Back to Journals » Patient Preference and Adherence » Volume 14
Preferred Medium of Receiving Diagnostic News Depending on Patients’ Perception of Their Health Status (Healthy or Sick)
Authors Adelekan A , Alrashah AS , Al Hutaylah IS , Lipert A , Dibwe PM, Rasmus P
Received 12 February 2020
Accepted for publication 12 May 2020
Published 29 May 2020 Volume 2020:14 Pages 903—915
DOI https://doi.org/10.2147/PPA.S247726
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Adediran Adelekan,1 Ahmed Saleh Alrashah,1 Ibrahim Saleh Al Hutaylah,1 Anna Lipert,2 Pierrot Musumbu Dibwe,3 Paweł Rasmus1
1Medical University of Lodz, Department of Medical Psychology, Lodz, Poland; 2Medical University of Lodz, Department of Sport Medicine, Lodz, Poland; 3Academy of Humanities and Economics in Lodz, Lodz, Poland
Correspondence: Adediran Adelekan
Medical University of Lodz, Flat 22, Narutowicza 30, Lodz 90-135, Poland
Tel +48-729-696-726
Email [email protected]
Background: The study aims to gain insight into people’s preferred medium of receiving diagnostic news depending on their perception of their health status (either sick or healthy).
Methods: Comprehensive research was carried out on two main groups of past and prospective patients, Polish respondents (N=72) and International respondents (N= 214), using a CAWI (Computer-Assisted Web Interview) technique. Respondents were asked in an online questionnaire about the past history of illness, whether they would like to receive their diagnostic news and preferred medium of receiving diagnostic news whether they perceive they are sick or healthy.
Results: Amongst the international group, majority of respondents (143 resp. – 73.71%) would generally like to receive their diagnostic news and 156 resp. (80.83%) would prefer to receive their bad diagnostic news (BDN) from medical specialist doctors as opposed to other technological and non-technological means. Meanwhile, in the polish group, 65 resp. (90.28%) would like to generally receive their diagnostic news and 66 resp. (91.67%) would prefer to receive their BDN from medical specialist doctors as opposed to other proposed means of obtaining BDN.
Conclusion: The result of this study indicates that medical doctors, especially specialists, are still a preferred medium of receiving diagnostic news. However, a certain proportion of respondents will be open to technological medium in receiving their diagnostic news.
Keywords: adherence, diagnosis, prognosis, paternalistic care, medical news, patient preference, patient-centered care
Introduction
Breaking down the diagnostic news to patients has usually been done by medical doctors and it is an important aspect of health-care delivery. However, with the emergence and application of digital technologies such as the internet and email, it would be helpful to enquire from people of different demographics in Poland and other countries what preferred medium they would want to utilize in receiving their diagnostic news. Medicine has been evolving from a paternalistic approach to a patient-centered type of health-care delivery. Monitoring patient’s preference in receiving diagnostic news, especially delivering bad diagnostic news (BDN), becomes imperative. This will enable legislators and innovators adapt to changing patients' need in a patient-centered eco-system.
In Poland, medical doctors are mandated legally to break down diagnostic news in person to patients. The Code of Medical Ethics which is currently the standard in Poland (article 17) enacts upon the doctor the responsibility of DBN (Delivering Bad News) to the patient “with tact and care”. This can cause unnecessary congestion of medical facilities especially in instances that do not require the doctor to deliver BDN, although breaking down diagnostic news is one of the most difficult activity encountered by medical doctors in their medical practice.1 An inapt way of communicating with the patient can have an enormous impact on the manner in which they perceive their disease, it can also determine whether they stop or adhere to their medical treatment. Many studies have indicated that there is a direct relationship between doctors’ communication skills and the therapeutic results of patients.2 However, technology can be leveraged according to patient’s preference to deliver diagnostic news (Figure 1), for instance if diagnostic news is classified as good or bad according to classification by artificial intelligence it can be decentralized using blockchain technology to the patient’s preferred medium for such classification of diagnostic news. However, if legislators and innovators do not have data to inform their decision about enabling patients preferred medium of receiving diagnostic news depending on whether their diagnosis is perceived as good or bad it will be difficult for them to initiate legislations or innovations to encourage patient-centered care. Our research finding indicates that medical doctors, especially specialists, are still the majorly preferred medium of receiving diagnostic news. However, a certain proportion preferred using technological means for receiving their diagnostic news.
The below diagram shows the possible flow of diagnostic information to patients through our hypothetically proposed process. We believe such a process will decongest health systems because patients will have more control over their health data just as in a patient-centered care and also patients will be able to pre-select through what medium they would like to receive their diagnostic news depending on whether it is good or bad.
 |
Figure 1 Hypothetical relay system for transmitting diagnostic and prognostic news based on the patient’s preference. |
Medical communication in patient–doctor interaction inevitably has a therapeutic dimension. It determines the increase of patient’s trust toward the doctor3 and also ascertains the therapeutic results2 as well as patient’s gratification with medical services.4,5 If we examine the benefits of the proper medical communication from the doctor’s perspective, we can observe that it averts work burnout6 and increases the level of self-efficacy.7 Regardless, the volume of work of doctors also causes burnout.8 Hence, technology can be leveraged to filter the type of diagnostic news that requires doctors’ attention based on each users’ preferences which then reduces the workload of doctors. Some previous studies by other researchers indicated that there are two integral factors that increase doctors' stress in the process of dispersing BDN which are deficits in education in terms of the soft skills required and the paternalistic approach of medical doctors.9,10 Our research indicated some patients would like to receive their diagnostic news from medium other than medical doctors, although the statistics varied depending on their perceived health status (sick or healthy). Another question that arises from our research is how equipped these other media are in delivering BDN. We would like our research to inform innovators of health solutions toward patients-centered care. Thanks to such monitoring of patients' preferred medium of receiving diagnostic news, innovators will be able to develop and implement more relevant patient-centered technological solutions to alleviate patient and doctor anxiety while decongesting medical facilities.
Our research aimed at evaluating patients preferred medium of receiving bad and good diagnostic news. We wanted to know if patients were interested in receiving their diagnostic news depending on their perceived health status as sick or healthy. In our study, we operationalized the definition of BDN based on another research work on DBN that “bad news” is any form of diagnosis related to permanent or relatively permanent changes in the organism that require a continuous or long-term medical treatment or a therapy focused on pain management.11 Hence, a good medical diagnosis is the opposite. Approaching bad news from this perspective, we see that it encompasses diseases as listed in ICD-10 classifications (eg, Certain infectious and parasitic diseases, Neoplasms, Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism, Endocrine, Nutritional and metabolic diseases, Mental and behavioral disorders, Diseases of the nervous system, Diseases of the circulatory system, Diseases of the respiratory system, Diseases of the digestive system, Diseases of the musculoskeletal system and connective tissue, Diseases of the genitourinary system and Factors influencing health status and contact with health services) amongst others.
Experimental Section
The research was carried out in the period between August 2018 and January 2019. The data were collected using the CAWI (Computer-Assisted Web Interview) technique. We used a meticulously designed e-questionnaire as our research tool. In the process of creating the questionnaire, we first matched our research aim, research question, hypotheses and survey questions as shown in Appendix A. We then took into account the available forms of receiving diagnostic news via human and technological means. Additionally, we conducted procedural consultations of the research tool that is capable of evaluating the correctness and unambiguity of the formulated questions. Patients were asked 21 closed questions and 1 semi-open question concerning their socio-demographic variables, willingness to receive prognostic news generally, willingness to receive diagnostic news whether they think it is either good or bad, past medical history, preferred medium of receiving diagnostic news and how much they are willing to pay. The study groups: Polish respondents (N=72) and International respondents (N= 214) were fully inclusive, and the participants were chosen at random by sending a web link of the e-questionnaire to email addresses and social media groups. Participation in the study was anonymous and voluntary. Information about the study was delivered to past and prospective patients via electronic media. The survey’s instructions informed the participants that, by completing the survey, they gave consent to take part in the research and the data obtained would be processed anonymously in aggregated statistical summaries. The survey was anonymous, and for this reason, our study was exempted from the ethical approval.
In the final analysis, all questionnaires were taken into account. The request to share information about the survey together with a link to the e-questionnaire was addressed to all our researchers. The sharing of the questionnaire link was undertaken by 5 of our researchers. Moreover, information about the survey was published on 15 social media forums administered by casuals (family and friend), academics and health-related groups. For the purposes of statistical analysis, python software was used as shown in Appendix B. Opinions and assessments of the patients were correlated with the sociodemographic variables (age, gender, marital status, education, and place of residence), health variables (type of disease), and how much patients were willing to pay potentially to receive their diagnostic news online. The technical analysis of the survey aimed to establish the reliability of the survey given the sizes of the samples. The first step in this was achieved using the principal component analysis. This statistical method helped us to establish the un-biasness in the data collection during the survey by linearly converting the probably correlated data into uncorrelated ones. In this case, we mapped the features into a two-dimensional component. An aspect that clearly established the un-biasness was observed by two facts: the data points in the PCA (Principal Component Analysis) are widespread on the figures in both cases and the colors of the data points are not overly clustered, the (Figures 2 and 3) below illustrates that.
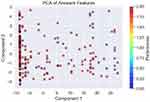 |
Figure 2 PCA of the international survey (n=211) respondents. |
 |
Figure 3 PCA of the Polish survey respondents (n=72). |
In addition to the PCA, we also explored the consistency in the answers, but in order to establish the consistency, we first stripped the survey of any redundancy between questions. This was achieved by effectively computing the correlation heatmaps for the two surveys and only running our consistency test using an AI method and only basing it on uncorrelated questions. The figures below (Figures 4 and 5) show the remaining questions fully capturing the consistency of the survey.
 |
Figure 4 Correlation heatmaps of the most relevant questions for exploring consistency in international survey. |
 |
Figure 5 Correlation heatmaps of the most relevant questions for exploring consistency in Polish survey. |
We used Python software analysis for analyzing the correlation between the responses of participants in our research. Specifically, we used PCA (Principal Component Analysis) to determine that our question design was not bias, the unanswered questions were treated statistically by assuming the median response, we correlated all the questions with each other and deduced that patients preferred medium in receiving good or bad diagnostic news was highly correlated. This might imply that patience preferred medium of receiving diagnostic news was the same whether the news was good or bad.
Using the AI algorithm, we have established that the English survey is consistent at 88% of reliability, while the Polish one is 100% reliable. The figures below (Figures 6 and 7) show what was obtained.
 |
Figure 6 Showing accuracy score of international survey. |
 |
Figure 7 Showing accuracy score of polish survey. |
Results
Amongst the international group, majority of respondents (143 resp. – 73.71%) would generally like to receive their diagnostic news (Table 3) (156 resp. - 80.83%) would prefer to receive their BDN from medical specialist doctors as opposed to other suggested media such as: Directly from their family doctor, Any means except doctors, Nurses, Hard copy paper of diagnostic news, Priest, Imam, Psychologist, Family members, Email if possible, Online website if possible, Phone call, MMS/SMS, Psychotherapist and Others. Meanwhile, in the polish group 65 resp. (90.28%) would like to generally receive their diagnostic news (Table 3), 66 resp. (91.67%) would prefer to receive their BDN from medical specialist doctors as opposed to other suggested media such as: Directly from their family doctor, Any means except doctors, Nurses, Hard copy paper of diagnostic news, Priest, Imam, Psychologist, Family members, Email if possible, Online website if possible, Phone call, MMS/SMS, Psychotherapist and Others (Table 4).
 |
Table 1 The Past Serious Illness Reported by International Group of Respondents (n=48) and Polish Group of Respondents (n=6) |
 |
Table 2 Table Showing the Characteristics of International Group (N=214) and Polish Group (N=72) of Respondents |
 |
Table 3 Table Showing the Willingness to Receive Diagnostic News Amongst International Group of Respondents (N=214) and Polish Group of Respondents (N=72) Depending on Health Status (Sick or Healthy) |
 |
Table 4 Showing Prefered Medium of Receiving Good and BDN for the Group of International Respondents (N=214) and Group of Polish Respondents (N=72) |
For the aim of classifying disease entities, ICD-10 was used. Most of the respondents from the international group reported that they had not have a serious past medical illness (78.97%), while the other respondents (21.03%) reported a serious past medical illness (Table 2) of which 14.58% were Certain infectious and parasitic diseases, 2.08% were Neoplasms, 6.25% were Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism, 2.08% were Endocrine, nutritional and metabolic diseases, 2.08% were Mental and behavioral disorders, 14.5% were Diseases of the nervous system, 16.67% were Diseases of the circulatory system, 12.50% were Diseases of the respiratory system, 8.33% were Diseases of the digestive system, 4.17% were Diseases of the musculoskeletal system and connective tissue, 2.08% were Diseases of the genitourinary system, 2.08% was Pregnancy, childbirth and the puerperium, 4.17% were Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified, 8.33% were Injury, poisoning and certain other consequences of external causes, 2.08% was Factors influencing health status and contact with health services (Table 1). Also, in the Polish group 63 resp. (87.50%) reported that they had not had a serious past medical history, while 9 resp. (12.50%) reported that they had had a serious past medical history of which one out of six (16.67%) were Neoplasms, three out of six (50%) were Endocrine, nutritional and metabolic diseases, one out of six (16.67%) were Diseases of the nervous system, one out six (16.67%) were Diseases of the digestive system (Table 1).
Amongst the international group, majority of respondents (143 resp. – 73.71%) would generally like to receive their diagnostic news, 156 resp. (80.83%) would prefer to receive their BDN from medical specialist doctors as opposed to other suggested mediums such as: Directly from their family doctor, Any means except doctors, Nurses, Hard copy paper of diagnostic news, Priest, Imam, Psychologist, Family members, Email if possible, Online website if possible, Phone call, MMS/SMS, Psychotherapist and Others. Meanwhile, in the Polish group 65 resp. (90.28%) would like to generally receive their diagnostic news, 66 resp. (91.67%) would prefer to receive their BDN from medical specialist doctors as opposed to other suggested mediums such as: Directly from their family doctor, Any means except doctors, Nurses, Hard copy paper of diagnostic news, Priest, Imam, Psychologist, Family members, Email if possible, Online website if possible, Phone call, MMS/SMS, Psychotherapist and Others (Table 4). Business and economics are an important aspect to consider in health-care delivery, we have deduced that majority of our respondents are not willing to pay to receive their diagnostic news through an online medium (Table 5). Nevertheless, if they were going to pay for getting this service from an online platform, the Polish participants will pay an average of 4.72 euro while the international respondents will pay an average of 15.34 euro per diagnostic news, this huge disparity could be as a result of differences is purchasing power of people between countries, we therefore recommend market research for each country before such patient-centered health service is offered.
 |
Table 5 Showing Willingness to Pay for Receiving Diagnostic News Online and Payment Preference for International Group Respondents (N=214) and Polish Group Respondents (N=72) |
Discussion
Health IT plays vital roles in different facets of the diagnostic process: capturing information about a patient that aids the diagnostic process, inclusive of the clinical history and interview, physical exam, and diagnostic testing results; therefore, shaping a clinician’s workflow and decision-making in the diagnostic process; and facilitating information exchange.12 Some demonstrations have already shown the positive use of health IT in aiding diagnosis clinically.13 However, the efficacy of technology has not been demonstrated in delivering diagnostic news especially BDN. A research study of 427 cancer patients indicated that 18% of people received their news of cancer diagnosis over the phone.14 The age group is a factor affecting patients’ preference in their medium of receiving diagnostic news as seen in our research result (Table 2). An elderly individual might react poorly to the impersonal use of a robot, while a youthful person may not have an issue. A 2010 study which reported cancer diagnoses found that the satisfaction was higher with patients told in person of their diagnosis. Although the study population had a median age of 53 years old and 85% of the participants were identified as Caucasian.14 The SPIKE protocol is a methodology used in delivering BDN to patient.15 In the study conducted out by Greiner and Conklin, 30% of patients suffered from undesirable feelings caused by inappropriately delivered bad news by doctors utilizing the SPIKES protocol.16 Perhaps, technology can complement the delivery of BDN and consequently improve patients’ satisfaction. It is important to emphasize that in Poland doctors are not mandated to use any protocols designed to deliver bad news.11 Although within the framework of medical education, students in Medical University of Lodz, Poland have the possibility to develop communication skills related to the process of delivering BDN because a course called “patient–doctor interaction” is included in the curriculum. However, the course does not focus on technology such as telemedicine as a means of delivering health care. According to studies in the context of patients' satisfaction and the development of medical therapy, the two crucial elements which were pointed out are: giving patient as detailed information as possible about the diagnosis and then supplementing this information with an outline of possible consequences of the diagnosis which will enable patients to take part in the decision-making process.11,17,18 These elements are possible through the framework (Figure 1) we have proposed in transmitting patients’ diagnostic news. In addition, it actually improves the patients’ engagement in their healing process.19 This requirement can be feasibly achieved by the technology of today. It is pertinent to emphasize that there are peculiar diseases cases in which the process of delivering information should foremostly include not just the patient but his or her closest relatives as it may be a condition which necessitates the process of taking up therapy.20 Today’s world technology can connect family virtually and improve adherence, especially in the global context. In fact, several studies have evaluated the use of emerging technologies to improve patient adherence to medication technology.21–26 According to a study conducted by Sobczak et al (2018) most of the patients reported that they had not been supplied with the information about causes of their disease (40%), various forms of medical treatment (45%), health consequences of quitting medical treatment (47%), and medical recommendations related to changes the patient should initiate in their life such as following: a prescribed diet and either engaging in or avoiding physical activity (45%). Precisely 63% of respondents confirmed that they had been in no way encouraged by the doctor to ask any questions or to clarify any concerning issues related to the diagnosis. More than 25% of the respondents reported that, while DBN, the doctor had been using incomprehensible medical terminology. Hence, it is recommended that DBN should be devoid of medical jargons.26,27 Technology can also be leveraged to dispense comprehensible news, perhaps the time constraint to deliver BDN can possibly be programmed for appropriateness. A study showed that 42% of patients stated that the doctor had too little time for them. In an OECD report, Poland is on the next-to-last place with regard to the amount of time spent on communicating the diagnosis: maximum: Belgium – 97.5, OECD32 – 81.3, Poland – 59.6, minimum: Japan – 39.0. It should be noted, however, that this status quo is caused, among other reasons, by the reality that Polish doctors are ranked top as regards the number of visits per doctor: Poland – 3179, OECD32 – 2295.28 According to a study, a significant number of patients than doctors expressed their need for partnership and open communication in clinical relationships that will enable them to engage in the procedure of decision-making as regards their further medical therapy and to fully realize the patient’s right to access all the information about their health.9 This is also possible through the technology-based framework we are proposing. This might also indicate a paradigm shift from paternalistic to patient-centered care. However, the present legal framework still makes it difficult for patients to determine how they receive their diagnostic news because of data protections and legislative restrictions. Our research result informs legislators about patients’ preference and we recommend a larger study to continuously monitor these preferences across different countries and socio-demography.
Our research indicated that specialist doctors are the most preferred medium for receiving diagnostic news. Probably it is because of their knowledge in the field or empathy for patients during communication. Further research can inform the direction of technology in patient-centered care by inquiring from patients why they prefer a doctor to deliver good or bad diagnostic compared to other media.
Strength of Study
The research problem stemmed from a real-life observation whereby a patient was waiting for a long duration before she could receive her diagnostic news. Two of our researchers who observed the problem asked themselves if there were other means of receiving diagnostic news and what limitations existed legally in dispensing diagnostic news via other media besides the medical doctor. We have since realized that the Article 17 was a limitation to receiving diagnostic news via other means in Poland. The f1-score, accuracy and precision score of the survey design were relatively high for both the international and Polish survey design. Also, the international group consisted of people from diverse nationality hence the results generalize beyond ethnic and national variables. IP restriction of our research tool prevented the same respondent from answering the survey more than once thereby decreasing biasness. The PCA (The Principal Component Analysis) indicated unbiasedness in the responses of the participants, especially in the Polish group.
In addition, it was stated in our discussion that a study showed that 42% of patients stated that the doctor had too little time for them. In an OECD report, Poland is on the next-to-last place with regard to the amount of time spent on communicating the diagnosis: maximum: Belgium – 97.5, OECD32 – 81.3, Poland – 59.6, minimum: Japan – 39.0. This makes researching Poland important in terms of evaluating patients preferred medium in receiving diagnostic news and the legal limitations to a patient-centered care.
Limitation of Study
The Polish group of respondents can be increased further from the 73 observations. However, the PCA and correlation of questions increase the credibility of the observations. We recommend that future studies should have a larger sample size. In addition, we utilized only one research tool which was a specially designed questionnaire. Nevertheless, in this type of research which analyses the opinion of the population, one of the best tools is questionnaires designed for the needs of the study.
Conclusions
In the modern technological world, the physician is still recognized as the best medium for receiving diagnostic news. Although there are patients opened to the new forms of transmission of medical information, their preference should be respected by innovators and legislators. Future research is recommended to define the profile of a patient interested in a form of information transfer other than human or determine medical situations in which information technology based on artificial intelligence would be the most appropriate.
Highlights
- Majority of people will not pay to receive their diagnostic news from an online medium.
- Doctors especially specialists are still the most preferred medium of receiving diagnostic news.
- Generally, people are willing to receive news of their diagnostic news.
- The preferred medium for receiving diagnostic news was not altered by their perceived good or bad health status.
Acknowledgments
We acknowledge the effort of the Medical University of Lodz in connecting the medical-student researchers to their supervisors after they had just observed the research problem. Our sincere appreciation also goes to Marta Perzyna for her insights in writing this article.
Funding
This research received no external funding.
Disclosure
The authors declare no conflicts of interest.
References
1. Hulsman RL, Pranger S, Koot S, Fabriek M, Karemaker JM, Smets EM. How stressful is doctor-patient communication? Physiological and psychological stress of medical students in simulated history taking and bad-news consultations. Int J Psychophysiol. 2010;77(1):26–34. doi:10.1016/j.ijpsycho.2010.04.001
2. Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi:10.1097/MLR.0b013e31819a5acc
3. Golin C, Dimatteo MR, Duan N, Leake B, Gelberg L. Impoverished diabetic patients whose doctors facilitate their participation in medical decision making are more satisfied with their care. J Gen Intern Med. 2002;17(11):857–866. doi:10.1046/j.1525-1497.2002.20120.x
4. Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15(1):25–38.
5. Clark PA. Medical practices’ sensitivity to patients’ needs. Opportunities and practices for improvement. J Ambul Care Manage. 2003;26(2):110–123. doi:10.1097/00004479-200304000-00004
6. Suchman AL, Roter D, Green M, Lipkin M
7. Ammentorp J, Sabroe S, Kofoed PE, Mainz J. The effect of training in communication skills on medical doctors’ and nurses’ self-efficacy. A randomized controlled trial. Patient Educ Couns. 2007;66(3):270–277. doi:10.1016/j.pec.2006.12.012
8. Downing NL, Bates DW, Longhurst CA. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med. 2018;169(1):50–51. doi:10.7326/M18-0139
9. Sobczak K, Pawłowski L, Pietrzykowska M, Spolak N. Delivering bad news by physicians – polish reality check. J Med Sci. 2016;85(3):172–177. doi:10.20883/jms.2016.117
10. Sobczak K, Leoniuk K, Janaszczyk A, Pietrzykowska M. Patients’ expectations as to doctors’ behaviors during appointed visits. Health Commun. 2017;32(4):517–519. doi:10.1080/10410236.2016.1140285
11. Sobczak K, Leoniuk K, Janaszczyk A. Delivering bad news: patient’s perspective and opinions. Patient Prefer Adherence. 2018;12:2397–2404. doi:10.2147/PPA.S183106
12. Committee on Diagnostic Error in Health Care; Board on Health Care Services; Institute of Medicine; The National Academies of Sciences, Engineering, and Medicine; Balogh EP, Miller BT, Ball JR, editors,. Improving Diagnosis in Health Care. Washington (DC): National Academies Press (US); 2015. Technology and Tools in the Diagnostic Process. Available from. https://www.ncbi.nlm.nih.gov/books/NBK338590/#.
13. El-Kareh R, Hasan O, Schiff G. Use of health information technology to reduce diagnostic error. BMJ Qual Saf. 2013;22(Suppl 2):ii40–ii51. doi:10.1136/bmjqs-2013-001884
14. Figg WD, Smith EK, Price DK, et al. Disclosing a diagnosis of cancer: where and how does it occur? J clin oncol. 2010;28(22):3630–3635. doi:10.1200/JCO.2009.24.6389
15. Baile W, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka A. SPIKES – a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302–311. doi:10.1634/theoncologist.5-4-302
16. Greiner AL, Conklin J. Breaking bad news to a pregnant woman with a fetal abnormality on ultrasound. Obstet Gynecol Surv. 2015;70(1):39–44. doi:10.1097/OGX.0000000000000149
17. Brown VA, Parker PA, Furber L, Thomas AL. Patient preferences for the delivery of bad news – the experience of a UK Cancer Centre. Eur J Cancer Care (Engl). 2011;20(1):56–61. doi:10.1111/j.1365-2354.2009.01156.x
18. Davison BJ, Parker PA, Goldenberg SL. Patients’ preferences for communicating a prostate cancer diagnosis and participating in medical decision-making. BJU Int. 2004;93(1):47–51. doi:10.1111/j.1464-410X.2004.04553.x
19. Edwards A, Elwyn G. Inside the black box of shared decision making: distinguishing between the process of involvement and who makes the decision. Health Expect. 2006;9(4):307–320. doi:10.1111/j.1369-7625.2006.00401.x
20. Outram S, Harris G, Kelly B, et al. “We didn’t have a clue”: family caregivers’ experiences of the communication of a diagnosis of schizophrenia. Int J Soc Psychiatry. 2015;61(1):10–16. doi:10.1177/0020764014535751
21. Shah BR, Adams M, Peterson ED, et al. Secondary Prevention Risk Interventions Via Telemedicine and Tailored Patient Education (SPRITE): a randomized trial to improve postmyocardial infarction management. Circ Cardiovasc Qual Outcomes. 2011;4(2):235–242. doi:10.1161/CIRCOUTCOMES.110.951160
22. Vervloet M, van Dijk L, Santen-Reestman J, et al. Improving medication adherence in diabetes type 2 patients through real time medication monitoring: a randomised controlled trial to evaluate the effect of monitoring patients’ medication use combined with short message service (SMS) reminders. BMC Health Serv Res. 2011;11:5. doi:10.1186/1472-6963-11-5
23. Du HY, Newton PJ, Zecchin R, et al. An intervention to promote physical activity and self-management in people with stable chronic heart failure. The Home-Heart -Walk study: study protocol for a randomized controlled trial. Trials. 2011;12(1):63. doi:10.1186/1745-6215-12-63
24. Koehler F, Winkler S, Schieber M, et al. Telemedical Interventional Monitoring in Heart Failure (TIM-HF), a randomized, controlled intervention trial investigating the impact of telemedicine on mortality in ambulatory patients with heart failure: study design. Eur J Heart Fail. 2010;12(12):1354–1362. doi:10.1093/eurjhf/hfq199
25. Feldman PH, McDonald MV, Mongoven JM, et al. Home-based blood pressure interventions for blacks. CircCardiovascQualOutcomes. 2009;2(3):241–248.
26. Kim MK, Alvi A. Breaking the bad news of cancer: the patient’s perspective. Laryngoscope. 1999;109(7 Pt 1):1064–1067. doi:10.1097/00005537-199907000-00010
27. Randall TC, Wearn AM. Receiving bad news: patients with haematological cancer reflect upon their experience. Palliat Med. 2005;19(8):594–601. doi:10.1191/0269216305pm1080oa
28. OECD. Health at a Glance 2017. OECD Indicators. Paris: OECD; 2017:1–220.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
