Back to Journals » Clinical and Experimental Gastroenterology » Volume 12
Preoperative high C-reactive protein level is associated with an increased likelihood for conversion from laparoscopic to open appendectomy in patients with acute appendicitis
Authors Shimoda M, Maruyama T , Nishida K, Suzuki K, Tago T, Shimazaki J, Suzuki S
Received 30 November 2018
Accepted for publication 1 March 2019
Published 5 April 2019 Volume 2019:12 Pages 141—147
DOI https://doi.org/10.2147/CEG.S196471
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Wing-Kin Syn
Mitsugi Shimoda, Tsunehiko Maruyama, Kiyotaka Nishida, Kazuomi Suzuki, Tomoya Tago, Jiro Shimazaki, Shuji Suzuki
Department of Gastroenterological Surgery, Tokyo Medical University, Ibaraki Medical Center, Ami, Ibaraki, Japan
Background: Laparoscopic appendectomy (LA) has been increasingly adopted for its advantages over the open appendectomy, but there are possibilities of conversion from laparoscopic to open appendectomy (CA) if the patients had complicated appendicitis concurrently, or when the extent of inflammation prohibits successful procedure. In this retrospective study, we aimed to clarify the preoperative predictors for CA.
Patients and methods: From January 2010 to April 2016, medical records of 93 consecutive patients who underwent LA for suspected appendicitis were reviewed retrospectively. Factors evaluated were age, gender, body mass index, C-reactive protein (CRP), white cell count, albumin, Neutrophil count, lymphocyte count, Neutrophil/lymphocyte ratio, preoperative CT imaging (abscess formation: yes/no, appendicolith: yes/no), operative factors (time to operation, amount of bleeding), length of hospital stay, period until oral intake after surgery, and period from initial symptoms to surgery.
Results: CA occurred in nine patients (9.7%). The reason for conversion was severe dense adhesion in two cases, inadequate exposure of appendix in two cases, uncompleted appendectomy in two cases, perforated appendicitis in one case, gangrenous appendicitis in one case, and abscess formation in one case. Based on 93 patients evaluated by preoperative CT scan, significant factors in the final multivariate analysis associated with CA was CRP [odds ratio=1.13, 95% CI:1.00–1.28, p=0.04].
Conclusion: Identifying the potential factors for conversion preoperatively may assist the surgeons in making decisions concerning the management of patients with appendicitis and in the judicious use of LA.
Keywords: laparoscopic, conversion, appendectomy, C-reactive protein
Introduction
Laparoscopic surgery is the preferred approach for many abdominal surgeries because of reduced postoperative incisional pain, short hospital stay, and improved cosmetic which follows a successful operation compared with standard open surgery.
Laparoscopic appendectomy (LA) was first published in an article reporting the first complete removal of the appendix using the laparoscopic technique in 1983,1 and Schreiber2 performed the first LA in a patient with acute appendicitis for women in 1987. The technique of LA has improved during the last decade, and the number of patients undergoing LA increased rapidly. LA also has been extended to complicated appendicitis. However, there were several occasions where conversion from laparoscopic to open appendectomy (CA) was necessary.
CA rates were about 0–17% in the previous reports,3–9 and some reports described that independent risk factors which lead to CA were age, male sex, diabetes, obesity, high C-reactive protein (CRP), low white cell count (WBC), base necrosis, and acute appendicitis with abscess or peritonitis.7–10 CA increases medical costs and operative times; furthermore, from our experience CA compromises the benefits of the laparoscopic approach and outcomes, such as fewer surgical site infections and shortened hospital stays. Thus, preoperative criteria or risk factors that can be used to decide the ideal operative approach for individual patients are required.
In this retrospective study, we evaluated the preoperative risk factors and radiological inflammatory findings by computed tomography (CT), to identify parameters that may prove useful in predicting the failure of LA.
Patients and methods
Patient population and selection
From 2010, we started and indicated LA procedure for acute appendicitis cases, and our eligibility criteria for LA were all cases of acute appendicitis. The number of LA cases were increasing year by year from 2010.
From January 2010 to April. 2016, a total of 93 LA were performed in our medical center, and the patients and their operational outcomes were retrospectively analyzed in this study.
Prior to surgery, all patients were subjected to clinical examination, blood and urine screening, and to physical examination of the abdomen. Preoperative CT was routinely carried out in all patients. We diagnosed in acute appendicitis from CT findings, elevated WBC and CRP, and with abdominal physical findings. If the patients had free air or ascites and suspected appendiceal carcinoma as a result of the preoperative diagnosis, we selected conventional open appendectomy. Some patients’ received interval appendectomy, which was defined as appendectomy after 7 days or more since the initial symptoms.
Surgical procedure
All operations were performed by a team of two surgeons, at least one supervisor must be scrubbed in the operation. They were adequately experienced in the open as well as the laparoscopic approach.
LA was performed using a standardized three-trocar approach (umbilical, 12 mm port; suprapubic, 5 mm port; and optional lower-left quadrant, 5 mm port) under general anesthesia. With the patient in the Trendelenburg position and right side up, the small bowel was retracted away from the lower right quadrant. An inflammatory mass or hard adhesions, if present, was dissected gently with blunt instruments. The appendix was divided using pretied loops (Endoloops, Ethicon, Johnson and Johnson, Arlington, TX, USA) and removed through 12 mm port, in general with use of a Memo bag (Teleflex, Tokyo, Japan). Generally, intraperitoneal irrigation was performed in all cases. Particularly in case of an abscess or perforated appendix, the lower-left quadrant, right paracolic gutter, and pelvis were irrigated with 1–2 L of physiological saline and was inserting continuous irrigation drain. In conversion appendectomy group (CA G), all of the cases were celiotomy by pararectal incision, stump was close by serosa-muscle interrupted sutures. We performed abdominal lavages with more than 5 L of physiological saline solution to avoid abscess formation, and were inserting continuous irrigation drain in the pelvic cavity. Blood loss was measured by the circulating nurse from suction volume or the weight of the gauze.
Study design
We evaluated clinical and operative factors in all of the 93 patients. We divided the patients into two groups; LA group (LA G) and CA G, and clinical factors were selected and compared between the two groups. Clinical factors included age, gender, body mass index (BMI), albumin (Alb), CRP, neutrophil to lymphocyte ratio (NLR), WBC, and pathological findings. We compared with both group according to the procedure, such as, time to surgery (TS), operative factors (operating time and amount of blood loss), length of hospital stay (LHS), period until start of ingestion (PSI), postoperative complication and interval appendectomy, and also compared both groups with and without an appendicolith and abscess on preoperative CT findings.
The study was approved by the research and ethics committee at the Tokyo Medical University, Ibaraki Medical Center (Number: 16–34). The patients who completed follow-ups were also included in the study. As this is a retrospective non-intervention study, the institutional review board waived the need for written informed consent from all patients. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1995 Helsinki Declaration.
Statistics
Statistical analyses were performed with the SPSS statistical software package (version 24.0; SPSS Inc., Chicago, IL). Median was used to define laboratory parameters such as age, gender, BMI, Alb, CRP, NLR, WBC, operating time, amount of blood loss, PSI,, and LHS. Univariate and multivariate analyses were performed to clarify the laboratory parameter and clinical factors most significantly associated with LA G and CA G. Univariate and multivariate analyses, Mann–Whitney U-test, and Fisher’s exact test were utilized, and odds ratios with 95% CI were calculated using logistic regression model analyses. P-values of less than 0.05 were considered to be statistically significant.
Results
From January 2006 to April 2016, a total of 186 cases were performed appendectomy in our medical center, 93 patients underwent LA and another 93 cases had open appendectomies (OA) under acute appendicitis. The CA occurred in 9 of 93 patients (9.7%) (Figures 1 and 2).
 | Figure 1 Number of laparoscopic appendectomies and open appendectomies during the study period. Abbreviations: OA, open appendectomy; LA, laparoscopic appendectomy. |
Characteristics of CA G groups
There were one female and eight male, and the median age was 51.4 years old (range: 17–71). Reason of conversion from LA to CA was severe dense adhesion in two cases, inadequate exposure of appendix in two cases, uncompleted appendectomy in two cases, perforated appendicitis in one case, gangrenous appendicitis in one case, and abscess formation in one case. All of the nine patients received conventional appendectomy, however, one patient needed additional surgery because the patient had appendiceal cancer according to the pathological findings.
Comparing LA G and CA G
Bivariate analysis
Preoperative characteristics
BMI and CRP were significantly higher and longer in CA G than in LA G (p=0.01 and 0.001). Preoperative Alb level was significantly lower in CA G than in LA G (p=0.04). Patients with histological gangrenous presented the highest in CA G: p=0.002 and 0.01: Table 1).
 | Table 1 The characteristics before and after surgery according to the procedure |
Operative and postoperative factors
Operating time, amount of bleeding, LHS and PSI were significantly higher and longer in CA G than in LA G (p=0.0001, 0.0001, 0.002 and 0.002: Table 2). Patients with an abscess in CT image presented the highest in CA G: p=0.002: Table 2).
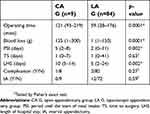 | Table 2 The outcomes according to the procedure |
Multivariate analysis
CRP level was an only significant adverse prognostic factor in multivariate analysis (odds ratio 1.13; 95% CI; 1.00–1.28, p=0.04: Figure 3, Table 3).
 | Table 3 Multivariable analysis clinical and operative factors according to the procedure |
Discussion
There have been several advancements in laparoscopic surgery during the last decade. These improvements have contributed to some advantages of LA over the OA, including reduced blood loss and improved postoperative morbidity rate. On the other hand, the disadvantages associated with the increase of LA are the use of disposable instruments which adds to the cost and increases the operating time compared to OA. Furthermore, there were occasions where LA cases had to be converted to open laparotomy. We believe that several factors could have played a role regarding this conversion, such as initial patient selection which can improve with better and more accurate preoperative diagnostic through CT scans, and an improved learning curve of surgical staff. But even so, conversion to laparotomy is unavoidable in some cases, and the conversion rate according to previous reports was about 0–17%.3–9 The major reason for conversion to laparotomy was inadequate exposure of appendix, bleeding, and iatrogenic bowel injuries according to previous reports.11–14
Some of the retrospective reports identified predictors of where conversion would be necessary from LA to open. The predictors were age, male, symptom duration, WBC over 20,000, surgeon experience, and CT scans findings.8,12,14 The conclusion from our study, CA was lengthened the operative time, delayed meal intake, increasing blood loss, and leads to a longer hospital stay.
CT finding is one of the important factors for determination of procedure for an appendectomy. Tuggle et al, defined the CT grading system through acute appendicitis using 6-point (0–5) scale.15 Several authors have evaluated this grading system for CA compared to LA. The patients had a fluid collection and/or abscess formation of the grade of 4 and 5, and those patients had a significantly higher risk of conversion.9,12 In the present study, abscess formation is considered as one of the risk factors for CA. OA was also our first choice to those patients who had surgery previously or had an obvious case of abscess formation through CT.
What this study adds is that a significantly elevated CRP of >9.9 mg/dL is also an independent risk factor for conversion from LA to CA. Only two studies verify CRP as a marker for conversion from LA.7,9 Those two papers described that preoperative CRP of >100 and >150 mg/L were a statistically significant predictor of CA. CRP is body’s acute phase inflammatory markers. A higher level of CRP is therefore suggestive of a more intense local inflammatory reaction and more severe acute appendicitis. We theorize that this is due to inflammatory and/or infective components, and it may be correlated with perforating appendix or abscess. Patients with high CRP should undergo abdominal CT and suspected gangrenous appendicitis and/or abscess formation. In order to build on this concept, our study shows that not only does a high CRP make the procedure more challenging technically but it also increases the chance of complications arising in the LA group.
Conclusion
Our study has identified that high CRP (more than 9.9 mg/dL) is associated with an increased likelihood for LA to CA in patients with acute appendicitis. We suggested that if the patients had high CRP level with abscess formation or gangrenous appendicitis on CT findings, we recommend the first approach to the conventional appendectomy for those patients.
Abbreviations list
LA, laparoscopic appendectomy; OA, open appendectomy; CA, conversion from laparoscopic to open appendectomy.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Semm K. Endoscopic appendectomy. Endoscopy. 1983;15(2):59–64. doi:10.1055/s-2007-1021466
2. Schreiber JH. Early experience with laparoscopic appendectomy in women. Surg Endosc. 1987;1(4):211–216.
3. Schlottmann F, Sadava EE, Pena ME, Rotholtz NA. Laparoscopic appendectomy: risk factors for postoperative intraabdominal abscess. World J Surg. 2017;41(5):1254–1258. doi:10.1007/s00268-017-3869-y
4. Lee SM, Hwang GS, Lee DS. Single-incision laparoscopic appendectomy using homemade glove port at low cost. J Minim Access Surg. 2016;12(2):124–128. doi:10.4103/0972-9941.169979
5. Popa D, Soltes M, Uranues S, Fingerhut A. Are there specific indications for laparoscopic appendectomy? A review and critical appraisal of the literature. J Laparoendosc Adv Surg Tech A. 2015;25(11):897–902. doi:10.1089/lap.2014.0624
6. Kucuk GO. Technical and social challenges of laparoscopic appendectomy performed in a rural setting. Ann Ital Chir. 2015;86(4):344–348.
7. Shelton JA, Brown JJ, Young JA. Preoperative C-reactive protein predicts the severity and likelihood of complications following appendicectomy. Ann R Coll Surg Engl. 2014;96(5):369–372. doi:10.1308/003588414X13946184901722
8. Gomes CA, Junior CS, Costa EDF, et al. Lessons learned with laparoscopic management of complicated grades of acute appendicitis. J Clin Med Res. 2014;6(4):261–266. doi:10.14740/jocmr1837w
9. Abe T, Nagaie T, Miyazaki M, Ochi M, Fukuya T, Kajiyama K. Risk factors of converting to laparotomy in laparoscopic appendectomy for acute appendicitis. Clin Exp Gastroenterol. 2013;6:109–114. doi:10.2147/CEG.S41571
10. Finnerty BM, Wu X, Giambrone GP, et al. Conversion-to-open in laparoscopic appendectomy: a cohort analysis of risk factors and outcomes. Int J Surg. 2017;40:169–175. doi:10.1016/j.ijsu.2017.03.016
11. Fleming CA, Kearney DE, Moriarty P, Redmond HP, Andrews EJ. An evaluation of the relationship between Enterobius vermicularis infestation and acute appendicitis in a paediatric population – a retrospective cohort study. Int J Surg. 2015;18:154–158. doi:10.1016/j.ijsu.2015.02.012
12. Gupta N, Machado-Aranda D, Bennett K, Mittal VK. Identification of preoperative risk factors associated with the conversion of laparoscopic to open appendectomies. Int Surg. 2013;98(4):334–339. doi:10.9738/INTSURG-D-13-00058.1
13. Nielsen LBJ, Tengberg LT, Bay-Nielsen M. Laparoscopy in major abdominal emergency surgery seems to be a safe procedure. Dan Med J. 2017;64:5.
14. Liu SI, Siewert B, Raptopoulos V, Hodin RA. Factors associated with conversion to laparotomy in patients undergoing laparoscopic appendectomy. J Am Coll Surg. 2002;194(3):298–305.
15. Tuggle KR, Ortega G, Bolorunduro OB, et al. Laparoscopic versus open appendectomy in complicated appendicitis: a review of the NSQIP database. J Surg Res. 2010;163(2):225–228. doi:10.1016/j.jss.2010.03.071
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.