Back to Journals » Journal of Blood Medicine » Volume 11
Preoperative Anemia Screening and Treatment Practices in Patients Having Total Joint Replacement Surgery: A Retrospective, Observational Audit
Authors Delaforce A , Galeel L , Poon E , Hurst C , Duff J , Munday J , Hardy J
Received 19 March 2020
Accepted for publication 29 June 2020
Published 6 August 2020 Volume 2020:11 Pages 259—265
DOI https://doi.org/10.2147/JBM.S254116
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Alana Delaforce,1,2 Lemya Galeel,2 Edgar Poon,3 Cameron Hurst,4 Jed Duff,1,5 Judy Munday,5,6 Janet Hardy2
1School of Nursing, University of Newcastle, Newcastle, NSW, Australia; 2Mater Research, Mater Health Services, South Brisbane, QLD, Australia; 3School of Pharmacy, University of Queensland, Brisbane, Australia; 4QIMR Berghoffer Medical Research Institute, Brisbane, QLD, Australia; 5School of Nursing, Queensland University of Technology, Brisbane, QLD, Australia; 6School of Nursing, The University of Agder, Kristiansand, Norway
Correspondence: Alana Delaforce
Mater Research Mater Health Services, Level 6, Duncombe Building, Raymond Terrace, South Brisbane, QLD 4101, Australia
Tel +61 3163 2853
Email [email protected]
Background: Surgical patients with preoperative anemia are more likely to experience adverse outcomes. Patient blood management (PBM) guidelines recommend screening and treating patients for anemia preoperatively to enable optimisation before surgery. This study investigates compliance with PBM guidelines and reports the association between length of stay and transfusion risk in patients with preoperative anemia.
Study Design and Methods: A retrospective, observational, chart audit that included all patients having primary, total hip and knee replacement surgery between July–December 2018 at a tertiary, metropolitan healthcare facility.
Results: Six hundred and seven patients patients were included, 96% (n = 583) patients had blood tests available (full blood count), and 8.1% (n = 49) had iron studies. Most patients 53% (n = 324) were screened between 2 and 6 days before surgery; 14.6% (n = 85) were anaemic preoperatively and only 5.9% (n = 5) of anaemic patients received treatment. Patients who had anemia preoperatively were more likely to receive a blood transfusion (odds ratio 8.65 [95% CI 3.98– 18.76]) and stayed longer in hospital (median difference = 1, χ2 LR = 17.2, df=1, p< 0.007).
Conclusion: Tests ordered for patients having major surgery should include iron studies, renal function, CRP and full blood count to enable detection and classification of preoperative anemia. Timing of screening relative to surgery needs to be sufficient to allow patient optimisation to occur. Appropriate treatment should be provided to anaemic patients to prevent unnecessary blood transfusions and reduce the length of stay. A standardised preoperative anemia pathway may assist in improving practice.
Keywords: preoperative anemia, patient blood management, surgery
Introduction
Anemia is a condition whereby a person’s blood has impaired oxygen-carrying capacity.1 A patient is defined as anaemic, according to the National Blood Authority (NBA) Australia, when their hemoglobin is below 130g/L for males and 120g/L for non-pregnant females.2 In surgical patients, there is an association between preoperative anemia and adverse outcomes, including increased length of stay, risk of infection, and risk of receiving a blood transfusion.3
The prevalence of preoperative anemia varies according to patient co-morbidities.4 In the colorectal surgical population (where patients may have impaired iron absorption), preoperative anemia is present in approximately 36% of patients.4 In the orthopaedic surgery population, a recent Australian study found that 13.9% of patients in an elective surgical cohort were anaemic.4 These figures mirror the results of another Australian, nationwide audit undertaken by Blood Matters, Victoria, that found 14% of orthopaedic surgery patients to be anaemic.5 These patient groups can be responsible for between 42% and 83% of blood transfusions provided to patients postoperatively.3,6 Blood transfusions should be avoided in otherwise healthy populations as they are associated with an increased risk of infection, coagulopathy and prolonged length of stay.7 Screening and treatment of anemia can help prevent unwarranted blood transfusions.
PBM guidelines outline recommended screening and treatment for anemia for patients having major surgery, and those at risk of losing >500mLs of blood.2,8-11 Recommended tests include a Full Blood Count (FBC), iron studies, C-reactive Protein (CRP) and renal function.2 Screening should occur at least six weeks before surgery to allow time for treatment to be provided.2 All patients detected as having anemia should undergo physician review, at which point the cause of the anemia should be ascertained and any underlying comorbidities identified.12 In the case of Iron Deficient Anemia (IDA), oral or IV Iron supplementation should be provided.2 Oral supplementation should be commenced at least 30 days before surgery, depending on the level of repletion required.13 Oral supplementation is traditionally poorly tolerated due to the unpleasant gastrointestinal side effects, and IV Iron may be more suitable in the instance of noncompliance.13
The PBM guidelines now form part of hospital accreditation processes.14 Hospitals must ensure that they have standardised pathways in place that support clinicians to screen and treat patients for anemia.14 Therefore, we sought to understand whether we were complying with these recommendations in the context of patients undergoing major joint replacement surgery. Within this population, anemia screening and preoperative optimisation can have a significant impact on reducing the length of hospital stay, and the probability of a patient requiring a blood transfusion.15,16 This study reports compliance levels with recommended preoperative anemia screening and treatment practices, and the impact on blood transfusions and length of stay.17
Materials and Methods
Study Design and Population
A retrospective audit of all patients who underwent total hip or knee replacement surgery during Jul–Dec 2018 was conducted. We included patients from four campuses (three private and one public) of a tertiary healthcare facility, in South East Queensland, Australia. The records were located by using the Diagnosis Related Group (DRG) codes I04A&B (total knee replacements, minor and major complexity), and I03A&B (total hip replacement, minor and major complexity). We included all patients over the age of 18 undergoing primary surgery of this nature. We excluded revision surgeries to ensure accurate and consistent measurement of usual preoperative screening and treatment processes.
As we included pre-collected patient data, an ethics exemption was sought from the Mater Misericordiae Ltd Human Research Ethics Committee: EXMT/MML/58392.
Measures
An audit tool was developed by the multidisciplinary team and piloted for face validity. Four team members (AD, LG, BH & EP) recorded data electronically. The audit tool aimed to measure practice against the NBA’s PBM guidelines and assessed whether patients were screened for anemia using recommended tests. It also recorded the time frame between testing and surgery and if patients identified as anaemic received appropriate treatment.2 We allowed up to six months for tests to be undertaken before surgery and searched for FBC, iron studies, CRP, and renal studies. We also collected the type of treatment that the patient received including iron supplementation (oral or IV) and blood transfusions. We assessed all treatment provided for clinical appropriateness based on the PBM guidelines2 (see Figure 1).
 |
Figure 1 Simplified guidance for appropriateness of treatment.Note: Data from the National Blood Authority Patient Blood Management guidelines.1 |
Decisions of the appropriateness of blood transfusions were also based on the additional practice points in the NBA Perioperative PBM guidelines.18 The practice points state that the decision to transfuse should be made in the context of the clinical picture (not just a hemoglobin “trigger”).18 The patient should demonstrate some form of clinical decompensation and the patient should be reassessed between transfusion episodes.18 In this study, to determine if a transfusion was part of a single or double transfusion episode, we checked to see if there was any evidence of a physician check or blood test within six-hours following the provision of a transfusion. If there was no evidence of follow up and two units were provided within six hours, they were considered a double unit episode.
Statistical Analysis
Patient characteristics were summarised using count and percentages if categorical, and mean and interquartile range for continuous variables. Odds ratios with confidence intervals have been used to determine the risk associated with preoperative anemia and receiving a blood transfusion. The relationship between preoperative anemia and acute length of stay was investigated using Kaplan–Meier estimates of the survival (length of hospitalisation) curves. A formal comparison of preoperative anemia status and length of stay was conducted using the Log Rank test. All analysis was conducted in the R statistical software (V3.6.1 R core team, 2019), and a significance level of 0.05 was used throughout all inferential analyses.
Results
Six hundred and seven patients were included. Of these, 61.3% (n= 372) underwent knee surgery, and 39% (n =235) had hip surgery. Overall, 96% (n = 583) patients had a full blood count in the six months prior. Only 8.1% (n = 49/607) of the patients included had iron studies. Of the patients with tests, 14.7% (n = 85) of 583 had preoperative anemia. Demographics are outlined in Table 1.
 |
Table 1 Demographics |
Screening
Almost all patients had a preoperative FBC and renal studies, but few had a CRP or iron studies. Only 2.4% (n = 15) of patients had all recommended screening required. The compliance with these tests is outlined in Table 2.
 |
Table 2 Screening Tests Utilised |
The majority of patients did not appear to have timely screening, with 3.95% (n = 24) of patients having it conducted in the recommended timeframes (6 weeks or more) (Table 3).
 |
Table 3 Timeframes of Screening |
Treatment Provided (Iron)
Only 4.3% (n = 26) of patients received iron supplementation, 38.5% (n = 10) of whom were anaemic prior to surgery. Of the anaemic patients who received treatment, 4.7% (n = 4) received IV Iron preoperatively, 1.2% (n =1) was taking oral iron preoperatively, and 5.9% (n = 5) received IV Iron postoperatively. Of the non-anaemic patients, 0.8% (n = 4) received IV Iron preoperatively, 0.2% (n = 1) received IV Iron postoperatively, 1.6% (n = 8) were on oral iron preoperatively, 0.4% (n = 2) were discharged on oral iron supplementation. Based on ferritin levels (of which there were small numbers), 1.2% (n = 1) received treatment that was concordant with guidelines.
Outcomes in Patients with Preoperative Anemia
Blood Transfusion
Blood products were provided to 4.8% (n = 29) of patients across 40 episodes. The pre-transfusion hemoglobin ranged from 69–110g/L (median 80g/L), however the patient with 110g/L was bleeding intraoperatively. 72.5% (n = 29) of episodes were single unit transfusion episodes, 27.5% (n = 11) were double unit transfusions (with no assessment between units). 47.5% (n = 19) episodes were provided according to the PBM guidelines, and the remaining 52.5% (n = 21) were not (16, had no evidence of decompensation, and 5 were due to a lack of evidence of reassessment). Patients with preoperative anemia were at a significantly increased risk of receiving a transfusion (odds ratio 8.65 [95% CI 3.98–18.76]) and represented 55% (n = 16) of the 29 patients who received blood.
Length of Stay
The Kaplan–Meier curve in Figure 2 reflects the probability of anaemic and non-anaemic patients remaining in hospital. Perusal of the curves suggests that there is some difference in the acute length of stay between patients with and without anemia, and that this difference is statistically significant (median difference = 1, χ2 LR = 17.2, df=1, p<0.007).
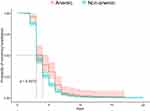 |
Figure 2 Kaplan–Meier survival curve: length of stay difference between patients who were anaemic and non-anaemic preoperatively. |
Patients who had preoperative anemia stayed one (1) day longer compared to non-anaemic patients (Figure 2). Patients treated with a blood transfusion also stayed one day longer, on average, than those who did not receive a transfusion (IQR 3–7and 3–5, respectively).
Discussion
This study reveals three key findings. The first is that at this institution, preoperative anemia screening is not occurring according to guidelines both in terms of the tests undertaken and the time of which they occur. Secondly, patients are not receiving appropriate treatment before surgery. Finally, patients with preoperative anemia are at a significantly higher risk of receiving a blood transfusion and staying longer in hospital.
This audit revealed that the vast majority of patients do not have the recommended screening tests. Preoperative anemia screening in the setting under study should be widened to include iron studies, CRP (to exclude chronic inflammatory causes) and renal studies.2 All patients at risk of losing >500mLs of blood intraoperatively should have the tests ordered as soon as it is decided that surgery is required so that their management can be optimised.1 The fact that the recommended tests are not being carried out in the institution under study is likely to be multifactorial. Currently, there is no standardised pathway in place.6 However, work is currently underway to rectify this and the orthopaedic team are already integrating the recommendations of this report into their practice.
In addition to the screening requiring improvement, the timing of the tests is not adequate to facilitate the optimisation of patients identified as anaemic before surgery. Most patients in this audit had tests 2–6 days before surgery, which, in the context of the guidelines, does not leave enough time to consider the use of oral supplementation.2 It also does not provide an opportunity to provide IV Iron in the currently recommend time frames (8 weeks);2 although some small studies are showing a benefit of ultra-short-term iron therapy.19,20 This presents a potential opportunity to consider when developing preoperative anemia treatment pathways. A double-blind, randomised, controlled study undertaken by Spahn and colleagues in 2019, tested the impact of ultra-short-term combination therapy for anaemic patients and found it reduced the rate of transfusion.19 The combination included IV Iron, subcutaneous erythropoietin alpha, B12 injections and oral folic acid.19 When the therapy was provided from one to three days before surgery, the median number of transfusions per patient was reduced from 1 to 0 (odds ratio 0.70 [95% CI 0.50–0.98]).19 A similar study found that short-term iron and recombinant human erythropoietin therapy given 2–5 days preoperatively, reduced blood transfusion rates from 48.8% to 32.4% (P = 0.001).20 These studies suggest that current guidelines may need to be revised, and short-term treatment may be a viable option if necessary for urgent, non-elective cases.
The second finding was that anemia is not routinely corrected. Only 10 of the 85 patients identified as anaemic had some form of preoperative treatment. Studies have shown that preoperative optimisation can reduce the number of blood transfusions provided in this population.17 Rineau and colleagues implemented a preoperative anemia pathway and found a significant reduction in the amount of blood transfusions required where anemia was corrected (13% non-corrected vs 5% corrected), consistent with the results of our previous audits.6 Had patients been screened and treated in a timely fashion, they may have avoided transfusion.
The final finding was that patients who were anaemic before surgery were more likely to receive a transfusion and have longer hospital stays. Our results show that patients who were anaemic stayed one day longer than those who were not (median difference = 1, χ2 LR = 17.2, df=1, p<0.007) and were also more likely to receive a transfusion (odds ratio 8.65 [95% CI 3.98–18.76]). These results mirror trends between preoperative anemia, blood transfusions and length of stay reported in the literature.21,22 A recent retrospective cohort study conducted in 2019 that included 1186 patients demonstrated that those with preoperative anemia were more likely to receive a blood transfusion 13.1% versus 0.7% (OR 21.7 (2.9–166.7, P<0.001)) in non-anaemic patients.21 They also found that patients with preoperative anemia stayed longer in hospital (3 days compared to 2.1 (P=0.006)) and had increased infectious complications (from 6.4% to 18.4%, (OR 3.3 (1.4–7.7), p=0.004)).21 Another 2017 cohort study including cardiac patients had similar findings. Patients who were anaemic preoperatively were three times more likely to receive a blood transfusion (OR 3.08, 95% CI 1.88–5.06, p < 0.001) and remained in hospital two days longer (8 vs 6 days, p < 0.0001).22 It is therefore important that steps are undertaken to prevent exposing surgical patients to unnecessary risks.
Development of standardised anemia screening and treatment pathways can help reduce variation in care and prevent unnecessary exposure to blood products. Implementation of such a pathway has demonstrated success in improving compliance with PBM guidelines.23 Morgan and colleagues undertook a “before and after” study in a private orthopaedic setting and improved both screening and treatment practices.16 Following implementation, they achieved a result of 94.6% (P<0.0001) of patients receiving required tests and reduced blood transfusions from 9.2% to 2.3% (P=0.001).16 Another example of this is reflected in a study that demonstrated a significant decrease from 20.8% to 14.4% (P = 0.001) over six years in anaemic admissions following the implementation of a preoperative anemia screening and treatment pathway.24 This study also detailed product-related cost savings of $18,507,092 AUD and up to $100 million when activity-based costs were factored in (over the six-year period).24 Similarly, Faulds and colleagues found decreased transfusion rates in patients who were treated according to a preoperative anemia pathway (17.4% versus 9.2%).3 Locally, significant progress has been made to develop a pathway. However, it has not been without challenges in the context of a facility that includes both public and private patients. Morgan and colleagues shared some of the challenges, including the care needed to navigate developing a pathway without dictating terms to private practitioners, who often have greater autonomy than their public colleagues.16 Continued work to develop locally agreed procedures that is underpinned by contemporary implementation theory is ongoing, but the uptake of these recommendations has already commenced within the orthopaedic team.
This study has limitations due to the retrospective nature of the data collection. We were unable to ascertain the specific type of anemia due to a lack of test results. The study is also limited to information documented in charts and blood results across multiple pathology providers. We could not guarantee that the general practitioner responsible for referring the patient had not previously identified the issue and treated the patient before the time of surgery. It is also difficult to comment on the appropriateness of blood transfusions, as clinical notes and observation charts were relied upon to assist in deciding whether the transfusion was provided according to guidelines. A prospective study design would be useful to ascertain more accurate trends in patients who have demonstrated preoperative anemia. A strength of the study is the large sample size.
All patients undergoing major surgery with a risk of blood loss >500mLs should be screened in advance for anemia by having a full blood count, iron studies, CRP and renal studies, regardless of the presence of comorbidities or a trigger during the preoperative assessment phase. Hospitals should develop pathways that consider the local context and the patient population. Further research that rigorously reports on the development of preoperative anemia screening pathways using implementation theory and the effect of those pathways are required to help advance the knowledge of how to achieve this.
Where patients are due for urgent surgery, they should be referred to an established IV Iron infusion clinic to enable optimisation for surgery.2 If the patient’s surgery is not booked within 30 days, oral supplementation is recommended as the first-line treatment option. Postoperatively, caution is needed when deciding to provide a blood transfusion, as the benefits must outweigh the risks. In healthy patients, a transfusion is likely to be unwarranted.
Conclusion
Preoperative anemia in this setting is an important condition to screen and treat to optimise a patient’s iron stores and reduce the risk associated with exposure to blood transfusions and prolonged length of stay. The facility under study will continue the process to establish standardised pathways that are context-specific and developed with the multidisciplinary team to support the implementation of the PBM guidelines.
Acknowledgments
The author AD gratefully acknowledges assistance received from the Australian Government Research Training Program Scholarship. We gratefully acknowledge the assistance with data collection provided by Dr Brittany Hulbert and assistance with consultation on the data collection forms and study design from Dr Treasure McGuire.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Seeber P, Shander A. Basics of Blood Management.
2. National Blood Authority and National Health Medical Research Council. Patient Blood Management Guidelines. Canberra, ACT: National Blood Authority; 2012.
3. Faulds J, Whately-Smith C, Clarke K. Transfusion requirement and length of stay of anaemic surgical patients associated with a patient blood management service: a single-centre retrospective study. Transfus Med. 2019;29(5):311–318. doi:10.1111/tme.12617
4. Hong FS, Sieradzki N, Pollock C, et al. Prevalence and causes of preoperative anemia in elective major surgery patients. Intern Med J. 2017;47(12):1400–1404. doi:10.1111/imj.13613
5. Blood Matters Victoria. Clinical Audit of Preoperative Anemia Assessment and Management in Elective Surgical Procedures 2015. Melbourne, Australia: Victorian Government; 2016.
6. Delaforce A, Moore D, Duff J, et al. Assessing transfusion practice in elective surgical patients: a baseline audit. ISBT Sci Ser. 2019;14(4):415–422. doi:10.1111/voxs.12496
7. Carson JL, Triulzi DJ, Ness PM. Indications for and adverse effects of red-cell transfusion. N Engl J Med. 2017;377(13):1261–1272. doi:10.1056/NEJMra1612789
8. National Institute for Health and Care Excellence. Blood Transfusion Guideline (Ng24). United Kingdom: National Institute for Health and Care Excellence (NICE); 2015.
9. Gammon HM, Waters JH, Watt A, et al. Developing performance measures for patient blood management. Transfusion. 2011;51(11):2500–2509. doi:10.1111/j.1537-2995.2011.03406.x
10. Vaglio S, Gentili S, Marano G, et al. The italian regulatory guidelines for the implementation of patient blood management. Blood Transfus. 2017;15(4):325–328. doi:10.2450/2017.0060-17
11. World Health Organisation. Haemoglobin Concentrations for Diagnosis of Anemia and Assessment of Severity, in Vitamin and Mineral Nutrition Information System. Geneva: WHO; 2011.
12. Desai N, Schofield N, Richards T. Perioperative patient blood management to improve outcomes. Anesth Analg. 2018;127(5):1211–1220. doi:10.1213/ANE.0000000000002549
13. Lopez A, Cacoub P, Macdougall IC, et al. Iron deficiency anemia. Lancet. 2016;387(10021):907–916. doi:10.1016/S0140-6736(15)60865-0
14. Delaforce A, Duff J, Ralph N. Changing the standard of blood management in australia: an overview. J Perioper Nurs. 2018;31(2):15–17. doi:10.26550/2209-1092.1026
15. Hong FS, Sieradzki N, Pollock C, et al. Correcting preoperative iron deficiency as part of patient blood management in the ‘real world’: results of an audit on an australian cohort. ISBT Sci Ser. 2018;13(2):165–170. doi:10.1111/voxs.12421
16. Morgan PN, Coleman PL, Martinez-Garduno CM, et al. Implementation of a patient blood management program in an australian private hospital orthopedic unit. J Blood Med. 2018;9:83–90. doi:10.2147/JBM.S157571
17. Munting KE, Klein AA. Optimisation of pre-operative anemia in patients before elective major surgery - why, who, when and how? Anaesthesia. 2019;74(Suppl 1):49–57. doi:10.1111/anae.14466
18. National Blood Authority and National Health Medical Research Council. Patient Blood Management Guidelines: Module 2 - Perioperative. Canberra, ACT: National Blood Authority; 2012.
19. Spahn DR, Schoenrath F, Spahn GH, et al. Effect of ultra-short-term treatment of patients with iron deficiency or anemia undergoing cardiac surgery: a prospective randomised trial. Lancet. 2019;393(10187):2201–2212. doi:10.1016/S0140-6736(18)32555-8
20. Munoz M, Gomez-Ramirez S, Cuenca J, et al. Very-short-term perioperative intravenous iron administration and postoperative outcome in major orthopedic surgery: a pooled analysis of observational data from 2547 patients. Transfusion. 2014;54(2):289–299. doi:10.1111/trf.12195
21. Morton LJ, Konrad KL, Xu TJ, et al. The interaction between pre-operative anemia and peri-operative blood transfusion on patient outcomes following general surgical procedure: a retrospective review. N Z Med J. 2019;132(1503):13–24.
22. Sanders J, Cooper JA, Farrar D, et al. Pre-operative anemia is associated with total morbidity burden on days 3 and 5 after cardiac surgery: a cohort study. Perioper Med (Lond). 2017;6:1. doi:10.1186/s13741-017-0057-4
23. Delaforce A, Duff J, Munday J, et al. Overcoming barriers to evidence-based patient blood management: a restricted review. Implement Sci. 2020;15(1):6. doi:10.1186/s13012-020-0965-4
24. Leahy MF, Hofmann A, Towler S, et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: a retrospective observational study in four major adult tertiary-care hospitals. Transfusion. 2017;57(6):1347–1358.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
