Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Predictors of Diabetes Self-Care Practice Among Patients with Type 2 Diabetes in Public Hospitals in Northeastern Ethiopia: A Facility-Based Cross-Sectional Study
Authors Gulentie TM, Yesuf EM, Yazie TS , Kefale B
Received 23 July 2020
Accepted for publication 15 August 2020
Published 10 September 2020 Volume 2020:13 Pages 3137—3147
DOI https://doi.org/10.2147/DMSO.S273682
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ming-Hui Zou
Tesfaye Molla Gulentie,1 Ebrahim Mohammed Yesuf,2 Taklo Simeneh Yazie,3 Belayneh Kefale4
1Department of Drug Distribution, Pharmaceutical Fund and Supply Agency, Samara, Ethiopia; 2Department of Public Health, Samara University, Samara, Ethiopia; 3Pharmacology Unit and Research Team, Department of Pharmacy, College of Health Sciences, Debre Tabor University, Amhara, Ethiopia; 4Clinical Pharmacy Unit and Research Team, Department of Pharmacy, College of Health Sciences, Debre Tabor University, Amhara, Ethiopia
Correspondence: Belayneh Kefale
Clinical Pharmacy Unit and Research Team, Department of Pharmacy, College of Health Sciences, Debre Tabor University, PO Box 272, Debre Tabor, Amhara, Ethiopia
Tel +251 913805289/90
Email [email protected]
Objective: Even though life-threatening complications in type 2 diabetes mellitus (T2DM) minimize through self-care practice, extensive studies in northeast Ethiopia have been scarce about self-care practice and predictors. This study aimed to assess diabetes self-care predictors among patients with T2DM patients at Dubti and Assaita hospitals in northeastern Ethiopia.
Methods: A facility-based cross-sectional study was conducted among 403 patients with T2DM who followed-up in northeastern Ethiopia’s Dubti and Assaita hospitals. Data were analyzed using SPSS version-22.0 after the data were entered, sorted and cleaned. Multiple stepwise backward logistic regression analysis was done for a P value of < 0.25 to identify the independent predictors of self-care practice.
Results: In the present study, males comprised 62% of the sex category. Overall, 63.8% of the study participants had adequate self-care practice, while 36.2% had inadequate self-care practice. Being younger age (AOR 2.27, 95% CI 1.27– 4.07, P= 0.005), monthly income status with low (AOR 3.08, 95% CI 1.08– 8.78, P= 0.04), average (AOR 2.43, 95% CI 1.15– 5.09, P= 0.02) and high (AOR 2.68, 95% CI 1.03– 6.99, P= 0.04), treated with oral hypoglycemic agents (OHA) (AOR 0.22, 95% CI 0.05– 0.95, P = 0.04) and insulin (AOR 0.18, 95% CI 0.04– 0.75, P= 0.01), having social support (AOR 3.09, 95% CI 1.76– 5.4, P ≤ 0.01) and diabetic education from health professionals (AOR 5.53, 95% CI 1.92– 15.93, P= 0.001) and media (AOR 2.63, 95% CI 1.47– 4.7, P = 0.001) were the independent predictors of self-care practice.
Conclusion: In this study, the practice of self-care found to be sub-optimal among patients with T2DM. Independent predictors of self-care practice were age, monthly income, treatment regimen, social support, and diabetic education. Therefore, a suitable approach should be built to improve self-care practice with diabetes.
Keywords: type 2 diabetes mellitus, diabetes complication, diet, diet therapy
Introduction
Diabetes mellitus is a group of metabolic disorders that affect the body’s ability to process and utilize glucose for energy.1 Type 2 diabetes mellitus (T2DM) usually caused by the combination of ineffective insulin secretion and insulin resistance.1,2 It is characterized by hyperglycemia and is associated with macrovascular, microvascular, and neuropathic complications and needs continuous medical treatment.3,4 These complications may result in poor quality of life, increased disability, and decreased productivity, decreased economic growth and life expectancy, and increased risk of morbidity and mortality due to poor self-care practice.5–7
Globally, Diabetes is one of the main causes of 21st-century morbidity and mortality and poses a threat to the health care system. Worldwide, there were 422 million people with diabetes and 4.6 million deaths in 2011, according to the World Health Organization (WHO) 2014 report8 and in developing countries, including Ethiopia, about 66% of the diabetic population lives.8,9 Based on the International Diabetes Federation (IDF) 2019 survey, the number of people with diabetes in Ethiopia was estimated at 1.7 million.10 Inadequate self-care education in patients with diabetes raises complications incidence, leading to increased morbidity and mortality.11,12 A research performed by Casagrande et al found that glycemic regulation is sub-optimal in T2DM, with only around 53% of patients meeting glycemic targets with their current care regimen.13 This low glycemic control can be increased throughout developing countries because of insufficient access to anti-diabetic drugs and technologies.14
Patients with diabetes need to perform various self-care practices recommended by the WHO, including a healthy diet, daily physical workouts, adherence to medication, and regulation of foot care control to avoid complications related to diabetes.15 Self-monitoring of blood glucose (SMBG) recommended for patients receiving insulin, and to have an action plan with their health care provider on how to tailor adjust insulin dosage, food consumption, and physical activity according to their blood glucose levels.16,17 Implementing of the prescribed self-care protocol in patients with T2DM is considered to avoid multiple complications due to uncontrolled glycaemia.18 Therefore, self-care activities are essential for all patients with T2DM to monitor the disease process, prevent complications, and manage glycemic that improve quality of life.19 However, in patients with T2DM, self-care practice involves coordination between the patient and the care provider. Inadequate facilities, and lack of resources for diabetes mellitus education in developing countries, especially Ethiopia, are the key challenges to achieving the recommended self-care practices.4,16 Globally, multiple studies have shown that diabetes self-care activities are sub-optimal. Close to one-third of patients with T2DM in the US have insufficient self-care procedures.20 Qualitative research in Addis Ababa found that the general standard of self-care was inadequate.5 On the other hand, longitudinal studies among diabetic patients in Ethiopia have shown that self-care activities vary from 44% to 65%.7,14,21-23 Specific socio-demographic, clinical characteristics and unequal distribution of health care professional between urban and rural areas are the key factors that limit glycemic control practices in developing countries.6,22-24 While great strides have been made in the treatment of diabetes over the past few decades, many patients have achieved sub-optimal results and encountered numerous complications due to insufficient self-care practice. Comprehensive researches have been scarce in the study settings. Therefore, this study’s goal was to assess predictors of diabetes self-care practices among patients with T2DM at referral hospitals in Dubti and Assaita in North-east Ethiopia.
Methods
Study Design and Period
The facility-based cross-sectional study design was conducted among patients with T2DM. They were on follow up at referral hospitals in Dubti and Assaita in northeastern Ethiopia to determine predictors of self-care practice. Dubti and Assaita referral hospitals in the Afar district, northeast Ethiopia, serve over 3 million people living in the catchment area. Based on eligibility criteria, four hundred three (403) patients with T2DM, who are on follow up and come to Dubti (213) and Assaita (190) referral hospitals during the study period were included. The data were collected from March through May 2019.
Eligibility Criteria
The study includes all adult patients (≥18 years) with T2DM who were on follow up at Dubti and Assaita referral hospitals from March to May 2019. Nevertheless, the study omitted people with T2DM, who are refused to participate and with cognitive impairment (Figure 1).
 |
Figure 1 Schematic presentation of sampling. |
Data Collection Instrument and Procedure
Structured questionnaires were adapted from various related literature and used to collect the data. The main components of the questionnaire were socio-demographic traits, self-care practices, and certain determinant factors such as social support, diabetes knowledge, and being a member of the association for diabetes. It was written in English and translated to Amharic afterward. The questionnaire was retranslated to English by an expert in the Amharic language to test its consistency. After a comprehensive review, the final version of the questionnaire was developed and pretested in patients with T2DM by 5%. Five volunteer and trained nurses were hired, and they participated in data collection. The training on data collection was structured and provided about the research purpose correct use of the data collection instruments, questionnaire materials, strict use of study requirements and obtaining verbal consent from study participants and ways of preserving confidentiality and privacy, and methods for solving problems. Participants with a value above mean score of self-care-related questions, knowledge-related questions, and social support-related questions were considered to have adequate self-care practice, knowledge, and social support, respectively. Concerning adherence, a participant deemed to be adherent for diet, SMBG, exercise, and medication when he/she followed the recommended diet, level of SMBG, level of exercise and amount of drug to take for more than 3, 2, 2 and 6 days in the last 7 days, respectively.
Data Processing and Analysis
The data collected were marked, entered, and cleaned using EPI-Data version 3.02 and SPSS v 22. For review, the data was exported to SPSS package version 22. Descriptive statistics such as frequency, percentage, and mean with standard deviations were used to describe the independent variables. Multiple stepwise backward logistic regression analysis was done for a P value of < 0.25 to identify the independent predictors of self-care practice. Statistical significance was set at p<0.05.
Ethical Consideration
Ethical clearance and approval of the study protocols have been received from the Samara University, College of Medicine and Health Sciences Ethical Review Board (SUU/RE/1/170/12). Additionally, permission for conducting the study was obtained from the respective responsible hospital body. Verbal informed consent was approved by the Samara University, College of Medicine and Health Sciences Ethical Review Board, and that this study was conducted in accordance with the Declaration of Helsinki.
Patient and Public Involvement
Patients were not involved in the design and conduction of this study. Patients were not invited to comment on the study design and were not consulted to develop patient-relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Results
Socio-Demographic Characteristics
In this study, a total of 403 type 2 diabetes mellitus patients were included. The majority of the study participants (250, 62%) were males. The mean age of the patients was 46.7±11.3, and the mean age in which diabetes diagnosed was found to be 36.7±11.02 years. Education-wise, 127 (31.5%) and 122 (30.3%) of study participants had no formal education and attended college/university education level, respectively. Occupationally, the majority (52.6%) of participants in the study were government employed. A significant proportion of the study participants (45.9%) had an average monthly family income (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Type 2 Diabetes Patients in Dubti and Assaita Hospitals, Northeast Ethiopia, 2019 |
Disease-Related Characteristics
The mean duration of diabetes was 10.26±6.94years. More than two-thirds of the study participants (287, 71.2%) did not have a family history of diabetes, and 243 (60.3%) participants had oral hypoglycemic agents. About 87 (21.6%) and 11 (2.7%) study participants had hypertension, kidney-related problems, respectively (Table 2).
 |
Table 2 Disease-Related Characteristics of Type 2 Diabetes Patients in Dubti and Assaita Hospitals, Northeast Ethiopia, 2019 |
Self-Care Practices
About two-third (276, 68.5%) and (249, 61.8%) of study participants were not adhered to recommended diet management and SMBG practice, respectively. 243 (60.3%) and 161 (40%) participants were adhered to any physical activity and regular exercise that met the recommended guidelines, respectively. Around half (212, 52.6%) of study participants adhered to the recommended diabetic foot care practices. Remarkable participants (378, 93.8%) adhered to anti-diabetic medications. Overall, self-care practice was found to be 63.8% (Figure 2).
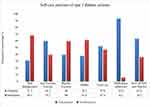 |
Figure 2 Overall self-care practice among the study participants. |
Diabetes Knowledge, Social Support and Other Related Factors
Of all participants, 232 (57.6%) were knowledgeable, and 252 (62.5%) had social support. Among participants, 230 (57.1%) were members of the Ethiopian Diabetic Association, and only 48 (11.9%) and 65 (16.2%) always attended diabetes education given by the association and health professionals, respectively (Table 3).
 |
Table 3 Diabetes Knowledge, Social Support and Other Related Factors of Type 2 Diabetes Patients in Dubti and Assaita Hospitals, Northeast Ethiopia, 2019 |
Factors Associated with Self-Care Practice
During bivariate analysis, socio-demographic variables such as age, educational status, monthly family income status, duration of diabetes mellitus, treatment intensity, diabetic knowledge, social support and diabetic education from health professionals and media showed significant association at p<0.25 and were a candidate for multivariate logistic regression analysis (Table 4).
 |
Table 4 Univariate Binary Logistic Regression Analysis of Predictors of Self-Care Practice |
In the multivariate logistic regression analysis, only age, income status, treatment regimen, social support, and diabetic education were the independent predictors of self-care practice. In this study, younger patients (≤50 years) were two (AOR= 2.27, 95% CI 1.27–4.07, p=0.005) times more likely to have adequate self-care practice as compared to their counterparts. Additionally, patients who had low, average and high monthly family income were about three (AOR=3.08, 95% CI: 1.08–8.78, p=0.04), two (AOR=2.43, 95% CI: 1.15–5.09, p=0.02) and three (AOR=2.68, 95% CI: 1.03–6.99, p=0.04) times, respectively, more likely to have adequate self-care practice as compared to those who had very low monthly family income. On the other hand, patients who were prescribed with OHA and insulin injection were 0.78 (AOR= 0.22, 95% CI: 0.05–0.95, p=0.04), 0.82 (AOR= 0.18, 95% CI: 0.04–0.75, p=0.01), times less likely to have adequate self-care practice compared to those prescribed with dual treatment regimen (OHA and Insulin). Patients with social support were three (AOR= 3.09, 95% CI: 1.76–5.4, p<0.01) times more likely to have adequate self-care practice than their counterparts. Furthermore, statistically significant associations were observed between self-care practice and received health education from health professionals and media. Patients received health education from health professionals, and media were six (AOR=5.53, 95% CI 1.92–15.93, P=0.001), three (AOR=2.63, 95% CI 1.47–4.70, p=0.001) times more likely to have adequate self-care practice (Table 5).
 |
Table 5 Multivariate Binary Logistic Regression Analysis of Predictors of Self-Care Practice |
Discussion
The present study was conducted in Dubti and Asayita referral hospitals to identify predictors of diabetes self-care practice among patients with type 2 diabetes. The study shows that 63.8% of adequate self-care practices were found, consistent with other research by Dedefo et al 60.7%,24 Mamo et al 60.3%.7 However, this finding is higher than studies done in Bahir Dar 28.4%,6 University of Gondar 48.14%,25 Jimma 50.9%,22 Addis Ababa 51.5%,26 Nekemte 54.7%,27 Mekelle 51%,28 Iran 36.4%29 and India 49.5%,30 Palestine 52%.31 This discrepancy may be due to the study participants’ differences in population source, sample size, diabetic awareness, socio-economic status, cultural variability, and lifestyle in the study mentioned above settings. Nearly half of the patients in our study had insufficient knowledge of diabetes and self-care habits, resulting in ineffective self-care behaviors on physical activity, a balanced diet after prescribed treatment, self-monitoring of blood glucose level, and foot care.
This study also found that OHA was being taken by 60.3% of the study participants. In comparison, previous studies conducted at Mekelle28 and Addis Ababa7 found that insulin was taken by 58.7% and 65.6%, respectively. This vice versa trend may be attributed to environmental factors rendering insulin shelf life compromised, further leading to poor patient compliance and choosing OHA in the current study over insulin injection.
With respect to adherence to medication, their prescription was adhered to by 93.8% of study participants. This result is in line with other earlier related studies at 91.7% in Addis Ababa and 95% in South India and higher than studies at 70.4% in Harar and 63.7% in Mangalore Karnataka.7,32-34 This variability may be due to variations between studies in the concept of adherence to the drug. Therefore, methodologies will vary between studies, leading to data variation, and socio-demographic and economic characteristics of the participants in the research may contribute to this variation.
On the other hand, diet control, daily exercise, and SMBG were recorded as 31.5%, 40%, and 38.2%, respectively, consistent with previous studies in the Warangal region of India and Jimma Western Ethiopia.23,35 Contrastingly, this finding is higher than the Addis Ababa diet control report, 15.4%, 7% daily exercise, and 29% SMBG.7 This disparity may likely have to do with the available transportation and socio-economic gap. Study participants in our study setting usually went to the health facility on bare feet, and socio-economic disparity and fear complications related to Diabetes made them stick health care diet management advice from health professionals and purchasing the device and its strips for SMBG.
Self-care practice on the examination of independent variables was found to be statistically associated with age, monthly income level, treatment regimen, social support, and diabetic education. This study found that younger patients (≤50 years) had a more fabulous experience of self-care for diabetes, which is consistent with a study done in Nekemte.27 Furthermore, monthly family income was significantly related to self-care practice as the monthly family income rose; study participants were found to be more likely to practice self-care. Similarly, our result is backed by previous studies performed in Nekemte and Tamil Nadu.27,36 Income status has been implicated in self-care practice in several studies of diabetic patients. Besides, the low socio-economic status of diabetes patients was significantly associated with medication non-adherence.37 Many diabetic patients in developing countries do not have access to health insurance and other essential items for self-care practice, making diabetes inexpensive and challenging.
Our study also showed that participants who took insulin or OHA agents were less likely than those who took insulin and OHA combinations to do self-care practice. Studies in Ethiopia and Turkey, on the other hand, found that patients who received one single treatment were more likely to conduct self-care than those who received combination treatment.23,38,39 In the present study, the comparatively better self-care score among combined drug users may be explained as diabetic patients may have an uncontrolled glycemic level with single-drug therapy and may have severe health issues needing special attention, and may have regular interaction with health care professionals and better family and friend’s social help.
Study participants who obtained guidance from health professionals and media were more likely to conduct self-care practice concerning diabetes awareness than their peers. This finding is consistent with other studies conducted by Amente et al7 and Ayele et al.40 They reported that patients with more frequent information were more likely to have good self-care practices than those with less common knowledge about their disease. Furthermore, the patient’s preference for media education over leaflet (written material) may be due to the diabetes association’s inaccessibility, and therefore, patients may not have access to leaflet education. Due to sensitive and personal issues related to diabetic self-care, social desirability bias may also lead to insufficient self-care practice, for example, financial related concerns. Besides, patients with T2DM having social support were more likely to practice self-care than their counterparts, which is equivalent to an Addis Ababa study.7 It is believed because social support from family, friends, and others was critical in worrying, empowering, and helping patients with diabetes practice self-care.
Participants with adequate self-care found to be suboptimal; the diabetic education program at the hospital and community level is recommended to create awareness and improve self–care practices. In the future, a large scale and longitudinal study suggested finding more predictors of self-care practices and monitoring behavioral changes towards self-care practices.
Limitations of the Study
There were other drawbacks to our study. Because of the cross-sectional study nature, a causal link cannot be established. Therefore, the research sample size is small; it may be challenging to identify any possible self-care practice predictors. The interview used to evaluate the practice self-care may underestimate the status of the practice of self-care patients. Therefore, longitudinal research should be performed to examine possible predictors for insufficient self-care practices with Diabetes, taking qualitative evaluations into account.
Conclusion
Adequate self-care practice was found to be 63.8%. Approximately two-thirds of study participants failed to follow the recommended diet management and SMBG practice. Nearly half the participants in the study had an insufficient understanding of diabetes and its self-care activities. The independent predictors of self-care practice have been age, monthly income, treatment regimen, social support, and diabetic education were the independent predictors of self-care practice. Developing diabetes approaches capable of strengthening self-care behaviors is key to addressing diabetes-related risks and mortality. The evidence available indicates community outreach and awareness building are successful in enhancing self-care practice. Therefore, programs on diabetic education at the community and hospital level will be structured to monitor contributing factors and behavioral changes.
Abbreviations
AOR, Adjusted odds ratio; IDF, International diabetes federation; OHA, Oral hypoglycemic agents; SMBG, Self-monitoring blood glucose; SPSS, Statistical package for social science; WHO, World health organization.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
Ethical approval was obtained from ethical review board of Samara University, College of Medicine and Health Sciences (SUU/RE/1/170/12).
Acknowledgments
We would like to acknowledge Dubti and Assaita referral hospital staff and data abstractors for their valuable contribution to this project.
Author Contributions
All authors contributed to conceptualization and design data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors have declared that no competing interests exist for this work.
References
1. Definition WH. Diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. Geneva: World Health Organization; 2006:1–50.
2. Hall V, Thomsen RW, Henriksen O, Lohse N. Diabetes in Sub Saharan Africa 1999–2011: epidemiology and public health implications. A systematic review. BMC Public Health. 2011;11(1):564. doi:10.1186/1471-2458-11-564
3. Cha S-A, Yun J-S, Lim T-S, et al. Severe hypoglycemia and cardiovascular or all-cause mortality in patients with type 2 diabetes. Diabetes Metab J. 2016;40(3):202–210. doi:10.4093/dmj.2016.40.3.202
4. Park PH, Wambui CK, Atieno S, et al. Improving diabetes management and cardiovascular risk factors through peer-led self-management support groups in Western Kenya. Diabetes Care. 2015;38(8):e110–e1. doi:10.2337/dc15-0353
5. Tewahido D, Berhane Y. Self-care practices among diabetes patients in Addis Ababa: a qualitative study. PLoS One. 2017;12(1):e0169062. doi:10.1371/journal.pone.0169062
6. Abate TW, Tareke M, Tirfie M. Self-care practices and associated factors among diabetes patients attending the outpatient department in Bahir Dar, Northwest Ethiopia. BMC Res Notes. 2018;11(1):800. doi:10.1186/s13104-018-3874-8
7. Mamo M, Demissie M. Self care practice and its associated factors among diabetic patients in Addisababa public hospitals, cross sectional study. Diabetes cholest metabol 1: 101. Diabetes Cholest Metabol. 2016;1(1):2–5.
8. Organization WH. Global status report on noncommunicable diseases 2014. World Health Organization; 2014.
9. Chaurasia B, Summers SA. Ceramides–lipotoxic inducers of metabolic disorders. Trends Endocrinol Metab. 2015;26(10):538–550. doi:10.1016/j.tem.2015.07.006
10. IDF G. ISPAD guideline for diabetes in childhood and adolescence. International diabetes federation; 2011:131.
11. Abebaw M, Messele A, Hailu M, Zewdu F. Adherence and associated factors towards antidiabetic medication among type II diabetic patients on follow-up at University of Gondar Hospital, Northwest Ethiopia. Adv Nurs. 2016;2016:1–7. doi:10.1155/2016/8579157
12. Association AD. Standards of medical care in diabetes–2014. Diabetes Care. 2014;37:S14. doi:10.2337/dc14-S014
13. Casagrande SS, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care. 2013;36(8):2271–2279. doi:10.2337/dc12-2258
14. Chali SW, Salih MH, Abate AT. Self-care practice and associated factors among diabetes mellitus patients on follow up in Benishangul Gumuz regional state public hospitals, Western Ethiopia: a cross-sectional study. BMC Res Notes. 2018;11(1):833. doi:10.1186/s13104-018-3939-8
15. Murri M, Insenser M, Bernal-Lopez MR, Perez-Martinez P, Escobar-Morreale HF, Tinahones FJ. Proteomic analysis of visceral adipose tissue in pre-obese patients with type 2 diabetes. Mol Cell Endocrinol. 2013;376(1–2):99–106. doi:10.1016/j.mce.2013.06.010
16. Mbanya JCN, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-saharan africa. Lancet. 2010;375(9733):2254–2266. doi:10.1016/S0140-6736(10)60550-8
17. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi:10.1016/j.diabres.2009.10.007
18. Bommer C, Heesemann E, Sagalova V, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5(6):423–430. doi:10.1016/S2213-8587(17)30097-9
19. Norris SL, Nichols PJ, Caspersen CJ, et al. The effectiveness of disease and case management for people with diabetes: a systematic review. Am J Prev Med. 2002;22(4):15–38. doi:10.1016/S0749-3797(02)00423-3
20. Gunggu A, Thon CC, Whye Lian C. Predictors of diabetes self-management among type 2 diabetes patients. J Diabetes Res. 2016;2016:1–7. doi:10.1155/2016/9158943
21. Ketema DB, Leshargie CT, Kibret GD, et al. Level of self-care practice among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):1–12. doi:10.1186/s12889-020-8425-2
22. Kassahun T, Gesesew H, Mwanri L, Eshetie T. Diabetes related knowledge, self-care behaviours and adherence to medications among diabetic patients in Southwest Ethiopia: a cross-sectional survey. BMC Endocr Disord. 2016;16(1):28. doi:10.1186/s12902-016-0114-x
23. Hailu E, Mariam WH, Belachew T, Birhanu Z. Self-care practice and glycaemic control amongst adults with diabetes at the Jimma University Specialized Hospital in south-west Ethiopia: a cross-sectional study. Afr J Prim Health Care Fam Med. 2012;4(1). doi:10.4102/phcfm.v4i1.311
24. Dedefo MG, Ejeta BM, Wakjira GB, Mekonen GF, Labata BG. Self-care practices regarding diabetes among diabetic patients in West Ethiopia. BMC Res Notes. 2019;12(1):212. doi:10.1186/s13104-019-4258-4
25. Aschalew AY, Yitayal M, Minyihun A, Bisetegn TA. Self-care practice and associated factors among patients with diabetes mellitus on follow up at University of Gondar referral hospital, Gondar, Northwest Ethiopia. BMC Res Notes. 2019;12(1):591. doi:10.1186/s13104-019-4630-4
26. Lemessa F Assessment of self care practices and associated factors among type 2 diabetic patients at Tikur Anbessa specialized hospital Addis Ababa, Ethiopia: Addis Ababa University; 2014.
27. Amente T, Belachew T, Hailu E, Berhanu N. Self care practice and its predictors among adults with diabetes mellitus on follow up at Nekemte hospital diabetic clinic, West Ethiopia. World J Med Med Sci. 2014;2(3):1–16.
28. Berhe KK, Gebru HB, Kahsay HB, Kahsay AA. Assessment of self care management and its associated factors among type 2 diabetes patients in Mekelle hospital and Ayder referral hospitals, Mekelle City, Tigray, Northern Ethiopia, 2012/13. Glob J Med Res. 2017;17:2249–4618.
29. Nejaddadgar N, Solhi M, Jegarghosheh S, Abolfathi M, Ashtarian H. Self-care and related factors in patients with type 2 diabetes. Asian J Biomed Pharm Sci. 2017;7(61):6–10.
30. Suguna A, Magal A, Stany A, Sulekha T, Prethesh K. Evaluation of self-care practices among diabetic patients in a rural area of Bangalore district, India. Int J Curr Res Aca Rev. 2015;3(6):415–422.
31. Mosleh RSA, Jarrar YB, Zyoud S, Morisky DE. Factors related to diabetes self-care management behaviors among patients with type II diabetes in Palestine. J Appl Pharm Sci. 2017;7(12):102–109.
32. Rajasekharan D, Kulkarni V, Unnikrishnan B, Kumar N, Holla R, Thapar R. Self care activities among patients with diabetes attending a tertiary care hospital in Mangalore Karnataka, India. Ann Med Health Sci Res. 2015;5(1):59–64. doi:10.4103/2141-9248.149791
33. Selvaraj K, Ramaswamy G, Radhakrishnan S, Thekkur P, Chinnakali P, Roy G. Self-care practices among diabetes patients registered in a chronic disease clinic in Puducherry, South India. J Soc Health Diabetes. 2016;4(1):25–29. doi:10.4103/2321-0656.176572
34. Ahmed O, Abdela J, Sisay M. Lifestyle modification: knowledge, attitude and practice among diabetic patients having chronic follow up in hiwot fana specialized university hospital, eastern Ethiopia. J Pharm Res. 2016;6(12).
35. Thungathurthi S, Thungathurthi S, Kumar V. Self care knowledge on diabetes among diabetic patients in Warangal region. Int J Life Sci Pharma Res. 2012;2(2):16–21.
36. Shrivastava P, Shrivastava S, Ramasamy J. An epidemiological study to assess the knowledge and self care practices among type 2 diabetes mellitus patients residing in rural areas of Tamil Nadu. Biol Med S. 2015;3:002.
37. Gelaw BK, Mohammed A, Tegegne GT, et al. Nonadherence and contributing factors among ambulatory patients with antidiabetic medications in Adama Referral Hospital. J Diabetes Res. 2014;2014:1–9. doi:10.1155/2014/617041
38. Kassahun T, Eshetie T, Gesesew H. Factors associated with glycemic control among adult patients with type 2 diabetes mellitus: a cross-sectional survey in Ethiopia. BMC Res Notes. 2016;9(1):78. doi:10.1186/s13104-016-1896-7
39. Kayar Y, Ilhan A, Kayar NB, et al. Relationship between the poor glycemic control and risk factors, life style and complications. 2017.
40. Ayele K, Bisrat Tesfa LA, Tilahun T, Girma E. Self-care behavior among patients with diabetes in Harari, Eastern Ethiopia: the health belief model perspective. PloS one. 2012;7(4).
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
