Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 7
Predictors of HIV-test utilization in PMTCT among antenatal care attendees in government health centers: institution-based cross-sectional study using health belief model in Addis Ababa, Ethiopia, 2013
Authors Workagegn F, Kirose G, Abebe L
Received 1 February 2015
Accepted for publication 25 March 2015
Published 13 July 2015 Volume 2015:7 Pages 215—222
DOI https://doi.org/10.2147/HIV.S82000
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Shenghan Lai
Fikremariam Workagegn, Getachew Kiros, Lakew Abebe
Health Education and Behavioral Sciences Department, Public and Medical Sciences College, Jimma University, Jimma, Ethiopia
Background: Human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS) is the most dramatic epidemic of the century that has claimed over two decades more than 3 million deaths. Sub-Saharan Africa is heavily affected and accounts for nearly 70% of all cases. Mother-to-child transmission of HIV is responsible for 20% of all HIV transmissions. With no preventive interventions, 50% of HIV infections are transmitted from HIV-positive mothers to newborns. HIV-testing is central to prevent vertical transmission. Despite, awareness campaigns, prevention measures, and more recently, promotion of antiviral regimens, the prevalence of cases and deaths is still rising and the prevalence of prevention of mother-to-child transmission (PMTCT) voluntary counseling test (VCT) use remains low. This study identifies predictors and possible barriers of HIV-testing among antenatal care attendees based on the health belief model (HBM) in Addis Ababa, Ethiopia.
Methods: The study was an institution-based cross-sectional survey conducted from September 1 to September 30, 2013. A total of 308 individuals were interviewed using structured questionnaires adopted and modified from similar studies. Data were collected through face-to-face interviews. A logistic regression was used to identify factors associated with HIV-test use.
Results: In spite of satisfactory knowledge on HIV/AIDS transmission, participants are still at high risk of contracting the infection, wherein only 51.8% tested for HIV; among the married, only 84.1% and among the gestational age of third trimester, 34.1% mothers tested for HIV. Based on the HBM, failure to use PMTCT-HIV-test was related to its perceived lack of net benefit (adjusted odds ratio [AOR] =0.34, confidence interval [CI] [0.19–0.58], P<0.001), but interviewees with high perceived self-efficacy were 1.9 times more likely to use HIV-test (AOR =1.90, CI [1.09–3.33], P<0.05).
Conclusion and recommendation: This study identifies perceived self-efficacy and perceived lack of net benefit as the main predictors of PMTCT-HIV-test use. Hence, prevention strategies based on increasing perceived risk, perceived severity, or adequate knowledge about HIV/AIDS may not be sufficient to induce PMTCT-HIV-test. These data will be useful in designing and improving HIV/AIDS prevention programs and focused health communication and counseling strategies in relation to PMTCT in Ethiopia.
Keywords: PMTCT, HIV-testing, health belief model, perceived net benefit, perceived threat, Addis Ababa, Ethiopia
Introduction
Mother-to-child transmission of human immunodeficiency virus (HIV) was estimated about 20% of all HIV transmissions. Out of 90% worldwide pediatrics HIV infections, 95% was recorded in the Sub-Saharan Africa.1 In all, 10% of childhood mortalities were counted due to HIV/acquired immune deficiency syndrome (AIDS) in Africa.2 If no interventions, 50% HIV infections were transmitted from HIV-positive mothers to the fetuses and newborns. On the other hand, despite there being a high HIV infection rate, antiretroviral prophylaxis coverage documented in Ethiopia is low.3,4
In all, 8,305 (9.3%) mothers received antiretroviral prophylaxis during 2010 all over the country. In Addis Ababa, 4,945 (34.6%) illegible mothers received antiretroviral prophylaxis during 2010.3 Similar antiretroviral prophylaxis use rate was recorded according to Ethiopian Demographic and Health Survey 2011.5 Ethiopian Demographic and Health Survey 2011 showed that 76% of antenatal clinic (ANC) attendees received counseling of HIV-test for prevention of mother-to-child transmission (PMTCT)-HIV infection.
Despite improved access to PMTCT services, the overall utilization rate remains low. However, there is a scarcity of operational research designed to identify predictors and facilitators to behavioral change.6
This study, which was conducted in Addis Ababa, identifies factors predicting PMTCT-HIV-test use that could be targeted by HIV outreach programs using the health belief model (HBM) framework. The HBM postulates that an individual’s actions are based on beliefs. It underlines main factors for decision making such as perceived vulnerability or susceptibility, perceived severity of the outcome or conditions, perceived efficacy or benefit of control measure, and the perceived barriers to prevention. It has been extensively used in behavioral sciences to predict behaviors and to design behavioral prevention programs.7
Methods and measurements
Study location and participants
Health institution-based cross-sectional study was conducted in 10% of government health centers. The study was conducted in Addis Ababa, Ethiopia, from September 1 to 30, 2013.
Sample size determination
Sample size of the study participants was determined using a single population proportion formula using prevalence of 0.76,5 alpha at 0.05 and CI at 95%.
The calculated sample size (n) =280. Final 308 sample size was determined by considering 10% non-response rate. Study participants were distributed based on 6 months average ANC attendee mothers’ flow in each health before the current study period. All women came to ANC follow-up at morning working hours from 8.30 am to 12.30 am and participated till all allocated sample size was fulfilled in each health center.
Sampling technique and procedures
Simple random sampling technique was employed to select ten health centers among 31 governmental health centers. Three months ANC follow-up and PMTCT counseling-registered mothers’ data were considered to get the average mothers’ flow rate per day, and then per month in each health center. Based on the average flow rate of ANC and PMTCT counseling services, proportional allocation of ANC flow attendees was made to each selected health center. Data were collected based on time-series during the morning working hours of all ANC attendees who are eligible for the study, till the sample size adequacy was fulfilled for each health center (Figure 1).
Data collection instruments and procedures
Research instruments were adopted and modified according to the context of the study area (29, 39). Nine sociodemographic questions and 12 knowledge questions were employed. For each six HBM constructs, six questions were used. The constructs perceived susceptibility, perceived severity, cues to action, self-efficacy, perceived barrier, and perceived benefit used six questions separately. Thus, there were 58 total questions, including the outcome variable in the questionnaire. English language questionnaire was translated to Amharic and back to English language to check consistency. Amharic’ version questionnaire was used during data collection.
Data collection was scheduled from 8.30 am to 12.30 am morning working hours and were collected by trained nurses through face-to-face interview. Days of data collection range from 21 days to 30 days based on actual ANC attendees flow.
Variables and measurements
Twelve multiple choice questions each having yes, I do not know, and no alternatives were used for knowledge items. These items include issues of HIV/AIDS, mother-to-child transmission, PMTCT, and HIV-testing. No and I do not know responses scored 0 point, while yes response scored 1 point. Responses were summed, and the mean score value was calculated. Score above the mean value was categorized as knowledgeable and below the mean value was considered as not knowledgeable.
Six HBM constructs measured using Likert-type questions of five scales scored ranging from 5 for strongly agree response to 1 for strongly disagree response in descending order. If negative statement was included, reverse coding was employed. Scores were summed for each construct items using compute and sum SPSS statistical tools. The mean total response per construct is determined based on the number of items provided or assigned for each construct per participant.
The outcome variable is utilization of PMTCT-HIV-test with response alternatives yes and no.
Data quality assurance
Data collection instruments were pretested and carried out by about 5% of pregnant women outside the target health centers. Modifications were made on perceived barriers and perceived benefits of response items. Principal investigators carried out supervision on a daily basis in each health center. Every afternoon, 5% of collected data were checked by three investigators for completeness and consistency. Collected data were locked inside a bookshelf and accessed by the investigators and the data clerk. Double entry using Epi Info version 3.2 and SPSS version 20 software was applied.
Data processing, analysis, and presentation
Collected data were coded and entered into Epi Info version 3.2 software and were cleaned and exported to SPSS version 20 for analysis. Data exploration and scatter plots were run to observe data concentrations and outlier responses. The mean score of computed items was used to dichotomize the variables. The reliability of each construct was checked using Cronbach’s alpha (α) (> =0.70. Those items with α value less than 0.7 were removed. Reliability test for knowledge items resulted in α value =0.744. Perceived threat items resulted in α value =0.713. Perceived net benefit items resulted in α value =0.790. Self-efficacy items resulted in α value =0.710.
Descriptive statistics, such as frequency and percentage, were used to describe categorical variables. Mean and standard deviation were computed for continuous sociodemographic variables.
Binary logistic regression was employed to investigate the association between independent variables and the outcome variable. Independent variables exhibited significant association at P<0.25 with outcome variable during binary logistic regression entered to multivariate logistic regression analyses for further statistical rigor in identifying predictors. Data were presented through tables.
Ethical appraisal
College of Public Health and Medical Sciences Research Ethics Committee (PHMRAC) reviewed the proposal and appraised. PHMRAC wrote a formal letter of appraisal. The department of Health Education and Behavioral Science wrote to the Addis Ababa Health Bureau for support and approval attached with ethical approval and proposal. The Addis Ababa Health Bureau received the proposal and an ethical appraisal letter, and gave a letter of permission to each selected health center. Respective health centers officially allowed carrying out the interviews. Each respondent was asked for willingness to participate after assuring confidentiality and anonymity. Verbal consent with yes and no check boxes was included on the questionnaire’s cover page. If the participant was willing to take part, yes box was marked and the interview was continued. Further, each study participant informed the right to withdraw from participation if felt uneasy during the interview. However, since interview did not incur health hazard and/or negatively affects true responses, written consent was not required from participants. Therefore, the researchers deliberately avoided written consent to get maximum true responses. Also, PHMRAC approval informed consent fitting. Every agreed and approved ethical condition was applied during the study.
Results
Sociodemographic characteristics
Among 308 pregnant women recruited in the study, 301 were interviewed (response rate of 97.7%). The mean age of the respondents was 29.4 (SD ±6.97). As to parity, 150 (49.8%) of them had two to four parity followed by one parity. In all, 121 (40.2%) and 30 (10.0%) of them had more than four parity. Concerning the current pregnancy gestational period, 118 (39.2%) and 99 (32.9%) of them were in the second and the third trimester, respectively.
As to marital status, 242 (80.4%) of them were married followed by 28 (9.3%) single, and the recent are widowed and separated. By ethnicity, 150 (49.8%) are Amhara, followed by Oromo, 64 (21.3%); Tigre, 35 (11.6%); Gurage, 30 (10.0%); and other ethnicity such as Afar, Nuer, and Anuak accounting for 22 (7.30%). One hundred seventy-nine (59.5%) of them were orthodox, followed by Protestant, 48 (15.9%); Catholic, 39 (13.0%); and Muslim, 35 (11.3%). The mean household income per month was 1,491 (SD ±1,980.14).
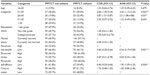
Pertaining to the respondents knowledge, 153 (50.8%) of them had good knowledge on HIV/AIDS and PMTCT-HIV-testing and its benefit. On the subject of the different dimensions of the HBM constructs, 139 (46.2%) of them had high perceived net benefits of having PMTCT-HIV-testing, even though among this group, only 95 (55.9%) of them had PMTCT-HIV-testing prior to the current study. Those who had high perceived threats were 169 (56.1%), of whom only 109 (64.1%) utilized PMTCT-HIV-testing. The high perceived self-efficacy group accounts for 153 (50.8%); of them, only 88 (51.8%) utilized PMTCT-HIV-testing. One hundred forty-five (48.2%) of them had high cues to action to utilize PMTCT-HIV-testing, but, among this group, only 87 (51.2%) of them utilized PMTCT-HIV-testing (Table 1).
Multivariate results
In order to predict the likelihood of utilization of PMTCT/HIV-test in both study subjects (not utilized and utilized), multiple logistic regression was used by controlling the effect of confounding variables if any exist and enter method was used. All the variables that were found significant (P-value <0.25) in the bivariate logistic regression were included in the process of fitting a model. The overall model to predict probability of utilization of PMTCT/HIV-test in participants was statistically significant (−2log likelihood =232.01, χ2=109.75, df =11) with a P-value <0.0001, and the overall prediction of the model was 80.5%.
Variables fitted to multiple logistic regressions were age, perceived net benefit, perceived threat, perceived self-efficacy, and cues to action. In multiple logistic regression model, marital status educational status, cues to action, and perceived threats did not show a valid statistical association with HIV-test utilization among ANC attendees.
But, ANC attendees between age group 21 and 25 years were 2.43 times (adjusted odds ratio [AOR] =2.43, CI [1.13–5.23], P<0.05) more likely to utilize HIV-test than those in the age group above 35 years. ANC attendees between age group 26 and 30 years were 2.3 times more likely (AOR =2.3, CI [1.08–4.88], P<0.05) to utilize HIV-test when compared to those above 35 years age group. Nevertheless, being either to age group 31–35 years or 16–24 years did not show a statistical association with HIV-test utilization.
Those ANC attendees who had low perceived net benefits were found to be 0.34 (AOR =0.34, CI [0.19–0.58], P<0.001) times less likely to utilize HIV-test for PMTCT. Respondents who had high perceived self-efficacy were found to be 1.90 (AOR =1.90, CI [1.09–3.33], P<0.05) times more likely to utilize HIV-test for PMTCT on the present pregnancy (Table 2).
Discussion
ANC attendee groups who were between 21–25 years and 26–30 years were found to be more likely to have HIV-test for PMTCT of HIV infection. Those who were either between age group 16–20 years or 31–35 years did not have better HIV-test utilization behavior when compared to older age groups. This might be due to low HIV risk perception when age increases or fearful threat perception when younger. Some studies support this finding,8,9 but other studies fail to show a statistical significant association between age and HIV-testing among ANC attendees.10,11 These two groups might be different in their perceived threats and risk perceptions, among many other factors. Thus, there is a need to study among different age groups differently with large samples.
Similar findings occurred regarding marital status and HIV-test among ANC attendees in the current study. Single and married ANC attendee groups were found to be more likely to have HIV-test for PMTCT of HIV infection than the widowed group. But predictors might differ among these marital groups. Single groups might be either young, educated, or unmarried, and with a greater perception of risk, as was supported by one Tanzanian study that suggested that the younger group had better knowledge level and utilized HIV-tests.10 On the other hand, those married might discuss with their husbands, and agreed decision may be in place. However, those divorced or separated, despite getting pregnancy, might have a different internal mental setup than the other groups. One probable explanation might be that they may perceive a low risk of HIV infection as the widowed group. The reason can be mindset, for example, perceiving low risk of HIV infection as a result of having infrequent sexual intercourse. But contracting HIV infection can be possible by even one-time sexual intercourse. At least they did have sexual intercourse while the recent pregnancy conception happened.
Altogether, marital status and HIV-test utilization among ANC attendees showed a statistical valid association with the other study10 as it is with the present study. However, segregation of these study groups and detail understanding of each group might be useful to understand predictors.
In our study, knowledge did not show a statistical association with HIV-test for PMTCT of HIV infection among ANC attendees. This finding is in incongruity with many previous studies where knowledge was mentioned as a predictor.8,9,11,12
Two constructs of HBM found predictors of HIV-test utilization of ANC attendees in our study. Perceived net benefit being low or negative was found to be negatively associated with utilization of HIV-test for PMTCT of HIV infection in this study. This finding is supported by other studies8–11,13 where perceived barriers were negatively affected by HIV-test among similar group of study participants.
This study exhibits that perceived self-efficacy being high was a strong predictor of HIV-test utilization among ANC attendees. This finding was supported by other recent studies as well.8,11,14 Therefore, building self-efficacy might have utmost effects to predispose pregnant mothers to have HIV-test for PMTCT of HIV infection.
Perceived threat (aggregate of the sum of perceived susceptibility and perceived severity) fails to produce a valid statistical association with HIV-test of ANC attendees in our study. This finding is in contrary to the previous studies. The previous studies focused on one subdimension (either perceived susceptibility or perceived severity), but the present study applied aggregated sum value of these two dimensions to measure perceived threat.8–11,14,15
Limitation
Since our study assesses only utilization of HIV-test for PMTCT of HIV infection, it does not mean that it is an end by itself. The pregnant mothers tested HIV positive may not step to all continuum. ART prophylaxis and correct breast replacement feeding practices and underlying factors need investigation as well. The findings have limitations to be generalized to other Ethiopian pregnant mothers’ HIV-test utilization for PMTCT of HIV infection, because Addis Ababa resident women might have a different social and economic background than others, particularly the rural Ethiopian women. This study may not reflect those ANC attendee pregnant mothers who went to private health institution for the same purpose. The other limitation of this study could be that its findings are not richly discussed with previous studies. This happens due to two main reasons. First, similar studies using HBM constructs were limited previously. Second, those limited HBM-based studies were oftentimes found measuring subdimension of a construct. For example, perceived net benefit has two dimensions, such as perceived barriers and perceived benefits, but most studies focused only on perceived barriers.
Strength
HBM constructs were measured through all dimensions using at least six questions per construct.
Conclusion
Age group and marital status, among sociodemographic variables, and perceived net benefit and self-efficacy among HBM constructs found statistically significant predictors on HIV-testing utilization of ANC attendees.
Family income, number of births, cues to action, and knowledge showed statistical association with HIV-test utilization of ANC attendees in many studies previously, despite these not showing prediction in this study. This may be due to the change in predictors of ANC attendees’ HIV-test utilization for PMTCT of HIV infection through time.
Recommendations
- Benefits of HIV-testing during pregnancy need to be communicated through focused and appropriate mechanisms by counselors and implementers.
- There has to be a mechanism to reduce the perceived barriers held by ANC attendees during counseling and health communication sessions.
- There has to be a mechanism to build the self-efficacy of mothers, particularly pregnant mothers, so that they feel confident and are able to undergo HIV-test.
Acknowledgments
The authors acknowledge Health Education and Behavioral Sciences Department of Jimma University, Addis Ababa Health Bureau, all the health centers, and study participants taking part in this study without whom this study might not be possible.
The authors deeply acknowledge Health Education and Behavioral Sciences Department’s experts for their critical advice, while they had been working on revising the manuscript to increase its readability.
Last but not the least, they deeply thank W/ro Zenebech Asefa who cared them during the previous 3 weeks, more than ever, while they had been rewriting and revisiting all analyses for longer hours per day.
Authors’ contributions
Fikremariam Workagegn (first author). Contributed to the development and write-up of the proposal, presenting to the Ethical Appraisal Committee, and reviewed and corrected the Ethical Appraisal Committee’s comments. He contributed to recruit data collectors, supervise data collection, and collect the filled questionnaire daily. He coded and entered data into Epi Info version 3.2 software for editing and transferring the data to SPSS version 20. He was the primary person to analyze and write draft results.
Getachew Kiros (second author) was the second adviser of this research. He reviewed the proposal, analyzed the final data, and prepared the draft manuscript. He was also involved in supervision of data collection and presentation of the proposal to the Ethical Appraisal Committee. The major revision of the analyses was carried out by him.
Lakew Abebe (third author) was the first adviser of this research undertaking. He also supervised the two authors during the concept development, research design, conceptualization of the research, and adoption and modification of the instruments. He supervised data collection, final analyses, and writing up. He revised the document and prepared the manuscript in detail. He is also the corresponding author of this article.
Disclosure
The authors have declared that there are no competing financial and non-financial competing interests.
References
Central Statistical Agency; ICF International. Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiopia: CSA; 2012. | |
UNAIDS. World AIDS Day Report. Geneva: UNAIDS; 2011. | |
WHO. Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants in Resource-Limited Settings: Towards Universal Access: Recommendations for a Public Health Approach. Geneva: WHO; 2006. | |
FDRE MOH. HSDP IV Annual Performance Report of the Ethiopian Fiscal Year 2010/2011. Ethiopia: EFY; 2003 (2010/2011):30. | |
Federal HAPCO. Strategic Plan II for Intensifying Multi-sectoral HIV and AIDS Response in Ethiopia. Multisectoral HIV/AIDS Response Annual Monitoring and Evaluation Report, Ethiopia; 2009. | |
Demissie A, Deribew A, Abera M. Determinants of acceptance of voluntary HIV testing among antenatal clinic attendees at Dil Chora Hospital, Dire Dawa, East Ethiopia. Ethiop J Health Dev. 2009;23(2):141–147. | |
Moges Z, Amberbir A. Factors associated with readiness to VCT service utilization among pregnant women attending antenatal clinics in Northwestern Ethiopia: a health belief model approach. Ethiop J Health Sci. 2011;21:107–115. | |
De Paoli MM, Manongi R, Klepp K-I. Factors influencing acceptability of voluntary counselling and HIV-testing among pregnant women in Northern Tanzania. AIDS Care. 2004;16(4):411–425. | |
Fanta W, Worku A. Determinants for refusal of HIV testing among women attending for antenatal care in Gambella Region, Ethiopia. Reprod Health. 2012;9:8. | |
Deressa W, Seme A, Asefa A, Teshome G, Enqusellassie F. Utilization of PMTC services and associated factors among pregnant mothers attending ANC clinics in Addis Ababa, Ethiopia. BMC Pregnancy Child Health. 2014;14:328. | |
Pharris A, Nguyen TK, Tishelman C, Brugha R, Nguyen PH, Thorson A. Expanding HIV testing efforts in concentrated epidemic settings: a population-based survey from rural Vietnam. PLoS One. 2011;6(1):e16017. | |
Kakimoto K, Sasaki Y, Kuroiwa C, Vong S, Kanal K. Predicting factors for the experience of HIV testing among women who have given birth in Cambodia. Biosci Trends. 2007;1(2):97–100. | |
Campbell-Stennett D, Holder-Nevins D, McCawBinns A, Eldemire-Shearer D. Are women ready to do HIV test? West Indian Med J. 2009; 58(6):575–579. | |
Brookmeyer R, Gail MH. AIDS Epidemiology. A Quantitative Approach. New York: Oxford University Press; 1994. | |
Coreil J, Bryant CA, Henderson JN. Social and Behavioral Foundations of Public Health. California: Sage Publications, Inc.; 2001. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.