Back to Journals » International Journal of Women's Health » Volume 12
Predictors of Postnatal Care Service Utilization Among Women of Childbearing Age in The Gambia: Analysis of Multiple Indicators Cluster Survey
Received 22 June 2020
Accepted for publication 2 September 2020
Published 9 September 2020 Volume 2020:12 Pages 709—718
DOI https://doi.org/10.2147/IJWH.S268824
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Amadou Barrow,1 Amienatta Jobe2
1Department of Public & Environmental Health, School of Medicine & Allied Health Sciences, University of the Gambia, Kanifing, The Gambia; 2Department of Obstetrics and Gynaecology, Edward Francis Small Teaching Hospital, Banjul, The Gambia
Correspondence: Amadou Barrow Tel +2203451109
Email [email protected]
Background: Despite the importance of postnatal care (PNC) in maternal and newborn health, however, such services have been underutilized in many resource-constrained settings including The Gambia. The objective of this study was to determine the coverage and factors of PNC in The Gambia.
Methods: The 2018 data from The Gambia Multiple Indicators Cluster Survey (MICS) were analyzed. Data from 9205 women with ages 15– 49 years, who also have given birth, were extracted for the analysis. Percentages and Chi-square tests were used. In addition, multivariable logistic regression model was used to calculate the adjusted odds ratios (with corresponding 95% CI). The level of significance was set at p< 0.05.
Results: The prevalence of PNC was 22.4% and 26.7% for women and children, respectively. Local government area (LGA) was associated with PNC for women and children alike. Furthermore, ethnicity was associated with PNC among women in The Gambia. Women who listened to radio almost every day had 1.51 increase in the odds of PNC (OR= 1.51; 95% CI: 1.15, 1.98) and 1.30 increase in the odds of PNC for children (OR= 1.30; 95% CI: 1.01, 1.67), respectively, when compared with women who do not listen to radio. Women who initiated antenatal care (ANC) at second or third trimester (late booking) had a 22% reduction in the odds of PNC (OR= 0.78; 95% CI: 0.64, 0.94), when compared with women who booked at first trimester.
Conclusion: The findings showed that geographical locations, ethnicity, use of radio, and timing to antenatal care initiation were associated with PNC. Women’s enlightenment and early ANC programs can be designed to improve PNC coverage.
Keywords: maternal health, post-delivery care, antenatal care, postpartum stay, skilled delivery
Background
The time frame from birth to 42 days is known as postnatal period. Majority of maternal and newborn mortality occur within this period.1 After childbirth, infection and bleeding pose a high risk to the life of mothers, similarly asphyxia, preterm birth, and infections also pose risk to the life of newborns.2 Several causes of maternal and newborn mortality are preventable due to the fact that health-care personnel provides solutions to avoid complications that are linked to pregnancy or pregnancy-related and childbirth. A great deal of the maternal and neonatal health-related issues can be completely eliminated if there is adequate uptake of PNC.2 PNC is a prominent approach recommended to reduce maternal and newborn mortality during the 42 days (6 weeks) of childbirth (postpartum period).3,4 The World Health Organization (WHO) has endorsed that mothers and their newborns should receive PNC for at least 1 day after childbirth if delivery was institution-based. However, if childbirth occurs outside health institutions, the first PNC visit should happen immediately or within 1 day of childbirth. Importantly, at least three subsequent PNC visits should follow between 7 and 14 days after delivery, and thereafter, up until the sixth week after childbirth.4 Unfortunately, the practice largely contravenes this recommendation in several Africa countries, where a good number of mothers and their newborns would not visit health facilities for PNC. By implication, there are gaps in PNC programs and other reproductive and child health programs.5
Sub-optimal PNC coverage can result in neonatal death. High neonatal mortality became a prominent bottleneck in attaining the MDGs goal-4, which poised to reduce under-five mortality by two-thirds by 2015.6 Approximately 4 million neonates (children within the first 6 weeks of life) die annually worldwide which account for about 40% of total deaths in children of 0–59 months.7,8 It is true that even in settings with poor health systems, timely prevention of neonatal deaths could still be possible. This can be done through family-community health care, and by creating demand for skilled health care, thereby bringing about improvement in healthcare-seeking behaviour among the populace. Concerted efforts towards clinical care for newborns and their mothers are essential tools that should be adopted to achieve a reduction in child mortality.3,9 Evidence-based interventions have been identified worldwide and its packages show that reduction in child mortality can be achieved.10
Effort to bring reduction to the problem of preventable mother and newborn mortality is a target for the global health community. It is based on this premise that the Sustainable Development Goals (SDGs) were adopted by the United Nations (UN) member states with a view to addressing a variety of health issues. Also, WHO has identified the first target of the third goal (SDGs-3) to reduce maternal death ratio to 70 or less deaths per 100,000 live births by 2030.6,9 The maternal death ratio globally is 216 deaths per 100,000 live births, whereas, in Africa, it is 542 deaths per 100,000 live births and in The Gambia, it is 706 deaths/100,000 live births.1 As a result of the large burden of maternal death, WHO developed a program “Global Strategy for Women’s, Children’s, and Adolescents’ Health (2016–2030)” through the “Every Woman Every Child” movement with the aim to end all preventable causes of deaths that occur among women and children.11
It has been argued that even if ANC and facility-based delivery utilization are adequately promoted, PNC should be promoted too as improvement in maternal and child health is not only hinged on ANC and facility-based delivery alone. Therefore, it is encouraged that PNC should be provided adequately to sustain the reduction in maternal and child mortality.12 There is staggering reports that up to 70% of neonatal mortalities take place in the first seven days after the childbirth and more than 50% of these deaths take place within the first 24hours of life. This points toward the fact the first 24 hours of life of a newborn are critical to survival.13,14 Unfortunately, PNC provision and utilization have been inadequate in The Gambia, regardless of the fact that it plays an important role in the reduction of maternal and newborn deaths all over the world. The inadequate provision of PNC contributes to the large childhood mortality often observed in The Gambia.15 Based on this, it is important that PNC services should be institutionalized in-country and scaled up.
PNC remains a key measure to the reduction of maternal and newborn deaths, particularly as an avenue for health-care providers to identify postpartum issues and administer timely treatment.16 Experts have argued that PNC has great potential for improving maternal and child survival if administered through the medium of health institution-based care or family-community care.17 The utilization of PNC by mothers improves both mothers’ and children’s lives.18 Despite these benefits, a huge number of women in The Gambia still do not uptake such services.19 There are many explanations by researchers on the poor utilization of PNC in many resource-constrained settings. Elsewhere, factors associated with PNC have been identified, which include; socioeconomic status, birth order, geographical region, occupation, ethnicity, number of pregnancies amongst others.18 Furthermore, exposure to mass media and proximity to health facilities have also reportedly been associated with PNC.17 However, there is a dearth of data reporting the coverage and associated factors of PNC in The Gambia. Thus, this study becomes important to explore the prevalence and examine the associated factors of PNC in The Gambia.
Methods
Data Extraction
Here, secondary data from The Gambia Multiple Indicator Cluster Survey (MICS) – 2018 were used. The data from 9205 women aged 15–49 years who have given birth were extracted for the analysis. The Gambia MICS carried out in 2018 provided the opportunity to strengthen the national statistical capacity of the country by making available technical guidance on the quality or excellence of survey information that needed to be gathered, statistical tracking as well as data gathering and data analysis. MICS ensures the measurement of key pointers which countries depend upon to generate data that are used in policy formulations and program planning to be able to monitor their progress in achieving the SDGs, as well as the National Development Plan (NDP) of The Gambia and other international commitments which the country is a signatory to. The contribution of the MICS on the strengthening of The Gambian’s improvement on data and systems monitoring and the provision of technical expertise in the design, implementation, and analysis of such systems. The major reason for the development of the MICS programme by UNICEF was to assist countries in internationally comparable data collection on an extensive variety of indicators ranging from data on children to that of women.
Variables Definitions and Measurement
Outcome Variable
The outcome variable is PNC and defined as been attended to by a trained medical professional gynaecology (either a doctor or a nurse/midwife), after childbirth lasting for a certain period of time. In this study, PNC was measured as a binary variable such that if a woman had received PNC, it was coded as 1, and if not, it was coded 0 for mothers and children alike.
Explanatory Variables
Child sex: male vs female; birth weight: underweight (<2.5kg) vs normal weight; LGA: Banjul, Basse, Brikama, Janjanbureh, Kanifing, Kerewan, Kuntaur and Mansakonko. Ethnicity: Fula, Jola, Mandinka, Sarahule, and Wollof, as well as other groups and non-Gambians, were computed. Health insurance coverage: covered vs not covered; educational level: pre-primary or none, primary, secondary+, functionality difficulty: has functional difficulty vs has no functional difficulty; the total number of children ever born: 1–2, 3–4, 5+; marital status; whether one is currently married/in the union, or was formerly married/in union and was never married/in the union; residential status: urban vs rural; age at first marriage/union: <18 years, 18–20 years, 20+ years; estimation of overall happiness: was very happy, or was somewhat happy, or was neither happy nor unhappy, or was somewhat unhappy, or was very unhappy; duration in residence: internal immigrant (lived in community <5years) vs native (lived in the community for 5+ years). The maternal age (years) was assessed by grouping the women age into seven groups from 15–19 to 45–49. The rate of listening to the radio or watching TV among was also assessed thus: do not listen to the radio or watch TV at all, listen to the radio or watch TV less than once a week, listen to the radio or watch TV at least once a week, listen to the radio or watch TV almost every day, received prenatal care was assessed by yes vs no; antenatal care visit initiation: early booking (within 1st trimester) vs late booking (after 1st trimester); place of delivery. These factors were selected as used by previous authors.20–22 the household wealth quintile of (a) poorest, (b) poorer, (c) middle, (d) richer, and (e) richest, were computed, was computed in a conventional approach from population-based data using a set of household assets.23,24
Ethical Consideration
In this study, we used datasets available in the public domain in which survey protocol was already approved by the Government of The Gambia and the Scientific Coordinating Committee (SCC) of the Medical Research Council (MRC) in March 2017. It is also on record that verbal consent was obtained from each participant of the survey. For underage children, the adult’s consent was gotten in advance of the child’s assent. All the survey respondents were intimated on the voluntariness of participation in the survey and that their confidentiality and anonymity were sacrosanct and guaranteed.
Statistical Analysis
Stata survey (“svy”) module was employed to adjust for stratification as well as for the clustering and sampling weights to compute the estimates of institutional-based delivery. The collinearity testing method was adopted in the correlation analysis to distinguish the interdependencies that exist between variables. In order to examine the multicollinearity that causes major concerns, a cut-off of 0.7 was used.25 No variable from the correlation matrix was removed in the model as a result of a lack of multicollinearity. Percentages and Chi-square test were used for univariate and bivariate analyses. All significant variables from chi-square analysis were included in the multivariable logistic regression model to calculate the adjusted odds ratios (with corresponding 95% CI) of the factors associated with institutional-based delivery. The level of significance was determined at p < 0.05. Version 14 of Stata (StataCorp., College Station, TX, USA) was used for data analysis.
Results
Based on the results, the prevalence of PNC among mothers was 22.4%, whereas among for children, it was reportedly 26.7%. See Figure 1 for the details.
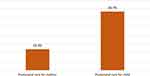 |
Figure 1 Postnatal care for mothers and children in The Gambia. |
The results showed that PNC for women and children were highest in Mansakonko with 36.9% and 41.4%, respectively, and the lowest in Kanifing with 7.3% and 13.8%, respectively. In addition, the prevalence of PNC among women and children was highest in Jola ethnic group with 29.0% and 32.8%, respectively, and lowest in minority ethnic groups with 14.6% and 23.6% among women and children, respectively. Further, women and children from the richest and richest household and rural residence reported less PNC. See Table 1 for the details.
 |  |  |
Table 1 Postnatal Care Among Women of Reproductive Age and Children Under-Five in The Gambia |

From the multivariable logistic regression model, there was a significant association between LGA and PNC for women and children alike. In addition, ethnicity was significantly associated with PNC among women of reproductive age in The Gambia. Women who listened to the radio almost every day had 1.51 increase in the odds of PNC for women (OR= 1.51; 95% CI: 1.15, 1.98), and 1.30 increase in the odds of PNC for children, respectively (OR= 1.30; 95% CI: 1.01, 1.67), when compared with women who do not listen to the radio. Furthermore, women who started ANC visits after the first trimester of their pregnancy had a 22% reduction in the odds of PNC among women (OR= 0.78; 95% CI: 0.64, 0.94) after adjusting for other confounding factors. See Table 2 for the details.
 |
Table 2 Factors That Associated with Postnatal Care in Women of Reproductive Age and Children Less Than 60 Months in The Gambia |
Discussion
In this study, we assessed the coverage of PNC and its associated factors in The Gambia. Interestingly, this has become one of the foremost studies to examine the prevalence and factors associated with PNC. Though PNC is among the most significant interventions designed to help in the reduction of maternal and child mortality, only about one-quarter of women and children in The Gambia received such services. In previous studies, sub-optimal levels of PNC were reported.21,26 The low prevalence could be explained by diverse conditions related to individual and community-level contextual factors. For example, the most recurrent reason why women do not uptake PNC was the absence of abnormal health conditions or complications in childbirth. This is followed by not been instructed to come back for PNC by their doctors, nurses or midwives.27
Several factors determined PNC utilization in The Gambia. For example, there was a significant association between PNC and timing to ANC initiation. Conventionally, one of the greatest benefits of ANC is the health education or counseling which women receive during the visits. This health education or counseling helps to promote maternal health-care utilization among women. During counseling, women are taught proper healthcare-seeking behaviours as measures to forestall preventable maternal and child mortality. It is true that women who miss out on counseling or health education during antenatal care visits will lack understanding of the importance and benefits of PNC.26 Therefore, it is not surprising for those women who had late ANC visit initiation, had a significant reduction in PNC in The Gambia. Improved antenatal care visits are reported to be interrelated with higher odds of PNC.20,28 This could explain why timing to ANC initiation was associated with PNC.
In addition, regional and ethnic differences in PNC were found to corroborate with reports from a previous study.27 It was found from this study that a significant association exists between the use of PNC and ethnic diversity. In separate studies, it was observed that significant disparities existed between racial/ethnicity and postpartum visits.29–31 The regional and ethnic differences could partly be due to the fact that certain regions or ethnic groups may have higher availability of hospital services, while some may have very low availability of hospital services.27 Consequently, this can be largely responsible for the low level of PNC, especially due to natural boundaries or separations in geographical settlements and which largely determine what health-care services are accessible to certain populace. This suggests that other factors such as regional and ethnic differences might affect PNC. There could be adverse effects of ethnic arrangement of communities on the outcomes of maternal and child health, including as PNC which can be multifaceted and occasionally difficult to comprehend.
Furthermore, we found that increased use of radio was positively associated with PNC. This is in agreement with the reports from an earlier study that revealed that mass media had a positive impact on the utilization of maternal health-care services, including; the regularity of ANC visits, nutritional supplementation of food products, physical examination, tetanus toxoid vaccination, rest and sleep.32 More so, report from a study conducted among Ugandan women revealed that access to media among the studied women increased their likelihood of using maternal health-care services, when compared to their counterparts with no access to media.33 The frequency of listening to radio messages was directly proportional to PNC. As expected, respondents with a higher frequency of listening to the radio were found to possess more information and uses PNC with its recommendation, when compared with their counterparts with the low frequency of listening to the radio. Individuals who had better information are more empowered for PNC uptake. These findings were in agreement with results from previous findings.28,33–35 If information about health-care services will get to the grassroots, the government must enact policies that will aid the media services to be at the forefront. Outright removal of or drastic reduction of tax for small radio suppliers, by the government, may aid in making these items available to both the rural dwellers and the urban poor. It is also important that policy follow-up is designed to ensure that insightful information on healthcare are always disseminated to the public. If many people have access to the right information about health-care services, the will be a reduction in the needless deaths that occur as a result of inappropriate healthcare decision-making. Therefore, having uncensored access to dependable health-care information is a foundation to enhanced and justifiable health outcomes.
Strength and Limitation
This is one of the foremost studies to be conducted using a nationally representative sample in the Gambia to examine and explore the prevalence and determining factors of PNC service utilization. However, as the study is based on a secondary dataset, the researcher has limited control over the type of data available. Moreover, the specific PNC services utilized by women and children were not captured. Furthermore, only association and not causality has been established in this study.
Conclusion
The findings of this present study showed a low prevalence of PNC coverage. In addition, the study identified geographical location, ethnicity, radio/media use, and timing to antenatal care booking as factors associated with PNC in The Gambia. Based on these findings, it is recommended that further studies can be conducted to explore the reasons for use or non-use of PNC services. Programmes to improve women’s timing to antenatal care initiation, media use, and behaviour change communication should be designed and implemented.
Disclosure
The authors report no conflicts of interest for this work.
References
1. World Health Organization, UNICEF, United Nations, Department of Economic and Social Affairs, Population Division, World Bank. Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division [Internet]. 2015 Available from: http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/.
2. WHO. Postpartum care of the mother and newborn: a practical guide. Technical Working Group, World Health Organization. Birth. 1999;26(4):255–258. doi:10.1046/j.1523-536x.1999.00255.x
3. Darmstadt GL, Bhutta ZA, Cousens S, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365(9463):977–988. doi:10.1016/S0140-6736(05)71088-6
4. World Health Organization, Department of Maternal N Child and Adolescent Health. WHO recommendations on postnatal care of the mother and newborn [Internet]. 2013Available from: http://www.ncbi.nlm.nih.gov/books/NBK190086/.
5. World Health Organization. World health statistics 2018: monitoring health for the SDGs [Internet]. 2018 Available from: http://apps.who.int/iris/bitstream/handle/10665/272596/9789241565585-eng.pdf?ua=1.
6. Kumar S, Kumar N, Vivekadhish S. Millennium Development Goals (MDGs) to Sustainable Development Goals (SDGs): addressing Unfinished Agenda and Strengthening Sustainable Development and Partnership. Indian J Community Med. 2016;41(1):1. doi:10.4103/0970-0218.170955
7. Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361(9376):2226–2234. doi:10.1016/S0140-6736(03)13779-8
8. Lawn JE, Cousens S, Zupan J. Lancet Neonatal Survival Steering Team 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891–900. doi:10.1016/S0140-6736(05)71048-5
9. Rosa W. Transforming Our World: the 2030 Agenda for Sustainable Development. In: A New Era in Global Health [Internet]. New York, NY: Springer Publishing Company; 2017. Available from http://connect.springerpub.com/lookup/doi/10.1891/9780826190123.ap02.
10. Haws RA, Thomas AL, Bhutta ZA, Darmstadt GL. Impact of packaged interventions on neonatal health: a review of the evidence. Health Policy Plan. 2007;22(4):193–215. doi:10.1093/heapol/czm009
11. World Health Organization. Every Woman Every Child. Global Strategy for Women’s, Children’s and Adolescents’ Health, 2016–2030. [Internet]. 2015. Available from: https://www.who.int/life-course/partners/global-strategy/ewec-globalstrategyreport-200915.pdf?ua.
12. Singh A, Yadav A, Singh A. Utilization of postnatal care for newborns and its association with neonatal mortality in India: an analytical appraisal. BMC Pregnancy Childbirth. 2012;Dec;12(1):33.
13. Guillot M, Gerland P, Pelletier F, Saabneh A. Child Mortality Estimation: A Global Overview of Infant and Child Mortality Age Patterns in Light of New Empirical Data. Byass P, editor. PLoS Med. 2012;9(8):e1001299. doi:10.1371/journal.pmed.1001299
14. Liu L, Johnson HL, Cousens S, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–2161. doi:10.1016/S0140-6736(12)60560-1
15. Rerimoi AJ, Jasseh M, Agbla SC, Reniers G, Roca A, Timæus IM. Under-five mortality in The Gambia: comparison of the results of the first demographic and health survey with those from existing inquiries. PLoS One. 2019;14(7):e0219919. doi:10.1371/journal.pone.0219919
16. Titaley CR, Hunter CL, Heywood P, Dibley MJ. Why don’t some women attend antenatal and postnatal care services?: a qualitative study of community members’ perspectives in Garut, Sukabumi and Ciamis districts of West Java Province, Indonesia. BMC Pregnancy Childbirth. 2010;10(1):61. doi:10.1186/1471-2393-10-61
17. Titaley CR, Dibley MJ, Roberts CL. Factors associated with non-utilisation of postnatal care services in Indonesia. J Epidemiol Community Health. 2009;63(10):827–831. doi:10.1136/jech.2008.081604
18. Dhakal S, Chapman GN, Simkhada PP, van Teijlingen ER, Stephens J, Raja AE. Utilisation of postnatal care among rural women in Nepal. BMC Pregnancy Childbirth. 2007;7(1):19. doi:10.1186/1471-2393-7-19
19. The Gambia Bureau of Statistics (GBOS) and ICF International. The Gambia Demographic and Health Survey 2013. Banjul, The Gambia, and Rockville, Maryland, USA: GBOS and ICF International. [Internet]; 2014. Available from: https://dhsprogram.com/pubs/pdf/FR289/FR289.pdf.
20. Abuka Abebo T, Jember Tesfaye D. Postnatal care utilization and associated factors among women of reproductive age Group in Halaba Kulito Town, Southern Ethiopia. Arch Public Health. 2018;76(1):9. doi:10.1186/s13690-018-0256-6
21. Ononokpono DN, Odimegwu CO, Imasiku ENS, Adedini SA. Does it Really Matter Where Women Live? A Multilevel Analysis of the Determinants of Postnatal Care in Nigeria. Matern Child Health J. 2014;18(4):950–959. doi:10.1007/s10995-013-1323-9
22. Wudineh KG, Nigusie AA, Gesese SS, Tesu AA, Beyene FY. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: a community- based cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):508. doi:10.1186/s12884-018-2138-x
23. Hruschka DJ, Gerkey D, Hadley C. Estimating the absolute wealth of households. Bull World Health Organ. 2015;93(7):483–490. doi:10.2471/BLT.14.147082
24. Rutstein SO, Staveteig S. Making the Demographic and Health Surveys Wealth Index Comparable. 2014;43.
25. Midi H, Sarkar SK, Rana S. Collinearity diagnostics of binary logistic regression model. J Interdisciplinary Mathematics. 2010;13(3):253–267. doi:10.1080/09720502.2010.10700699
26. Limenih MA, Endale ZM, Dachew BA. Postnatal Care Service Utilization and Associated Factors among Women Who Gave Birth in the Last 12 Months prior to the Study in Debre Markos Town, Northwestern Ethiopia: A Community-Based Cross-Sectional Study. Int J Rep Med. 2016;2016:1–7. doi:10.1155/2016/7095352
27. Dhaher E, Mikolajczyk RT, Maxwell AE, Krämer A. Factors associated with lack of postnatal care among Palestinian women: A cross-sectional study of three clinics in the West Bank. BMC Pregnancy Childbirth. 2008;8(1):26. doi:10.1186/1471-2393-8-26
28. Bwalya BB, Mulenga MC, Mulenga JN. Factors associated with postnatal care for newborns in Zambia: analysis of the 2013-14 Zambia demographic and health survey. BMC Pregnancy Childbirth. 2017;13:17.
29. Thiel de Bocanegra H, Braughton M, Bradsberry M, Howell M, Logan J, Schwarz EB. Racial and ethnic disparities in postpartum care and contraception in California’s Medicaid program. Am J Obstet Gynecol. 2017;217(1):
30. Kozhimannil KB, Trinacty CM, Busch AB, Huskamp HA, Adams AS. Racial and Ethnic Disparities in Postpartum Depression Care Among Low-Income Women. Psychiatr Serv. 2011;62(6):619–625. doi:10.1176/ps.62.6.pss6206_0619
31. Henderson J, Gao H, Redshaw M. Experiencing maternity care: the care received and perceptions of women from different ethnic groups. BMC Pregnancy Childbirth. 2013;13(1):196. doi:10.1186/1471-2393-13-196
32. Acharya D, Khanal V, Singh JK, Adhikari M, Gautam S. Impact of mass media on the utilization of antenatal care services among women of rural community in Nepal. BMC Res Notes. 2015;12:8.
33. Edward B. Factors influencing the utilisation of antenatal care content in Uganda. Australas Med J. 2011;4(9):516–526. doi:10.4066/AMJ.2011.849
34. Matsumura M, Gubhaju BB. Women’s status, household structure and the utilization of maternal health services in Nepal. Asia Pacific Population J. 2001;16(1):23–44. doi:10.18356/e8a4c9ed-en
35. Zamawe COF, Banda M, Dube AN. The impact of a community driven mass media campaign on the utilisation of maternal health care services in rural Malawi. BMC Pregnancy Childbirth. 2016;16(1):21. doi:10.1186/s12884-016-0816-0
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
