Back to Journals » Cancer Management and Research » Volume 12
Predictors of Resilience Among Parents of Children with Cancer: Cross-Sectional Study
Authors Mezgebu E, Berhan E, Deribe L
Received 11 August 2020
Accepted for publication 4 November 2020
Published 16 November 2020 Volume 2020:12 Pages 11611—11621
DOI https://doi.org/10.2147/CMAR.S276599
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chien-Feng Li
Esubalew Mezgebu,1 Emebet Berhan,2 Leul Deribe2
1Jimma Medical Center, Pediatrics Oncology Unit, Jimma, Ethiopia; 2Addis Ababa University College of Health Science, School of Nursing and Midwifery, Addis Ababa, Ethiopia
Correspondence: Leul Deribe
Addis Ababa University College of Health Sciences, School of Nursing and Midwifery, Addis Ababa 4412, Ethiopia
Tel +251 911 97 39 83
Email [email protected]
Purpose: Resilience is an ability to overcome adversities in response to a potentially traumatic event. It relieves parents’ discomfort and builds personal capacity when facing a stressful situation like childhood cancer. Therefore, the study’s objective is to assess the magnitude of resilience and its predictors among the parents of children with cancer at Jimma medical center, Ethiopia, 2020.
Methods: The institutional-based cross-sectional design was employed on 126 parents of children with cancer at Jimma Medical Center. All study populations who attend the hospital from February 25 to April 25, 2020, and fulfill the inclusion criteria were included. Data were entered into Epi data version 4.6.0.2 and analyzed by SPSS version 25. Descriptive analysis was used to describe the study variables. Furthermore, linear regression analysis was calculated to assess predictors of resilience.
Results: The level of resilience among parents’ children with cancer were a mean scored 51.41± 12.02. In this study, factors associated with resilience were receiving support from friends (β=5.67, 95% CI=1.58, 9.77; P=0.007), attend recreational activities (β=13.8, 95% CI=5.32, 22.37; P=0.03) and receiving health information from health care professionals (β=6.37; 95% CI= (1.75, 11.00), P=0.007), parents depression (β= − 0.827, 95% CI= (− 1.619,-0.034), P=0.041) and parents stress (β =− 0.88,95% CI (− 1.54,-0.23), P=0.031).
Conclusion: The magnitude of resilience among parents of children with cancer was low relative to other studies. Support from friends, attending recreational activities, and receiving health information from health care professionals were positively associated with resilience. In contrast, parents’ depression and stress were negatively associated with resilience.
Keywords: resilience, Jimma Medical Center, parents of children with cancer
Introduction
Childhood cancer is a life-threatening illness and a leading cause of child mortality in low and middle-income countries.1 As stated by a world health organization, every year, 300,000 new cases are diagnosed with cancer in children aged between 0–19 years.2 The most common childhood cancers are leukemia, brain cancer, lymphomas, and solid tumors like neuroblastoma and Wilm’s tumor.3 Each year, 100,000 children less than fifteen years of age lose their life by cancer, and most of the death, around 90% occurs in developing countries. Lack of specialized human power in cancer, correct diagnosis, and treatment and expensive cost of the drug, and diagnostic investigation causes decreased survival rates in low and middle-income countries.4
The global burden of cancer estimated the incidence rate of East African countries like Tanzania at 134 new cases per million, and the Extrapolation from clinical documents at Tikur Anbessa Specialized Hospital (TASH) Radiotherapy Centre estimates that there was 120,500 new cancer cases/year, even though GLOBOCAN estimates are much less than 51,000 per year. Based on extrapolating estimates of new pediatric cancer cases in Ethiopia, there are 6000 new cancer cases per million. The most common childhood cancer in Ethiopia is leukemia, lymphoma, retinoblastoma, Wilm’s tumor, and bone and soft tissue sarcomas.5
Diagnosis of pediatric cancer implies one of the most significant challenges for the family: physical, mental, socioeconomic, and social effects on patients and their parents. These effects result in susceptibility and failure in parents’ quality of life and functioning.4 However, parents of children with cancer can positively adapt and cope with childhood cancer diagnosis and treatment despite these difficulties. Parents’ positive coping is indispensable for successfully provide care for their ill children. Coping is anything people do to adjust to the challenges and demands of stress or any adjustments made to lessen the negative impact of stress.6
A key reason behind effective coping with problems related to being parents of children with cancer is resilience. Resilience is an ability to overcome difficulties and the absence of psychological distress or adoption of a positive attitude in response to a potentially traumatic event. Commonly it is used to refer to parents’ ability to understand unfavorable psychological conflict when confronted with stressful conditions. It includes adaptability and capability to recover from traumatic events and stressful circumstances.7
Resilience allows parents to achieve a balance of emotions. Parents need to have the resilience and experience positive adaptive skills to successfully manage their children’s cancer and related difficulties.8 As a personal characteristic, resilience helps to ease parents’ discomfort and build personal capacity.9
The metatheory of resilience could be a basis for an explanation for resilience. Most of the resiliency studies showed that priory identifying either internal or external factors for resiliency helps an individual to easily find protective factors to cope with or “bounce back” in case of stressful situations. According to Richardson, the theory of resilience was categorized into three called “waves”. The first wave of research identifies qualities (protective factors) for a person to react positively to stressful events. The second research wave examined resilience in coping with stress, or difficulty, change, or opportunity. The third wave explains the finding of motivational forces within an individual and a group that drives them toward self-actualization in life.10
Most of the theories have a common consensus on resilience, as it is a dynamic process that can be changed. There would be a wide range of different factors that determine an individual practice of the resilience process itself. Different studies in different countries showed that there are variations in resilience across the countries. For example, in the study conducted in Iran and china on parents’ children with cancer, the mean resilience and standard deviation vary between 66.83–54.83 and standard deviation 14.28–12.88.7,8,11 There are different predictors which affect parents from being resilient these include: socio-demographic predictors,12–14 children health-related factors,15,16 psychological predictors,17,18 parents behavioral related predictors19–21 and service-related predictors.22,23
Therefore, determining the level and associated factors of resilience can help build capacity for positive adaptation to different health problems.24 Most studies on resilience have been conducted among parents of children with psychiatric illnesses and only included mothers. Thus, there is limited published research on resilience among parents of children with cancer involving both fathers and mothers. Besides this, it is studied insufficiently in Ethiopia, and no study was conducted particular to the study area. To fulfill this gap. We conducted this study to fill these gaps and assess parents’ resilience and predictors among parents of children with cancer at Jimma medical center (JMC). The hypothesis of the study was a level of resilience and factors affecting it are not homogeneously distributed. This study’s findings will contribute to healthcare providers’ need to identify potentially vulnerable parents and provide better psychological and educational support.
Methods and Materials
Study Area, Period, and Study Design
The facility-based cross-sectional study design was used from February 25-April 25, 2020, at Jimma Medical Center, Jimma Town. Jimma town is in Ethiopia’s southwest, 352 Km away from Addis Ababa (the capital city of Ethiopia). The hospital provides different services to the people living in Jimma town and its surroundings. Among the primary services, the pediatric hematology/oncology ward is the one that provides services to pediatric cancer patients. There are 22 beds with one oncologist, two residents, and 15 nurses in this ward, and it serves over 300 new pediatrics cancer patients per year.25
Participants
Because of a few patients’ flow, the study included all parents of children with cancer who visited the hospital during the data collection period and fulfilled the inclusion criteria. We approached 126 parents during the given period and obtained complete data from 122 parents. In this study parent is defined as “a person who has a significant emotional bond with the patient; this is a family member who is a part of the patient’s family life cycle, offers emotional-expressive, instrumental, and tangible support, and provides help and comprehensive care during the chronic illness, acute illness, or disability of a child”.26
In this study, children are those clients who are less than 18 years old, and parents or caregivers are those whose age is greater than 18 years old and live together with their child playing the role of caregiver to the sick child. Those parents’ children with suspected or unconfirmed diagnoses and those parents with critically sick children at the time of the interview were excluded from the study.
Data Collection Tool and Procedures
The data was collected using an interviewee-administered structured questionnaire adapted from different works of literature.11,15,18,27–29 The tools include questions related to parent socio-demographic characteristics, child health, anxiety depression and stress, and parent resilience.
Stress and anxiety were measured using depression anxiety stress scales (DASS); this scale comprised 21 items responded through a 4-point Likert scale (0=never, 1=sometimes, 2=often, and 3=almost always). Thus, the scores could range from 0 to 63, with higher scores showing higher depression levels, anxiety, and stress. Each of the sub-scales examines depression, anxiety, and stress with seven items for each. In the present study, the reliability test (Cronbach’s alpha coefficient) of the scale was 0.86.
Resilience was measured using 25 items Connor-Davidson Resilience Scale, a 4-point Likert scale (0-never true, 1-seldom true, 2-sometimes true, 3-often true 4-always true). The scale’s total continuous score can range from 0 to 100; the higher the score, the more resilient the parent is. It was developed by Connor and Davidson in the United States in 2003 with the reliability of Cronbach’s alpha 0.89.30 In the present study, the Cronbach’s alpha coefficients were 0.83. The tool was assessed and confirmed in different countries like China,31 India,32 Iran,33 Turkey,34 Korea,35 and South Africa.36 Also, it was translated and tested with different languages.30
The data was collected using four data collectors and one supervisor. The selection criteria for data collectors were having a BSc in the nursing, not working in the Jimma medical center and data collection experience.
Data Quality Control
The tools were prepared in English and translated into local languages, Oromiffaa and Amharic, because these were the most widely spoken languages. Then it was re-translated back to English by another person to check the consistency. The tool was pre-tested with fifteen parents before actual data collection. Before data collection, careful modification of the tool was made. The pre-test was conducted at a similar setting at Tikur Anbessa specialized hospital pediatric oncology unit. Two-days training was given for data supervisors and collectors on how to collect and handle the data.
Data Processing and Analysis
Before data was entered into Epi data version 4.6.0.2, it was checked for omissions, legibility of handwriting, and completeness by the principal investigator and supervisor and then exported to SPSS Version 25 for analysis. Missing value and outliers were cheeked and corrected. Recoding, categorizing, computing, counting, and other statistical analyses were made. Descriptive analysis (including means, standard deviations, frequencies, and percentages) were used to analyses the independent-samples, and the data were presented with tables, graphs, and frequencies.
First, simple linear regression was done to select candidate variables for multiple linear regression. All variables having P-value ≤0.25 during linear regression were selected for the multiple linear regression. After the multiple linear regression analysis, variables having p-values <0.05 were having a statistically significant association with parents’ resilience. The strength of the association between independent and dependent variables was described using unstandardized β with 95% CI.
The final fitted model was constructed using forced entry by multiple linear regression analysis methods. Multicollinearity was checked by examining the variance inflation factors (VIF), and it showed no multicollinearity on the final model: the value for each variable was less than ten.
Ethical Consideration
The study was conducted following the Declaration of Helsinki. Ethical clearance was obtained from the Ethics Review Board of Addis Ababa University, school of nursing and Midwifery (protocol No034/20/SNM). Further permission was received from the pediatric oncology unit at JMC. Each participant provided informed consent for the interviewee. To keep the physical privacy of respondents’ different place was prepared for interview purpose. Participants were guaranteed their right to withdraw from the interview at any time and told as participation in this study or refusal to take part would not affect the ability to access health services or any other services.
Names and other personal information, which can violate the study subjects’ confidentiality, were not taken or recorded. Any information was kept confidential. During data collection, parents having severe anxiety and severe stress were linked for further psychiatric consultation and treatment.
Result
Population
Socio-Demographic Characteristics of the Study Participants
Among 126 participants in the study period, 122 responded to the questionnaires fully, giving a response rate of 96.8%. Little more than half (54.1%) of the respondents were mothers. Concerning occupation, 70 (57.4%) mothers were self-employed whereas 85 (69.7%) of the fathers were self-employed. Besides, 86 (69.7%) of participants were rural in residents. Concerning marital status, 113 (92.6%) of the participants were married. Furthermore, 63 (51.6%) mothers cannot read and write, and 41 (33.6%) fathers had primary school education.
Regarding religion, seventy-one (58.2%) of the study subjects belonged to Muslims. Concerning social support, 104 (85.2%) reported receiving support from family. The respondents’ median monthly income was 2746.15 Ethiopian Birr (ETB), ranging between 500–8000 ETB. The mean (SD) distance of parent’s from JMC was 58.30±49.8km ranging about 1 to 200km (Table 1)
 |
Table 1 Socio-Demographic Characteristics of Parent’s Children with Cancer at Jimma Medical Center, Oromia, Ethiopia, February 25, 2012 to April 25, 2020 (n=122) |
Children Health-Related Factors, Parents’ Behavioral Characteristics, and Service-Related Information
More than half of (64.8%) of children with cancer were females. Moreover, the children’s mean age was 7.11 years and 4.09 standard deviation with a range of 1–18 years old. More than health-related (4%) of the children have no history of relapse. Besides, 107 (87.7%) of households have more than one child. Leukemia was the most common malignancy type among children, experienced by 59 (48.4%) participants. The majority of parents, 116 (95.1%), were not reported to have experience of recreational activities. Though, many of the participants, 62 (50.8%), had frequent contact with their religious leaders.
Among the study participants, 92 (75.4%) got information from the health care providers. Regarding the treatment, more than half, 76 (62.3%) of the treatment was chemotherapy. In addition, the treatment duration was averagely eight months, with a standard deviation of 5.54 months (Table 2).
 |
Table 2 Child Health Related, Parents Behavioral and Service-Related Characteristics at Jimma Medical Center, Oromia, Ethiopia, February 25, 2020 to April 25, 2020 (n=122) |
Psychological Characteristics of Participants
The mean and standard deviation score of depression was 19.04±6.48. As indicated in Figure 1, 50 (40.98%) had mild, and 6(4.91%) had moderate depression levels. Nevertheless, no one was diagnosed with severe and very severe levels of depression. Regarding level anxiety, the mean score and standard deviation were 15.14 and 6.58, respectively. Twenty-eight (22.95%) and 20 (16.39%) of the parents had mild and moderate anxiety levels, respectively. Besides, the mean and standard deviation score of stress was 15.64±6.98; 23 (18.85%) where mildly stressed, 10 (8.19%) where severely stressed, and 1(0.82%) where very severely stressed.
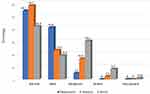 |
Figure 1 Psychological predictors for parent’s of children with cancer at Jimma medical center, Oromia, Ethiopia, February 25, 2012 to April 25, 2020 (n=122). |
Level of Resilience Parents’ Children with Cancer
The mean resilience among parents of children with cancer was 51.41, with a standard deviation of 12.02, ranging from 29 to 86. Sixty-five (53.3%) of study participants had a resilience score below the mean value. The result of an independent t-test showed that the magnitude of resilience among parents of children with cancer was different between mothers with a mean and standard deviation of 48.91±12.34 and fathers 54.48±1.99, respectively. “Sometimes fate or God can help me” had the highest mean score of 3.3 and 1.04 standard deviation. A mean, 0.98± 1.02, score for the phrase “make unpopular or difficult decisions” was the least. (Table 3).
 |
Table 3 The Frequency Distribution of Level of Resilience Among Parents’ Children with Cancer at Jimma Medical Center, Oromia, Ethiopia, February 25, 2020 to April 25, 2020 (n=122) |
Factors Associated with Resilience Among Parents of Children with Cancer
Simple linear regression analysis was done between each socio-demographic characteristics and resilience to select variables for multiple linear regression. Parents gender (p=0.01), mothers’ educational status (p=0.124), mother’s employment status (p=0.009), monthly family income (p=0.001) were selected from sociodemographic variables. Similarly, support from family (p=0.165), support from friends (p=0.001), and attending recreational activates (p=0.214) had P-value ≤0.25 and considered for further analysis. Similarly, the level of depression (p<0.001), level of anxiety (p=0.013), and level of stress (p<0.001) were a selected from psychological variables for further multiple linear regression analysis.
Among service-related variables, parents behavioral and children’s health-related characteristics; types of malignancy (abdominal tumor (p=0.001)), lymphoma (p=0.040), received health information from health care professionals (p<0.001) and types of treatment (both surgery and chemotherapy) (p=0.016) had relationship with the level of resilience at p-value ≤0.25 in simple linear regression. Consequently, we used them for multiple linear regression.
Accordingly, thirteen variables were entered into multiple- linear regression. In multiple linear regression analysis, social support, stress, depression, attending recreational activities, and received health information from health care professionals were significant predictors of resilience. The model can explain 45% of the variation in parents’ children’s resilience with cancer, and the remaining other factors can explain 55%. (R Square =0.45, unadjusted R Square=0.426) of the variability in the magnified of resilience among parents of children with cancer (Table 4).
 |
Table 4 Multiple Linear Regression Analysis Predicting Parents’ Resilience at JMC, Oromia, February, 25, 2020 to April 25, 2020 (n=122) |
Keeping constant all other variables in the model, a one-unit increase in social support from friends increases the parents’ resilience by 6.6 (95% CI=(2.96, 10.37); P=0.011). The result also showed that keeping other factors constant one-unit increase health information from health care provider increases the parents’ resilience by 6.37 (95% CI=(1.754, 11), P=0.012). Similarly, a one-unit increase in attending recreational activities increases the parents’ resilience by 13.8 (95% CI (5.32, 22.37), p=0.03). However, there is a negative linear association between depression, stress, and resilience among parents of children with cancer. Keeping other factors constant one-unit increase in depression score decreases resilience of the parents by –0.827 (95% CI= (−1.634,-0.048); P=0.038). Keeping other factors constant one-unit increase in stress score decrease resilience of parents by- 0.88 (95% CI= −1.54,-0.23),P=0.031 (Table 4).
Discussion
This study assessed the magnitude of resilience and its predictors among parents of children with cancer at Jimma medical center, and it showed that the level of resilience among parents’ children with cancer was low. Support from friends attends recreational activities receiving health information from health care professionals were positively associated with resilience. At the same time, parents’ depression and stress were negatively associated with resilience.
The present study showed that the total mean and standard deviation of parents’ resilience score was 51.41 and 12.02. This finding is comparable with the result of two types of research done in China, which showed that the mean (SD) of resilience score among parents of children with cancer were similar to our study.37,38 This finding may imply that parents with cancer were in danger of developing physical and mental problems that contribute to having difficulty recovering from the traumatic situation.
The present finding was lower than the result of the research, which was done in Iran.11 In the same way, in another study in which was conducted, Iran and India also showed the same report.39,40 This difference may be due to differences in the medical service and socioeconomic status. Better medical technologies might be available in Iran and India compared to our country, leading to a better prognosis on child health status leading to low parents’ resilience.
Based on this finding, there was a statistically significant difference in mean resilience between mothers and fathers of children with cancer. The finding was supported by previous research findings done in Iran.8 This might because culturally, women are more compassionate to take of their child and acceptable by society as usual. Furthermore, this could be because mothers have more attachment with their children than their fathers.
The way people perceive social support was different in a different culture and a different society. In the Middle East and Asian countries, people fear to receive social support about childhood cancer due to fear of stigma. Studies showed that giving social support may not always be helpful; it may lead parents to have low resilience.41 However, in the present study receiving social support is a positive predictor of parent’s resilience; having a history of support from friends resulted in an increment of resilience among parents of children with cancer. This might be due to differences in culture, societal, educational level, working habits, and religion. So, understanding societal culture is crucial to finding the best ways to help and enhance parents’ resilience.
In this study, there is a negative association between parental depression and stress with resilience. This study was supported by a study conducted in Iran and China.42,43 This finding is also supported by the study conducted in Jordan, Greek, and Bangladesh.28,44,45 This implies that parents’ psychological disturbance will contribute to declining their level of resilience. Those who had no depression on parents’ children with cancer had a better level of resilience.
There is a significant positive association between receiving health information about cancer from health care professionals and resilience in the present study. Receiving health information about cancer treatment from health care professionals resulted in an increment of resilience. Providing information at an appropriate time could help avoid unnecessary distress; this helps parents to have better resilience. The finding is supported by a study conducted in Switzerland, which showed that the medical staff, especially health care providers, can most directly impact improving psychological factors that helped to decrease parental distress that helps parents have a better adaptation to the stressful situation.46
Consistent with this idea study conducted in Finland reported, lack of information about the diseases and treatment plan created distrust in health care providers and leads parents to be worried and frustrated, which contributes to low resilience.23 This indicates that parents need to have the right information about the diseases and their treatment plan, and also need to know every procedural and therapeutic information. This may be due to their prior misinformation about the disease, characteristics, or treatment, fearing the hectic hospital environment.
Similarly, attending recreational activity is one of the positive predictors for resilience. This indicates that the parent’s participation in different shared recreational activities helped develop a better positive adaptation. Parents’ having an enjoyable time can yield attachments, happiness, learning, humor, and the pleasure of shared experiences. Previous studies also support the finding.20,47
Limitation of the Study
Since our study population was small, it limits our generalizability of the findings on parents’ children with cancer and difficult to incorporate additional predictors. So, it needs a large sample size to incorporate other aspects of parents’ resilience in children with cancer. Being self-report is a limitation for this paper, which can increase social desirability bias.
Conclusion and Recommendation
In conclusion, the magnitude of resilience among parents of children with cancer was low relative to previous studies. More than half of the study participants were having a resilience score below the mean value. Receiving support from friends, attending recreational activities, and receiving health information from health care professionals are positive predictors of resilience, whereas parents’ depression and stress negatively predict resilience.
Improving regular health education and communication programs, implementing a multidisciplinary team approach, promoting social support systems, focusing on parents of children with cancer, and conducting further study with larger samples were recommended.
Abbreviations
DASS, Depression, Anxiety and Stress Scale; ETB, Ethiopian Birr; GLOBOCAN, Global Burden of Cancer; HCP, health care provider; HH, house hold; JMC, Jimma Medical Center; QOL, quality of life; SD, standard deviation; TASH, Tikur Anbessa Specialized Hospital.
Data Sharing Statement
The data supporting our findings are kept confidential and stored by the corresponding author both in hard and soft copies. If someone wants our data, we will voluntarily share it, and he/she can contact the author through the email and phone address in the corresponding author’s information.
Acknowledgments
We would like to thank Jimma medical center, pediatric oncology clinic. We are also grateful for the study participants for their willing responses and precious time, and finally, we acknowledge all those who contributed to this study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
All authors report no conflicts of interest in this work.
References
1. Magrath I, Steliarova-Foucher E, Epelman S, et al. Paediatric cancer in low-income and middle-income countries. Lancet Oncol. 2013;14(3):e104–16. doi:10.1016/S1470-2045(13)70008-1
2. WHO. Global initiative for childhood cancer: progress on all fronts; 2020. Available from: https://www.who.int/news-room/detail/14-02-2020-who-global-initiative-for-childhood-cancer-progress-on-all-fronts.
3. Gupta S, Howard SC, Hunger SP, et al.Treating childhood cancer in low-and middle-income countries. 2015.
4. Sullivan R, Kowalczyk JR, Agarwal B, et al. New policies to address the global burden of childhood cancers. Lancet Oncol. 2013;14(3):e125–e135. doi:10.1016/S1470-2045(13)70007-X
5. Ribeiro RC, Steliarova-Foucher E, Magrath I, et al. Baseline status of pediatric oncology care in ten low-income or mid-income countries receiving My Child Matters support: a descriptive study. Lancet Oncol. 2008;9(8):721–729. doi:10.1016/S1470-2045(08)70194-3
6. Neugebauer R. Handbook of International Disaster Psychology: Practices and Programs. Westport (CT): Praeger Publishers/Greenwood Publishing Group; 2006.
7. Rosenberg AR, Wolfe J, Bradford MC, et al. Resilience and psychosocial outcomes in parents of children with cancer. Pediatr Blood Cancer. 2014;61(3):552–557. doi:10.1002/pbc.24854
8. Asghari Nekah SM, Jansooz F, Kamali F, Taherinia S. The resiliency status and emotional distress in mothers of children with cancer. J Clin Psychol. 2015;7(1):15–26.
9. Rodriguez EM, Dunn MJ, Zuckerman T, Vannatta K, Gerhardt CA, Compas BE. Cancer-related sources of stress for children with cancer and their parents. J Pediatr Psychol. 2012;37(2):185–197. doi:10.1093/jpepsy/jsr054
10. Richardson GE. The metatheory of resilience and resiliency. J Clin Psychol. 2002;58(3):307–321. doi:10.1002/jclp.10020
11. Habibpour Z, Mahmoudi H, Nir MS, Areshtanab HN. Resilience and its predictors among the parents of children with cancer: a descriptive-correlational study. Indian J Palliat Care. 2019;25(1):79–83.
12. Bahri SL, Dehghan Manshadi M, Dehghan Manshadi Z. To investigate the effect of predicting resiliency and social support in general mental health in parents of deaf and blind children. Except Educ J. 2014;1(123):5–12.
13. Sinha D, Verma N, Hershe D. A comparative study of parenting styles, parental stress and resilience among parents of children having autism spectrum disorder, parents of children having specific learning disorder and parents of children not diagnosed with any psychiatric disorder. Ann Int Med Dent Res. 2019;2(4).
14. Carsten W, Michael FS, Gregory EM, Richard S, Charles SC. Adaptive self-regulation of unattainable goals: goal disengagement, goal reengagement, and subjective well-being, 2003.
15. Dibaei S, Janbozorghi M, Arefnazar M. The relation between emotional ambivalence and emotional control in mothers and anxiety in children with cancer and the modifying role of children’s sex. 2009.
16. Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med. 1998;21(6):581–599.
17. Fotiadou M, Barlow JH, Powell LA, Langton H. Optimism and psychological well-being among parents of children with cancer: an exploratory study. Psychooncology. 2008;17(4):401–409. doi:10.1002/pon.1257
18. Basher MK, Karim MR, Sultana N, Hossain KJ, Kamal MM. Parent stress in childhood cancer. Bangladesh Med J. 2012;41(1):8–13. doi:10.3329/bmj.v41i1.18773
19. Keri B, Marie L. A conceptual review of family resilience factors; 2008. Available from: https://journals.sagepub.com/doi/abs/10.1177/1074840707312237.
20. Bagley S, Salmon J, Crawford D. Family structure and children’s television viewing and physical activity. Med Sci Sports Exerc. 2006;38(5):910–918. doi:10.1249/01.mss.0000218132.68268.f4
21. Atashzadeh-Shoorideh F, Zakaryaee NS, Fani M. The barriers and facilitators in providing spiritual care for parents who have children suffering from cancer. J Fam Med Prim Care. 2018;7(6):1319–1326. doi:10.4103/jfmpc.jfmpc_76_18
22. Miller LE. Sources of uncertainty in cancer survivorship. J Cancer Surviv. 2012;6(4):431–440. doi:10.1007/s11764-012-0229-7
23. Ford K. ‘I didn’t really like it, but it sounded exciting’: admission to hospital for surgery from the perspectives of children. J Child Health Care. 2011;15(4):250–260. doi:10.1177/1367493511420185
24. Chung H, Gale J. Family functioning and self-differentiation: a cross-cultural examination. Contemp Fam Ther. 2009;31(1):19–33. doi:10.1007/s10591-008-9080-4
25. Hailu D, Adamu H, Fufa D, et al. Training pediatric hematologists/oncologists for capacity building in Ethiopia. Blood. 2019;134(Supplement_1):3423. doi:10.1182/blood-2019-121796
26. Toledano-Toledano F, Contreras-Valdez JA. Validity and reliability of the Beck Depression Inventory-II (BDI-II) in family caregivers of children with chronic diseases [Internet]. PLoS One. 2018;13.
27. Eilertsen M-E, Hjemdal O, Le TT, Diseth TH, Reinfjell T. Resilience factors play an important role in the mental health of parents when children survive acute lymphoblastic leukemia. Acta Paediatr. 2016;105(1):e30–4. doi:10.1111/apa.13232
28. Tsironi S, Koulierakis G Factors associated with parents’ levels of stress in pediatric wards; 2017. Available from: https://journals.sagepub.com/doi/full/10.1177/1367493517749327.
29. Burnette D, Duci V, Dhembo E. Psychological distress, social support, and quality of life among cancer caregivers in Albania. Psychooncology. 2016;26:
30. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. doi:10.1002/da.10113
31. Yu X, Lau JTF, Mak WWS, Zhang J, Lui WWS, Zhang J. Factor structure and psychometric properties of the Connor-Davidson Resilience Scale among Chinese adolescents. Compr Psychiatry. 2011;52(2):218–224. doi:10.1016/j.comppsych.2010.05.010
32. Singh K, Yu X. Psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) in a sample of indian students. J Psychol. 2010;1(1):23–30. doi:10.1080/09764224.2010.11885442
33. Khoshouei MS. Psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) using Iranian students. Int J Test. 2009;9(1):60–66. doi:10.1080/15305050902733471
34. Karaırmak Ö. Establishing the psychometric qualities of the Connor–Davidson Resilience Scale (CD-RISC) using exploratory and confirmatory factor analysis in a trauma survivor sample. Psychiatry Res. 2010;179(3):350–356. doi:10.1016/j.psychres.2009.09.012
35. Jung Y-E, Min J-A, Shin AY, et al. The Korean version of the Connor-Davidson Resilience Scale: an extended validation: validation of K-CD-RISC. Stress Health. 2012;28(4):319–326. doi:10.1002/smi.1436
36. Jorgensen IE, Seedat S Factor structure of the Connor-Davidson Resilience Scale in South African adolescents; 2008. Available from: http://www.degruyter.com/view/j/ijamh.2008.20.1/ijamh.2008.20.1.23/ijamh.2008.20.1.23.xml.
37. Rosenberg AR, Baker KS, Syrjala KL, Back AL, Wolfe J. Promoting resilience among parents and caregivers of children with cancer. J Palliat Med. 2013;16(6):645–652. doi:10.1089/jpm.2012.0494
38. Porter CL, Hart CH, Yang C, et al. A comparative study of child temperament and parenting in Beijing, China, and the western United States. Int J Behav Dev. 2005;29(6):541–551. doi:10.1177/01650250500147402
39. Edraki M, Rambod M. Psychological predictors of resilience in parents of insulin-dependent children and adolescents. Int J Commun Based Nurs Midwifery. 2018;6(3):239–249.
40. Anugraha MR, Romate J. Resilience and impact of children’s intellectual disability on Indian parents; 2017. Available from: http://login.research4life.org/tacsgr1journals_sagepub_com/doi/full/10.1177/1744629516654588?utm_source=summon&utm_medium=discovery-provider.
41. Johnson LA, Schreier AM, Swanson M, Moye JP, Ridner S. Stigma and quality of life in patients with advanced lung cancer. Oncol Nurs Forum. 2019;46(3):318–328.
42. Rahmani A, Azadi A, Pakpour V, Faghani S, Afsari EA. Anxiety and depression: a cross-sectional survey among parents of children with cancer. Indian J Palliat Care. 2018;24(1):82–85.
43. Ye ZJ, Guan HJ, Wu LH, Xiao MY, Luo DM, Quan XM. Resilience and psychosocial function among mainland chinese parents of children with cancer: a cross-sectional survey. Cancer Nurs. 2015;38(6):466–474. doi:10.1097/NCC.0000000000000220
44. Bashir A, Bashir U, Lone A, Ahmad Z. Challenges faced by families of autistic children. Int J Interdiscip Res Innov. 2014;2(1):64–68.
45. Qadire M, Al-Sheikh H, Suliman M, et al. Predictors of anxiety and depression among parents of children with cancer in Jordan. Psychooncology. 2018;9:27.
46. Vetsch J, Rueegg CS, Gianinazzi ME, Bergsträsser E. Information needs in parents of long-term childhood cancer survivors. Pediatr Blood Cancer. 2015;62(5):859–866. doi:10.1002/pbc.25418
47. Black K, Lobo M, Conceptual A. Review of family resilience factors. J Fam Nurs. 2008;14(1):33–55. doi:10.1177/1074840707312237
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
