Back to Journals » Journal of Pain Research » Volume 13
Predictors of Opioid Prescription Among a Sample of Patients with Acute Musculoskeletal Pain at a Tertiary Care Hospital in Saudi Arabia
Authors AlRuthia Y , Alhazzani H , Alhindi G, Alarfaj M, Almutairi L, Alanazi M, Alokili K, Alanazi N , Alodaibi F , Alwhaibi M , Bashatah AS , Asiri Y, Alsanawi H
Received 11 August 2020
Accepted for publication 21 October 2020
Published 16 November 2020 Volume 2020:13 Pages 2929—2936
DOI https://doi.org/10.2147/JPR.S276630
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Yazed AlRuthia,1,2 Hawazin Alhazzani,1 Ghaida Alhindi,1 Maryam Alarfaj,1 Lama Almutairi,3 Miteb Alanazi,4 Khaulah Alokili,1 Nouf Alanazi,1 Faris Alodaibi,5 Monira Alwhaibi,1 Adel S Bashatah,6 Yousif Asiri,1 Hisham Alsanawi7
1Department of Clinical Pharmacy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia; 2Pharmacoeconomics Research Unit, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia; 3Department of Pharmacy, King Abdulaziz University Hospital, Riyadh, Saudi Arabia; 4Department of Pharmacy, King Khalid University Hospital, Riyadh, Saudi Arabia; 5Department of Rehabilitation Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia; 6Department of Nursing Education and Administration, College of Nursing, King Saud University, Riyadh, Saudi Arabia; 7Department of Orthopedic Surgery, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Correspondence: Yazed AlRuthia
Department of Clinical Pharmacy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia
Tel +996 114677483
Fax +966 114677480
Email [email protected]
Background: Musculoskeletal pain is one of the most complex and debilitating types of pain. Although different pharmacologic treatments are available, very few studies have explored the predictors for opioid analgesics prescription to manage this type of pain.
Objective: The aim of this study was to explore the predictors for opioid prescription in patients with acute musculoskeletal pain in Saudi Arabia.
Methods: This was a single-center, retrospective chart review of adult patients (≥ 18 yrs.) with an acute nociceptive musculoskeletal pain at a university-affiliated medical center in Riyadh, Saudi Arabia. Cancer patients and those with chronic neuropathic pain were excluded. Patients’ age, gender, number of comorbidities, duration of pain management, number of clinic visits for pain, and Numeric Pain Rating Scale (NPRS) scores at rest and with normal activities were collected. Multiple logistic regression was conducted to examine the relationship between the type of musculoskeletal pain and the prescription of opioid analgesics controlling for NPRS score on activity, age, gender, number of comorbidities, duration of pain treatment, and number of clinic visits for pain.
Results: The mean age of the 227 patients, who met the inclusion criteria, was 39 years and 68% of them were male. Sixty-three percent of the patients were prescribed opioid analgesics, and 61% of them had shoulder pain, 29% had back pain, and 10% had lower extremity pain (eg, hip, thigh, lower leg, knee, ankle, and foot pain). Tramadol was the most commonly prescribed opioid analgesic (82%), followed by codeine (13%). Ninety-seven percent of patients who were prescribed non-opioid analgesics had shoulder pain. Patients with shoulder pain had lower odds of receiving opioid analgesics (OR=0.019, P< 0.0001, 95% CI=0.004– 0.081) in comparison to their counterparts who had lower extremity or back pains. Moreover, the higher the pain score on activity was, the higher odds of receiving opioid analgesics (OR=1.317, P< 0.0001, 95% CI=1.029– 1.685).
Conclusion: Future studies should explore the impact of different opioid prescribing policies to improve the quality of patient care and reduce the unnecessary prescribing of opioids for patients with non-cancer musculoskeletal pain.
Keywords: analgesics, opioid, musculoskeletal pain, shoulder pain, Saudi Arabia
Introduction
Musculoskeletal disorders include more than 150 diagnoses affecting muscles, bones, joints and associated tissues, such as tendons and ligaments, as stated in the International Classification of Diseases.1 These conditions can occur anytime during people’s lifetime resulting in persistent pain that negatively impact their quality of life. Musculoskeletal pain is one of the most commonly encountered pain in healthcare settings, and is considered the largest cause of disability in many countries, such as the United Kingdom.2–4 It was found to be one of the three major causes of the global burden of non-communicable diseases in 2016 representing about 16% of all disability adjusted life-years (DALYs).5 Moreover, it was reported that musculoskeletal pain and disorders account for 22.6% of the total costs of illnesses in Sweden.6 In the United Kingdom, the cost of opioid prescriptions for musculoskeletal pain management varied from £3 to £4,844 per patient per year, and the cost of opioid overprescription could exceed £100 million per year assuming that 40% of patients with musculoskeletal pain are overprescribed.2 The cost of managing musculoskeletal pain is not limited to the cost of prescriptions or clinic visits; the productivity loss and absenteeism due to musculoskeletal pain is also significant.7 In Saudi Arabia, few research studies have explored the prevalence of musculoskeletal pain among the public. In a questionnaire-based study that explored the prevalence of musculoskeletal pain among 165 construction workers in the cities of Riyadh and Dammam, 48.5% of the respondents reported having musculoskeletal pain, such as low back and knee pain.8 Musculoskeletal pain was found to be also prevalent among medical professionals. In a study that explored the prevalence of musculoskeletal pain among medical and surgical residents at a tertiary care center in Riyadh, the majority of the respondents (82.5%) reported suffering from musculoskeletal pain at least once during their medical training, and the low back pain was the most prevalent (53%).9 Low back pain is also prevalent among dental practitioners according to multiple studies that explored the prevalence of musculoskeletal pain among dentists in the Kingdom.10–12
Although multiple non-pharmacologic treatments, such as physiotherapy and acupuncture, are used in the management of musculoskeletal pain, pharmacotherapy (eg, nonsteroidal anti-inflammatory drugs (NSAIDs), selective COX-2 inhibitors, oral and injectable corticosteroids, and opioids) remains the mainstay of musculoskeletal pain treatment.13 Opioids are the most commonly prescribed analgesics used in the management of acute musculoskeletal pain.2 Nearly 90% of patients who visit pain clinics in the United Kingdom are prescribed some forms of opioid analgesics.2 Although opioids are deemed to be the most effective analgesics in the management of acute musculoskeletal pain, their use is associated with higher risk of abuse, misuse, and serious adverse events.14 Therefore, the lowest effective dose of opioids should be used for the shortest appropriate period of time whenever needed in the management of musculoskeletal pain.15 Additionally, it was found that the early use of opioids in the management of both acute and chronic musculoskeletal pain has been associated poorer clinical outcomes especially in the case of low back pain according to a recently published systematic review of clinical practice guidelines.16 However, another systematic review and meta-analysis has found that the use of opioids in the management of low back pain is associated with greater pain relief in the short term, but this effect was not observed in the long term.17
There has been an upward trend in the opioids prescribing rate for both acute and chronic musculoskeletal pain globally over the last two decades particularly in the United States.18,19 It is believed the rate of opioids prescription for patients with musculoskeletal pain has seen a 50% increase between the years of 2001 and 2010.18 This was accompanied with a significant increase in the rates of opioid-related death.20 Unfortunately, research studies aimed at exploring the rates of opioids consumption are scarce in the Middle East.21 Although the rates of opioids utilization in the management of pain states have significantly increased in the world over the last two decades, some Middle Eastern countries have seen either a modest increase or a decrease in the rates of opioids utilization.21,22 This could be attributed to several reasons, such as poor palliative care services, lack of essential opioid stock, and strict regulations.22 Although no study has explored the pain management adequacy among patients with musculoskeletal disorders in Saudi Arabia, many believe that there is an underutilization of analgesics in general, and opioids in particular, in the management of musculoskeletal pain.22 This assumption is mainly based on the findings of previously published studies that assessed the pain management adequacy among patients with more severe disease states, such as cancer and cardiac surgery.23,24 Moreover, very few tertiary care hospitals in Saudi Arabia have pain management clinics, and those with such clinics require special forms to be filled for any opioid prescriptions by a medical specialist or consultant only. These regulations besides the local drug enforcement laws that require a narcotic pharmacist to be in charge of auditing all narcotic prescriptions in each public or private hospital as well as the fact that those who engage in any prescription drug diversion can be sentenced to death could explain the reason behind the underutilization of opioid analgesics in Saudi Arabia.22,25 Understanding the predictors for opioids prescription should help in formulating a safe and effective opioid prescribing protocol for patients with musculoskeletal pain.
Therefore, the aim of this study was to explore the predictors for opioids prescription among a sample of patients with acute musculoskeletal pain in Saudi Arabia.
Methods
Study Design, Setting, and Subjects
This was a single-center, retrospective medical chart review study that was conducted at King Khalid University hospital, which is a university-affiliated hospital in Riyadh, Saudi Arabia. The hospital’s bed capacity is 1,200 beds, and it provides primary, secondary, and tertiary health services to university faculty and their families as well as to Saudi citizens on a referral basis. Although the hospital has recently established pain clinics for patients with chronic pain, patients with acute pain are treated with opioid or non-opioid analgesics based on physicians’ discretion. Furthermore, there are no published pain management guidelines for physicians to follow or adhere to. However, only licensed medical specialists or consultants can prescribe opioids for legitimate medical indications.
Adult patients (≥18 years old) with an acute nociceptive musculoskeletal pain who have been seen in the orthopedic outpatient clinics were identified via the hospital electronic health record (EHR) system (eg, Cerner Millennium). Patients with cancer, neuropathic pain, prior use of opioids or substance abuse history, osteoarthritis, and those with other pain disorders that necessitate long-term pain management (eg, inflammatory bowel disease, fibromyalgia, post-trauma or post-surgical pain) were excluded. Systematic random sampling was used by choosing every 100th patient health record of all patients who were prescribed opioid and/or non-opioid analgesics for acute musculoskeletal pain between May 2015 and December 2017. Patients’ age, gender, body mass index (BMI), number of clinic visits, pain location, number of comorbidities, number of prescription medications, duration of pain treatment which was written in the prescriptions for the different dispensed analgesics, and the Numeric Pain Rating Scale (NPRS) scores at rest and with normal activities were collected for both cases (patients on opioid analgesics) and controls (patients on non-opioid analgesics). The NPRS is an 11-point verbal scale which has been validated to assess the pain intensity across multiple patient populations and in different healthcare settings.26 The study was approved by the institutional review board of King Saud University College of Medicine (Research Project No. E-17-2587). No patient consent form was required per the institutional policy since the study was a retrospective chart review, and no personal identifiers were collected. Furthermore, the study adhered to the ethical principles of the declaration Helsinki with regard to data storage and handling.27
Statistical Analysis
Descriptive statistics using means, standard deviations, frequencies, and percentages were used to describe the patient characteristics. The baseline characteristics for the cases (patients on opioid analgesics) and controls (patients on non-opioid analgesics) were compared using Chi-square test, Fisher’s exact test, and Student’s t-test as appropriate. The pain location was dichotomized into shoulder pain versus the other types of pain. Multiple logistic regression analysis to identify the predictors for opioids prescription was conducted and included the following variables: age, gender, NPRS score on activity, number of comorbidities, number of clinic visits, duration of pain treatment, and pain location.28 The minimum sample size for multiple logistic regression that included seven predictor variables for opioids prescription with at least 10 events (cases on opioids) per variable matched to controls (patients with musculoskeletal pain on non-opioid analgesics) based on a 1:1 ratio was estimated to be 140 patients.29 All statistical analyses were conducted using SAS® version 9.4 (SAS institute, Cary, NC, USA).
Results
Out of 1,651 randomly selected patients who received prescription analgesics between May 2015 and December 2017, 227 patients met the inclusion criteria and were included in the study. Approximately 64% of the patients with acute musculoskeletal pain were prescribed opioid analgesics. The mean age of the patients was 39 years with no significant difference between the cases (patients on opioid analgesics) and controls (patients on non-opioid analgesics). Most of the patients were male (68.28%) with no significant difference in the percentages of males or females between the two groups. Most of the sampled patients had shoulder pain (60.79%), followed by back pain (29.07%), and lower extremity pain (eg, hip, thigh, lower leg, knee, ankle, and foot pain) (10.13%). The majority of the patients with shoulder pain (97.56%) were prescribed non-opioid analgesics (eg, nonsteroidal anti-inflammatory drugs, celecoxib, and acetaminophen), whereas only two patients with back pain and none of the patients with lower extremity pain were prescribed non-opioid analgesics (P<0.0001). Approximately 21% of the patients who were prescribed opioid analgesics had more than one comorbidity, and 17.24% were taking more than two prescription medications in comparison to 3.66% and 4.88%, respectively, among their counterparts who were prescribed non-opioid analgesics (P<0.05). The mean number of clinic visits for the patients was 1.72 visits with no significant difference between the two groups. Pain treatment mean duration was significantly higher among patients treated with opioid analgesics in comparison to their counterparts on non-opioid analgesics (19.14 days versus 10.44 days, P<0.0001). The mean NPRS scores with activity for patients who were prescribed opioid analgesics was slightly but significantly higher than their counterparts who were prescribed non-opioid analgesics (3.73 versus 3.06, P=0.0012). On the other hand, the mean NPRS scores at rest were not significantly different between the two groups. NO significant difference between the NPRS scores with activity and rest for the different pain locations (eg, lower limb, shoulder, and back pain) was found. The baseline characteristics of the patients are shown in Table 1. There were 158 opioid prescriptions dispensed for 145 patients who received opioid analgesics, and tramadol was the most commonly prescribed opioid (82.27%), followed by codeine (12.66%), morphine (2.53%), and fentanyl (2.53%) as shown in Figure 1. Patients with shoulder pain had 98.1% lower odds of receiving opioid analgesics in comparison to their counterparts with back or lower extremity pain (OR=0.019, 95% CI= 0.004–0.081, P<0.0001) controlling for age, NPRS score with activity, gender, number of comorbidities, duration of pain treatment, and number of clinic visits. On the other hand, patients with lower limb or back pain had more than 50 times higher odds of receiving opioid analgesics in comparison to their counterparts with shoulder pain (OR=53.59, 95% CI= 12.34–232.74, P<0.0001) controlling for age, NPRS score with activity, gender, number of comorbidities, duration of pain treatment, and number of clinic visits. Moreover, every additional point in the NPRS score with activity was associated with 31.7% increase in the odds of receiving opioid analgesics (OR=1.317, 95% CI= 1.029–1.685, P=0.0285) controlling for pain location, age, gender, number of comorbidities, duration of pain treatment, and number of clinic visits. The results of the multiple logistic regression analysis are shown in Table 2.
 |
Table 1 Patients’ Baseline Characteristics |
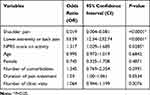 |
Table 2 The Odds of Opioids Prescription Among Patients with Musculoskeletal Pain |
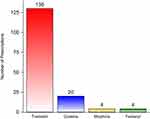 |
Figure 1 The type and number of opioid analgesic prescriptions for 145 patients. |
Discussion
The utilization of opioids in the management of chronic and acute pain has significantly increased worldwide especially in the western countries, such as the United States, where it largely contributed to the current opioid epidemic.18–20 However, there is a lack of studies that explored the predictors for opioids prescription in the management of musculoskeletal pain in the Middle East where the medical practice and the regulations that govern the prescription of opioids are starkly different.21,22 Thus, the findings of this study shed light on the prescribing pattern of opioid analgesics in the management of acute musculoskeletal pain, which is largely unknown in Saudi Arabia. Contrary to what was expected, opioids are not infrequently prescribed in the management of acute pain among the patients in the study. The vast majority of patients seen in the outpatient orthopedic clinics for acute back and lower extremity pain were prescribed opioid analgesics. Patients with lower extremity and back pain have more than 50 times higher odds of receiving opioid analgesics in comparison to their counterparts with shoulder pain despite controlling for a multitude of factors that are known to influence opioids prescription.28 The high utilization rates of opioids in the management of lower extremity and back pain observed in this study are consistent with the reported high opioids utilization rates in the literature.18–20,30 The use of opioids in the management of acute back and lower extremity pain for short term (eg, <90 days) result in greater pain relief according to a moderate level of evidence.17 However, the results of recently published systematic reviews are against the use of opioids for acute and chronic musculoskeletal pain conditions.16 Moreover, the use of opioids in the management of acute and chronic low back pain have not shown to be superior when compared to other non-opioid analgesics.31
On the other hand, shoulder pain was associated with significantly lower odds of opioid prescription. The reasons behind that can be attributable to the increasing evidence that discourage the use of opioids in the management of shoulder pain.32,33 In a retrospective cohort study that examined the impact of opioids use on clinical outcomes among patients who underwent arthroscopic rotator cuff repair, patients who were treated with opioids pre-operatively did not reach the same level of functionality and required higher dosages of opioids post-operatively.33 Additionally, patients with upper extremity pain are believed to require shorter period of opioids treatment in comparison to patients with other types of musculoskeletal pain.34 However, the use of opioids in the management of other types of musculoskeletal pain, such as back pain, is not encouraged either.31 Therefore, it is unclear why patients with back or lower extremity pain were more likely to be treated with opioid analgesics in comparison to their counterparts with shoulder pain despite the fact that the pain severity, as measured by the NPRS, was controlled for. This can be partly explained by the fact that physicians have different beliefs about the consequences of their prescribing decisions, emotionally charged physician–patient interactions, and patients’ and physicians’ characteristics, and preferences.35,36 The severity of pain, as measured by the NPRS, was positively associated with opioids prescribing, which is consistent with the preponderance of evidence.28 However, female gender, age, duration of pain treatment, and number of clinic visits were not associated with opioid prescribing among the sample of patients in this study as shown in the adjusted odds ratios. On another note, tramadol was the most commonly prescribed opioid analgesics. This can be due to the beliefs among some physicians that tramadol is a safe and “opioid-lite”.37 However, the use of tramadol for acute pain is associated with high risk of misuse, adverse effects, and chronic use after an acute pain episode.38
Although this is the first study to the best of our knowledge that explored the predictors for opioids prescribing in Saudi Arabia, it has multiple limitations that must be acknowledged. First, this was a retrospective chart review study that is fraught with information bias, such as documentation and recall bias.39 In addition, this was a single-center study with limited generalizability.40 Furthermore, important variables, such as patient education level, prescribers’ characteristics (eg, education, years of experience, previous history of prescribing opioids), patient satisfaction with care, and patients’ perceptions about the adequacy of pain management, have not been collected and were not controlled for.28 Moreover, not all patients with acute musculoskeletal pain were included in this study although systematic random sampling was used. Despite all of the above-mentioned limitations, this study highlights the gaps in knowledge about opioids prescribing for acute musculoskeletal pain in Saudi Arabia. Although it is largely believed that pain management is inadequate for some patient populations, such as cancer, this might not be the case for patients with acute musculoskeletal pain.24 Future studies should examine the appropriateness and predictors of opioids prescribing in Saudi Arabia for patients with acute and chronic pain at a national level in order to formulate a national policy for opioids prescribing that ensures safe and effective management of pain.
Abbreviations
NPRS, Numeric Pain Rating Scale; DALYs, disability adjusted life-years; EHR, electronic health record.
Data Sharing Statement
Study data are available from the corresponding author (Yazed AlRuthia) upon request.
Acknowledgment
The authors acknowledge financial support from Researchers Supporting Project number (RSP-2020/16), King Saud University, Riyadh, Saudi Arabia.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Musculoskeletal conditions. Available from: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions.
2. Ashaye T, Hounsome N, Carnes D, et al. Opioid prescribing for chronic musculoskeletal pain in UK primary care: results from a cohort analysis of the COPERS trial. BMJ Open. 2018;8(6).
3. Schnitzer TJ. Update on guidelines for the treatment of chronic musculoskeletal pain. Clin Rheumatol. 2006;25(1):22–29. doi:10.1007/s10067-006-0203-8
4. Woolf AD, Akesson K. Understanding the burden of musculoskeletal conditions. BMJ. 2001;322:1079–1080. doi:10.1136/bmj.322.7294.1079
5. Hay SI, Abajobir AA, Abate KH, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1260–1344.
6. Jacobson L, Lindgren B. Vad Kostar Sjukdomarna? [What are the Costs of Illness?]. Stockholm: Socialstyrelsen (National Board of Health and Welfare); 1996.
7. Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol. 2004;14(1):13–23. doi:10.1016/j.jelekin.2003.09.015
8. Alghadir A, Anwer S. Prevalence of musculoskeletal pain in construction workers in Saudi Arabia. Sci World J. 2015;2015:529873. doi:10.1155/2015/529873
9. Alsultan A, Alahmed S, Alzahrani A, et al. Comparison of musculoskeletal pain prevalence between medical and surgical specialty residents in a major hospital in Riyadh, Saudi Arabia. J Musculoskelet Surg Res. 2018;2(4):161–166. doi:10.4103/jmsr.jmsr_36_18
10. Meisha DE, Alsharqawi NS, Samarah AA, et al. Prevalence of work-related musculoskeletal disorders and ergonomic practice among dentists in Jeddah, Saudi Arabia. Clin Cosmet Investig Dent. 2019;11:171–179. doi:10.2147/CCIDE.S204433
11. Al-Mohrej OA, AlShaalan NS, Al-Bani WM, et al. Prevalence of musculoskeletal pain of the neck, upper extremities and lower back among dental practitioners working in Riyadh, Saudi Arabia: a cross-sectional study. BMJ Open. 2016;6(6):e011100. doi:10.1136/bmjopen-2016-011100
12. Aljanakh M, Shaikh S, Siddiqui AA, et al. Prevalence of musculoskeletal disorders among dentists in the Hail Region of Saudi Arabia. Ann Saudi Med. 2015;35(6):456–461.
13. Babatunde OO, Jordan JL, Van der Windt DA, et al. Effective treatment options for musculoskeletal pain in primary care: a systematic overview of current evidence. PLoS One. 2017;12(6):e0178621.
14. Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4):569–576. doi:10.1097/01.j.pain.0000460357.01998.f1
15. Hsu JR, Mir H, Wally MK, Seymour RB. Orthopaedic trauma association musculoskeletal pain task force. Clinical practice guidelines for pain management in acute musculoskeletal injury. J Orthop Trauma. 2019;33(5):e158–e182.
16. Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79–86. doi:10.1136/bjsports-2018-099878
17. Shaheed CA, Maher CG, Williams KA, et al. Efficacy, tolerability, and dose-dependent effects of opioid analgesics for low back pain: a systematic review and meta-analysis. JAMA Intern Med. 2016;176(7):958–968. doi:10.1001/jamainternmed.2016.1251
18. Larochelle MR, Zhang F, Ross‐Degnan D, et al. Trends in opioid prescribing and co‐prescribing of sedative hypnotics for acute and chronic musculoskeletal pain: 2001–2010. Pharmacoepidemiol Drug Saf. 2015;24(8):885–892. doi:10.1002/pds.3776
19. Bedson J, Chen Y, Hayward RA, et al. Trends in long-term opioid prescribing in primary care patients with musculoskeletal conditions: an observational database study. Pain. 2016;157(7):1525–1531. doi:10.1097/j.pain.0000000000000557
20. Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The global burden of musculoskeletal pain-where to from here? Am J Public Health. 2019;109(1):35–40. doi:10.2105/AJPH.2018.304747
21. Wilby KJ, Wilbur K. Cross-national analysis of estimated narcotic utilization for twelve Arabic speaking countries in the Middle East. Saudi Pharm J. 2017;25(1):83–87. doi:10.1016/j.jsps.2016.01.001
22. Cleary J, Silbermann M, Scholten W, et al. Formulary availability and regulatory barriers to accessibility of opioids for cancer pain in the Middle East: a report from the Global Opioid Policy Initiative (GOPI). Ann Oncol. 2013;24(11):xi51–xi59. doi:10.1093/annonc/mdt503
23. Alharbi HA, Albabtain MA, Alobiad N, et al. Pain perception assessment using the short-form McGill pain questionnaire after cardiac surgery. Saudi J Anaesth. 2020;14(3):343–348. doi:10.4103/sja.SJA_34_20
24. Al-Rowaili A, Al-Aqeel SA, Al-Naim LS, et al. Appropriateness of cancer pain management in Saudi teaching hospital. Breast. 2009;39(5):37–43.
25. Alomi YA. National pharmacy pain management program at ministry of health in Saudi Arabia. J Pharmacol Clin Res. 2017;3(2):1–7. doi:10.19080/JPCR.2017.03.555606
26. Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10(4):390–392. doi:10.1197/aemj.10.4.390
27. Williams JR. The declaration of Helsinki and public health. Bull World Health Organ. 2008;86:650–652. doi:10.2471/BLT.08.050955
28. Simon LS. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. J Pain Palliat Care Pharmacother. 2012;26(2):197–198. doi:10.3109/15360288.2012.678473
29. Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–1379. doi:10.1016/S0895-4356(96)00236-3
30. Azad TD, Zhang Y, Stienen MN, et al. Patterns of opioid and benzodiazepine use in opioid-naïve patients with newly diagnosed low back and lower extremity pain. J Gen Intern Med. 2020;35(1):291–297. doi:10.1007/s11606-019-05549-8
31. Tucker H, Scaff K, McCloud T, et al. Harms and benefits of opioids for management of non-surgical acute and chronic low back pain: a systematic review. Br J Sports Med. 2020;54(11):664. doi:10.1136/bjsports-2018-099805
32. Morris BJ, Sciascia AD, Jacobs CA, et al. Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(4):619–623. doi:10.1016/j.jse.2015.09.017
33. Williams BT, Redlich NJ, Mickschl DJ, et al. Influence of preoperative opioid use on postoperative outcomes and opioid use after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28(3):453–460. doi:10.1016/j.jse.2018.08.036
34. Rodgers J, Cunningham K, Fitzgerald K, et al. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am. 2012;37(4):645–650. doi:10.1016/j.jhsa.2012.01.035
35. Heins JK, Heins A, Grammas M, et al. Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs. 2006;32(3):219–224. doi:10.1016/j.jen.2006.01.010
36. Desveaux L, Saragosa M, Kithulegoda N, et al. Understanding the behavioural determinants of opioid prescribing among family physicians: a qualitative study. BMC Fam Pract. 2019;20(1):1–12. doi:10.1186/s12875-019-0947-2
37. Stannard C. Tramadol is not “opioid-lite”. BMJ. 2019;365:2095. doi:10.1136/bmj.l2095
38. Thiels CA, Habermann EB, Hooten WM, et al. Chronic use of tramadol after acute pain episode: cohort study. BMJ. 2019;57(4):595.
39. Vassar M, Holzmann M. The retrospective chart review: important methodological considerations. J Educ Eval Health Prof. 2013;10:12. doi:10.3352/jeehp.2013.10.12
40. Panacek EA. Performing chart review studies. Air Med J. 2007;26(5):206–210. doi:10.1016/j.amj.2007.06.007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
