Back to Journals » International Journal of Women's Health » Volume 12
Predictors of Postpartum Persisting Hypertension Among Women with Preeclampsia Admitted at Carlos Manuel de Cèspedes Teaching Hospital, Cuba
Authors Fajardo Tornes Y , Nápoles Mèndez D , Alvarez Aliaga A, Santson Ayebare D , Ssebuufu R , Byonanuwe S
Received 8 June 2020
Accepted for publication 2 September 2020
Published 6 October 2020 Volume 2020:12 Pages 765—771
DOI https://doi.org/10.2147/IJWH.S263718
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Yarine Fajardo Tornes,1,2 Danilo Nápoles Mèndez,3 Alexis Alvarez Aliaga,4 David Santson Ayebare,5 Robinson Ssebuufu,6 Simon Byonanuwe2
1Department of Obstetrics and Gynaecology, Granma University of Medical Sciences, Bayamo, Cuba; 2Department of Obstetrics and Gynaecology, Kampala International University Western Campus, Bushenyi, Uganda; 3Department of Obstetrics and Gynaecology, Santiago de Cuba University of Medical Sciences, Santiago de Cuba, Cuba; 4Department of Internal Medicine, Granma University of Medical Sciences, Bayamo, Cuba; 5Interdisciplinary Research & Development Center Limited, Mbarara, Uganda; 6Department of Surgery, Kampala International University Western Campus, Bushenyi, Uganda
Correspondence: Simon Byonanuwe
Department of Obstetrics and Gynaecology, Kampala International University Western Campus, P. O. Box 71, Bushenyi, Uganda
Tel +256 775 730088
Email [email protected]
Purpose: We established the prevalence and predictors of persisting hypertension in women with preeclampsia admitted at the Carlos Manuel de Cèspedes Teaching Hospital in Cuba so as to guide the health-care providers in early identification of the patients at risk for timely intervention.
Patients and Methods: A three-year prospective cohort study was conducted between March 2017 and March 2020. A cohort of 178 women diagnosed with preeclampsia at the hypertension unit of Carlos Manuel de Cèspedes Teaching Hospital were recruited. Interviewer administered questionnaires and laboratory and ultrasound scan result forms were used to collect the data. Binary logistic regression was conducted to determine the predictors. All data analyses were conducted using STATA version 14.2.
Results: Forty-five (27.8%) of the studied 162 patients were still hypertensive at 12 weeks postpartum. Maternal age of 35 years or more (aRR=1.14,95% CI:1.131– 4.847, p=0.022), early onset preeclampsia (before 34 weeks of gestation) (aRR=7.93, 95% CI:1.812– 34.684, p=0.006), and elevated serum creatinine levels of more than 0.8mg/dl (aRR=1.35, 95% CI:1.241– 3.606, p=0.032) were the independent predictors of persisting hypertension at 12 weeks postpartum.
Conclusion: Recognition of these predictors and close follow-up of patients with preeclampsia will improve the ability to diagnose and monitor women likely to develop persisting hypertension before its onset for timely interventions.
Keywords: persisting hypertension, preeclampsia, postpartum hypertension, pyruvate glutamic transaminase, serum creatinine
Introduction
Hypertensive disorders of pregnancy are a serious problem among patients and their attending obstetricians all over the world with associated high maternal and fetal morbidity and mortality.1 These have been classified as preeclampsia, chronic hypertension, preeclampsia superimposed on chronic hypertension, and gestational hypertension (traditionally known as pregnancy induced hypertension).2,3 Preeclampsia alone complicates about 6–8%4 of all pregnancies worldwide with increased maternal morbidity and mortality.5–8 Although in most patients the preeclampsia resolves soon after delivery, the condition heralds a higher incidence of cardiovascular disease later in life. In about 2–4%9 it persists up to beyond twelve weeks postpartum which in the context of this study is what we are referring to as persisting hypertension. This (persisting) hypertension has been noted to be a major threat to the quality of life of the women.1 A two- to four-fold increased risk of long-term hypertension has been reported in women with preeclampsia and hence a doubling of the risk of cardiovascular mortality and major adverse cardiovascular events such as stroke.7–13 Associated factors of this condition however remain obscure. Awareness of this association may lead to earlier diagnosis and improved management thus reducing associated morbidity and mortality. Also, early interventions tailored at controlling the high blood pressure during the postpartum period would result in reduction in associated morbidity and mortality resulting from this persisting hypertension.14 There is currently no any reliable information regarding predictors of progression to persisting hypertension in the postpartum period in Cuba. This study aimed to identify the predictors so as to guide the health-care providers in this setting for easy and timely identification of the women at risk for the early initiation of relevant interventions so as to minimize any associated complications.
Patients and Methods
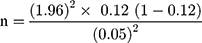
This was a prospective cohort study conducted over a period of three years in the months of March 2017 to March 2020. The study was conducted in the hypertension unit of Obstetrics and Gynaecology department of Carlos Manuel de Cèspedes Teaching Hospital located in Bayamo city, Granma Province, Southeastern Cuba. This is a public tertiary teaching hospital for the University of Medical Science of Granma with 879 bed capacity. The obstetric unit where the study was done has 234 bed capacity and conducts on average, about 5000 deliveries per year according to the hospital records of 2017 to 2019. These are admitted either as referrals from other health facilities or direct patients from their homes. A total of 178 pregnant women above 24 weeks of gestation admitted in the hypertension unit with a diagnosis of preeclampsia that consented to participate in the study were enrolled. Consecutive enrolment of all the pregnant women who met the inclusion criteria for the study was done until the required sample size was realised. Diagnosis of preeclampsia was made following the American College of Obstetricians and Gynaecologists’ protocol 2016.10 Preeclampsia was defined as the presence of hypertension of 140/90 mmHg or more15 repeated four hours apart with proteinuria of +1 or more in a previously normotensive patient above 20 weeks of gestation. Only women above 24 weeks of gestation were however included in the study since we also targeted doppler ultrasound scan results at 24 weeks of gestation. Women with preeclampsia superimposed on chronic hypertension were excluded from the study since they were already chronically hypertensive. Women with known history of kidney disease were also excluded from the study since serum creatinine was one of our study variables. This is usually deranged in patients with kidney disease. Sample size was estimated using Daniel’s formula16 as shown below;
where;
n = Desired sample size
z = Z-statistic at α= 1.96; 95% level of confidence
p =0.12%, according to a study report in neighboring Colombia17 where the prevalence of persisting hypertension was reported to be 12%.
d= Level of precision= 0.05
n =162. However, in order to account for the non-respondents or loss to follow-ups, the sample was increased by 10%; which increased the total required sample size to 178 participants.
This study was conducted in accordance with the Declaration of Helsinki. Voluntary recruitment of all the study participants was done. Informed consent from the participants was obtained after fully explaining the details of the study in Spanish, the national language for Cuba. An informed consent document in Spanish language approved by the research ethics committee of Carlos Manuel de Cèspedes Teaching Hospital was signed by every participant, the investigator and a witness. Participants were not forced to enroll if they did not want to. The participant was free to withdraw from the study at any time she wished, without coercion or compromise of care that she was entitled to. Questionnaires, laboratory and ultrasound scan request forms were used to collect the data. Blood pressure measurements were done using a manual mercury sphygmomanometer using the right hand at the level of the heart with the patient in sitting position. About six millilitres of venous blood were also withdrawn from every participant immediately after the diagnosis of preeclampsia was made and taken to the laboratory within five minutes for the different biochemical tests which included serum Pyruvate Glutamic Transaminase (PGT) and serum creatinine. A complete blood count was also done to ascertain the platelet count. These were all measured in conventional units as is documented subsequently in the tables of results. FullPIERS (Preeclampsia Integrated Estimate of Risk) test was based on gestational age (in weeks), history of chest pain or dyspnea, platelet count (x 109/l), serum creatinine (in µmol/l-specifically for this calculator), PGT (IU/l), and peripheral capillary blood oxygen saturation (sPO2) which was measured using a pulse oximeter. The values for the different parameters were fed into the standard fullPIERS calculator using a smartphone, and the result was obtained in percentage. A result of more than 5% was reported as positive while 5% and below as negative. Doppler ultrasound scan assessed the uterine-placenta blood flow to the fetus at 24 weeks of gestation. Women with increased impedance (particularly, increased resistance index or the presence of an early diastolic notch) were considered positive. Those with normal flow velocity waveforms were considered negative. Meanwhile all the enrolled participants were managed according to the hospital protocol which includes antihypertensive drugs, administration of magnesium sulfate for those with severe preeclampsia and subsequently delivery. Participants were followed up at twelve weeks post-delivery and their blood pressure measurements re-taken as already explained above so as to ascertain their blood pressure status. Those whose blood pressure was still above 140 mmHg systolic and 90 mmHg diastolic were considered to have chronic hypertension. Individuals with a systolic blood pressure lower than 140 mmHg and diastolic blood pressure lower than 90 mmHg were defined as normotensive. All the collected data were entered into Microsoft excel version 2010 and then imported into STATA version 14.2. Data analysis and presentation were carried out according to specific objectives. The prevalence of persisting hypertension was summarized as frequencies and percentages and presented in a table. The predictors of persisting hypertension were assessed using binary logistic regression. Both bivariate and multivariate logistic regression analysis were carried out. The variables in the final multivariate model were significant when p<0.05. The measure of association was reported as risk ratios with corresponding 95% confidence interval and p-value. All statistical analyses were carried out in STATA version 14.2.
Results
A total of 178 women with preeclampsia were enrolled over the period of three years. Nine patients were however excluded from the study due to superimposed preeclampsia on chronic hypertension. Four women had history of isolated renal disease (that is, had history of only renal disease without chronic hypertension) and were also excluded while three patients failed to attend the postnatal follow up at twelve weeks. Therefore, only 162 patients were successfully studied and data analyzed.
Out of a cohort of 162 participants, 45 (27.8%) had persisting hypertension at twelve weeks postpartum. Univariate analysis for the predictors of persisting hypertension showed that maternal age, early onset preeclampsia, doppler ultrasound scan of uterine arteries at 24 weeks, serum PGT and creatinine levels were significant. This is shown in Table 1. Further analysis at multivariate level revealed that maternal age of 35 years or more (aRR=1.14,95% CI:1.131–4.847, p=0.022), early onset preeclampsia (aRR=7.93, 95% CI:1.812–34.684, p=0.006), and elevated serum creatinine levels of more than 0.8 mg/dl (aRR=1.35, 95% CI:1.241–3.606, p=0.032) were the independent predictors for persisting hypertension at twelve weeks postpartum among women with preeclampsia admitted at this hospital. This is shown in Table 2.
 |
Table 1 Univariate Analysis for Predictors of Persisting Hypertension in Women with Preeclampsia at Manuel de Cèspedes Teaching Hospital |
 |
Table 2 Multivariate Analysis for Predictors of Persisting Hypertension at Manuel de Cèspedes Teaching Hospital |
Discussion
The prevalence of persisting hypertension following preeclampsia at twelve weeks postpartum in this hospital was found to be 27.8%. Although this was comparable to the one reported by Ndayambagye et al4 in Mulago hospital in Uganda, this result was higher than that reported by Fathy et al1 in Egypt, Amougou et al18 in Cameroon and Sing et al19 in the United States of America (USA). This result was also higher than the one reported by Levine et al20 of 21% in the USA, and Babah et al21 of 10.3% at the Lagos University Teaching Hospital in Nigeria, although their follow up was particularly at six weeks postpartum. Our prevalence was however lower than that reported by Nakimuli et al22 in Mulago hospital in Uganda who reported a slightly higher prevalence of 34%. We attribute these variations to contextual differences that exist among the different study populations and settings.
Pregnant women aged 35 years and more were at risk of persisting hypertension than those aged below 35 years (aRR=1.14,95% CI:1.131–4.847, p=0.022). This finding was consistent with that of Nakimuli et al22 and Ndayambagye et al4 all conducted in Uganda, Shopen et al23 in Israel as well as the one of Behrens et al24 in Denmark. Consistently also was the findings of Amougou et al18 in Cameroon where old age of more than 40 years was independently associated with progression to persistent arterial hypertension in women with preeclampsia. The association between persisting hypertension and advancing age may be explained by various proposed pathophysiologic pathways related to the age mediated reduced elastic arterial compliance and increased peripheral resistance as suggested by Rohrscheib et al25 Saini et al26 and Lardoeyt et al27 which puts them at higher risk of developing persisting hypertension. The greater frequency of persisting hypertension in women aged 35 years and more has also been recently hypothesized to result in increased release of angiogenic factors and abnormal placentation thus increasing susceptibility to severe preeclampsia and its sequelae such as persisting hypertension. Indeed, study results of Saini et al26 and Levine et al20 revealed that severe preeclampsia was an independent predictor of persisting hypertension postpartum. And the reverse is reportedly true for women with persisting hypertension.28
Women with early onset preeclampsia before 34 weeks of gestation (aRR=7.93, 95% CI:1.812–34.684, p=0.006) were found to be at high risk for having persistent hypertension at 12 weeks postpartum compared with those with late onset preeclampsia of 34 weeks of gestation and above. Previous studies such as that by Amougou et al18 Fathy et al1 and Hwang et al29 have all shown similar results. Early onset preeclampsia has been noted to take a more severe and aggressive course with more likelihood for recurrence.30,31 For example, a comparative study between early onset preeclampsia and late onset preeclampsia by Anna et al31 found that compared to the latter, the former had a higher proportion of women with severe preeclampsia, higher mean systolic and diastolic blood pressure, as well as resistant hypertension; with more frequent complications in the puerperium. As Nakimuli et al22 suggest, women with early onset preeclampsia are likely to share genetic features that give a susceptibility predisposing them to both preeclampsia and cardiovascular problems since some of the risk factors are shared. That aside, early onset preeclampsia has been noted to be more strongly associated with a wide range of internal placental factors with which their subsequent release into maternal circulation leads to endothelial dysfunction, generalized vasospasms and ultimately impaired multiple organ function. This severe endothelial dysfunction that gives rise to the generalized systemic disorder of preeclampsia may therefore lead to permanent alteration in the vasculature, thus predisposing these patients to future hypertension, as in the case of persistent hypertension, and other cardiovascular complications.22,25
High levels of serum creatinine were associated with persisting hypertension at twelve weeks postpartum among preeclampsia patients (aRR=1.35, 95% CI:1.241–3.606, p=0.032) at this hospital. This result was consistent with the one of Ndayambagye et al4 in Mulago hospital in Uganda, Saini et al in India26 as well as that by Babah et al21 in Nigeria. Because raised serum creatinine is a known marker for chronic renal disease, it is possible that the women who had elevated serum creatinine had underlying kidney injury resulting from either the preeclampsia itself, or probably were previously undiagnosed asymptomatic patients of kidney disease, which per se is an independent predictor of the development and progression of persisting hypertension and its associated morbidity and mortality.
Limitation
Although this study is the first documented to provide vital information regarding the prevalence and predictor factors of persisting hypertension following preeclampsia at this teaching hospital, we were not equipped enough and in position to do further assessment to rule out the possible confounding effects of our predictor variables such as age and elevated serum creatinine level. This study was also not in position to check for the normal physiologic alterations in the blood levels of some of our variables such as serum creatinine, Pyruvate Glutamate Transaminase and platelet number. A more detailed study to establish causal relationship of persisting hypertension in women with preeclampsia is therefore strongly recommended in the future.
Also, given the scope of our study, particularly in regard to the study design and methods, coupled by the fact that this was an institutional based study; we could not include more details of the baseline population and number of women with preeclampsia who were not recruited. This may have impacted on our overall prevalence. We believe this is an important aspect for future research in this area of the study.
Conclusion
A significant number of women with preeclampsia are candidates for future persisting hypertension and its related cardiovascular complications. Recognition of these predictors and close follow up of patients with preeclampsia will therefore go a long way towards improving the ability to diagnose and monitor women likely to develop chronic hypertension before its onset for timely interventions.
Ethical Approval
This study was approved by the Research Ethics Committee of Carlos Manuel de Cèspedes Teaching Hospital, approval number; 11 of 2016.
Acknowledgment
Goes to all our participants who consented to participate in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fathy HM, Makled AK, Sabaa HA, Yonis MA. Incidence and risk factors that predict chronic hypertension after delivery in women with hypertensive disorders of pregnancy. Egypt J Hosp Med. 2017;69:1901–1907. doi:10.12816/0040620
2. Subki AH, Algethami MR, Baabdullah WM, et al. Prevalence, Risk factors, and fetal and maternal outcomes of hypertensive disorders of pregnancy: a retrospective study in western Saudi Arabia. Oman Med J. 2018;33(5):409–415. doi:10.5001/omj.2018.75
3. Lowe SA, Bowyer L, Lust K, et al. Guideline for the management of hypertensive disorders of pregnancy. Soc Obstet Med Aust New Zeal. 2014.
4. Ndayambagye EB, Nakalembe M, Kaye DK. Factors associated with persistent hypertension after puerperium among women with pre- eclampsia/eclampsia in Mulago hospital, Uganda. BMC Pregnancy Childbirth. 2010;10(12):1–7. doi:10.1186/1471-2393-10-12
5. Begum T, Ali KS, Khanam S, et al. Clinico-demographic profiles and urinary albumin in prediction of preeclampsia among pregnant women at a tertiary care hospital. J Sci Found. 2018;16(2):54–59. doi:10.3329/jsf.v16i2.40870
6. Belay AS, Wudad T. Prevalence and associated factors of pre-eclampsia among pregnant women attending anti-natal care at Mettu Karl referal hospital, Ethiopia: cross-sectional study. Clin Hypertens. 2019;25:14.
7. Fox R, Kitt J, Leeson P, Aye CYL, Lewandowski AJ. Preeclampsia: risk factors, diagnosis, management, and the cardiovascular impact on the off spring. J Clin Med. 2019;1625(8):1–22.
8. Direkvand-moghadam A, Khosravi A, Sayehmiri K. Predictive factors for preeclampsia in pregnant women: a receiver operation character approach. Arch Med Sci. 2013;9:684. doi:10.5114/aoms.2013.36900
9. Dutta DC. DC Dutta’s Textbook of Obstetrics Including Perinatology and Contraception.
10. Cunningham FG, Leveno KJ, Bloom SL, Dashe JS, Hoffman BL, Casey BM. Williams Obstetrics.
11. Delfín M, Caballero P, Luis IJ, et al. Guía cubana de diagnóstico, evaluación y tratamiento de la hipertensión arterial * Cuban guide for hypertension diagnosis, evaluation and treatment. Rev Cubana Med. 2017;56(4):242–321.
12. Ferdinand KC, Fleg JL. Hypertension across a woman’ s life cycle. J Am Coll Cardiol. 2019;71(16):1797–1813.
13. Institute of Obstetricians and Gynaecologists. Royal college of physicians of Ireland and the clinical strategy and programmes division HSE. Clin Pract Guideline. 2019;2016:1–32.
14. Strobino D, Werner E, Mandal M. Literature review: antihypertensive medication in pregnancy an update from the 2011 WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. Jhpiego [Internet]; 2015. Available from: www.jhpiego.org/accelovate.
15. Hossain S, Roy S, Kirk K, Warren C. Hypertensive disorders in pregnancy: assessing postnatal quality of care and outcomes for women and their infants in Bangladesh. 2019.
16. Daniel WW. Biostatistics: A Foundation for Analysis in the Health Sciences. John Wiley & Sons, Inc; 2009.
17. Alonso A, Alfonso CG, Alejandro GD, Coronado-abella KLCV. Hipertensión postparto: una revisión de la literatura y los protocolos de manejo Postpartum hypertension: literature review and management protocols. Revista de la Facultad de Medicina. 2015;63(2):251–258. doi:10.15446/revfacmed.v63n2.48001
18. Amougou SN, Mbita SMM, Danwe D, Tebeu P-M. Factor associated with progression to chronic arterial hypertension in women with preeclampsia in Yaoundé, Cameroon. Pan African Med. 2019;200(33):1–7.
19. Singh GK, Siahpush M, Liu L, Allender M. Racial/ethnic, nativity, and sociodemographic disparities in maternal hypertension in the United States,2014–2015. Int J Hypertens. 2018;2018(26):1–14. doi:10.1155/2018/7897189
20. Levine L, Nkonde-Price C, Limaye M, Srinivas S. Factors associated with postpartum follow-up and persistent hypertension among women with severe preeclampsia. J Perinatol. 2017;36(12):1079–1082. doi:10.1038/jp.2016.137
21. Babah OA, Olaleye O, Afolabi BB. Postpartum sequelae of the hypertensive diseases of pregnancy: a pilot study. Niger Med J. 2018;59(1):1–6. doi:10.4103/nmj.NMJ_101_18
22. Nakimuli A, Elliott AM, Kaleebu P, Moffett A, Mirembe F. Hypertension persisting after pre-eclampsia: a prospective cohort study at Mulago Hospital, Uganda. PLoS One. 2013;8(12):1–7. doi:10.1371/journal.pone.0085273
23. Shopen N, Schiff E, Koren-morag N, Grossman E. Factors that predict the development of hypertension in women with pregnancy-induced hypertension. Am J Hypertens. 2016;29(1):141–146. doi:10.1093/ajh/hpv073
24. Behrens I, Basit S, Melbye M, et al. Risk of post-pregnancy hypertension in women with a history of hypertensive disorders of pregnancy: nationwide cohort study. BMJ. 2017;358(17):1–9.
25. Rohrscheib MR, Myers OB, Servilla KS, et al. Age-related blood pressure patterns and blood pressure variability among hemodialysis patients. Clin J Am Soc Nephrol. 2008;3(2):1407–1414. doi:10.2215/CJN.00110108
26. Saini V, Gupta M, Kumar DS, Singh H, Gupta SK. Preeclampsia: postpartum resolution of hypertension, proteinuria and serum N-terminal B-type natriuretic peptide. Indian J Med Biochem. 2019;23(2):278–286. doi:10.5005/jp-journals-10054-0104
27. Lardoeyt R, Vargas G, Lumpuy J, García R, Torres Y. Contribution of genome – environment interaction to pre-eclampsia in a Havana maternity hospital. MEDICC Rev. 2013;15(3):143–178.
28. Bilano VL, Ota E, Ganchimeg T, Mori R, Souza JP. Risk factors of pre-eclampsia/eclampsia and its adverse outcomes in low- and middle-income countries: a WHO secondary analysis. PLoS One. 2014;9(3):1–9. doi:10.1371/journal.pone.0091198
29. Hwang J, Park S, Oh S, et al. The risk factors that predict chronic hypertension after delivery in women with a history of hypertensive disorders of pregnancy. Medicine. 2015;94(42):1–6. doi:10.1097/MD.0000000000001747
30. Ukah UV, Payne B, Hutcheon JA, et al. Assessment of the fullPIERS risk prediction model in women with early-onset preeclampsia. Hypertension. 2018;71(4):659–665. doi:10.1161/HYPERTENSIONAHA.117.10318
31. Anna W, Zembala-szczerba M, Babczyk D, Kołodziejczyk-pietruszka M, Lewaczy O, Huras H. Early-and late-onset preeclampsia: a comprehensive cohort study of laboratory and clinical findings according to the new ISHHP criteria. Int J Hypertens. 2019;19(3):1–9.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.