Back to Journals » Cancer Management and Research » Volume 12
Preoperative Combined Prediction Models Have Superior Capability in Predicting Survival as the Child-Pugh Grade in Patients with HCC after Interventional Embolotherapy
Authors Xu MQ, Dai JJ, Jiang ZS, Xu F, Wang L, Zhang WJ , Guo ZG
Received 10 August 2020
Accepted for publication 27 October 2020
Published 7 December 2020 Volume 2020:12 Pages 12537—12547
DOI https://doi.org/10.2147/CMAR.S274970
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eileen O'Reilly
Meng Qing Xu,1,* Jin Jin Dai,2,* Zhi Sheng Jiang,3 Fang Xu,1 Long Wang,1 Wen Jie Zhang,4 Zhi Guo Guo1
1Department of Gastroenterology, Suzhou Hospital of Anhui Medical University, Suzhou, Anhui 234000, People’s Republic of China; 2Department of Infection, Suzhou Hospital of Anhui Medical University, Suzhou, Anhui, 234000, People’s Republic of China; 3Department of Cardiothoracic Surgery, Jinling Hospital, Nanjing 210000, People’s Republic of China; 4Department of Pathology, School of Medicine, Shihezi University, Shihezi, Xinjiang 832002, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhi Guo Guo
Suzhou Hospital of Anhui Medical University, Suzhou, Anhui 234000, People’s Republic of China
Email [email protected]
Background: It is of important clinical significance for hepatocellular carcinoma (HCC) patients to evaluate prognosis before interventional embolotherapy.
Methods: A total of 106 patients with HCC after interventional embolotherapy who had complete data with follow-up information until September 2019 were included in this study. These data were analyzed using SPSS Version 22.0 and R (version 3.6.1) statistical software.
Results: 1) The diameter of the tumor, ascites, FIT, AFP, ALT, AST, GGT, and Child–Pugh score had the ability to predict the prognosis and survival of patients with HCC. Among these molecules, the predictive effectiveness (or the area under the receiver operating characteristic [ROC] curve) of GGT was the highest, although it was slightly lower than the predictive effectiveness of the Child–Pugh score, which is the gold standard for survival analysis. 2) Among survival analyses combining five molecular indicators, the predictive postoperative viability for combination 1 was the strongest with an area under the ROC curve (AUC) of 0.856 (0.779, 0.932), similar to the all-molecular combination (combination 16) with an AUC of 0.872 (0.798, 0.945), but much higher than that of the Child–Pugh score of 0.720 (0.616, 0.823) for HCC patients (all p< 0.05). 3) Kaplan–Meier analyses showed that the 3-year cumulative survival rates were 55.3% for low-risk patients and 2.6% for high-risk patients.
Conclusion: A combined prediction model can determine the optimal combination of preoperative routine detection indices in patients with HCC intervention, and ROC curve analysis can quantify the efficacy of these indices in the survival and prognosis of HCC. Interestingly, combination 1 showed stronger predictive capability than the Child–Pugh score in predicting death risks for postoperative patients with HCC. When combination 1 has several missing clinical data, these combination prediction models (12, 3, 7, 13, 16) are also a replaceable choice. These findings may have important clinical significance in the formulation of individualized medical programs.
Keywords: hepatocellular carcinoma after interventional embolotherapy, preoperative combined prediction model, survival prognosis, death risk, Child–Pugh score
Introduction
Liver cancer is very common in China, posing a threat to public health. According to the Global Cancer Statistics 2018, an estimate of 392,868 new liver cancer cases and 368,960 deaths occurred in China, accounting for 46.7% and 47.2% of the world, respectively, with high morbidity and mortality ranks.1,2 In recent years, with the advancement of science and technology and the increase in people’s awareness of health, the morbidity and mortality in patients with liver cancer have been controlled. However, the situation remains severe. Without routine screening, early diagnosis of hepatocellular carcinoma (HCC) is difficult, and treating late-stage HCC is often unsatisfactory, resulting in poor survival.3 Cancer invasion and metastasis are the major causes of death in patients with HCC,4,5 and interventional embolotherapy for metastatic tumors is routine management.6 Therefore, it is undoubtedly of great significance for these patients to carry out research on the factors affecting the prognosis of HCC after interventional embolotherapy, and to construct a predictive model for the prognosis of HCC.
As we all know, the main treatment for patients with advanced HCC is interventional embolotherapy, chemotherapy and radiotherapy. There are many studies on the prognosis of HCC surgery, but there are relatively few studies on the survival prognosis of patients after HCC intervention therapy.7,8 The Child–Pugh grade is well established as a prognostic factor for patients with HCC.9 We tried to evaluate the survival of patients with HCC after interventional therapy by combining imaging and blood tests evaluating liver function.10–12 Basic clinical data mainly included: gender, age, FIT, basic physical examination, and related complications such as hepatic encephalopathy. Imaging data mainly included: tumor size, number of tumors, presence or absence of ascites, PVTT, and metastasis. Liver function-related detection indicators mainly include AFP, ALT, AST, TBIL, ALB, ALP, GGT, and the Child–Pugh grade, which have an impact on the prognosis of HCC.
The combined detection13–15 and prediction model can continuously combine multiple detection indicators to evaluate its ability to predict the survival prognosis of patients after HCC intervention therapy, until a model with a small number of combinations, high sensitivity, and specificity is selected for clinical application. The establishment of apreoperative combined detection and prediction model to assess the risk of postoperative HCC patients with high or low mortality will not only provide advice for the doctor to choose a treatment strategy for the patient but also assist in the formulation of individualized medical treatment after intervention.
Materials and Methods
Patients and Follow-Up
A total of 106 patients (2013–2017) with hepatocellular carcinoma after interventional therapy who had complete data with follow-up information until September 2019 were included in this study. These data included basic characteristics of patients, FIT, imaging data (computer tomography and color Doppler ultrasound), and detection of liver function-related indicators (AFP, ALT, AST, ALT/AST, AG, GGT, TBIL, DBIL, IBIL, TP, ALB, GLB, ALP, PAB, TBA, ADA, AFU, PT, and the Child–Pugh score). None of the patients received chemotherapy and/or radiotherapy before interventional embolotherapy. After interventional embolotherapy, HCC patients were followed up for 64 months (5 years and 4 months) with a median follow-up time of 18 months. Overall survival (OS) was defined from the date of interventional embolotherapy until the date of death or the date of the last follow-up.
Examination of Liver Function-Related Indicators
Before interventional embolotherapy, heparinized blood was drawn from patients after fasting overnight, centrifuged, and liver function-related indicators in the plasma was tested using the Roche Automatic biochemical Analyzer (Roche, Shanghai, China).
Statistical Analyses
Data analyses were performed using the statistical software package SPSS, R (version 3.6.1; http://www.R-project.org). The Kaplan–Meier method was used to calculate and plot survival curves, and a two-Log rank test was used to evaluate differences in survival curves. Univariate and multivariate analyses of the relative prognostic importance of the parameters were performed using the Cox proportional hazards model. The Spearman rank correlation method was employed to identify correlations among preoperative and/or postoperative variables. In addition, we first introduced the receiver operating characteristic (ROC) curve and the area under the curve (AUC) to quantify impact weights (or powers) of survival-predicting factors in terms of their differential abilities to predict survival. ROC is a graphical plot that illustrates the performance of a binary classifier system as its discrimination threshold is varied. AUC is a product of considering both sensitivity and specificity of a factor in predicting survival, which can be translated to discriminative power, that is, the larger the AUC, the more powerful the factor that can be used to predict prognosis. Logistics combined with ROC were used to describe the predictive ability of combined detection on prognosis and survival. The cutoff value was used to divide the patients into high-risk and low-risk groups. The Kaplan–Meier method was used to re-verify the ability to evaluate the prognosis model and identify the high and low mortality risk of patients with HCC after interventional embolotherapy. All P values were 2-sided and differences with P<0.05 were considered statistically significant.
Results
Baseline Characteristics of the Participants
A total of 106 patients after HCC intervention therapy were included in this study. There were 88 men and 18 women, accounting for 83.0% and 17.0% of the total cases, respectively. The age ranged from 29 to 85 years, and the median age was 58 years. The average age of the patients was 58.85±11.17 years old. There were 63 cases (59.4%) of Child–Pugh Grade A, 35 cases (33.0%) of Grade B, and 8 cases (7.5%) of Grade C. There were 44 patients (41.5%) who underwent only one interventional embolotherapy, 34 patients (32.1%) underwent two interventional embolotherapy, and 28 (26.4%) had more than three interventional embolotherapy. There were 78 cases (73.6%) with a previous history of cirrhosis. Fifty-three patients (50%) had ascites. Seventy-six patients (71.7%) had splenomegaly. Seven patients (6.6%) had hepatic encephalopathy. In the imaging data, the smallest tumor size was 0.4 cm and the largest was 19.8 cm, the median tumor diameter was 6.6 cm, and the average tumor diameter was 6.80±3.47. There were 65 cases (61.3%) with 3 or more tumors and 39 cases (36.8%) with PVTT. Fifty-eight cases (54.7%) were transferred. In addition, baseline characteristics of liver function-related indicators was shown in (Supplementary Table 1). The longest survival time of patients with HCC after the intervention has reached 64 months. On September 1, 2019, 24 (22.6%) HCC patients were still alive, whereas 82 (77.4%) had died. Follow-up ranged from 0 to 64 months after intervention until September, 2019 and the median follow-up time was 18 months (Supplementary Figure 1).
Correlation Analysis of Various Indices in Patients with HCC
We tested correlations among liver function-related indicators, imaging data, and the Child–Pugh grade. As shown in Supplementary Table 2, positive correlations were observed between the Child–Pugh grade and cirrhosis, splenomegaly, presence of PVTT, presence of ascites, and presence of hepatic encephalopathy, respectively (P<0.01). Negative correlations were found between the Child–Pugh grade and age. Further analysis showed that liver function-related indicators (AFP, ALT, AST, TP, ALB, GLB, PT, TBIL, DBIL, IBIL, GGT, PAB, TBA, and ADA) were positively correlated with the Child–Pugh grade (P<0.01).
Risk Factors Affecting the Prognosis of Patients with HCC
As shown in Table 1, univariate analyses demonstrated that in HCC patients, survival prognosis was associated with tumor diameter, the number of tumors, metastasis, portal vein thrombi, ascites, FIT, AFP, ALT, AST, TBIL, ALB, ALP, GGT, the Child–Pugh grade, and so on (P<0.05). Furthermore, multivariate analyses (Table 2) showed that metastasis (HR=1.911, 95% CI = (1.151, 3.174), P=0.012), portal vein thrombi (HR=1.610, 95% CI = (1.014, 2.557), P=0.043), FIT (≥3 vs. 1, HR=0.400, 95% CI = (0.207, 0.772), P=0.006), GGT (HR=2.132, 95% CI = (1.295, 3.508), P=0.003), and the Child–Pugh grade (B vs A, HR=2.504, 95% CI = (1.533, 4.091), P<0.001; C vs A, HR=2.734, 95% CI = (1.257, 5.945), P=0.011) were independent factors affecting HCC patient survival. The mortality risk of patients with metastasis was 1.911 times that of patients without metastasis, with a 95% CI (1.151, 3.174). The risk of death in patients with portal vein tumor thrombi was 1.610 times that of those without, with a 95% CI (1.014, 2.557). The number of interventional embolotherapy (≥3 times) was a protective factor compared with the number of patients who underwent interventional embolotherapy only once. Patients with GGT (≥79.8) higher than the median were 2.132 times less than the median (<79.8), with a 95% CI (1.295, 3.508). Child–Pugh grade B was 2.504 times higher than A, with a 95% CI (1.533, 4.091). Class C was 2.734 times higher than class A, with a 95% CI (1.257, 5.945).
 |
Table 1 Risk Factors Affecting the Prognosis of Patients with HCC by Cox Single Factor Analysis |
 |
Table 2 Risk Factors Affecting the Prognosis of Patients with HCC by Cox Multiple Factor Regression Analysis |
Basic Information, Imaging Data, and Liver Function Blood Indicators Correlate with Survival in Patients with HCC
Tumor diameter, the number of tumors, metastasis, PVTT, FIT, and ascites have an impact on the prognosis and survival of patients after HCC interventional embolotherapy. Tumor diameter (≥7 cm), the number of tumors (≥3), the presence of metastasis, portal vein tumor embolism, and ascites were associated with poor prognosis in patients with HCC after interventional embolotherapy (P<0.05); patients with only one intervention had a worse prognosis than those with more than three interventions. Therefore, these imaging data can predict the poor prognosis of patients with HCC.
AFP, ALT, AST, TBIL, ALB, ALP, GGT, the Child–Pugh grade, and other indicators have an impact on the prognostic survival of patients after HCC intervention therapy. The survival curve of patients is getting lower and lower, and the prognosis is getting worse. The survival analysis revealed that high expression of AFP, ALT, AST, TBIL, ALB, ALP, and GGT correlated with poor prognosis in HCC. The Child–Pugh grade (including grades B and C) suggests poor prognosis (Supplementary Figure 2).
Predictive Ability of Various Indicators of HCC in Predicting Survival
As shown in Table 3, the numeric value of an AUC represents the power or weight of a risk factor impacting survival prognosis, which we term as impact weight (IW). The higher the AUC/IW of a factor is, the more powerfully that factor impacts on survival prognosis. Tumor diameter (AUC=0.676, P=0.009), ascites (AUC=0.635, P=0.045), FIT (AUC=0.648, P=0.028), AFP (AUC=0.642, P=0.035), ALT (AUC=0.681, P=0.007), AST (AUC=0.670, P=0.012), TBIL, ALB, ALP, GGT (AUC=0.707, P=0.002), and the Child–Pugh grade (AUC=0.720, P=0.001) can predict the postoperative survival of HCC patients, of which GGT has the greatest ability to predict survival time and quality of life of HCC patients, which was slightly lower than the Child–Pugh grade (AUC=0.720, P=0.001).
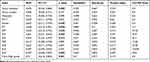 |
Table 3 The Area of ROC Curve Between Various Indexes of HCC Patients |
ROC Curve to Evaluate the Efficacy of Combined Prediction of Postoperative Survival of HCC
The predictive postoperative viability for combination 1 of the Child–Pugh score, FIT, GGT, metastasis, and PVTT (Child–Pugh score + FIT + GGT + metastasis + PVTT) was much higher than a single indicator because the combination produced an AUC of 0.856 (95% CI, 0.779–0.932), which was second only to the combination of imaging data and all liver function indicators (0.872 (0.798, 0.945)), and far higher than the predictive ability of the Child–Pugh grade on the survival of patients with HCC after interventional embolotherapy (0.720 (0.616, 0.823)). We select the most appropriate combination with the best prediction ability and the least indicators from the continuous combination of each indicator. Our results show that combinations 3, 7, 12, and 13 predicted the survival ability of patients after HCC intervention therapy (the AUC was 0.84 (0.758, 0.923), 0.833 (0.741, 0.925), 0.804 (0.697, 0.910), and 0.798 (0.711, 0.885), respectively), P values were all <0.001. We can make the following individualized judgments: we substitute Child–Pugh score + FIT + GGT + metastasis + PVTT into the logistic equation to obtain the combined predicted probability value of the combination for death events, if it is greater than the optimal critical probability value 0.703, then the postoperative outcome of HCC patients can be predicted and evaluated with an accuracy rate of 82.1% (Table 4, Supplementary Figure 3).
 |
Table 4 ROC Curve to Evaluate the Efficacy of Combined Prediction of Postoperative Survival of HCC |
Multi-Factor Combined Detection Predicts the Advantages of Postoperative Survival in HCC
This study combined imaging data and liver function-related indicators to predict the survival prognostic efficacy of HCC after interventional embolotherapy. Predicted low-risk (PLR) and predicted high-risk (PHR) represent the low and high death risk groups in Figure 1, respectively, and the cutoff value of combination prediction probability is taken as the boundary. If postoperative survival time was longer than the cutoff value, it was PHR and less than the cutoff value was PLR. The difference shown in the figure is the difference between the cumulative survival rates of the low- and high-risk groups, reflecting the ability of multi-factor joint detection to distinguish them. The difference shown in the figure represents the difference in cumulative survival among the low- and high-risk groups, reflecting the ability of multifactorial combination detection to distinguish them. Kaplan–Meier method analysis showed that the 3-year cumulative survival rates of the low and high mortality risk groups of combinations 1, 3, 7, 12, 13 and 16 were 55.3%, 2.6%; 47.8%, 2.8%; 46%, 2.7%; 62.5%, 7.5%; 46%, 4.75%; and 46.2%, 0%, respectively.
Discussion
Primary liver cancer is characterized by a high degree of malignancy, strong invasiveness, rapid recurrence, and metastasis. It is difficult to achieve early detection for poor prognosis in the late stage, and high mortality rate.1,2 It seriously endangers the lives and health of our people and causes huge economic burdens and losses.16 Therefore, it is particularly important to study the prognosis of patients with HCC.12 Patients with early HCC often undergo hepatectomy, while patients with advanced HCC often receive only local interventional embolotherapy, with a short postoperative survival time and worse prognosis,6 and there are fewer relevant studies.
Most patients with HCC in our country are accompanied by diagnoses of hepatitis or cirrhosis, and evaluation of liver reserve function is particularly important.17,18 The Child–Pugh score integrates indicators of patients with hepatic encephalopathy, ascites, ALB, TBIL, PT, etc., and is the gold standard for clinical evaluation of liver function. A number of studies have shown that the Child–Pugh score is an independent prognostic factor for multiple treatments and stages of HCC.19–21 This study also showed that the Child–Pugh score was an independent risk factor for survival of BCLC stage B HCC patients treated with TACE.
We followed up patients with HCC for more than 5 years and found that tumor diameter (≥7 cm), the number of tumors (≥3), the presence of metastasis, portal vein tumor thrombi and ascites, FIT (≥3), AFP (≥60.7 ng/mL), ALT (≥46.9 U/L), AST (≥52.8 U/L), ALB (≥35.4 g/L), ALP (≥116.1 U/L), GGT (≥79.8 U/L), the Child–Pugh grade (Grade B+C), etc. (P <0.05) have important significance for the prognosis of patients after HCC intervention therapy.22,23 Among them, metastasis, PVTT, FIT (≥3 times), GGT (≥79.8 U/L), and Child–Pugh grades (Grade B+C) are independent risk factors affecting the postoperative survival of HCC patients. It has been shown that in primary liver cancer, GGT is hypersynthesized in the liver, which can cause a significant increase in blood transpeptidase, even more than 10 times normal.24,25 It is an independent risk factor for predicting the prognosis of HCC after intervention therapy. FIT, the presence of metastasis, and PVTT26 are common clinical risk factors that affect the prognosis.
The area under the ROC curve shows that the Child–Pugh score has the largest area and therefore, the strongest predictive ability. This result suggests that the population is reliable. The predictive power of GGT (the area under the line is 0707) is slightly lower than that of the Child–Pugh score. This shows that the high blood level of GGT has a considerable early warning effect on the survival time of patients after intervention.27
Our main purpose is to use the commonly used clinical indicators to establish a combination of prognostic predictions for patients with HCC that have the best detection effect and a small number of indicators. The area under the ROC of single clinical indicators in this study was lower than that under the Child–Pugh score. This indicated that the predictive ability of a single clinical indicator for survival and prognosis of hepatocellular carcinoma patients after the intervention was lower than that of the Child–Pugh grade. The prediction probability of the combined indicators made using logistic regression was analyzed by ROC curve, and the cutoff value was used to divide the high-risk and low-risk groups. The results show that combination 1 predicts the survival ability of patients after HCC intervention therapy (the AUC is 0.856 (0.779, 0.932)), which is much higher than a single index, second only to combination 16 (0.872 (0.798, 0.945)), and much higher than the predictive ability of the Child–Pugh grade for the survival of patients after HCC intervention therapy (0.720 (0.616, 0.823)). The above research results indicate that we can predict the postoperative survival of patients with HCC through combination 1. We can randomly select a patient and substitute each indicator in combination 1 into the logistic equation to obtain the prediction probability value of the combination to the death event, and determine its critical probability value (Figure 2). Therefore, it can be evaluated with an accuracy rate of 82.1% to determine the possible outcome of the patient as death. The logistic equation can be set to the inherent paper ruler or computer-fixed mode running formula, and directly enter the combined index score to judge the survival and death of the patient under the corresponding accuracy, sensitivity, and specificity. In addition, if the patient is assessed as a high-risk patient, the patient’s next diagnosis and treatment plan (interventional surgery/palliative care) can be clarified.
Kaplan–Meier analyses showed that the cumulative survival rate of the PLR group is higher than that of the PHR group, suggesting that the multi-factor combined prediction group has the ability to distinguish between HCC PHR and PLR groups, with statistical significance. Our results showed that combination 1 had a high difference in predicting the prognosis of HCC, indicating that the combination has a stronger predictive capability in predicting death risks for postoperative HCC patients (see Figure 1).
We have established a multi-factor combined prediction model for HCC patients after interventional embolotherapy, which has important clinical significance for the survival prognosis of patients with HCC.13–15 Combination 1 was used to predict the HCC prognosis group to assess the survival of HCC patients, that is, to determine whether they were part of PLR or PHR. We take different measures depending on the level of danger. According to the expression of “Child–Pugh score + FIT + GGT + metastasis + PVTT” in HCC patients, postoperative survival can be comprehensively evaluated to determine the next diagnosis and treatment plan. The combination is used as a “high risk pre-warning combination.” When the five clinical data of the combination were missing, the combination prediction models 12, 3, 7, 13, and 16 were also a superior choice. Therefore, if the clinical data obtained before interventional embolotherapy can be administered to patients with individualized surgical planning, the best radiotherapy and chemotherapy dose and time, and appropriate follow-up interval can be determined.28
Abbreviations
HCC, hepatocellular carcinoma; PVTT, portal vein tumor thrombus; FIT, frequency of interventional treatment; AFP, α-fetoprotein; ALT, alanine transaminase; AST, aspartate aminotransferase; TP, total protein; ALB, albumin; GLB, globulin; AG, ALB/GLB; GGT, gamma-glutamyl transpeptidase; TBIL, total bilirubin; DBIL, Direct Bilirubin; IBIL, indirect bilirubin; ALP, Alkaline Phosphatase; PAB, prealbumin; TBA, Total Bile Acid; ADA, adenosine deaminase; AFU, fucosidase; PT, prothrombin time; HE, hepatic encephalopathy; PLR, predicted low-risk group; PHR, predicted high-risk group; HR, hazard ratio; CI, confidence interval; AUC, area under the curve; ROC, receiver operating characteristic; Combination 1, Child–Pugh score+FIT+GGT+ metastasis +PVTT; Combination 12, Child–Pugh score+FIT; Combination 3, Child–Pugh score+FIT+GGT+ PVTT; Combination 7, Child–Pugh score+FIT+metastasis; Combination 13, Child–Pugh score+GGT; Combination 16, Child–Pugh score+13 items (Tumor diameter, Tumor number, metastasis, PVTT, ascites, FIT, AFP, ALT, AST, TBIL, ALB, ALP, GGT).
Ethics Statement
This study was approved by the Institutional Ethics Review Board at Suzhou Hospital of Anhui Medical University (2,019,006). The verbal informed consent was approved by the Institutional Ethics Review Board at Suzhou Hospital of Anhui Medical University. Patients’ informed consents were obtained orally by phone during follow-up communications and standard university hospital guidelines in accordance with the Declaration of Helsinki including confidentiality and anonymity were followed in the handling and publication of patients’ tissues.
Acknowledgments
This work was supported by grants from the Scientific Research Fund of Anhui Medical University in 2019 (2019xkj242), Provincial Quality Engineering Project of Institutions of Higher Learning in 2017 (No. 2521), Corps achievements transfer and transformation project (2018BA006).
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
2. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132.
3. Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–1075.
4. Lau WY, Lai EC. Hepatocellular carcinoma: current management and recent advances. Hepatobiliary Pancreat Dis Int. 2008;7(3):237–257.
5. Maehara Y, Kabashima A, Koga T, et al. Vascular invasion and potential for tumor angiogenesis and metastasis in liver carcinoma. Surgery. 2000;128(3):408–416. doi:10.1067/msy.2000.107265
6. Boulin M, Delhom E, Pierredon-Foulongne MA, et al. Transarterial chemoembolization for hepatocellular carcinoma: an old method, now flavor of the day. Diagn Interv Imaging. 2015;96(6):607–615.
7. Cheng X, Sun P, Hu Q-G, et al. Transarterial (chemo) embolization for curative resection of hepatocellular carcinoma: a systematic review and meta-analyses. J Cancer Res Clin Oncol. 2014;140(7):1159–1170. doi:10.1007/s00432-014-1677-4
8. Choi JW, Park JY, Ahn SH, et al. Efficacy and safety of transarterial chemoembolization in recurrent hepatocellular carcinoma after curative surgical resection. Am J Clin Oncol. 2009;32(6):564–569. doi:10.1097/COC.0b013e3181967da0
9. Jennifer P, Issam EN, Sanford NN, et al. Dosimetric analysis and normal-tissue complication probability modeling of child-pugh score and albumin-bilirubin grade increase after hepatic irradiation. Int J Radiat Oncol Biol Phys. 2020.
10. Wang H, L J B, Patel J, et al. Imaging-based vascular-related biomarkers for early detection of acetaminophen-induced liver injury. Theranostics. 2020;10(15):6715–6727. doi:10.7150/thno.44900
11. Mahlstedt J. Clinical aspects of detection and imaging of tumors of liver and spleen. In: Nuclear Medicine in Clinical Oncology. Springer Berlin Heidelberg; 1986:80–87. doi:10.1007/978-3-642-70947-0_14
12. Wu AW, Ji JF, Yang H. Long-term outcome of a large series of liver cancer patients in China. Chin J Cancer Res. 2010;22(1):167–175. doi:10.1007/s11670-010-0167-8
13. Jiming B, Jianhua LI, Hao Q. Study on combined detection of AFP AFU and GPC3 in the diagnosis of primary hepatic cancer. Heb Med. 2012;18(3):273–287.
14. Wenjuan X, Wenjing Z, Medicine DO. Combined detection of GP73, AFP and CA-199 in the diagnosis of primary liver cancer. J Mod Oncol. 2016.
15. Chen D, Jain S, Y H S, et al. Building classification models with combined biomarker tests: application to early detection of liver cancer. J Stat Sci Appl. 2017;5(3):91.
16. Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi:10.1016/S0140-6736(19)30427-1
17. Zhou Y, Zhou N, Fang W, et al. Overexpressed HDGF as an independent prognostic factor is involved in poor prognosis in Chinese patients with liver cancer. Diagn Pathol. 2010;5(1):1–10. doi:10.1186/1746-1596-5-58
18. Lishuang C. Analysis the inspection results of liver function in patients with liver cirrhosis. China Health Stand Manage. 2017;8(03):116–117.
19. Yoo D-J, Kim KM, Jin Y-J, et al. Clinical outcome of 251 patients with extrahepatic metastasis at initial diagnosis of hepatocellular carcinoma: does transarterial chemoembolization improve survival in these patients? J Gastroenterol Hepatol. 2011;26(1):145–154. doi:10.1111/j.1440-1746.2010.06341.x
20. Chung GE, Lee J-H, Kim HY, et al. Transarterial chemoembolization can be safely performed in patients with hepatocellular carcinoma invading the main portal vein and may improve the overall survival. Radiology. 2011;258(2):627–634. doi:10.1148/radiol.10101058
21. Jeon SH, Park KS, Kim YH, et al. Incidence and risk factors of acute hepatic failure after transcatheter arterial chemoembolization for hepatocellular carcinoma. Koren J Gastroenterol. 2007;50(3):176–182.
22. Nishikawa H, Osaki Y, Kita R, et al. Comparison of transcatheter arterial chemoembolization and transcatheter arterial chemotherapy infusion for patients with intermediate –stage hepatocellular carcinoma. Oncol Rep. 2014;31(1):65–72. doi:10.3892/or.2013.2845
23. Jun Z, Yue-yong C, Yong H, Xu-yang D. Prognostic factors of primary hepatic carcinoma treated with TACE. Western Med. 2011;23(11):2195–2197.
24. Jiafu F, Ed. Huang Wenfang, Modern Clinical Laboratory Diagnostic Manual. Vol. 09. Sichuan Science and Technology Press; 2013:206.
25. Zhao Z, Zhenfang D, Ju Y, Xu R. Investigation on the clinical significance of combining determination of AFP, AFP/AFP - L3, PIVKA –II and GGT for the diagnosis of hepatocellular carcinoma. Int J Lab Med. 2019;40(6).
26. Yoon HM, Kim JH, Kim E-J, et al. Modified cisplatin-based transcatheter arterial chemoembolization for large hepatocellular carcinoma: multivariate analysis of predictive factors for tumor response and survival in a 163-patient cohort. J Vasc Interv Radiol. 2013;24(11):1639–1646. doi:10.1016/j.jvir.2013.06.017
27. Whitfield JB. Serum gamma glutamyl transferase and risk of disease. Clin Chem. 2007;53(1):1–2. doi:10.1373/clinchem.2006.080911
28. Wang Q, Q F Z, Shen F, et al. Clinical prediction models for individualized treatment of hepatocellular carcinoma. J Clin Hepatol. 2018;34(07):21–25.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


