Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Predictors of Discrimination Towards People Living with HIV/AIDS Among People Aged 15–49 Years in Ethiopia: A Multilevel Analysis
Authors Arefaynie M , Damtie Y , Kefale B , Yalew M
Received 15 January 2021
Accepted for publication 18 February 2021
Published 15 March 2021 Volume 2021:13 Pages 283—292
DOI https://doi.org/10.2147/HIV.S299812
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Mastewal Arefaynie, Yitayish Damtie, Bereket Kefale, Melaku Yalew
Department of Reproductive and Family Health, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Mastewal Arefaynie
Department of Reproductive and Family Health, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Tel +251 912867518
Email [email protected]
Background: There is limited national representative evidence on determinants of discrimination towards people living with HIV/AIDS especially, community-level factors that are not investigated in Ethiopia. Thus, this study aimed to assess individual and community-level factors associated with discrimination towards people living with HIV/AIDS among 15– 49 age people in Ethiopia.
Methods: A secondary data analysis was done on the 2016 Ethiopian Demographic and Health Survey dataset which was collected cross-sectional. A total of 25,927 weighted 15– 49 age people were included in the analysis. Multi-level mixed-effect logistic regression analysis was done by STATA version 14.0 to identify individual and community-level factors. Adjusted odds ratio with 95% confidence interval was used to show the strength and direction of the association and statistical significance was declared at P value less than 0.05.
Results: From individual level factors, being female [AOR=1.47, 95% CI= (1.18, 1.83)], not attend education [AOR=5.88,95% CI= (4.50, 7.67)], attending primary education [AOR=3.03, 95% CI= (2.40, 3.81)] and attending secondary education [AOR=1.48, 95% CI= (1.19, 1.82)] have discrimination attitude towards people living with HIV/AIDS. From community level factors, live in low proportion of educated communities [AOR=1.33, 95% CI= (1.01, 1.65)], rural dweller [AOR=1.65, 95% CI= (1.23, 2.21)], live in low proportion of HIV tested communities [AOR=1.61, 95% CI= (1.33, 1.93)] were significantly associated with discrimination attitude towards people living with HIV/AIDS.
Conclusion: Sex of the respondent, religion, educational status, household wealth index, marital status, media exposure, internet use, HIV test status, region, and residence, community level of education, and community level of HIV test status were predictors of discrimination attitude towards people living with HIV/AIDS in Ethiopia. Improving educational and community-level HIV/AIDS test coverage are important interventions to reduce discrimination towards people living with HIV/AIDS in the country.
Keywords: discrimination, people living with HIV/AIDS, Ethiopia, multilevel analysis
Introduction
Collaborative international and national efforts during Millennium Development Goals (MDGs), decreases HIV/AIDS-related deaths and infections.1,2 The extension of MDGs, Sustainable Development Goals (SDGs), aims to end the HIV/AIDS epidemic by 2030.3,4 At the end of 2030, there will be a 90% decline in the number of new HIV infections and AIDS-related deaths.5,6
The fast-track response sets targets on the HIV treatment cascade: 90% of people living with HIV (PLHIV) knowing their HIV status, 90% of people who know their status receiving treatment, and 90% of people on treatment having a suppressed viral load.7,8
HIV/AIDS is both a medical and social problem. People living with HIV are stigmatized leading to severe social consequences related to their rights, health care services, freedom, self-identity, and social interactions. It also severely hampers the treatment and diagnosis of HIV contributing to the further spread of the disease. Such responses disrupt an individual’s social interactions and thereby lead to a feeling of isolation.9–16
AIDS-related discriminations are the product of multiple social influences including attributions of responsibility for HIV infection and beliefs that individuals with HIV/AIDS are contaminated and tainted. The discrimination also reproduces inequalities of class, race, and gender.14,15,17–22
Discrimination greatly affects the quality of life of PLWHA, their family members, and the healthcare providers who work with them.8,10,23–27 People who experienced discrimination face loss of income or job, isolation from communities, and inability to participate as a productive member of society.28 Moreover, it is a barrier for ART adherence which accelerates disease progression.23,29–32 It increases the risk of mental health problems,33–35 hinders the utilization of different HIV/AIDS-related services.31,36–38
Even though, magnitude of discrimination towards PLWHA is reduced in the last decade in Africa, it is still a public health problem which affects the successes of HIV-related programs in the continent.39–43
In Ethiopia, the prevalence of HIV/AIDS-related discrimination is high. In Dessie (41.93%),44 Jimma referral hospital (56%),45 Oromia (62%),24 Amhara (34%).46 Sex of the respondent,44,45 residence,44,47 non-disclosure of HIV status,44 educational status45 is some of the factors responsible for HIV/AIDS-related stigma. But, all the studies were done at the local level, use a small sample size, and do not consider the effect of community-level factors. Besides, the association at the individual level may not work at the community-level and vice versa. Even all the studies were fitted with standard logistic regression which may lead them to loss of power. National representative evidence is important to achieve national and international goals. Thus, the current research aimed to determine individual and community level factors affecting discrimination on PLWHA using multilevel modeling using EDHS 2016 data. It will be important to develop community-level information education communication and behavioral change communication to reduce the prevalence and impact discrimination towards PLWHA in the country.
Methods
Study Setting and Period
The study was conducted in Ethiopia, which is located in the northeastern (horn of) Africa, lies between 3° and 15° North latitude and 33° 48° and East longitudes. EDHS is carried out every five years. The 2016 EDHS was carried out in all parts of Ethiopia, in nine regional states and two administrative regions. 2016 EDHS dataset was collected by the Central Statistical Agency (CSA).48 Data were accessed from their URL: www.dhsprogram.com by contacting them through personal accounts after justifying the reason for requesting the data. Secondary data analysis was done on 2016 EDHS among 15–49 aged people who were heard about HIV/AIDS.
A total of 25,927 weighted 15–49 year people were included in the analysis. EDHS 2016 sample was stratified into two stages. The first stratification was done by region and then each region stratified as urban and rural, yielding 21 sampling strata. A total of 645 (202 urban and 443 rural) enumeration areas (EAs) were selected. In the second stage affixed number of 28 households were selected per cluster in equal chance.
Variable Measurement
In this study, the outcome variable (discrimination towards PLWHA) was dichotomized as (Yes/No) which was generated from EDHS-2016.49 EDHS-2016 uses two questions to assess the level of HIV/AIDS discrimination (children with HIV should be allowed to attend school with children without having HIV and buy vegetables from a vendor who has HIV). People answering “Yes” for both of the above questions were considered as not having a discrimination attitude towards PLWHA. Otherwise, they were considered as having a discriminatory attitude towards PLWHA. The independent variables were individual-level factors including (sex, religion, marital status, wealth index, educational status, media exposure, internet use, HIV tested) and community-level factors were created by aggregating individual-level factors in each cluster (region, residence, community level of education, community-level wealth index, community-level media exposure, community level of HIV test).
Data Processing and Analysis
Data cleaning was conducted to check for consistency with the EDHS-2016 descriptive report. Recoding, variable generation, labeling, and analysis were done by using STATA/SE version 14.0. Descriptive statistics were done to describe the study participants about socio-demographic characteristics that were presented in tables and text. Sample weight was used to compensate for the unequal probability of selection between the strata that were geographically defined and for non-responses. Multilevel analysis was conducted after checking the data was eligible for multilevel analysis (by using an intra-cluster correction coefficient). When the ICC is greater than 10% (ICC= 36.6%) the community-level factors affect the dependent variable. Therefore, it is better to identify community-level factors to develop and take different interventions. Since EDHS data were hierarchical (individual “level 1” were nested within community “level 2”), a two-level mixed-effects logistic regression model was fitted to estimate both independent (fixed) effects of the explanatory variables and community level random effects on discrimination towards PLWHA. The log of the probability of discrimination was modeled using a two-level multilevel model as follows:50 Log = β0 + β1Xij + B2Zij + µj + eij Where I and j are individual level and community level (2) units, respectively; X and Z refer to individual and community level variables, respectively;
= β0 + β1Xij + B2Zij + µj + eij Where I and j are individual level and community level (2) units, respectively; X and Z refer to individual and community level variables, respectively;  is the probability of discrimination for the ith people in the jth community; β’s indicates the fixed coefficients. (Β0) is the intercept, the effect on the probability of discrimination in the absence of influencing factors; and µj showed the random effect (the effect of the community on discrimination of the jth community), and eij showed random errors at an individual level. By assuming each community had a different intercept (Β0) and fixed coefficient (β), the clustered data nature and intra- and inter-community variations were taken into account.
is the probability of discrimination for the ith people in the jth community; β’s indicates the fixed coefficients. (Β0) is the intercept, the effect on the probability of discrimination in the absence of influencing factors; and µj showed the random effect (the effect of the community on discrimination of the jth community), and eij showed random errors at an individual level. By assuming each community had a different intercept (Β0) and fixed coefficient (β), the clustered data nature and intra- and inter-community variations were taken into account.
During analysis first, bi-variable multilevel logistic regression was fitted and variables with p-value less than 0.2 at model I, and model II were selected to develop the 3rd model (the final model). The analysis was done in four models. The first model was, model-0 (empty model or null model/without explanatory variable; to secure the need for multilevel analysis). The second model was, model-I (analyzing only individual-level variable), the 3rd model was, model-II (analyzing only community-level variable), the last model, model-III (analyzing both community level and individual level variables based on the cutoff point).
The measure of association (fixed effects) estimates the association between the likelihood of discrimination towards PLWHA and different explanatory factors were expressed by Adjusted Odds Ratio (AOR) with respective 95% confidence level. A P-value less than 0.05 was used as a cut-off point to declare significant association at model-III. The random-effects (variations) were measured by using ICC (model-0), Median Odds Ratio (MOR) in (model-I and II), and Proportional Change in Variance (PCV) was measured to show variation between clusters.
The higher the ICC, the community characteristics are more relevant to understand individual variation. It is calculated as ICC =  , where δ2 indicates the estimated variance of clusters. MOR is the median value of the odds ratio between the area at highest risk and the area the lowest risk when randomly picking out two areas and it was calculated as MOR= exp. (
, where δ2 indicates the estimated variance of clusters. MOR is the median value of the odds ratio between the area at highest risk and the area the lowest risk when randomly picking out two areas and it was calculated as MOR= exp. (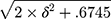 )≈ exp (0.95δ). In this study, MOR shows the extent to which the individual probability of discrimination towards PLWHA was determined by place of residence. PCV measures the total variation attributed by individual-level variables and area51 level variables in the final model (model-III).
)≈ exp (0.95δ). In this study, MOR shows the extent to which the individual probability of discrimination towards PLWHA was determined by place of residence. PCV measures the total variation attributed by individual-level variables and area51 level variables in the final model (model-III).
It is calculated as PVC = [(δ2of null model – δ2 of each model)/δ2of null model]. δ2 of the null model is used as a reference. Multicollinearity was checked among explanatory variables by using standard error at cutoff point ±2. No Multicollinearity is the standard errors were between ±2. The log-likelihood test was used to estimate the goodness of fit of the adjusted final model (model-III) in comparison to the preceding models (model-I and model-II) individual and community model adjustments, respectively.
Ethical Approval
Ethical clearance was obtained from Ethical Review Committee of Wollo University College of Medicine and Health Science. An authorization letter was also obtained from CSA for downloading the EDHS data set by requesting the website www.measuredhs.com. The accessed data were used for the registered research only. All data were treated as confidential and no effort was done to identify any household or individual respondent interviewed in the survey. The detailed information on methodology and the ethical issues was published in the EDHS report.
Results
Characteristics of the Respondents
A total of 25,927 people aged from15-49 years were included in the analysis. A total of 14,599 of the respondents were female. In total, 9704 (37.4%) of the respondents did not attend school. A total of 13,720 (52.9%) of the population have media exposure and 13,712 (52.9%) of the population did not ever test for HIV (Table 1).
 |
Table 1 Individual and Community-Level Characteristics of 15 to 49 Age People in Ethiopia, EDHS 2016 (n=25,927) |
Individual and Community-Level Factors Associated with Discrimination Towards PLWHA
In the final model (model-III) sex of the respondent, educational status, household wealth index, internet use, residence, media exposure, tested for HIV, marital status, region, community level of education, and community level of tested for HIV had a statistical association with discrimination towards PLWHA.
The odds of discrimination towards PLWHA were 1.5 times more among female participants as compared to males [AOR=1.47,95% CI= (1.18, 1.83)]. The odds of discrimination towards PLWHA were 1.7 times more among participants who are rural residents as compared to urban dwellers [AOR=1.65, 95% CI= (1.23, 2.21)]. People who were not attend education, attending primary education and attending secondary education 6 times, 3 times and 1.5 times more likely discriminate PLWHA when compared with people attending higher education [AOR=5.88,95% CI= (4.50, 7.67)], [AOR=3.03, 95% CI= (2.40, 3.81)], and [AOR=1.48, 95% CI= (1.19, 1.82)], respectively.
People who live in a low proportion of educated communities were 1.3 times more discriminatory attitudes towards PLWHA than people who live in a high proportion of educated community [AOR=1.33,95% CI= (1.01, 1.65)]. Women who live in a low proportion of HIV-tested communities were 1.6 times more discriminatory attitudes towards PLWHA than people who live in a high proportion of HIV-tested community [AOR=1.61,95% CI= (1.33, 1.93)] (Table 2).
 |
Table 2 Multilevel Logistic Regression Analysis of Individual and Community-Level Factors Associated with Discrimination Towards PLWHA in Ethiopia, EDHS 2016 (n=25,927) |
Random Effects (Measures of Variation)
Discrimination towards PLWHA varies significantly across each cluster. ICC indicated, 36.6% of the variation in discrimination attitude towards PLWHA among 15 to 49 age population was attributed to community-level factors. PCV in the final model shows 78% of the variation in discrimination towards PLWHA across communities was explained. Likewise, MOR for discrimination towards PLWHA among the population, in the null model was 28.8 which shows the presence of variation across each cluster (Table 3)
 |
Table 3 Measure of Variation for Discrimination Towards PLWHA Among 15 to 49 Year People at Cluster Level in Multilevel Logistic Regression Analysis, EDHS 2016 |
Discussion
The analysis in model-III showed that; Individual-level factors (sex of the respondent, religion, educational status, household wealth index, marital status, media exposure, internet use, and HIV test status) and community-level factors (region, residence, community level of education, and community level of HIV test status) have a significant association with HIV related stigma in Ethiopia.
HIV testing status affects discrimination attitude towards PLWHA at the individual and contextual level in Ethiopia. People who are not tested for HIV/AIDS have a more expressive discriminatory attitude towards PLWHA. Similarly, when a low proportion of people tested for HIV live in the cluster, the contextual level of discrimination towards PLWHA is high. The finding is consistent with previous researches done in Kenya52 and Thailand. This might be due to pre-test information and post-test counseling on the key principles of HIV testing and counseling and is expected to create an opportunity to avoid misconceptions about HIV/AIDS. Moreover, during HIV testing clients might get comprehensive information on the availability of different interventions which are essential to correct misconceptions including discrimination. Community-level of HIV/AIDS-related attitudes and knowledge might be high when a high proportion of the community is tested for HIV. HIV testing might initiate a formal or informal discussion about HIV/AIDS among the community, which is a mechanism that has been suggested to have a greater influence on personal knowledge of PLWHA that decreases HIV-related discrimination and risk behaviors related to HIV.52 On the other hand, fear of stigmatization and discrimination is a barrier to HIV testing in diverse settings.53–56 Discussion about HIV/AIDS in informal or formal settings within existing social networks may reduce negative attitudes towards PLWHA.14
Media exposure and utilization of the internet reduce discrimination towards PLWHA. The finding is consistent with researches done in china.57 This might be since the media has an enormous influence on educating and imparting proper knowledge that dilutes pre-existing misconceptions regarding HIV/AIDS.
The community-level and individual level of education affect the acceptance of discrimination towards HIV/AIDS. When educational attainment increases, the acceptance of HIV-related discrimination is reduced. Similarly, when a low proportion of educated individuals live in the cluster, the acceptance of HIV-related discrimination is high. The result is supported by researches in China,57 Nigeria,58 Dominican Republic,59 Haiti,59 Botswana,60 Ghana.61 This might be due to educated individuals have access to better information through mass media, the internet, and access to health services related to HIV/AIDS. Moreover, the contextual level of education plays a great role in the reduction of discriminatory attitudes on PLWHA at the community level.
Females have more odds of discrimination towards PLWHA than males in Ethiopia. The finding is similar to findings in china,57 Dominican Republic,59 Nigeria.58,62 The reason might be due to better education, media exposure, and health service access for males in Ethiopia than female.49
Married individuals have a more discriminatory attitude toward HIV/AIDS than singles. This is evidenced by other studies done in China57 and Nigeria.58 It might be due to most married people live in rural settings in Ethiopia and have not attended school to a high level. Moreover, they might not access the internet, television, and radio due to workload and/living arrangements.
As the household wealth index increases, discrimination on PLWHA is reduced. The finding is supported by researches from Nigeria,58 Ghana,61 Kenya,52 Sub-Saharan Africa.63 This might be due to rich peoples may have good health-seeking behavior, better knowledge on HIV, and access different behavioral change communication through mass media or social media. This may change the values and norms of the community towards PLWHA.
Rural dwellers have a discriminatory attitude towards PLWHA than urban residents. The finding is consistent with previous researches in Nigeria,58 Turkish,64 Dominican Republic,59 Ghana.61 There may be greater access to accurate information about HIV/AIDs in urban settings. When high social support is there, HIV-related discrimination is reduced. Social urbanization might create a big opportunity to mass media exposure, internet access, formal and informal education on HIV/AIDS, comprehensive knowledge on the transmission and prevention mechanisms of the virus.
There is a regional variation on discrimination towards PLWHA in Ethiopia. People who live in developing regions have a discriminatory attitude toward HIV/AIDS than developed regions. In developed regions, there might be accessible health services, educational opportunities, and information on HIV/AIDS. Moreover, cultural, religious values, and norms may be different across the regions. Moreover, people who live in these developing regions of Ethiopia, have poor access to education, media, and health-care facilities. Most pastoralist communities are living in those regions where delivering health and other developmental services has been very difficult, depriving them of awareness of HIV.
The result of this study was more representative than other studies and the model considered different levels of analysis as the outcome was affected by community-level variables. Despite this strength, the result may be prone to recall bias because the data were collected from a history of the event.
Conclusion
After computing multi-level analysis, sex of the respondent, religion, educational status, household wealth index, marital status, media exposure, internet use, HIV test status, region, residence, community level of education, and community level of HIV test status have a significant association with HIV related discrimination in Ethiopia. Improving educational coverage, improving community-level HIV/AIDS test coverage are important interventions to reduce discrimination towards people living with HIV/AIDS in the country. Since discrimination towards PLWHA has differences across the community, better to develop community-sensitive approaches for different communities.
Abbreviations
CSA, Central Statistics Agency; EA, enumeration area; ICC, inter cluster coefficient; MOR, median odds ratio; PCV, proportional change variance.
Data Sharing Statement
The datasets used and/or analysed during this study are available from the corresponding author on reasonable request.
Acknowledgment
The authors would like to acknowledge the Ethiopian Central Statistical Agency for providing an authorization letter to access the EDHS-2016 dataset to conduct this study.
Disclosure
The authors declare that they have no competing interests.
References
1. HIV/AIDS JUNPo. Miles to go: closing gaps, breaking barriers, righting injustices. Geneva: UNAIDS; 2018:4.
2. HIV/AIDS JUNPo. UNAIDS data 2017. Geneva: UNAIDS; 2017:1–248.
3. Tinasti K. HIV and AIDS among adolescents who use drugs: opportunities for drug policy reform within the sustainable development agenda. J Int AIDS Soc. 2018;21:e25045. doi:10.1002/jia2.25045
4. Sidibé M, Nygren-krug H, Mcbride B, Buse K. The Future of Global Governance for Health. Human rights in global health: rights-based governance for a globalizing world; 2018:87.
5. Del Rio C. The global HIV epidemic: What the pathologist needs to know. Semin Diagn Pathol. 2017;34(4):314–317. doi:10.1053/j.semdp.2017.05.001.
6. Xia Q, Lazar R, Bernard MA, et al. New York City achieves the UNAIDS 90-90-90 targets for HIV-infected whites but not Latinos/Hispanics and blacks. JAIDS. 2016;73(3):e59–e62. doi:10.1097/QAI.0000000000001132
7. HIV/AIDS JUNPo. Global AIDS update 2016. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2017.
8. Assefa Y, Gilks CF, Dean J, et al. Towards achieving the fast-track targets and ending the epidemic of HIV/AIDS in Ethiopia: successes and challenges. Int J Infect Dis. 2019;78:57–64. doi:10.1016/j.ijid.2018.10.022
9. Ahsan Ullah A. HIV/AIDS-related stigma and discrimination: a study of health care providers in Bangladesh. J Int Assoc Physicians AIDS Care. 2011;10(2):97–104. doi:10.1177/1545109710381926
10. Ajong AB, Njotang PN, Nghoniji NE, et al. Quantification and factors associated with HIV-related stigma among persons living with HIV/AIDS on antiretroviral therapy at the HIV-day care unit of the Bamenda Regional Hospital, North West Region of Cameroon. Global Health. 2018;14(1):56. doi:10.1186/s12992-018-0374-5
11. Bharat S. A systematic review of HIV/AIDS-related stigma and discrimination in India: current understanding and future needs. SAHARA J. 2011;8(3):138–149. doi:10.1080/17290376.2011.9724996
12. Doka PJS, Danjin M, Dongs IS. HIV/AIDS-related stigma and discrimination among health-care providers in a tertiary health facility. J Med Sci. 2017;37(2):44. doi:10.4103/jmedsci.jmedsci_99_16
13. Odimegwu CO, Alabi O, De Wet N, Akinyemi JO. Ethnic heterogeneity in the determinants of HIV/AIDS stigma and discrimination among Nigeria women. BMC Public Health. 2018;18(1):763. doi:10.1186/s12889-018-5668-2
14. Seeley J, Blanc AK. Reducing stigma and discrimination: new evidence and its implications. LWW; 2020.
15. Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823–1831. doi:10.1016/j.socscimed.2007.01.006
16. Sweileh WM. Bibliometric analysis of literature in AIDS-related stigma and discrimination. Transl Behav Med. 2019;9(4):617–628. doi:10.1093/tbm/iby072
17. Arrey AE, Bilsen J, Lacor P, Deschepper R. Perceptions of stigma and discrimination in health care settings towards sub-Saharan African migrant women living with HIV/AIDS in Belgium: a qualitative study. J Biosoc Sci. 2017;49(5):578–596. doi:10.1017/S0021932016000468
18. Logie CH, Jenkinson JI, Earnshaw V, Tharao W, Loutfy MR. A structural equation model of HIV-related stigma, racial discrimination, housing insecurity and wellbeing among African and Caribbean Black women living with HIV in Ontario, Canada. PLoS One. 2016;11(9):e0162826. doi:10.1371/journal.pone.0162826
19. Parker CM, Garcia J, Philbin MM, Wilson PA, Parker RG, Hirsch JS. Social risk, stigma and space: key concepts for understanding HIV vulnerability among black men who have sex with men in New York City. Cult Health Sex. 2017;19(3):323–337. doi:10.1080/13691058.2016.1216604
20. Parker RG, Aggleton P, Attawell K, Pulerwitz J, Brown L. HIV/AIDS-related stigma and discrimination: a conceptual framework and an agenda for action. New York: Population Council; 2002.
21. Parker W, Schubert J, Owusu-Ansah S, et al. Addressing community-level stigma toward key populations: communication insights from action research in Ghana. African J AIDS Res. 2020;1–8.
22. Sen S, Aguilar JP, Petty M. An ecological framework for understanding HIV-and AIDS-related stigma among Asian American and Pacific Islander men who have sex with men living in the USA. Cult Health Sex. 2019;1–13.
23. Dehghan M, Shokoohi M, Mokhtarabadi S, et al. HIV-related knowledge and stigma among the general population in the southeast of iran. Shiraz E Med J. 2020;21(7):1–8. doi:10.5812/semj.96311
24. Parcesepe A, Tymejczyk O, Remien R, et al. HIV-related stigma, social support, and psychological distress among individuals initiating ART in Ethiopia. AIDS Behav. 2018;22(12):3815–3825. doi:10.1007/s10461-018-2059-8
25. Tesfay F, Javanparast S, Mwanri L, Ziersch A. Stigma and discrimination: barriers to the utilisation of a nutritional program in HIV care services in the Tigray region, Ethiopia. BMC Public Health. 2020;20(1):1–13. doi:10.1186/s12889-020-09040-6
26. Johnny L, Mitchell C. “Live and let live”: an analysis of HIV/AIDS-related stigma and discrimination in international campaign posters. J Health Commun. 2006;11(8):755–767. doi:10.1080/10810730600934708
27. Kabbash IA, Ali EAA, Elgendy MM, et al. HIV/AIDS-related stigma and discrimination among health care workers at Tanta University Hospitals, Egypt. Environ Sci Pollut Res. 2018;25(31):30755–30762. doi:10.1007/s11356-016-7848-x
28. dos Santos MM, Kruger P, Mellors SE, et al. An exploratory survey measuring stigma and discrimination experienced by people living with HIV/AIDS in South Africa: the People Living with HIV Stigma Index. BMC Public Health. 2014;14(1):80. doi:10.1186/1471-2458-14-80.
29. Turan B, Rice WS, Crockett KB, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: the mediating role of depression. AIDS. 2019;33(3):571. doi:10.1097/QAD.0000000000002071
30. Camacho G, Kalichman S, Katner H. Anticipated HIV-related stigma and HIV treatment adherence: the indirect effect of medication concerns. AIDS Behav. 2020;24(1):185–191. doi:10.1007/s10461-019-02644-z
31. Logie CH, Lacombe-Duncan A, Wang Y, et al. Pathways from HIV-related stigma to antiretroviral therapy measures in the HIV care cascade for women living with HIV in Canada. J Acquired Immune Deficiency Syndromes. 2018;77(2):144. doi:10.1097/QAI.0000000000001589
32. Rueda S, Mitra S, Chen S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6(7):e011453. doi:10.1136/bmjopen-2016-011453
33. Mascayano F, Toso-Salman J, Ho YCS, et al. Including culture in programs to reduce stigma toward people with mental disorders in low-and middle-income countries. Transcult Psychiatry. 2020;57(1):140–160. doi:10.1177/1363461519890964
34. Prentice JL. The stigma of depression across cultures: the role of theory of mind. Arts; 2019
35. Mann SKF, Chong BBW. How stigma from the public and significant others affects self-perception in people with mental illness in Hong Kong: a qualitative study. Hong Kong J Soc Work. 2016;50(01n02):3–25. doi:10.1142/S0219246216000036
36. Uzorma OP, Obaghwarhievwo AJ, Ego CH, Osagie OM. Stigmatization of people living with HIV/AIDS in Ndokwa West Local Government Area of Delta State, Nigeria. Int STD Res Rev. 2020;16–29. doi:10.9734/ISRR/2020/v9i130104
37. Figueiredo Catelan R, Azevedo F, Sbicigo JB. et al. Anticipated HIV stigma and delays in HIV testing among Brazilian heterosexual male soldiers. Psychol Sexuality;2020. 1–14. 10.1080/19419899.2020.1773909
38. Sullivan MC, Rosen AO, Allen A, et al. Falling short of the First 90: HIV stigma and HIV testing research in the 90–90–90 Era. Springer; 2020.
39. Bonnington O, Wamoyi J, Ddaaki W, et al. Changing forms of HIV-related stigma along the HIV care and treatment continuum in sub-Saharan Africa: a temporal analysis. Sex Transm Infect. 2017;93(Suppl):3. doi:10.1136/sextrans-2016-052975
40. Feyissa GT, Lockwood C, Woldie M, Munn Z. Reducing HIV-related stigma and discrimination in healthcare settings: a systematic review of quantitative evidence. PLoS One. 2019;14(1):e0211298. doi:10.1371/journal.pone.0211298
41. M JV. Change in HIV-related stigma in South Africa between 2004 and 2016: a cross-sectional community study. AIDS Care. 2018;30(6):734–738. doi:10.1080/09540121.2018.1425365
42. Peltzer K, Pengpid S. Prevalence and associated factors of enacted, internalized and anticipated stigma among people living with HIV in South Africa: results of the first national survey. HIV/AIDS. 2019;11:275.
43. Stangl AL, Pliakas T, Mainga T, et al. The effect of universal testing and treatment on HIV stigma in 21 communities in Zambia and South Africa. Aids. 2020;34(14):2125–2135. doi:10.1097/QAD.0000000000002658
44. Adane B, Yalew M, Damtie Y, Kefale B. Perceived stigma and associated factors among people living with HIV attending ART clinics in public health facilities of Dessie City, Ethiopia. HIV/AIDS-Res Palliative Care. 2020;12:551–557. doi:10.2147/HIV.S274019
45. Fido NN, Aman M, Brihnu Z. HIV stigma and associated factors among antiretroviral treatment clients in Jimma town, Southwest Ethiopia. HIV/Aids. 2016;8:183.
46. Wodajo BS, Thupayagale-Tshweneagae G, Akpor OA. HIV and AIDS-related stigma and discrimination in two referral hospitals in Ethiopia. African J AIDS Res. 2017;16(2):137–144. doi:10.2989/16085906.2017.1325755
47. Subedi B, Timilsina BD, Tamrakar N. Perceived stigma among people living with HIV/AIDS in Pokhara, Nepal. HIV/AIDS. 2019;11:93.
48. Kashitala J, Nyambe N, Mwalo S, et al. Is male involvement in ANC and PMTCT associated with increased facility-based obstetric delivery in pregnant women? Afr J Reprod Health. 2015;19(2):116–123.
49. Edhs E. demographic and health survey 2016: key indicators report. DHS Program ICF. 2016;363:364.
50. Christ O, Hewstone M, Schmid K, et al. Advanced multilevel modeling for a science of groups: a short primer on multilevel structural equation modeling. Group Dyn. 2017;21(3):121. doi:10.1037/gdn0000065
51. Brault MA, Ngure K, Haley CA, et al. The introduction of new policies and strategies to reduce inequities and improve child health in Kenya: a country case study on progress in child survival, 2000-2013. PLoS One. 2017;12(8):e0181777. doi:10.1371/journal.pone.0181777
52. Muthoni C. Community stigma and discrimination against persons living with HIV/AIDS in Kenya; 2016.
53. Sambisa W, Curtis S, Mishra V. AIDS stigma as an obstacle to uptake of HIV testing: evidence from a Zimbabwean national population-based survey. AIDS Care. 2010;22(2):170–186. doi:10.1080/09540120903038374
54. Liu H, Li X, Stanton B, et al. Relation of sexual risks and prevention practices with individuals’ stigmatising beliefs towards HIV infected individuals: an exploratory study. Sex Transm Infect. 2005;81(6):511–516. doi:10.1136/sti.2005.014977
55. Rankin WW, Brennan S, Schell E, Laviwa J, Rankin SH. The stigma of being HIV-positive in Africa. PLoS Med. 2005;2(8):e247. doi:10.1371/journal.pmed.0020247
56. Koku EF. Desire for, and uptake of HIV tests by Ghanaian women: the relevance of community level stigma. J Community Health. 2011;36(2):289–299. doi:10.1007/s10900-010-9310-1
57. Chen J, Choe M, Chen S, Zhang S. The effects of individual-and community-level knowledge, beliefs, and fear on stigmatization of people living with HIV/AIDS in China. AIDS Care. 2007;19(5):666–673. doi:10.1080/09540120600988517
58. Dahlui M, Azahar N, Bulgiba A, et al. HIV/AIDS related stigma and discrimination against PLWHA in Nigerian population. PLoS One. 2015;10(12):e0143749. doi:10.1371/journal.pone.0143749
59. Perrin G. A comparative analysis of the attitudes towards people living with HIV/AIDS between Haiti and the Dominican Republic; 2010.
60. Letamo G. Prevalence of, and factors associated with, HIV/AIDS-related stigma and discriminatory attitudes in Botswana. J Health Popul Nutr. 2003;347–357.
61. Novignon J, Novignon N, Aryeetey G, Nonvignon J. HIV/AIDS-related stigma and HIV test uptake in Ghana: evidence from the 2008 demographic and Health Survey. African Popul Stud. 2014;28(3):1362–1379. doi:10.11564/0-0-626
62. Alawode OA, Arinze I, Olashore EA. Socio-demographic determinants of accepting behaviours towards HIV infected persons in Nigeria; 2018.
63. Tsai AC. Socioeconomic gradients in internalized stigma among 4314 persons with HIV in sub-Saharan Africa. AIDS Behav. 2015;19(2):270–282. doi:10.1007/s10461-014-0993-7
64. Ayranci U. AIDS knowledge and attitudes in a Turkish population: an epidemiological study. BMC Public Health. 2005;5(1):95. doi:10.1186/1471-2458-5-95
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
