Back to Journals » Patient Preference and Adherence » Volume 12
Prehospital Index provides prognosis for hospitalized patients with acute trauma
Authors Ruan H, Ge W, Chen J, Zhu Y, Huang W
Received 20 October 2017
Accepted for publication 24 February 2018
Published 13 April 2018 Volume 2018:12 Pages 561—565
DOI https://doi.org/10.2147/PPA.S154670
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Hai-lin Ruan,1,* Wen-han Ge,2,* Jian-ping Chen,1 Yuan-qun Zhu,3 Wei Huang1
1Department of Emergency, Fourth Affiliated Hospital of Guangxi Medical University, Liuzhou, Guangxi, 2Department of Emergency, Huai’an Hospital Affiliated with Xuzhou Medical University, Huai’an, Jiangsu, 3Department of Neurology, Fourth Affiliated Hospital of Guangxi Medical University, Liuzhou, Guangxi, China
*These authors contributed equally to this work
Objective: To evaluate the prognostic value of the Prehospital Index (PHI) for hospitalized patients with acute trauma.
Materials and methods: PHI score and the Injury Severity Score (ISS) were determined in 1,802 hospitalized patients with acute trauma. Receiver-operator characteristic (ROC) curves were used to compare the PHI and ISS in subgroups, and corresponding prediction indicators were calculated.
Results: There were significant differences in PHI score and ISS between the survival group and the death group (Z=2.674, P=0.007). The area under the ROC curve was 0.871 (95% CI 0.855–0.886) for PHI score and 0.792 (95% CI 0.773–0.811) for ISS. Optimal cutoff points to determine the risk of critical illness were PHI ≥4 and ISS ≥22. The sensitivity of the PHI was superior to the ISS (χ2=6.975, P=0.008), but the specificity and the accuracy of the PHI and ISS showed no significant difference (P>0.05).
Conclusion: The PHI is valuable in prognostic prediction of hospitalized patients with acute trauma, and it is superior to the ISS. The PHI has such advantages as being simple in operation, easy to learn, capable of reflecting conditions timely and reliably, and suitable for dynamic evaluation and screening for critical patients with trauma.
Keywords: Prehospital Index, trauma, hospitalized patient, Injury Severity Score
Introduction
Due to socioeconomic, industrial, and transport development, people are engaged in outdoor activities more frequently. Trauma has become a major threat to human health in modern society. Trauma-induced mortality has been decreasing in the past 20 years, due to progress in transport, emergency rescue, and resuscitation of wounded people.1,2 According to World Health Organization statistics, over 5 million people die from trauma worldwide each year. It is expected that by 2020, there will be 800 trauma-related deaths worldwide. China ranks first in the world in the number of deaths related to traffic accidents. Trauma is the leading reason of death among people aged 1–44 years and ranks the third among all causes of death.3 Trauma is a serious public health issue and brings a huge burden to the society.
Severe trauma, especially multiple trauma, is usually caused by one or several factors that affect multiple sites of the body.4 Patients cannot present a medical history or cooperate with physical examination, contributing to difficult early diagnosis. Patient conditions are usually combined with various complications and infection, and may die because of delayed treatment.5–7 There are three peaks of death after severe trauma.8 The first peak occurs several seconds or minutes after trauma, which is known as death at the scene, accounting for about 50% of deaths. The second peak occurs within several hours after trauma, and is known as early death, accounting for about 30% of deaths. The third peak occurs 24 hours after trauma, typically in the first to fourth week after the injury and accounting for 10%–20% of deaths. Therefore, the prognosis of patients with severe trauma depends largely on prehospital emergency rescue. Effective first aid within 10 minutes is crucial for reducing death at the scene. Definitive treatment within 1 hour determines the prognosis of severe-trauma patients, and mortality may decrease by about 10% if the emergency rescue is timely and effective.9
One retrospective cohort study showed that lowering mortality rates in trauma patients may require reducing both the incidence of major complications and the incidence of death after major complications.10 The Prehospital Index (PHI) was developed to provide an objective prehospital scoring system for distinguishing minor-trauma patients from those requiring general or neurosurgical operative intervention within 24 hours (major trauma).11 To develop an easy and reliable method to assess hospitalized patients with trauma, improve the quality of in-hospital rescue, and reduce trauma-related deaths, in this study we assessed the prognostic value of the PHI at 24 hours before being hospitalized for patients with trauma.
Materials and methods
Subjects
All patients provided written informed consent and this study was performed following the requirements of the ethics committee of the Fourth Affiliated Hospital of Guangxi Medical University. A total of 15,074 hospitalized patients with trauma from 2008 to 2011 were included. Stratified random sampling was performed to ensure that each subgroup within the population received proper representation within the sample, and 20% of cases (3,015) were chosen. These cases were further screened based on criteria of initial diagnosis at our hospital, Abbreviated Injury Scale (AIS) score ≥3, prehospital time ≤24 hours, explicit outcomes, and intact data.
Scoring
Trauma Database version 3.0, developed by the Trauma Database Research Center of the Third Military Medical University (Chongqing, China), was used. The initial course of diseases upon admission and relevant data during the hospitalization period were recorded, including test results, surgical procedures, and final diagnoses. The data elements were coded, and the PHI and Injury Severity Score (ISS) were calculated automatically. Assessment parameters of PHI were all based on medical records upon initial admission following the scoring criteria described previously.11 AIS scores and ISS were calculated according to AIS-ISS 2005.12
Statistical analysis
All data are expressed as mean ± SD. Measurements were compared using Student’s t-test, and counts were compared using χ2 tests. Receiver-operator characteristic (ROC) curves were plotted and the area under the curve (AUCROC) calculated. Optimal cutoff points were determined. Inferences about differences in AUC were made using Z-tests. All statistical analyses were performed using SPSS 13.0 software (SPSS Inc., Chicago, IL, USA). P<0.05 indicated significant difference.
Results
Baseline information
Based on stratified random sampling of 15,074 hospitalized patients with trauma, 20% of the cases (3,015) were chosen, and the sampling error was estimated as <5%. Based on inclusion criteria, 1,802 hospitalized patients (1,283 males and 519 females) with trauma were eligible. They were aged 0–100 years, with an average of 41±22 years. The average length of hospital stay was 26±31 days and 104 patients died, with a mortality of 5.77%.
PHI and ISS scores in patients with different prognoses
Depending on prognosis, patients were divided into a survival group (1,698 cases) and a death group (104 cases). The PHI was 1.36±2.18 in the survival group and 6.46±4.54 in the death group, significantly higher in the latter (t=11.384, P<0.001). The ISS was 13.56±6.48 in the survival group and 21.88±7.82 in the death group, significantly higher in the latter (t=10.621, P<0.001).
AUC values for PHI and ISS
ROC curves were plotted for the PHI and ISS (Figure 1). AUCROC was 0.871 for the PHI (95% CI 0.855–0.886) and 0.792 (95% CI 0.773–0.811) for the ISS, which indicated a significant difference between the two groups (Z=2.674, P=0.007). Optimal cutoff points were determined based on Youden’s index. Cutoff values for diagnosing potential critical diseases among hospitalized patients with acute trauma were PHI ≥4 and ISS ≥22, respectively.
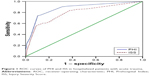  | Figure 1 ROC curves of PHI and ISS in hospitalized patients with acute trauma. |
Comparison of evaluation indices of PHI and ISS
Sensitivity, specificity, accuracy, Youden’s index, false-positive rate, false-negative rate, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio were calculated for the PHI and ISS (Table 1). The sensitivity of PHI was superior to that of ISS (χ2=6.975, P=0.008), but there was no significant difference in specificity (χ2=1.907, P=0.167) or accuracy (χ2=0.156, P=0.693).
Comparison of death rate between mild-severity group and critical-severity group
Based on the scoring criteria and optimal cutoff for the PHI, cases with PHI <4 were put into a mild-severity group (1,510 cases, with mortality of 1.72%) and those with PHI ≥4 were put into a critical-severity group (292 cases, with mortality of 26.71%). The mortality of the critical-severity group was significantly higher than that of mild-severity group (χ2=280.991, P<0.001). Based on the scoring criteria and optimal cutoff for the ISS, cases with ISS <22 were assigned to the mild-severity group (1,554 cases, with mortality of 2.83%) and those with ISS ≥22 were assigned to the critical-severity group (248 cases, with mortality of 24.19%). The mortality of the critical-severity group was significantly higher than that of the mild-severity group (χ2=179.464, P<0.001).
Discussion
A fast, accurate, and standard condition assessment for patients with severe trauma is a great challenge in emergency rescue. Commonly used assessment tools include the Trauma and Injury Severity Score (TRISS) and a Severity Characterization of Trauma (ASCOT). Outcome prediction varies with the conditions of injury, response time, prehospital emergency rescue, medical care levels, and pretrauma diseases. China has not yet established a national trauma database, and the data required for the prediction are neither fully available nor accurate.13 Therefore, the prediction of survival simply based on TRISS and ASCOT may not be reasonable among Chinese patients.
The collection of data required for TRISS and ASCOT is time-consuming. Acute Physiology and Chronic Health Evaluation (APACHE) can offer a reliable assessment of trauma severity,4 but some problems still exist: APACHE applies to all intensive care unit patients, and may not be suitable for trauma patients; the acquisition of data for some parameters may take a long time, which affects the timeliness of assessment, and trauma patients usually undergo physiological disorders and constant changes. Frequent implementation of APACHE will increase not only pain and economic burden for patients but also the workload for medical staff. Moreover, patients may show low compliance with APACHE. The PHI can be determined easily within a short time, and has certain discriminating and assessing power for hospitalized patients with trauma.
The closer the ROC curve to the opportunity line (ie, the closer the AUCROC to 0.5), the lower the discriminating power of the diagnostic indicator will be. The closer the AUCROC value to 1, the stronger the accuracy will be. It is generally believed that the diagnostic value is low when AUCROC is 0.5–0.7, moderate at 0.7–0.9, and high above 0.9.14 In this study, we found that AUCROC values for the PHI and ISS were 0.871 and 0.792, respectively. These data indicate that the PHI has high discriminating power for potential critical illness among hospitalized patients with trauma and is superior to the ISS.
We performed a retrospective analysis based on test results, surgical records, and final diagnosis of included cases. The data from 1,802 hospitalized patients with trauma were collected. Among these patients, the mechanism of trauma was varied, such as traffic trauma, trauma related to work, burns, and accidental falls. In addition, males were dominant, because more males drive and work in industry in China than females. However, tolerance of trauma and responsiveness to treatment vary from one individual to another. Posttrauma physiological disturbance may not always correspond to the severity of anatomical injury, which leads to the diversity of clinical manifestations. Trauma patients usually undergo ultrasound and X-ray to determine severity after admission. However, of parenchymal viscera and neurovascular injuries cannot be diagnosed until surgery. In practice, the ISS may not be as accurate as expected. ISS scores are fixed for trauma patients with confirmed diagnosis, and thus cannot reflect the physiological disturbance dynamically. In spite of these advantages, the ISS reflects the severity of trauma and still applies to assessment and death prediction. Previous studies have shown that the ISS is an independent risk factor of death in trauma patients.15,16 In the present study, the AUCROC was 0.792 for ISS, indicating moderate diagnostic value. The death rate was as high as 24.19% for cases with ISS ≥22, and special care was required for these cases.
The PHI is determined based on such indices as systolic blood pressure, pulse rate, breathing state, and consciousness. The PHI is easy to operate, and has been widely applied as an ideal prehospital quantitative scoring method for trauma scenes. Mild severity is defined as PHI score of 0–3, corresponding to zero death rate and surgical rate of 2%. Critical severity is defined as PHI value of 4–20, corresponding to a death rate of 16.4% and surgical rate of 49.1%. The optimal cutoff point for the PHI after admission was basically consistent with the value used for prehospital assessment. In our study, the death rate was 1.72% for PHI 0–3 and 26.71% for PHI 4–20. Some patients still had a PHI ≥4 after prehospital and nosocomial emergency-rescue measures, such as basic life support. A PHI score ≥4 indicated failure to reverse physiological disturbance and the deterioration of patient conditions, so their mortality was far higher than prehospital mortality. However, patient characteristics may affect mortality, eg, sicker patients are more likely to be admitted and their mortality will be high. Therefore, the proportion of sicker patients in total patients enrolled in this study would have impacted the mortality association with either the ISS or PHI. This is one limitation of this study. Further prospective studies are needed to confirm our results. In addition, this was a single-center study, and biases could not be avoided. Multiple-center studies are necessary to test the prognostic value of the PHI in patients with trauma.
Comparison of the ISS and PHI showed that the sensitivity of the PHI was superior to the ISS, but there were no significant differences in specificity and accuracy between the two indicators. The PHI has a lower rate of missed diagnosis, and thus is more suitable for screening for potential critical illnesses at an earlier stage. Medical staff can provide extra care for acute-trauma patients with high PHI values.
In conclusion, the PHI is an easy, reliable, and objective outcome predictor for hospitalized patients with acute trauma. More importantly, the PHI can provide a timely and dynamic reflection of patient conditions. It is a useful tool to screen preliminarily for potential critical illnesses, and medical staff can get better preparation for the at-risk population.
Acknowledgment
This study was supported by the Specific Research Project of Health Pro Bono Sectors, Ministry of Health, China (01002014).
Disclosure
The authors report no conflicts of interest in this work.
References
Twijnstra MJ, Moons KG, Simmermacher RK, Leenen LP. Regional trauma system reduces mortality and changes admission rates: a before and after study. Ann Surg. 2010;251(2):339–343. | ||
Spahn DR, Bouillon B, Cerny V, et al. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Crit Care. 2013;17(2):R76. | ||
Zhu Z, Shang X, Qi P, Ma S. Sex-based differences in outcomes after severe injury: an analysis of blunt trauma patients in China. Scand J Trauma Resusc Emerg Med. 2017;25(1):47. | ||
Frith D, Goslings JC, Gaarder C, et al. Definition and drivers of acute traumatic coagulopathy: clinical and experimental investigations. J Thromb Haemost. 2010;8(9):1919–1925. | ||
Schöchl H, Nienaber U, Maegele M, et al. Transfusion in trauma: thromboelastometry-guided coagulation factor concentrate-based therapy versus standard fresh frozen plasma-based therapy. Crit Care. 2011;15(2):R83. | ||
Schöchl H, Frietsch T, Pavelka M, Jámbor C. Hyperfibrinolysis after major trauma: differential diagnosis of lysis patterns and prognostic value of thrombelastometry. J Trauma. 2009;67(1):125–131. | ||
Khan S, Davenport R, Raza I, et al. Damage control resuscitation using blood component therapy in standard doses has a limited effect on coagulopathy during trauma hemorrhage. Intensive Care Med. 2015;41(2):239–247. | ||
Moore EE, Knudson MM, Jurkovich GJ, Fildes JJ, Meredith JW. Emergency traumatologist or trauma and acute care surgeon: decision time. J Am Coll Surg. 2009;209(3):394–395. | ||
Lansink KW, Gunning AC, Leenen LP. Cause of death and time of death distribution of trauma patients in a level I trauma centre in the Netherlands. Eur J Trauma Emerg Surg. 2013;39(4):375–383. | ||
Glance LG, Dick AW, Meredith JW, Mukamel DB. Variation in hospital complication rates and failure-to-rescue for trauma patients. Ann Surg. 2011;253(4):811–816. | ||
Koehler JJ, Baer LJ, Malafa SA, Meindertsma MS, Navitskas NR, Huizenga JE. Prehospital Index: a scoring system for field triage of trauma victims. Ann Emerg Med. 1986;15(2):178–182. | ||
Gennarelli TA, Wodzin E. AIS 2005: a contemporary injury scale. Injury. 2006;37(12):1083–1091. | ||
Hannan EL, Mendeloff J, Farrell LS, Cayten CG, Murphy JG. Validation of TRISS and ASCOT using a non-MTOS trauma registry. J Trauma. 1995;38(1):83–88. | ||
Gunning AC, Leenen LP. Applicability of the predictors of the historical trauma score in the present Dutch trauma population: modelling the TRISS predictors. J Trauma Acute Care Surg. 2014;77(4):614–619. | ||
Abdelrahman H, El-Menyar A, Al-Thani H, et al. Time based trauma-related mortality patterns in a newly created trauma system. World J Surg. 2014;38(11):2804–2812. | ||
Morey AF. Re: External validation of a substratification of the American Association for the Surgery of Trauma renal injury scale for grade 4 injuries. J Urol. 2014;192(2):448–449. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

