWT was originally designed to measure sub-maximal aerobic capacity in patients with cardiorespiratory diseases28 and it has shown good test–retest reliability in community-dwelling elderly (ICC=0.95).29 When performing the test, the person walks back and forth along a 30-meter corridor with markings every five meters. The instruction is to walk as far as possible during a six-minute period. In the present study, patients were allowed to stop and continue during the test, but the test was interrupted if the patient was unable to complete, usually due to dyspnea and dizziness. Walking aids were allowed.
The handgrip strength (HS) test is a valid test of muscle strength and has been shown to have good test–retest reliability in community-dwelling elderly and in older persons with dementia (ICC=0.97).30,31 The HS test was performed using an hydraulic hand dynamometer (SAEHAN) with the option of an individually adapted grip position.30 The patient had to be in a sitting position with his/her arm next to the body, the elbow flexed at 90° and the wrist in a neutral position and he/she was then instructed to squeeze the dominant hand as hard as possible and relax. The result is the peak value (kg) of three attempts, with a short rest (about one minute) between each attempt. A few patients did not manage to sit independently. They were allowed to lie in bed with the head end raised and the elbow supported.
Patient descriptive characteristics
Age, gender and other demographics were identified and retrieved from medical records or in conversation with the patient or the patient’s next of kin.
Frailty was assessed by a nurse or physician at the time of inclusion, using the FRESH screening instrument.26,27 The original FRESH consists of five items related to tiredness, falls, endurance, needing support while shopping and three or more visits to the ED in the past 12 months. If the patient fulfills two or more of the items, he or she is considered to be frail. The four physical questions (ED visits excluded) has been validated to identify frail individuals in an emergency hospital setting compared with the frailty phenotype indicators.26 The four-question FRESH screening instrument has been shown to have good sensitivity (81%) and specificity (80%).26 In this study the fifth question about ED-visits was omitted.
Comorbidity is a frequently used predictor of mortality. Charlson’s Comorbidity Index (CCI)32 is a validated instrument for assessing the comorbidity burden and predicting short- and long-term mortality in an acute medical setting.33 The CCI consists of 19 conditions, each of which is given a severity weighting depending on the risk of dying associated with this condition. From this an index is produced, which may give an indication of the prognosis. In a previous study, a CCI of ≥3 was regarded as a substantial comorbidity burden.34 In this study, the assessing physician completed the CCI before discharge and again at the three-month follow-up visit.
Statistical analyses
This study is a sub-study of the research project known as TREEE. The sample size calculation was based on the primary outcome, ie a decline in ADL (Katz index) from baseline to three months after discharge. The power analysis has been previously described.24
The data were computerized and analyzed using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, Version 22.0, Armonk, NY: IBM Corp).
The characteristics of the population at baseline and at the three-month follow-up were described as continuous variables and divided into categories. Time to death was analyzed using the number of days after discharge from hospital.
The hazard ratios (HR) were calculated using the results of the physical fitness measurements (6MWT and HS) in two different models of multivariate Cox proportional hazard regression analysis. First, a model analyzing the baseline values of physical fitness in relation to all-cause 1-year mortality, and the second model analyzing the 0–3 months change in physical fitness in relation to all-cause 1-year mortality. The proportional hazard assumption was visually evaluated with log minus log plots and Schoenfeld residuals and in addition analyzed by modeling of the interaction between time and each covariate. The proportional hazard assumption was met in all presented models. The analyses were adjusted for age, gender, comorbidity burden and degree of frailty. In addition, the second analysis was adjusted for the index measurement value.
In the first analysis, HS was dichotomized as low versus normal based on a previously used definition of sarcopenia (normal >20 kg women, >30 kg men).35 The results for the 6MWT were divided into the categories of 0–100 m, 101–200 m and >200 m, which were adapted to fit our population where most patients walked only short distances. Patients who did not manage to perform the tests were categorized as low HS or in the 0–100 m group. In the second analysis, the 0–3 month changes were trichotomized as decline, stability and improvement. There were no consensus definitions of the minimal clinically important change for frail elderly hospitalized patients in relation to the measurements used. The cut-off values for each test had to be stipulated from a statistical viewpoint. As a result, the change from index to follow-up of the study population was used and if it had decreased by one quartile or more, it was assumed to be a relevant decline. HS: decline less than −2 kg, stable −1 kg to +2 kg, improvement +3 kg or more. 6MWT: decline less than −50 m, stable −49 m to +23 m, improvement more than +24 m.
Results
In this study 408 hospitalized frail elderly patients (56.7% females, mean age 85.7 years, age range 75–99 years) were included. Eighteen patients died during the index hospital stay. The post-hospitalization mortality was calculated for those 390 patients discharged alive. The patients were heavily affected by diseases, especially cardiovascular disease. The most common diagnoses were renal failure (87%), hypertension (71%), heart failure (40%), ischemic heart disease (30%) and cerebrovascular disease (26%). During the first three months after discharge 11.5% of the patients died and after one year mortality was 37.9%, see the flow chart in Figure 1. For index and three-month characteristics of the population, see Table 1.
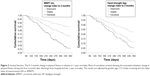
The Cox-regression analysis showed that both the 6MWT at index and the change during the first three months were associated with 1-year mortality. The adjusted hazard ratios were HR6MWT 3.31 (95% CI 1.89–5.78, p<0.001) for 1-year mortality, where those with a walking distance of <100 m at index ran a higher risk of dying than those who walked >200 m. Patients who declined during the first three months ran a higher risk of poorer 1-year prognosis than those who improved in walking distance, HR6MWT decline 3.80 (95% CI 1.44–10.06, p=0.007), see Table 2 and Figure 2. In addition, the adjusted analysis showed that a high comorbidity burden at index (CCI ≥8) and male gender were associated with higher mortality, but degree of frailty and age did not have a significant influence, see Table 3.
The Cox regression analysis showed that both low HS at index and a decline in HS during the first three months were associated with 1-year mortality. The adjusted hazard ratios were HRHS low 2.39 (95% CI 1.33–4.27, p=0.003) for 1-year mortality and patients who declined during the first three months had higher risk of poorer 1-year prognosis than those who improved in HS, HRHS decline 2.21 (95% CI 1.07–4.58, p=0.032), see Table 2 and Figure 2. In addition, the adjusted analysis showed that a high comorbidity burden at index (CCI ≥8) and male gender were associated with higher mortality, but degree of frailty and age did not have a significant influence, see Table 3.
Discussion
To our knowledge, this is the first study that has shown that both walking distance and HS at baseline are associated with 1-year mortality. The results also demonstrate that the preservation of or improvement in physical fitness during the first three months after hospital care is associated with better long-term survival. If the patient declined in terms of walking distance or HS and did not recover in the first three months after hospitalization, the 1-year mortality rate was higher compared with those who preserved or improved their physical fitness.
It is well known that poor cardiorespiratory fitness and muscle strength are associated with increased mortality in healthy individuals36,37 but, as yet, this has not been extensively investigated in frail patients with a severe comorbidity burden. In the present study, poor physical fitness was independently associated with higher 1-year mortality, which is consistent with previous research on hospitalized elderly patients,38 showing that HS and the ability to perform the 6MWT at the time of hospital discharge were predictive of the long-term prognosis. Previous research on elderly patients with chronic obstructive pulmonary disease found a walking distance in the 6MWT of below 330 m was associated with an increased risk of dying39 and if the cutoff was lowered to <200 m, the analysis showed even better sensitivity and specificity in relation to mortality.40 In frail patients with heart failure, a walking distance of <300 m was associated with increased mortality.41 The present study indicates that, in hospitalized frail elderly patients with a severe comorbidity burden even shorter distances may have a prognostic impact. Even after taking account of other factors relevant to mortality, in patients who walked <100 m in the 6MWT, the risk of dying was more than three times higher than in those who walked >200 m.
In a study of ambulatory old patients with heart failure (age 85.2 years and CCI 3.2) recently discharged from hospital, the prevalence of frailty, based on Fried’s criteria, was associated with 1-year mortality.42 Frail patients ran a greater risk of physical decline compared with non-frail patients, but, as single markers, the authors found no significant associations between slow gait speed or muscle weakness and mortality. These results are contrary to those in the present study. It is probably that the already reduced margins in a frail patient play a major role and make a frail, severely ill patient more likely to deteriorate further, which in turn appears to be associated with an increased risk of dying.
Most studies focus on improvements after an intervention. In the present study, it is important to note that, in a group of frail elderly patients with a severe comorbidity burden, even interventions that prevent deterioration appear to be valuable in a longer perspective. There are examples of care that routinely work for the preservation of physical fitness in hospitalized patients. Recently, another study from the TREEE study was published. It found that hospital care in a CGA unit was superior in terms of preserving physical fitness in frail elderly patients over a three-month follow-up period, compared with conventional care.24 Some intensive care units work in a structured manner on the early mobilization of critically ill patients, including early initiated activities that help restore cardiopulmonary and muscular systems, prevent joint contractures and focus on the patient’s autonomy at an early stage. Improvements in the recovery of physical function and quality of life in both frail and non-frail elderly patients have been reported.21,43 It is probable that the interdisciplinary approach in these care units contributes to that result.
Physical function is an important factor when decisions about nursing homes are to be taken and it is crucial for the ability to ambulate, maintain independence in daily activities and maintain good autonomy, factors that are rated as important by older people.44 Small improvements in physical function can have a major impact on the quality of life of severely ill patients.45
Mobility limitations and morbidity are strong predictors of higher inpatient and post-acute healthcare utilization.46 A study of the cost-effectiveness of CGA units for acutely ill frail elderly patients indicated that CGA might be cost-effective in comparison to conventional care.47 Based on estimated population demographics in the coming years, with increasing numbers of aging people in society, CGA should be a reasonable alternative for more patients in daily hospital care.
Limitations
The results of this study need to be considered in relation to the study limitations. The patients were first assessed during their index hospital stay and then again in connection with a follow-up visit three months later. The first analysis used the index value of measurements for the 6MWT and HS in relation to 1-year mortality. In this analysis, all patients who survived the index hospital stay were included. The second analysis used the differences between the index- and the three-month assessments in relation to 1 year-mortality. This analysis only included patients who survived the first three months and were assessed for physical fitness twice. To improve the generalizability and enable the inclusion of as many patients as possible, those assessed as “not able to perform” were categorized in the lowest group, ie, <100 m and <10 kg. The main strength of the study is probably the clinical setting, where this study succeeded in measuring a 1-year mortality based on objective values of physical fitness in a population of hospitalized frail elderly patients with a severe comorbidity burden. From the perspective of rehabilitation, it appears to be important that these patients are able to benefit from interventions that simply preserve physical fitness. In relation to prognostic long-term effects, avoiding deterioration and not only improvement should be the aim.
Conclusion
Physical fitness in connection with emergency hospital care is independently associated with 1-year mortality. Moreover, the preservation of or improvement in physical fitness during the first months after hospital care is associated with a better long-term prognosis. These results emphasize the importance of evaluating physical fitness and offering interventions to prevent physical decline in frail elderly patients.
Acknowledgment
The authors wish to thank the NU Hospital Group, Department of Research and Development, for financing research time and all the co-workers within the study group for their great assistance with data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
SBU. Comprehensive Geriatric Assessment and Care of Frail Elderly. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2014. SBU report no 221 (in Swedish). Available from: https://www.sbu.se/sv/publikationer/SBU-utvarderar/omhandertagande-av-aldre-som-inkommer-akut-till-sjukhus--med-fokus-pa-skora-aldre/. Accessed March 7, 2019. | ||
Roberts DC, McKay MP, Shaffer A. Increasing rates of emergency department visits for elderly patients in the United States, 1993 to 2003. Ann Emerg Med. 2008;51(6):769–774. | ||
Vermeiren S, Vella-Azzopardi R, Beckwee D, et al. Frailty and the prediction of negative health outcomes: a meta-analysis. J Am Med Dir Assoc. 2016;17(12):1163.e1–1163.e17. | ||
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):M255–M263. | ||
Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA. 2011;306(16):1782–1793. | ||
Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370(17):1626–1635. | ||
Zisberg A, Shadmi E, Gur-Yaish N, Tonkikh O, Sinoff G. Hospital-associated functional decline: the role of hospitalization processes beyond individual risk factors. J Am Geriatr Soc. 2015;63(1):55–62. | ||
Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59(2):266–273. | ||
Mahoney JE, Sager MA, Jalaluddin M. New walking dependence associated with hospitalization for acute medical illness: incidence and significance. J Gerontol A Biol Sci Med Sci. 1998;53(4):M307–M312. | ||
Afilalo J, Alexander KP, Mack MJ, et al. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol. 2014;63(8):747–762. | ||
Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56(12):2171–2179. | ||
Hatheway OL, Mitnitski A, Rockwood K. Frailty affects the initial treatment response and time to recovery of mobility in acutely ill older adults admitted to hospital. Age Ageing. 2017;46(6):920–925. | ||
Socorro Garcia A, de la Puente M, Perdomo B, Lopez Pardo P, Baztan JJ. Functional status and mortality at month and year in nonagenarians hospitalized due to acute medical illness. Eur J Intern Med. 2015;26(9):705–708. | ||
Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397. | ||
Cesari M, Calvani R, Marzetti E. Frailty in older persons. Clin Geriatr Med. 2017;33(3):293–303. | ||
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495. | ||
Fried LP, Tangen CM, Walston J, et al; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. | ||
Banerjee S. Multimorbidity–older adults need health care that can count past one. Lancet. 2015;385(9968):587–589. | ||
Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009;57(9):1660–1665. | ||
Ellis G, Gardner M, Tsiachristas A, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9:CD006211. | ||
Goldfarb M, Afilalo J, Chan A, Herscovici R, Cercek B. Early mobility in frail and non-frail older adults admitted to the cardiovascular intensive care unit. J Crit Care. 2018;47:9–14. | ||
Surkan MJ, Gibson W. Interventions to mobilize elderly patients and reduce length of hospital stay. Can J Cardiol. 2018;34(7):881–888. | ||
Pilotto A, Cella A, Pilotto A, et al. Three decades of comprehensive geriatric assessment: evidence coming from different healthcare settings and specific clinical conditions. J Am Med Dir Assoc. 2017;18(2):192.e1–192.e11. | ||
Ahlund K, Back M, Oberg B, Ekerstad N. Effects of comprehensive geriatric assessment on physical fitness in an acute medical setting for frail elderly patients. Clin Interv Aging. 2017;12:1929–1939. | ||
Ekerstad N, Karlson BW, Dahlin Ivanoff S, et al. Is the acute care of frail elderly patients in a comprehensive geriatric assessment unit superior to conventional acute medical care? Clin Interv Aging. 2017;12:1–9. | ||
Eklund K, Wilhelmsson K, Landahl S, Ivanoff-Dahlin S. Screening for frailty among older emergency department visitors: validation of the new FRESH-screening instrument. BMC Emerg Med. 2016;16(1):27. | ||
Wilhelmson K, Duner A, Eklund K, et al. Design of a randomized controlled study of a multi-professional and multidimensional intervention targeting frail elderly people. BMC Geriatr. 2011;11:24. | ||
Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132(8):919–923. | ||
Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82(2):128–137. | ||
Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am. 1984;9(2):222–226. | ||
Alencar MA, Dias JM, Figueiredo LC, Dias RC. Handgrip strength in elderly with dementia: study of reliability. Rev Bras Fisioter. 2012;16(6):510–514. | ||
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. | ||
Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE. Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc. 2014;62(2):342–346. | ||
de la Rica-Escuin M, Gonzalez-Vaca J, Varela-Perez R, et al. Frailty and mortality or incident disability in institutionalized older adults: the FINAL study. Maturitas. 2014;78(4):329–334. | ||
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al; European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–423. | ||
Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024–2035. | ||
Leong DP, Teo KK, Rangarajan S, et al; Prospective Urban Rural Epidemiology (PURE) Study investigators. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015;386(9990):266–273. | ||
Martin-Ponce E, Hernandez-Betancor I, Gonzalez-Reimers E, Hernandez-Luis R, Martinez-Riera A, Santolaria F. Prognostic value of physical function tests: hand grip strength and six-minute walking test in elderly hospitalized patients. Sci Rep. 2014;4:7530. | ||
Spruit MA, Polkey MI, Celli B, et al; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) study investigators. Predicting outcomes from 6-minute walk distance in chronic obstructive pulmonary disease. J Am Med Dir Assoc. 2012;13(3):291–297. | ||
Karpman C, DePew ZS, LeBrasseur NK, Novotny PJ, Benzo RP. Determinants of gait speed in COPD. Chest. 2014;146(1):104–110. | ||
Boxer R, Kleppinger A, Ahmad A, Annis K, Hager D, Kenny A. The 6-minute walk is associated with frailty and predicts mortality in older adults with heart failure. Congest Heart Fail. 2010;16(5):208–213. | ||
Rodriguez-Pascual C, Paredes-Galan E, Ferrero-Martinez AI, et al. The frailty syndrome is associated with adverse health outcomes in very old patients with stable heart failure: A prospective study in six Spanish hospitals. Int J Cardiol. 2017;236:296–303. | ||
Joseph B, Jehan FS. The mobility and impact of frailty in the intensive care unit. Surg Clin North Am. 2017;97(6):1199–1213. | ||
Kus S, Muller M, Strobl R, Grill E. Patient goals in post-acute geriatric rehabilitation–goal attainment is an indicator for improved functioning. J Rehabil Med. 2011;43(2):156–161. | ||
Rizzoli R, Reginster JY, Arnal JF, et al. Quality of life in sarcopenia and frailty. Calcif Tissue Int. 2013;93(2):101–120. | ||
Ensrud KE, Lui LY, Langsetmo L, et al; Osteoporotic Fractures in Men (MrOS) Study Group. Effects of mobility and multimorbidity on inpatient and postacute health care utilization. J Gerontol A Biol Sci Med Sci. 2018;73(10):1343–1349. | ||
Ekerstad N, Karlson BW, Andersson D, et al. Short-term resource utilization and cost-effectiveness of comprehensive geriatric assessment in acute hospital care for severely frail elderly patients. J Am Med Dir Assoc. 2018;19(10):871–878.e2. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.