Back to Journals » Journal of Pain Research » Volume 15
Preoperative Vitamin D Level is Associated with Acute Pain After Video-Assisted Thoracoscopic Surgery: A Retrospective Cohort Study
Authors Zeng X , Chen X, Li C, Shi H
Received 14 July 2022
Accepted for publication 28 September 2022
Published 12 October 2022 Volume 2022:15 Pages 3189—3196
DOI https://doi.org/10.2147/JPR.S382407
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ellen M Soffin
Xiaoping Zeng,1,* Xue Chen,1,* Caixia Li,2 Hong Shi1
1Department of Anesthesiology, Shanghai Pulmonary Hospital, School of Medicine, Tongji University, Shanghai, 200433, People’s Republic of China; 2Department of Anesthesiology, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, 200437, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Caixia Li, Department of Anesthesiology, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, 200437, People’s Republic of China, Tel +86-21-65161782-3235, Email [email protected] Hong Shi, Department of Anesthesiology, Shanghai Pulmonary Hospital, school of Medicine, Tongji University, Shanghai, 200433, People’s Republic of China, Tel +86-21-65115006-2060, Email [email protected]
Purpose: Low vitamin D levels have been associated with musculoskeletal pain, cancer pain, chronic postoperative pain, and post-traumatic pain. However, their association with postoperative pain after video-assisted thoracoscopic surgery has not been explored. The aim of this study was to examine the association between vitamin D levels and postoperative pain after video-assisted thoracoscopic surgery.
Patients and Methods: This study enrolled 194 adult patients who underwent elective non-cardiac thoracic surgery in Shanghai Pulmonary Hospital from February 2021 to June 2021. Following application of the exclusion criteria, 135 patients who underwent video-assisted thoracoscopic surgery were included in the final analysis. The primary outcome was the incidence of acute postoperative moderate-severe pain. Secondary outcomes included C-reactive protein (CRP), interleukin (IL)-1, IL-6, and tumor necrosis factor-α levels in the immediate postoperative (48 hours) period, as well as pain scores at 3 months after surgery. A multivariable logistic regression model was used to analyze the association between vitamin D levels and acute postoperative moderate-severe pain.
Results: Among 135 patients, 54.1% were categorized as having a low vitamin D level (< 30 nmol/L). On multivariable analysis, patients with a low 25-hydroxy-vitamin D (25[OH]D) level had a higher risk of postoperative moderate-severe pain (odds ratio, 2.44; 95% confidence interval, 1.181– 5.041; P = 0.016) when compared to patients with a sufficient 25(OH)D level. Static and dynamic pain scores at 3 months after surgery, as well as serum levels of CRP, IL-1, IL-6, and tumor necrosis factor-α were not significantly different between patients with low and sufficient 25(OH)D levels.
Conclusion: Patients with low vitamin D levels are at a higher risk of acute moderate-severe pain after video-assisted thoracoscopic surgery.
Trial Registration: http://www.chictr.org.cn, ChiCTR2100052380.
Keywords: vitamin D, video-assisted thoracoscopic surgery, moderate-severe pain, chronic pain, inflammatory response
Introduction
Vitamin D deficiency is a universal problem that seriously affects human health.1 The prevalence of vitamin D deficiency among adults in America ranges from 34–37%.2 Approximately one billion people worldwide have vitamin D deficiency.3 Vitamin D plays important roles in calcium homeostasis and musculoskeletal health. The anti-inflammatory and immunomodulatory effects of vitamin D are mediated through its control of cytokine release and suppression of T-cell responses.4–6 As vitamin D controls genes encoding for proteins involved in modulating neuronal axon growth and pain signaling pathways, it may also be involved in pain perception and processing.3,6,7
Several studies have reported that vitamin D deficiency is associated with musculoskeletal pain, cancer pain, postoperative pain, and post-traumatic pain.8–15 Low vitamin D levels have been linked with higher opioid use and an increased risk of opioid use disorders in patients undergoing common surgical procedures.10,16 Two meta-analyses of randomized controlled trials (RCTs) highlighted a correlation between vitamin D supplementation and pain reduction.17,18 An additional RCT reported the promising report of vitamin D supplementation in patients with post-craniotomy pain after brain tumor surgery.19
Postoperative patients often suffer from pain caused by surgical incision, which is related to the postoperative inflammatory response and immunomodulation. Theoretically, patients with vitamin D deficiency are more susceptible to severer acute pain and chronic pain after surgery. However, no prior studies have investigated the potential association between vitamin D levels and postoperative pain after video-assisted thoracoscopic surgery. Thus, the objective of this study was to evaluate the association of preoperative serum vitamin D levels with the incidence of moderate-severe pain in the immediate postoperative (48 hours) period among patients after video-assisted thoracoscopic surgery. The secondary objective was to determine whether lower vitamin D levels increase the degree of inflammatory response in the immediate postoperative period, as well as chronic pain at 3 months after surgery.
Materials and Methods
Setting and Population
This retrospective cohort study was conducted from February 2021 to June 2021 and enrolled 194 adult patients who underwent elective non-cardiac thoracic surgery in the Shanghai Pulmonary Hospital. Patients were excluded if they (1) lacked serum 25-hydroxy-vitamin D (25[OH]D) level data, (2) received thoracotomy or video-assisted mini-thoracotomy, (3) were administered analgesics before surgery, (4) did not undergo preoperative pain assessment, or (5) were lost to follow-up. The study protocol was approved by the Medical Ethics Committee of Shanghai Pulmonary Hospital (L21-307), and registered in Chinese Clinical Trial Registry (ChiCTR2100052380).
Exposure Variable
Serum 25(OH)D levels were measured within the week before surgery. Patients were divided into two groups based on whether they had a sufficient (≥30 nmol/L) or low (<30 nmol/L) 25(OH)D level.
Outcome Variables
Pain scores (numerical rating scale) were collected in surgical wards every 12 hours after surgery. Laboratory tests for C-reactive protein (CRP), interleukin (IL)-1, IL-6, and tumor necrosis factor (TNF)-α levels were routinely performed before surgery and on postoperative day (POD) 1 and 2; results were recorded on postoperative test sheets. Postoperative follow-up assessments in the third month were conducted by assistants through telephone. Patients with a pain score of >3 within 48 hours after surgery (immediate postoperative period) were considered to have moderate-severe pain. The primary outcome was the incidence of moderate-severe pain in the immediate postoperative period. Secondary outcomes included the levels of CRP, IL-1, IL-6, and TNF-α in the immediate postoperative period, as well as pain scores at 3 months after surgery.
Covariates
Patient demographic characteristics (age, sex, body mass index [BMI]), educational time, comorbidities (eg, hypertension, diabetes mellitus, coronary disease), smoking status, American Society of Anesthesiologists grade, and pain dimension score of the Quality of Recovery (QoR)-40 scale were collected by assistants before surgery. The pain dimension of the QoR-40 scale was used to assess preoperative pain.
Intraoperative data (type of surgery, regional anesthesia, sufentanil consumption, preoperative location, lymph node dissection) were recorded by anesthesiologists in the operating room during surgery. The nerve block method for each patient was selected by the anesthesiologist before surgery. The type of surgery, preoperative location, and need for intraoperative lymph node dissection were determined by the surgeon according to the patients’ situation. Postoperative data including pathological diagnosis, remedial analgesia incidence, and duration of hospital stay were obtained from medical records. Remedial analgesia was considered to have occurred upon the administration of analgesic medications, such as non-steroidal anti-inflammatory drugs.
Postoperative Pain Management
Postoperative pain was managed via patient-controlled intravenous analgesia, which consisted of sufentanil (100 μg) diluted with normal saline to 100 mL; the background dose was 1 mL/h, the self-controlled additional dose was 2 mL, and the locking time was 10 min. Postoperative nausea and vomiting were prevented by the administration of dexamethasone (5 mg) during induction and ondansetron (4 mg) before completion of the surgery.
Statistical Analysis
Missing values for baseline characteristics and secondary outcomes were imputed using the linear regression method. Normally distributed continuous variables are presented as mean ± standard deviation. Non-normally distributed continuous variables are expressed as median and interquartile range. The two-sample t-test or Mann–Whitney U-test was used to analyze data. Categorical data are reported as frequencies and proportions, which were compared with the Chi-square test.
A stepwise multivariable logistic regression model was used to analyze the association between the vitamin D level and postoperative moderate-severe pain; the P-values for entry and removal of variables were 0.05 and 0.10, respectively. We adjusted for possible confounding variables, including age, sex, BMI, educational time, and smoking status. A multiple imputation method was used for missing values for the covariates in the adjusted statistical models. Statistical analyses were performed with SPSS version 26.0 (IBM, Armonk, NY, USA). P < 0.05 was considered to be statistically significant.
Results
A total of 194 adult patients underwent elective non-cardiac thoracic surgery in the Shanghai Pulmonary Hospital between February 2021 and June 2021, with 189 patients having undergone a 25(OH)D test within a week before surgery. Following application of the exclusion criteria, 135 patients who underwent uniportal video-assisted thoracoscopic surgery were included in the final analysis (Figure 1).
 |
Figure 1 Flowchart of patient enrollment and follow-up. |
Among 135 patients, 54.1% were categorized as having a low vitamin D level (<30 nmol/L). The mean age of the patients with a low vitamin D level was 57.5 years, and 53.4% were female. There were no significant differences in demographic, intraoperative, or postoperative parameters between patients with low and sufficient vitamin D levels (P > 0.05) (Table 1).
 |
Table 1 Baseline Characteristics Based on Serum Vitamin D Level |
Primary Outcomes
Postoperative moderate-severe pain was observed in 57 (42.2%) patients (sufficient 25[OH]D group, 19 [30.6%]; low 25[OH]D group, 38 [52.1%]) in the immediate postoperative period (Table 2). After adjusting for potential confounders, patients with low 25(OH)D levels (<30 nmol/L) had a higher risk of postoperative moderate-severe pain (adjusted odds ratio, 2.44; 95% confidence interval, 1.181–5.041; P = 0.016) compared to patients with sufficient 25(OH)D levels (Figure 2).
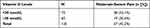 |
Table 2 The Number of Patients with Moderate-Severe Pain in the Immediate Postoperative (48 Hours) Period Stratified by Vitamin D Levels |
Secondary Outcomes
The serum levels of CRP, IL-1, IL-6, and TNF-α were not significantly different between patients with low and sufficient 25(OH)D levels before surgery or on POD1 or POD 2 (Table 3). There were also no significant differences in static or dynamic pain scores at 3 months after surgery (Table 4).
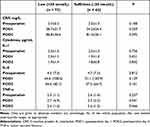 |
Table 3 Secondary Outcomes - Levels of CRP and Cytokines |
 |
Table 4 Secondary Outcomes - Pain Scores at 3 Months After Surgery |
Discussion
In this study, we found that low vitamin D levels (<30 nmol/L) among patients who underwent video-assisted thoracoscopic surgery were associated with increased postoperative moderate-severe pain in the immediate postoperative (48 hours) period when compared to those with sufficient vitamin D levels (≥30 nmol/L). This association remained significant after adjustment for potential confounding factors including age, sex, BMI, educational time, and smoking status. Although the levels of CRP, IL-1, IL-6, and TNF-α in patients with low vitamin D levels were higher than those with sufficient levels, the differences were not statistically significant. To the best of our knowledge, this is the first study to describe the relationship between vitamin D levels and acute postoperative pain after non-cardiac thoracic surgery. Furthermore, our study also explored whether postoperative inflammation is a potential mechanism by which vitamin D affects acute postoperative pain.
To date, the association between vitamin D levels and postoperative pain has remained unclear; while a few studies have reported an association, other studies have failed to observe a relationship between these two parameters. Song et al conducted a retrospective study of 226 postmenopausal women who underwent primary total knee arthroplasty. They reported that vitamin D deficiency was a risk factor for postoperative pain at 3 months after surgery.8 However, in an observational study, Bose et al did not observe a link between vitamin D levels and postoperative pain after laparoscopic bariatric surgery.20 This discrepancy may be attributed to differences in patient populations, particularly in terms of vitamin D levels and the types of surgery performed. The standard threshold value for vitamin D deficiency (<50 nmol/L) was lower than the median vitamin D level in the study conducted by Bose et al. Furthermore, the surgical procedure they estimated was less painful, which may have caused the differences in outcomes to be less evident.20 Both may have contributed to the difference in results. According to previous studies, patients with lower vitamin D levels (<30 nmol/L) are more likely to benefit from vitamin supplements, thus indicating that these patients may suffer from more severe pain.21,22 Therefore, the connection between vitamin D levels and postoperative pain may be more obvious in patients with severer pain and lower vitamin D levels.
The underlying mechanisms linking vitamin D and the degree of pain are currently unclear. Both clinical and animal studies suggest that vitamin D inhibits the synthesis of prostaglandin E2 and decreases the level of pain-related cytokines including TNF-α, IL-6, and leukotriene B4.5,23–25 We failed to demonstrate that the inflammatory response is a potential mechanism for the association between vitamin D levels and postoperative pain. This may be attributed to the small sample size and large amount of missing data in our study. In addition, vitamin D may affect peripheral and central nerve functions, as well as the perception and processing of pain.26,27 It is worth mentioning that ultraviolet B light can induce endogenous opioids in the skin (endorphins) and has strong analgesic effects; this suggests that vitamin D levels may be simply a consequence of ultraviolet B light exposition.28 While this appears to explain the results of our observational study, this interpretation contradicts the positive effects of vitamin D supplementation on pain management demonstrated by previous RCTs and meta-analyses.21,29,30
The current study has several limitations. First, the range of vitamin D levels in the patients was far lower than the standard threshold value for vitamin D deficiency (<50 nmol/L). Thus, it may not be possible to extrapolate our results to other patient populations. Second, our data set had a large number of missing values, since we excluded patients who were lost to follow-up and were without vitamin D level data.
Conclusion
In summary, our results suggest that patients with low vitamin D levels are at a higher risk of acute moderate-severe pain after video-assisted thoracoscopic surgery. This finding highlights an underlying risk factor that can be used to predict patients who are likely to have more severe postoperative pain. Further clinical trials should be conducted to confirm the association between vitamin D and postoperative pain.
Abbreviations
BMI, body mass index; CRP, C-reactive protein; IL, interleukin; POD, postoperative day; QoR-40, Quality of Recovery-40; RCT, randomized controlled trial; 25(OH)D, 25-hydroxy-vitamin D; TNF-α, tumor necrosis factor-α.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Medical Ethics Committee of Shanghai Pulmonary Hospital (L21-307) and the written informed consent was waived. At the same time, this study conforms to the principles outlined in the Declaration of Helsinki.
Author Contributions
XZ and XC collected the clinical data and participated in the design of the study. CL participated in the designing the study and supervised the analyses of the research data. HS designed the study and drafted the manuscript. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Shanghai Special Program for Research on Aging and Women and Children’s Health (No. 2020YJZX0136), Shanghai Committee of Science and Technology Project (21Y11906100), and Talent Program of Shanghai Pulmonary Hospital (No. fkgg1809, HL-C6).
Disclosure
XZ, XC, CL and HS declare that they have no competing interests in this work.
References
1. van Schoor N, Lips P. Global overview of vitamin D status. Endocrin Metab Clin. 2017;46(4):845–870. doi:10.1016/j.ecl.2017.07.002
2. Roth DE, Abrams SA, Aloia J, et al. Global prevalence and disease burden of vitamin D deficiency: a roadmap for action in low- and middle-income countries. Ann Ny Acad Sci. 2018;1430(1):44–79. doi:10.1111/nyas.13968
3. Holick MF. Vitamin D deficiency. New Engl J Med. 2007;357(3):266–281. doi:10.1056/NEJMra070553
4. Hewison M. Antibacterial effects of vitamin D. Nat Rev Endocrinol. 2011;7(6):337–345. doi:10.1038/nrendo.2010.226
5. Liu X, Nelson A, Wang X, et al. Vitamin D modulates prostaglandin E-2 synthesis and degradation in human lung fibroblasts. Am J Respir Cell Mol Biol. 2014;50(1):40–50. doi:10.1165/rcmb.2013-0211OC
6. Wang TT, Nestel FP, Bourdeau W, et al. Cutting edge: 1,25-dihydroxyvitamin D-3 is a direct inducer of antimicrobial peptide gene expression. J Immunol. 2004;173(5):2909–2912. doi:10.4049/jimmunol.173.5.2909
7. Habib AM, Nagi K, Thillaiappan NB, Sukumaran V, Akhtar S. Vitamin D and its potential interplay with pain signaling pathways. Front Immunol. 2020;11. doi:10.3389/fimmu.2020.00820
8. Song Y, Liu S-F, Wu Z, Wang M, Cong R-J, Tao K. Effects of preoperative serum vitamin D levels on early clinical function outcomes and the moderate-to-severe pain prevalence in postmenopausal women after primary total knee arthroplasty. Menopause. 2021;28(8):893–898. doi:10.1097/GME.0000000000001789
9. Matossian-Motley DL, Drake DA, Samimi JS, Camargo CA, Quraishi SA. Association between serum 25(OH)D level and nonspecific musculoskeletal pain in acute rehabilitation unit patients. J Parenter Enteral Nutr. 2016;40(3):367–373. doi:10.1177/0148607114555909
10. Bergman P, Sperneder S, Hoijer J, Bergqvist J, Bjorkhem-Bergman L, Ikeda K. Low vitamin D levels are associated with higher opioid dose in palliative cancer patients--results from an observational study in Sweden. PLoS One. 2015;10(5):e0128223. doi:10.1371/journal.pone.0128223
11. Knutsen KV, Brekke M, Gjelstad S, Lagerlov P. Vitamin D status in patients with musculoskeletal pain, fatigue and headache: a cross-sectional descriptive study in a multi-ethnic general practice in Norway. Scand J Prim Health Care. 2010;28(3):166–171. doi:10.3109/02813432.2010.505407
12. McCarty DE, Reddy A, Keigley Q, Kim PY, Cohen S, Marino AA. Nonspecific pain is a marker for hypovitaminosis D in patients undergoing evaluation for sleep disorders: a pilot study. Nat Sci Sleep. 2013;5:37–42. doi:10.2147/NSS.S42641
13. Morioka TY, Lee AJ, Bertisch S, Buettner C. Vitamin D status modifies the association between statin use and musculoskeletal pain: a population based study. Atherosclerosis. 2015;238(1):77–82. doi:10.1016/j.atherosclerosis.2014.11.012
14. Lotfi A, Abdel-Nasser AM, Hamdy A, Omran AA, El-Rehany MA. Hypovitaminosis D in female patients with chronic low back pain. Clin Rheumatol. 2007;26(11):1895–1901. doi:10.1007/s10067-007-0603-4
15. Atherton K, Berry DJ, Parsons T, Macfarlane GJ, Power C, Hypponen E. Vitamin D and chronic widespread pain in a white middle-aged British population: evidence from a cross-sectional population survey. Ann Rheum Dis. 2009;68(6):817–822. doi:10.1136/ard.2008.090456
16. Kim Y, Zhang F, Su K, et al. Perioperative serum 25-hydroxyvitamin D levels as a predictor of postoperative opioid use and opioid use disorder: a cohort study. J Gen Intern Med. 2020;35(9):2545–2552. doi:10.1007/s11606-020-06001-y
17. Wu ZQ, Malihi Z, Stewart AW, Lawes CMM, Scragg R. Effect of vitamin D supplementation on pain: a systematic review and meta-analysis. Pain Physician. 2016;19(7):415–427.
18. Gao XR, Chen YS, Deng W. The effect of vitamin D supplementation on knee osteoarthritis: a meta-analysis of randomized controlled trials. Int J Surg. 2017;46:14–20. doi:10.1016/j.ijsu.2017.08.010
19. Hajimohammadebrahim-Ketabforoush M, Shahmohammadi M, Khoundabi B, Shariatpanahi ZV. Effect of vitamin D supplementation on postcraniotomy pain after brain tumor surgery: a randomized clinical trial. World Neurosurg. 2019;130:E105–E111. doi:10.1016/j.wneu.2019.05.250
20. Bose S, Khanna A, You J, Arora L, Qavi S, Turan A. Low serum vitamin D levels are not associated with increased postoperative pain and opioid requirements: a historical cohort study. Can J Anaesth. 2015;62(7):770–776. doi:10.1007/s12630-015-0357-4
21. Helde-Frankling M, Bjorkhem-Bergman L. Vitamin D in Pain Management. Int J Mol Sci. 2017;18(10):2170. doi:10.3390/ijms18102170
22. Shipton EE, Shipton EA. Vitamin D deficiency and pain: clinical evidence of low levels of vitamin D and supplementation in chronic pain states. Pain Ther. 2015;4(1):67–87. doi:10.1007/s40122-015-0036-8
23. Gendelman O, Itzhaki D, Makarov S, Bennun M, Amital H. A randomized double-blind placebo-controlled study adding high dose vitamin D to analgesic regimens in patients with musculoskeletal pain. Lupus. 2015;24(4–5):483–489. doi:10.1177/0961203314558676
24. Qin W, Smith C, Jensen M, Holick MF, Sauter ER. Vitamin D favorably alters the cancer promoting prostaglandin cascade. Anticancer Res. 2013;33(9):3861–3866.
25. Xu H-W, Zhang S-B, Yi Y-Y, et al. Relationship between vitamin D and nonspecific low back pain may be mediated by inflammatory markers. Pain Physician. 2021;24(7):E1015–E1023.
26. Kuru P, Akyuz G, Yagci I, Giray E. Hypovitaminosis D in widespread pain: its effect on pain perception, quality of life and nerve conduction studies. Rheumatol Int. 2015;35(2):315–322. doi:10.1007/s00296-014-3099-7
27. von Kanel R, Muller-Hartmannsgruber V, Kokinogenis G, Egloff N. Vitamin D and central hypersensitivity in patients with chronic pain. Pain Med. 2014;15(9):1609–1618. doi:10.1111/pme.12454
28. Fell GL, Robinson KC, Mao J, Woolf CJ, Fisher DE. Skin beta-endorphin mediates addiction to UV light. Cell. 2014;157(7):1527–1534. doi:10.1016/j.cell.2014.04.032
29. Zarrati M, Sohouli MH, Aleayyub S, et al. The Effect of Vitamin D Supplementation on Treatment-Induced Pain in Cancer Patients: a Systematic Review. Pain Manag Nurs. 2022;23(4):458–466. doi:10.1016/j.pmn.2022.02.001
30. Ali M, Uddin Z, Hossain A. Combined effect of vitamin D supplementation and physiotherapy on reducing pain among adult patients with musculoskeletal disorders: a quasi-experimental clinical trial. Front Nutr. 2021;8. doi:10.3389/fnut.2021.717473
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

