Back to Journals » Patient Preference and Adherence » Volume 14
Preferences for Primary Healthcare Services Among Older Adults with Chronic Disease: A Discrete Choice Experiment
Authors Peng Y, Jiang M, Shen X, Li X, Jia E, Xiong J
Received 29 May 2020
Accepted for publication 13 August 2020
Published 17 September 2020 Volume 2020:14 Pages 1625—1637
DOI https://doi.org/10.2147/PPA.S265093
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Naifeng Liu
Yingying Peng, Mingzhu Jiang, Xiao Shen, Xianglin Li, Erping Jia, Juyang Xiong
School of Medicine and Health Management, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei 430030, People’s Republic of China
Correspondence: Juyang Xiong
School of Medicine and Health Management, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei 430030, People’s Republic of China
Tel +86-13995629873
Email [email protected]
Purpose: The aim of this study was to quantify the relative importance of the preference heterogeneity of Chinese older adults with chronic disease for primary healthcare service (PHCS) in the hypothetical minor chronic disease scenario.
Patients and Methods: A discrete choice experiment (DCE) was administered to the patients aged 60 and above with at least one chronic disease in China. Five DCE attributes were considered, including types of service, treatment options, out-of-pocket (OOP) cost per visit, distance to practice, and the seniority of medical practitioners. DCE data were analysed taking into account of potential preference heterogeneity using both a mixed logit model (MLM) and a latent class logit model (LCLM).
Results: A total of 432 respondents consented to complete the questionnaires and 372 valid respondents were included in analysis. All attributes were significantly influencing respondents’ PHCS choice except for the types of service. Significant preference heterogeneity was observed among respondents. Based on the preferred LCLM estimates, four latent classes were identified. The first class (28.8%) valued modern medicine service the most, the second class (17.8%) was dominated by distance to practice, the third class (29%) preferred all the attributes except the types of services and valued TCM service most, the fourth class (24.4%) paid more attention to the types of service. Education, gender, age, income, regions of residence, and status of the chronic condition were found to be associated with latent class memberships.
Conclusion: A better understanding of the relative importance of PHCS characteristics is a crucial step for the future policy implementations. The significant preference heterogeneity identified in this study highlights that effective policy interventions should be tailored to different patients’ characteristics.
Keywords: discrete choice experiment, older adults, chronic diseases, preference heterogeneity, primary healthcare service
Introduction
As the pace of ageing accelerating, healthcare delivery in China is challenged by the increasing number of older adults with chronic disease.1 Between 2010 and 2018, China’s older adults (≥60) soared from 177 million to 249 million.2,3 One of the major concerns in the ageing society was deemed as the heavy burden of chronic diseases.3 In 2015, more than 69.13% of older people in China suffered from at least one chronic illness and the prevalence of multimorbidity was 43.65%.4 As the health status deteriorates, older adults will seek healthcare services more frequently and intensively.5 Current interventions for the elderly related to chronic diseases (including medical treatment and prevention) require a substantial amount of resources.6 The average length of stay (ALOS) for admitted older adults with chronic disease was 27.43 days annually, costing 2618.16 CNY per time.7 It is imperative for China to address how to meet the increasing healthcare need and allocate limited healthcare resources more efficiently in an ageing society.
World Health Organization (WHO) has recommended that chronic disease control at the community level is one of the effective avenues to cope with the rapidly increasing disease burden and meet the healthcare needs of older adults.1 As part of China’s new healthcare reform which was initiated in 2009, the government aimed to rebuild an effective primary healthcare system to allocate healthcare resources better and relieve the burden of chronic diseases.8 Encouraging patients with minor chronic diseases to seek primary healthcare services (PHCS) is one of the most crucial ways to achieve this goal.9 The government increased its subsidies to primary healthcare (PHC) institutions from 19 billion CNY (2.8 billion USD) in 2008 to 198 billion CNY (30 billion USD) in 2018.10,11 The number of PHC centers has also increased from 858,015 (2008) to 943,639 in 2018, which are 47 times of the total number of hospitals (19,693 in 2018);10 however, it only provided 53% of outpatient care (4.4 billion visits) and 17% of inpatient care (43.8 million hospital admissions) in China.10 The Occupancy rate of hospital beds of the hospital (84.2%) was 1.6 times of the primary healthcare centers (52%), and more than 70% of patients with general diseases and chronic diseases chose to visit tertiary hospitals.10,12 By far, the reform has not yet shown a significant expected effect on improving the utilisation of PHCS.13
Many countries start to value public preferences in healthcare policy decision-making.14 The United States Food and Drug Administration (FDA) has issued guidance to incorporate patient preferences into their decision-making15 and approve new treatments referring to patient preferences.16 Accounting for consumer’s preferences in health policy and system design can improve health outcomes and levels of satisfaction,17 and help policymakers to optimize service provision for targeted people. However, healthcare reform in developing countries often runs the risk of failing to cater for the neediest majority.18 This is not an exception in China. Research has also shown that even in developed countries, older people were less likely to be involved in medical consultations and shared-decision making than younger people, their concerns were often ignored or dismissed.19 Redesigning the primary healthcare system to promote the policy tailored to actual contexts needs more scientific evidence from the patients’ perspective.
The discrete choice experiment (DCE) is a stated preference method that has gained popularity in health services research to understand the patients’ preference for healthcare service.20 Comparing with the revealed preference survey which is based on real market data, DCEs can be used to investigate the healthcare services that are not yet on the market and to reflect the expectation of respondents.21 Furthermore, by including the cost attribute, the DCE can quantify the relative importance of each attribute or characteristic by calculating the marginal willingness to pay (MWTP).22 The literature reported several PHCS characteristics that were valued by patients, such as physical accessibility, financial accessibility, professional skill of care provider.23 China is a unique country in the world that both modern medicine (MM) and traditional Chinese medicine (TCM) are operated alongside each other and respected at every level of the healthcare system. However, there is a lack of empirical studies to explore the impacts of TCM, MM and the integration of TCM and MM on patients’ preference for primary healthcare.
There is also evidence suggesting that patients’ preference for healthcare intervention is not homogeneous.24 Ignoring preference heterogeneity may bias the utility estimates derived from DCE studies.25 A better understanding of influential and differential factors that underpin preference heterogeneity is required if they are to be used to drive decision-making in health.26 However, there is limited information about preference heterogeneity in the delivery of primary healthcare for older adults with chronic disease.
By using the DCE technique with respondents recruited from different regions of mainland China, this study aimed to understand the preferences of older adults with chronic diseases to facilitate the development of more effective policies to encourage the utilization of PHCS in China. The potential preference heterogeneity of respondents was investigated in detail. The results of this study will shed light on the current health reform in China.
Methods
The DCE was conducted in accordance with the four stages proposed by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Conjoint Analysis Task Force Report.27 Literature suggests that it has an advantage over other stated preference techniques for the elicitation of preferences in a less abstract way.28 A previous study in mainland China has also demonstrated that conducting DCEs among the elderly with lower education level is feasible.29
Establishing the Attributes and Levels
The whole process of the selection of attributes and their levels followed three steps: 1) A literature review on the key topic; 2) Conducting a semi-structured interview among patients; 3) Developing an expert group interview. To identify the initial attributes and their corresponding levels, a rapid literature review was firstly performed in the Web of Science and China Academic Journals Full-text Database (also known as CNKI). Search terms consisted of keywords and terms including “primary healthcare”, “primary health care”, “primary care”, or “general practice” combined with “expectation”, “priority” or “preference”, and “review”. Searched articles were excluded if (i) the studies were not directly related to the preference for primary healthcare; (ii) the full text was not available (eg, conference abstract) (refer to Table S1 including the specific search strategy and the results). Based on a rapid review and the context of the Chinese healthcare System, eight important attributes were considered: the seniority of medical practitioner, distance to practice, waiting time, treatment options, types of service, out-of-pocket (OOP) cost, professional skill, shared-decision making.
To ensure the validity of the DCE, we recruited 10 patients with chronic diseases to participate in a semi-structured interview in March 2017 in Wuhan, China. All interviewees had a clinician-confirmed diagnosis of chronic diseases and currently or previously had primary care-seeking experiences. The mean age of this group participants was 64.9 years (range 60–70 years; SD=3.0 years), and 50% were female. Following the semi-structured interview guide, the participants were asked to debate on the importance of eight attributes in primary healthcare-seeking. They were also offered opportunities to propose new attributes. No new attribute was proposed, and the wordings of the proposed attributes are suitable. Besides, six patients thought that the shared-decision making would not influence the choice of PHCS, seven patients considered that the level of care provider already represented the professional skills, and eight patients thought that far distance to practice was more uncomfortable than long waiting time. More than half of the respondents considered the remaining five attributes were important to the PHCS. Consequently, professional skills, shared-decision making, waiting time were excluded.
Next, one expert group interview with nine specialists (four GPs and five researchers) was further conducted in April 2017 in Wuhan, China. It was aimed to understand, from the supply-side, whether health professionals think the key attributes have all been included and whether any other potential attributes were relevant. During this process, the specialists put forward a new treatment option level “integrated Traditional Chinese Medicine and modern medicine”. It was considered as one of the crucial concerns in determining Chinese patients’ health-seeking behavior and then was included in the DCE. The wordings of the final five attributes and levels are refined in Table 1.
 |
Table 1 DCE Attributes and Attribute Levels |
Experimental Design
Based on the attributes and levels, there are 72 possible profiles, and 2,556 [=72* (72–1)/2] possible combinations of pairwise choice questions. An orthogonal design was used to generate a total of 18 choice tasks initially in the IBM SPSS Statistics (version 22.0) software. After deleting two unrealistic choice alternatives, 16 manageable choice tasks were determined (with two blocks such that each respondent answered eight choice sets). An additional dominant choice task (in which one alternative should clearly be chosen) was also included as the first task to serve as a rationality test. Prior evidence suggests that unforced options are preferable.37 Since the key objective of this study was to identify patients’ preference for the relative importance of those attributes for future policy implementation, rather than to predict the take-up rate among participants, the opt-out option was excluded to reduce the cognitive burden of respondents. An example choice set presents in Table 2.
 |
Table 2 An Example of a Choice Set from the Discrete Choice Experiment |
Besides the DCE section, there are three other sections in the questionnaire. Section A included a series of questions regarding respondents’ socio-demographic characteristics (eg, gender, age, marital status); Section B was about their medical insurance status; Section C assessed the disease burden of respondents (eg, the status of chronic conditions, the self-rated economic burden of chronic disease).
Before finalizing the whole questionnaire, we conducted a pilot for 30 patients with chronic diseases aged over 60 years in the Qiaokou community, Wuhan city to check if respondents can understand the DCE tasks and whether they have any other suggestions on formatting the questionnaire. We refined the format and layout of questionnaires according to their feedbacks. Overall, respondents indicated that the survey was easy to be understood and the number of choice tasks was acceptable.
Data Collection
Our sample satisfies the minimum size suggested based on the rule of thumb proposed by Orme:38
where n is the recommended minimum sample size, t is the number of tasks, a is the number of choices per task, and c is the maximum number of attribute levels in the DCE. According to the above formula, the minimum acceptable sample size of this DCE (t=8, a=2 and c=3) is 94 respondents.
A multistage strata sampling method was adopted to recruit respondents from different regions and development stages in mainland China. First, six administrative regions, namely Pudong New Area in Shanghai, Taizhou in Jiangsu province, Wuhan in Hubei province, Xuchang in Henan province, Guiyang in Guizhou Province, and Chengdu in Sichuan Province were selected representing eastern, middle and western China. A metropolis and a micropolis were randomly selected from each of the three regions (see Table S2). Within each city, six community healthcare centers (CHCs) were chosen based on their availability by the local health bureau. Respondents were recruited by the sampled CHCs. Considering the possibility of investigating preference heterogeneity, we aimed to invite 15 respondents through each CHC, which equivalent to the target sample size of 540 respondents in total. Respondents’ inclusion criteria were as follows: (1) Chinese ethnicity; (2) age 60 or above; (3) suffering from one or more chronic diseases which must have been formally diagnosed according to the medical record; (4) voluntary to participate in this survey. Exclusion criteria included the adults with cognitive impairment, mental diseases, and currently suffering from aphasia, deafness or other communication disorders that influenced the completion of investigations. The strata was pre-defined by gender quota (female: male, 53:47).39 The directors of the selected CHCs contacted the qualified respondents from the local residential registration databases based on the recruit criteria and strata of gender.
The survey was conducted by the study coordinators who have been trained to administer the questionnaires following the study protocol to ensure giving consistent information. Study coordinators administered the questionnaires via a one-to-one, face-to-face interview to ensure the quality of the responses. Before conducting the surveys, the study coordinators introduced the study, explained the meaning of each attribute and assisted respondents in completing the questionnaires. CHCs provided separate rooms for the interviews. On average, it took respondents 40 mins to complete a whole questionnaire. Each respondent received a set of tableware (valued at 30 CNY, 4.25 USD) as a gift after completing the survey. The survey was conducted from May 2017 to August 2018.
Data Analysis
The DCE data were analyzed under the random utility theory.40 The utility (U) of alternative j for individual i in the choice set k was specified as:
where  was an explanatory vector of the observed attribute and β is a vector of coefficients that represent the corresponding strength of preference to be estimated. The error term
was an explanatory vector of the observed attribute and β is a vector of coefficients that represent the corresponding strength of preference to be estimated. The error term  was assumed to be independently and identically distributed as a type 1 extreme value.
was assumed to be independently and identically distributed as a type 1 extreme value.
Considering the potential preference heterogeneity, a mixed logit model (MLM) was used. It estimates both a mean coefficient and a standard deviation for each attribute level.41 In order to calculate the MWTP, the OOP attribute was modelled as fixed parameters for avoiding divisions by zero and positive coefficients for cost.42 Other attributes were modelled as random coefficients which were specified to be normally distributed.22 Statistically significant coefficients demonstrate the importance of those attributes in influencing preferences and determining overall utility. Coefficients with a positive sign show that respondents valued that particular attribute level, whereas coefficients with a negative sign show that respondents were averse to that attribute level. Statistically significant standard deviations (p<0.05) indicate the existence of preference heterogeneity among respondents. Effects coding was used for all attributes except for OOP attribute, which was included as a continuous variable in the regression analyses. The utility function to be estimated using MLM can be specified as (the variable-specific information is shown in Table S3):
 represents the observable relative preference of patient (i) for the primary healthcare service (j), which can be defined as a sum of preference scores for attributes/levels.
represents the observable relative preference of patient (i) for the primary healthcare service (j), which can be defined as a sum of preference scores for attributes/levels.  is the constant and
is the constant and  are the mean attribute utility weights.
are the mean attribute utility weights.  represents the random parameter for patient i. The relative importance (RI) of each attribute represents the relative weight of its impact on decision making.18 Based on the MLM estimates, these were calculated via dividing the utility range of each attribute by the sum of utility ranges for all attributes.43
represents the random parameter for patient i. The relative importance (RI) of each attribute represents the relative weight of its impact on decision making.18 Based on the MLM estimates, these were calculated via dividing the utility range of each attribute by the sum of utility ranges for all attributes.43
The latent class logit model (LCLM) is an alternative approach to study preference heterogeneity. By using the respondents’ characteristics, we can get a better understanding of the latent class membership. As recommended in the literature, the optimal number of classes was selected using log-likelihood tests, information criteria (Akaike Information Criterion (AIC), Bayesian information criterion (BIC)) and consistent Akaike information criterion (CAIC)), model parsimony and also in terms of appropriate interpretation of classes.44 The information criteria can also be used to select the preferred models between MLM and LCLM. The socio-demographic characteristics that used to predict latent class membership include gender, age, marital status, education, income, the self-rated economic burden of chronic disease and status of the chronic condition (Table S3). All respondents’ characteristics were dummy coded, except age and income, which were included as continuous variables. The final model specification contains respondents’ characteristics that were statistically significant (p<0.05) in predicting latent class membership.
MWTP represents the rate at which the participants were willing to tradeoff gains relative to one criterion against losses relative to another. We calculated the MWTP for the attributes by taking the ratio of the coefficient of an attribute to the monetary attribute. We used the MWTP to examine the tradeoffs between different attribute levels. All analyses were conducted in Stata version 15.0 (College Station, TX: Stata Corp LLC.).
Results
Respondents
Over the data collection period, 540 community-dwelling older adults with chronic diseases were telephoned to be invited to join the study, and 432 older patients were recruited and filled out the survey. Among them, 372 respondents (a valid response rate of 68.9%) passed the dominant choice task and were included in the main analyses.
Table 3 presents the socio-demographic characteristics of respondents. The mean (±SD) age was 71.2±7.1 years and ranged from 60 to 91 years. More patients were female (64.5%) and had a higher education level (ie high school or above, 55.6%). The vast majority (97%) of the respondents have enrolled with at least one type of medical insurance schemes. Among participants, 34.9% suffered from more than two chronic diseases. More than half of the participants perceived a high or severe economic burden of chronic diseases.
 |
Table 3 Characteristics of Participants |
Discrete Choice Experiment: Mixed Logit Estimates
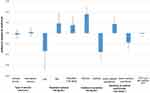
Figure 1 and Table S4 show the results of the mixed logit model. It can be seen that all attributes were highly significant except for the types of service. Overall, PHCS was preferred when the treatment options were integrated TCM and MM service, and when the distance to practice was closer, the seniority of medical practitioner was the junior medical practitioner, and OOP cost was lower. The significant standard deviations (SDs) of attribute levels further suggest the existence of preference heterogeneity across respondents (Table S4). SDs of all attribute levels except integrated TCM and MM service were significant. Patients’ preferences for the TCM service had relatively high significant SD compared to other attribute levels, followed by the MM service. It indicates higher uncertainty among respondents for the attribute levels of the treatment option.
The relative preference weights with a 95% confidence interval are illustrated in Figure 1. The corresponding RI of non-monetary attributes indicated that respondents considered the distance to practice as the most important attribute of PHCS (relative importance=40.1%; Figure 1). PHCS with closer distance to practice (<30mins) was preferred over service further away. The next most highly valued were treatment options, seniority of medical practitioners.
Discrete Choice Experiment Results: Latent Class Estimates
In Table S5, we estimated a series of LCLM with different numbers of classes and compared them using model parsimony, four goodness of fit measures (log-likelihood tests, BIC, CAIC, and AIC) and sound interpretation of classes. The results identified that four classes fit the data better than models with 2, 3, or 5 classes and the mixed logit model (Table S5). The main results of the final latent class model are summarized in Table S6 and Figure 2, and MWTP estimates of all attribute levels and their confidence intervals in each latent class are presented in Table S7. Average class probabilities within the respondent population were 28.8%, 17.8%, 29.0% and 24.4% for latent classes 1 to 4, respectively. Gender, age, education, income, the region of residence, and status of chronic conditions are identified as important factors in explaining preference heterogeneity. Marital status and self-rated economic burden of chronic disease did not predict class membership (p >0.05).
 |
Figure 2 Latent Class model estimates: Likelihood of preferring PHCS scenario for each latent class (OR with 95% CI). |
Latent Class 1
The treatment option was the most important consideration for respondents in this class; the likelihood of members of this class preferring a PHCS was significantly increased when the treatment option was MM service (OR=4.02, 95% CI 3.24–5.01) or integrated TCM and MM service (OR=1.29, 95% CI 1.04–1.59). MWTP suggests that MM service, integrated TCM and MM service were highly valued by the members in class 1 as worth around 348 CNY (49.22 USD), 63 CNY (8.91 USD) respectively. Respondents in class 1 preferred senior medical practitioners (OR=1.23, 95% CI 1.08–1.40) rather than the junior medical practitioner, and they would on average be willing to pay 51 CNY (7.21 USD) for PHCS provided by the senior medical practitioner. The decrease in OOP cost for a visit was less influential on preferences than the seniority of medical practitioners. Respondents in class 1 (28.8%), compared to reference class 4, were significantly likely to live in the eastern region, having a higher income and education level.
Latent Class 2
Distance to practice (<30mins, OR=5.20, 95% CI 3.35–8.09) was most influential for respondents in class 2, followed by the OOP cost for a visit (OR=0.99, 95% CI 0.98–0.99). Patients would on average be willing to pay 234 CNY (33.10 USD) for a reduction in distance to practice for less 30 mins. Types of service, treatment options, and the seniority of medical practitioners did not significantly influence preferences for PHCS. The members of class 2 (17.8%) tended to be older and live in the western region.
Latent Class 3
Preferences for PHCS of class 3 were more multidimensional. The treatment option was the most important consideration for respondents in class 3. It was exactly opposite to the members in class 1 that when the treatment option was the TCM service (OR=1.86, 95% CI 1.59–2.17), the odds of preferring the PHCS were significantly higher. MWTP suggested that the members of this class would be willing to pay 296 CNY (41.87 USD) to seek PHCS with TCM service. They were willing to take MM service only when compensated 370 CNY (52.33 USD). Unlike respondents in class 1, this class more likely preferred the junior medical practitioner (OR=1.45, 95% CI 1.31–1.60), and they were willing to pay 177 CNY (25.04 USD) for PHCS provided by the junior medical practitioner. The reduction in distance to practice and OOP cost were all less influential on preferences than TCM service and junior medical practitioners. All attributes except types of service significantly influenced preferences (p < 0.05). In class 3 (29.0%), respondents more likely to be female and multimorbid.
Latent Class 4
Respondents from Class 4 appeared to be primarily focused on the types of service and OOP cost for a visit. The likelihood of members of this class preferring a PHCS was significantly increased when the type of service was a general service (OR=1.36, 95% CI 1.01–1.83), and respondents would on average be willing to pay 8 CNY (1.13 USD) for general service. The OOP cost for a visit followed, and the odds of preferring the PHCS were significantly lower with the increasing level of OOP cost (OR= 0.96, 95% CI 0.95–0.97). Compared with class 1, members in class 4 (24.4%) tended to have a lower income level.
Discussion
By using a DCE, this study investigated the characteristics that matter for the choice of PHCS in mainland China among older adults with chronic disease. To the best of our knowledge, this is the first DCE study that focused on older patients’ healthcare seeking in China. Our results revealed significant heterogeneity in respondents’ preferences for PHCS. The mixed logit estimates indicate the existence of preference heterogeneity of all attributes. Furthermore, the latent class analysis identified four distinct classes with substantially different patterns in their preferences, and this new information complements the current literature on older patients’ preferences over PHCS.
A unique attribute considered in this study is the treatment option. TCM is considered to be slow in action but more thorough in “curing the root of the problem”, while western medicine is “more powerful and quick” but may also cause significant side effects.45 Previous studies suggest that the middle-aged and older patients in China significantly more preferred TCM for the treatment of common chronic conditions.46 Our research indicates that there still exists preference heterogeneity for TCM service among elderly patients, while respondents’ characteristics such as gender, education level and income are identified as important variables in explaining preference heterogeneity for TCM service or MM service. Female and multimorbid patients (class3) showed a strong preference for TCM service. This may because they are more sensitive about self-health,47 the TCM service has been proved to be relatively safe in the treatment of chronic diseases48 and can improve the life quality in a patient-centered and healing-oriented manner with fewer side effects,49 which leads to its high acceptance in the group with vulnerable health. On the other hand, the MM service has been found to be more attractive to older patients with higher educational level and high income (class 1), which is consistent with previous studies that, people with high socioeconomic status (SES) tend to have higher trust in MM service.50 As the results of the full sample showed, respondents presented an average positive preference for the integrated TCM and MM service. Integrated TCM and MM service can combine TCM and MM to maximize the positive effects and improve the quality of life of patients with chronic diseases effectively.51 It indicates that an integrated approach to control chronic diseases by using a combination of TCM and MM treatments is acceptable and could play an important role in primary healthcare in China.
Among non-monetary attributes, the distance to practice is the most important one. With the distance to practice increasing, the possibility of choosing PHCS decreases, which is consistent with the results of previous studies.52 It is worth noting that the uncertainty also exists among the preferences of older patients for distance to practice. Older patients who live in the western region and the more senior patients (class 2) are more sensitive about the distance to practice. Previous studies found that comparing eastern and central China, the PHCS availability in the western region is more inadequate.53 Age is always associated with mobility impairment.54 Therefore, this attribute is more important in class 2, in which the patients are more senior and living in the western China.
Patients’ choice of a medical practitioner is not always a rational and straightforward process.26 Their SES and previous experience may influence the preference for the primary medical practitioner. Older patients with high SES (class 1) may be more quality-oriented and preferred the senior medical practitioners to provide PHCS.55 In contrast, some patients often attach great importance to their own healthcare experience than comparative information. Since 2009, community health service centers have delivered health management services for the elderly, usually provided by the junior general practitioners. Familiarity and availability may play a role, as the respondents in class 3 who are female and multimorbid. Female and multimorbid patients may pay more attention to health. They have more experience in seeking PHCS.56,57 They may tend to stay with their current provider. The positive experience influences their attitudes and future choices.25
Although the types of service are not significant for the full sample, respondents in class 4 who have a lower income level show a preference for the general service comparing with specialized service in the hypothetical minor disease scenario. Previous literature finds that people with disadvantaged SES are more willing to access general service, which presumably are easier to be affected by financial attribute (cost).24 More specialised services are provided in tertiary hospitals currently in China’s health system. Some respondents suggested that they would like to get more specialized general practices in the PHCS, and they may seek advice from the medical guide staff to choose the types of service in healthcare seeking.
Preference heterogeneity is an important consideration from the policy perspective aiming at the greater individualization of primary healthcare. The current hierarchical medical system put forward that the provision of TCM services and the training of general practitioners should be enhanced in primary healthcare institutions.9 Encourage senior physicians from urban higher hospitals to practice in more primary healthcare institutions.9 These findings from latent class estimates highlighted that for a country with huge regional socioeconomic differences, the policies of provision to PHCS should be tailored to local conditions rather than one-size-fits-all strategies. The quality of PHCS is the core appeal for older patients with higher SES and living in the eastern region (class 1). Improving the medical practice skill of the primary medical practitioner, widely apply the integrated TCM & MM services and enhance the dissemination of correct TCM knowledge will improve the utility of PHCS utilization for this targeted population. The geographical and financial accessibility should be targeted as the priority for older patients with mobility impairment and live in the western region (class 2). Due to the weak mobility of older adults with chronic disease and poor PHCS availability of the western region, primary healthcare centers can consider providing distance supports and assistance to the targeted older patient population through telemedicine technology. For the vulnerable health groups, which consist of the female and multimorbid older patients (class 3), the policy implementation of PHCS delivery will need to be multidimensional. Except considering the geographical and financial accessibility, the provision of TCM service and the familiar medical practitioner involving PHCS can take account in delivery policy for the targeted population. It is worth noting that all the respondents present a preference for the lower OOP cost, which indicates that the price lever worked in guiding all the older patients to use PHCS. Especially in older patients with lower income (class 4) who preferred general service, the larger gap of the reimbursement ratio among the general services from different levels of health facilities might help increase their utilization of primary health institutions.
This study has some limitations. First, although we maximize the sample size based on the rule of thumb by Orme, the minimum sample size requirement based on the parameter estimates are preferred. Second, the design of the survey using the regional quota method ensured that our sample of respondents was representative of the Chinese community-dwelling adults ≥60 years old with chronic disease in terms of geographical location. However, the actual sampling existed a limitation due to the practical difficulties of random sampling. The recruitment remained the bias of gender, education levels, and SES. There were more females than males among the respondents in our study. During the survey process, the female patients were found to be more cooperative and willing to participate in the survey. Moreover, the types of service were found to be non-significant in the whole sample, it might be related to the recruitment of the interviewees who selected attributes and levels in the focus group. Latent class estimates suggested that types of service may be an important factor for certain patients choosing the PHCS. All the interviewees in the focus group were from Wuhan, while the respondents in this study came from different provinces and cities. It may cause some deviations that the result of focus group interview may not broadly represent viewpoints of whole patients. Moreover, the DCE is a valid method to understand preference, its results may indicate the preferences at the time of the survey.31
Conclusion
Considering that older adults are the key components of the chronic disease population, this study used DCE to investigate key factors influencing older patients’ preferences for PHCS in the minor disease scenario in China. Relatively large heterogeneity in older patients’ preferences for PHCS was detected. To the extent that we can identify four classes of the older patient with distinct preferences for different service attributes. Education, gender, age, income, ill status, and regions of residence could predict the different preference classifications. These findings may help policymakers in delivering a primary care system better suited to the preferences of their core patients.
Abbreviations
AIC, Akaike information criterion; BIC, Bayesian information criterion; CI, confidence interval; CHC, community healthcare center; CNY, Chinese Yuan; DCE, discrete choice experiment; LCLM, latent class logic model; Mins, minute; MM, Modern Medicine; MWTP, marginal willingness to pay; OOP, Out-of-pocket; OR, odds ratio; PHC, primary healthcare; PHCS, primary healthcare service; RI, relative importance; SD, standard deviation; SE, standard error; SES, socioeconomic status; TCM, traditional Chinese Medicine; USD, United States dollar.
Details of Ethics Approval
The study protocol and verbal informed consent were acceptable and approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG No: IORG0003571). All participants were informed of the purpose, method and publication of the study, that participation was anonymous and voluntary, and that they could withdraw at any time.
Acknowledgments
We are grateful to the Health Commissions of Shanghai Municipal, Taizhou Municipal, Xuchang Municipal, Wuhan Municipal, Chengdu Municipal, Guizhou Municipal for assistance at the stage of data collection. We would like to thank all the participants for their involvement. This study was funded by the National Natural Science Foundation of China (Grant number 71673095). Gang Chen, Ph.D., contributed to the polishing and advised on statistical analysis.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work. Gang Chen, Ph.D., who contributed to the polishing and advised on statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. China country assessment report on ageing and health. Geneva: World Health Organization; 2015. Available from: https://www.who.int/ageing/publications/china-country-assessment/en/.
2. National Bureau of Statistics. Bulletin of the sixth national population censusNational Bureau of Statistics; 2010. Available from: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/201104/t20110428_30327.html2011.
3. National Bureau of Statistics. Statistical communique of the People’s Republic of China on the 2019 national economic and social development. National Bureau of Statistics; Available from: http://www.stats.gov.cn/tjsj/zxfb/202002/t20200228_1728913.html2020.
4. Wei Yan YL, Zhang R, Chang F. Multimorbidity status of the elderly in China-research based on CHARLS data. Chin J Dis Control Prev. 2019;23(4):426–430.
5. Mohan G, Nolan A, Lyons S. An investigation of the effect of accessibility to general practitioner services on healthcare utilisation among older people. Soc Sci Med. 2019;220:254–263. doi:10.1016/j.socscimed.2018.11.028
6. Bloom DE, Chen S, Kuhn M, McGovern ME, Oxley L, Prettner K. The economic burden of chronic diseases: estimates and projections for China, Japan, and South Korea. J Econ Ageing. 2018;100163. doi:10.1016/j.jeoa.2018.09.002
7. Lj J, Wj Y. Analysis of change trend of chronic diseases of Chinese residents based on reports of five national health service surveys. Chin Health Ser Manag. 2018;35(11):874–876.
8. Liu Q, Wang B, Kong Y, Cheng KK. China’s primary health-care reform. Lancet. 2011;377(9783):2064–2066. doi:10.1016/S0140-6736(11)60167-0
9. Central People’s Government of the People’s Republic of China. Guiding opinions of the general office of the state council on promoting the construction of hierarchical diagnosis and treatment system. General Office of the State Council, PRC; 2015.
10. National Health Commission of the People’s Republic of China. China Health Statistics Yearbook 2019. Beijing: Peking Union Medical College; 2019.
11. Ministry of Health of the People’s Republic of China. China Health Statistics Yearbook 2009. Beijing: Peking Union Medical College; 2009.
12. Yong L. An empirical study on the selection behavior of patients in outpatient clinics under the background of hierarchical diagnosis and treatment. Chin Hosp Manag. 2020;40(6):50–54.
13. Zeng Y, Xu W, Chen L, Chen F, Fang Y. The influencing factors of health-seeking preference and community health service utilization among patients in primary care reform in Xiamen, China. Patient Prefer Adherence. 2020;14:653–662.
14. Abelson J, Giacomini M, Lehoux P, Gauvin FP. Bringing ‘the public’ into health technology assessment and coverage policy decisions: from principles to practice. Health Policy. 2007;82(1):37–50. doi:10.1016/j.healthpol.2006.07.009
15. United States Food and Drug Administration. Patient engagement in the design and conduct of medical device clinical investigations. Center for Devices and Radiological Health, Center for Biologics Evaluation and Research. 2019.
16. Peay HL, Hollin I, Fischer R, Bridges JF. A community-engaged approach to quantifying caregiver preferences for the benefits and risks of emerging therapies for duchenne muscular dystrophy. Clin Ther. 2014;36(5):624–637. doi:10.1016/j.clinthera.2014.07.001
17. Foster MM, Earl PE, Haines TP, Mitchell GK. Unravelling the concept of consumer preference: implications for health policy and optimal planning in primary care. Health Policy. 2010;97(2–3):105–112. doi:10.1016/j.healthpol.2010.04.005
18. Font JC, Forns JR, Sato A. Eliciting health care priorities in developing countries: experimental evidence from Guatemala. Health Policy Plan. 2016;31(1):67–74. doi:10.1093/heapol/czv022
19. Muscat DM, Shepherd HL, Hay L, et al. Discussions about evidence and preferences in real-life general practice consultations with older patients. Patient Educ Couns. 2019;102(5):879–887. doi:10.1016/j.pec.2018.12.001
20. McAteer A, Yi D, Watson V, et al. Exploring preferences for symptom management in primary care: a discrete choice experiment using a questionnaire survey. Br J Gen Pract. 2015;65(636):e478–488. doi:10.3399/bjgp15X685705
21. Ryan M, Watson V. Comparing welfare estimates from payment card contingent valuation and discrete choice experiments. Health Econ. 2009;18(4):389–401. doi:10.1002/hec.1364
22. Liu Y, Kong Q, de Bekker-grob EW. Public preferences for health care facilities in rural China: a discrete choice experiment. Soc Sci Med. 2019;237:112396. doi:10.1016/j.socscimed.2019.112396
23. Kleij KS, Tangermann U, Amelung VE, Krauth C. Patients’ preferences for primary health care - a systematic literature review of discrete choice experiments. BMC Health Serv Res. 2017;17:12. doi:10.1186/s12913-017-2433-7
24. Zhu J, Li J, Zhang Z, Li H, Cai L. Exploring determinants of health provider choice and heterogeneity in preference among outpatients in Beijing: a labelled discrete choice experiment. BMJ Open. 2019;9(4):e023363. doi:10.1136/bmjopen-2018-023363
25. Zhou M, Bridges JFP. Explore preference heterogeneity for treatment among people with Type 2 diabetes: a comparison of random-parameters and latent-class estimation techniques. J Choice Model. 2019;30:38–49.
26. Sever I, Verbic M, Sever EK. Valuing the delivery of dental care: heterogeneity in patients’ preferences and willingness-to-pay for dental care attributes. J Dent. 2018;69:93–101. doi:10.1016/j.jdent.2017.12.005
27. Reed Johnson F, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis experimental design good research practices task force. Value Health. 2013;16(1):3–13. doi:10.1016/j.jval.2012.08.2223
28. Milte R, Ratcliffe J, Chen G, Crotty M. What characteristics of nursing homes are most valued by consumers? A Discrete choice experiment with residents and family members. Value Health. 2018;21(7):843–849. doi:10.1016/j.jval.2017.11.004
29. Ye T, Wang M, Hu W, Liu Y, Shi P. High liabilities or heavy subsidies Farmers’ preferences for crop insurance attributes in Hunan, China. China Agric Econ Rev. 2017;9(4):588–606. doi:10.1108/CAER-06-2016-0093
30. Güneş ED, Yaman H, Çekyay B, Verter V. Matching patient and physician preferences in designing a primary care facility network. J Oper Res Soc. 2017;65(4):483–496. doi:10.1057/jors.2012.71
31. Li J, Feng XL. Health care-seeking behaviours and health expenditures in adults aged 45 years and older in China, 2011–2013. Trop Med Int Health. 2017;22(5):638–654. doi:10.1111/tmi.12865
32. Kleij KS, Tangermann U, Amelung VE, Krauth C. Patients’ preferences for primary health care - a systematic literature review of discrete choice experiments. BMC Health Serv Res. 2017;17(1):476. doi:10.1186/s12913-017-2433-7
33. Seghieri C, Mengoni A, Nuti S. Applying discrete choice modelling in a priority setting: an investigation of public preferences for primary care models. Eur J Health Econ. 2014;15(7):773–785. doi:10.1007/s10198-013-0542-8
34. Ministry of Health of the People’s Republic of China. Notice of the general office of the ministry of health on further promoting appointment diagnosis and treatment services. Medical Administration and Hospital Authority. 2011.
35. Tingting Yang JZ. Summarizing related policies and discussing problems about medical service prices in public hospitals. Chin Health Econ. 2015;34(12):66–68.
36. OECD. Exchange rates (indicator). Published 2020. Available from: https://data.oecd.org/conversion/exchange-rates.htm.
37. Ravi Dhar AIS. The effect of forced choice on choice. J Mark Res. 2003;40(2):146–160.
38. Finkelstein EA, Bilger M, Flynn TN, Malhotra C. Preferences for end-of-life care among community-dwelling older adults and patients with advanced cancer: a discrete choice experiment. Health Policy. 2015;119(11):1482–1489. doi:10.1016/j.healthpol.2015.09.001
39. National Health Commission of the people’s republic of China. China Health Statistics Yearbook 2018. Beijing: Peking Union Medical College; 2018.
40. Chang JB, Lusk JL. Mixed logit models: accuracy and software choice. J Appl Econom. 2011;26(1):167–172. doi:10.1002/jae.1201
41. Johnson J, Howard K, Wilson A, Ward M, Gilbert GL, Degeling C. Public preferences for one health approaches to emerging infectious diseases: a discrete choice experiment. Soc Sci Med. 2019;228:164–171. doi:10.1016/j.socscimed.2019.03.013
42. Bliemer MCJ, Rose JM. Confidence intervals of willingness-to-pay for random coefficient logit models. Transport Res B-Meth. 2013;58:199–214.
43. Lancsar E, Louviere J, Flynn T. Several methods to investigate relative attribute impact in stated preference experiments. Soc Sci Med. 2007;64(8):1738–1753. doi:10.1016/j.socscimed.2006.12.007
44. Pacifico D, Yoo HI. lclogit: a Stata command for fitting latent-class conditional logit models via the expectation-maximization algorithm. Stata J. 2013;13(3):625–639. doi:10.1177/1536867X1301300312
45. Chung VCH, Lau CH, Yeoh EK, Griffiths SM. Age, chronic non-communicable disease and choice of traditional Chinese and western medicine outpatient services in a Chinese population. BMC Health Serv Res. 2009;9(1):1–8. doi:10.1186/1472-6963-9-207
46. Liu T, Li X, Zou ZY, Li C. The prevalence and determinants of using traditional chinese medicine among middle-aged and older Chinese adults: results from the China health and retirement longitudinal study. J Am Med Dir Assoc. 2015;16(11):1002e1001–1005. doi:10.1016/j.jamda.2015.07.011
47. Boye LK, Mogensen CB, Mechlenborg T, Waldorff FB, Andersen PT. Older multimorbid patients’ experiences on integration of services: a systematic review. BMC Health Serv Res. 2019;19(1):795. doi:10.1186/s12913-019-4644-6
48. Jiang M, Zhang C, Cao H, Chan K, Lu A. The role of Chinese medicine in the treatment of chronic diseases in China. Planta Med. 2011;77(9):873–881. doi:10.1055/s-0030-1270983
49. Fan X, Meng F, Wang D, et al. Perceptions of traditional Chinese medicine for chronic disease care and prevention: a cross-sectional study of Chinese hospital-based health care professionals. BMC Complement Altern Med. 2018;18(1):209. doi:10.1186/s12906-019-2434-7
50. Cai Y, Mao Z, Xu B, Wu B. Factors associated with traditional Chinese medicine utilization among urban community health centers in Hubei Province of China. Asia Pac J Public Health. 2015;27(2):NP2489–2497. doi:10.1177/1010539513491415
51. Wang Y, Xie B, Tao Y, Ma Y, Zhang K. Impact of community-based integrated traditional Chinese and Western medicine metabolic syndrome intervention technology in rural residents in Southern Jiangsu, China. Med Sci Monit. 2015;21:2163–2169. doi:10.12659/MSM.893972
52. Hu X, Zhang H, Sun X, et al. Older adults’ choices of first-contact care and related factors in Zhejiang and Qinghai Province, China. Geriatr Gerontol Int. 2019;19(9):938–944. doi:10.1111/ggi.13746
53. Tang S, Meng Q, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. 2008;372(9648):1493–1501. doi:10.1684/pnv.2016.0591
54. Bonnefoy M, Berrut G, Gilbert T. Prevention of impaired mobility in the elderly in primary care: a brief report. Geriatrie Et Psychologie Neuropsychiatrie De Vieillissement. 2016;14(1):16–22.
55. Sable-Smith A, Arnett KR, Nowels MA, Colborn K, Lum HD, Nowels D. Interactions with the healthcare system influence advance care planning activities: results from a representative survey in 11 developed countries. Fam Pract. 2018;35(3):307–311. doi:10.1093/fampra/cmx113
56. Chylinska J, Lazarewicz M, Rzadkiewicz M, et al. The role of gender in the active attitude toward treatment and health among older patients in primary health care-self-assessed health status and sociodemographic factors as moderators. BMC Geriatr. 2017;17(1):284. doi:10.1186/s12877-017-0677-z
57. Li H, Ai-juan MA, Kai F, Jing D, Chen X. The awareness rate, treatment rate, control rate of dyslipidemia and the influencing factors in the residents (18–65 years old) of Beijing. Chin J Prev Control Chronic Dis. 2017;25(7):489–493. doi:10.16386/j.cjpccd.issn.1004-6194.2017.07.003
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.