Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Predictive Value of Noninvasive Peripheral Atherosclerosis Measurement for Coronary Artery Disease in Patients with Long T2DM Duration
Authors Chen W, Wang L, Hu B, Zheng Y, Zhang S, Zhou Z, Mai Y
Received 16 January 2023
Accepted for publication 22 March 2023
Published 18 April 2023 Volume 2023:16 Pages 1075—1083
DOI https://doi.org/10.2147/DMSO.S404937
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Konstantinos Tziomalos
Wanjiao Chen,1 Li Wang,1 Bin Hu,1 Ying Zheng,1 Shuya Zhang,1 Zhong Zhou,2 Yifeng Mai2
1Health Science Center, Ningbo University, Ningbo, 315020 People’s Republic of China; 2The First Affiliated Hospital of Ningbo University, Ningbo, 315020, People’s Republic of China
Correspondence: Zhong Zhou; Yifeng Mai, The First Affiliated Hospital of Ningbo University, 247 Renmin Road, Jiangbei District, Ningbo, Zhejiang Province, 315020, People’s Republic of China, Tel +8613736099999, Email [email protected]; [email protected]
Objective: This study aimed to compare the predictive value of carotid or femoral artery ultrasound for coronary artery disease (CAD) in type 2 Diabetes mellitus (T2DM) patients free from known CAD, and to assess the relationship with the severity of coronary artery stenosis.
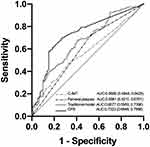
Methods: Cross-sectional study in adults with a T2DM duration of at least 5 years and without established CAD. Carotid plaque score (CPS) and Gensini score were used to measure the severity of carotid and coronary artery stenosis, respectively, and patients were divided into no or mild group, moderate group, and severe group according to the tertile of the score. Univariate and multivariate logistic regression analysis was used to explore the possible risk factors for CAD. Receiver operating characteristic (ROC) curves were created to determine the most accurate assessment for detecting significant CAD (≥ 50% stenosis).
Results: 245 patients (137 male) aged 68.21± 9.5 years (range: 36– 95 years), with T2DM duration 12.04± 6.17 years (range: 5– 34 years), and without CVD were included. CAD was diagnosed in 165 patients (67.3%). Multiple regression analysis showed that CPS, femoral plaque, and smoking were independently and positively correlated with CAD. CPS yielded the highest area under the curve for detecting significant coronary disease (AUC=0.7323). In contrast, the area under the curve of femoral artery plaque and carotid intima-media thickness was lower than 0.7, which was at a lower prediction level.
Conclusion: In patients with long T2DM duration, CPS has a higher ability to predict the occurrence and severity of CAD. However, femoral artery plaque has special value in predicting moderate to severe coronary artery disease in patients with long-term T2DM.
Keywords: peripheral atherosclerosis, coronary artery disease, type 2 diabetes mellitus, Gensini score, carotid plaque score, femoral artery plaque
Introduction
The prevalence of diabetes mellitus in the world continues to rise, and in countries such as China, the proportion has risen to 10% of the population.1 By 2045, there will be more than 600 million people suffering from type 2 diabetes mellitus (T2DM) in the world. A meta-analysis of 102 prospective studies showed that diabetes increased the risk of multiple vascular diseases by about two times, independent of other conventional risk factors.2 The hormonal and physiological abnormalities associated with diabetes, including oxidative stress, insulin resistance, reactive oxygen generation, advanced glycation end products, and increased inflammatory cytokine production, jointly promote the occurrence of vascular complications.3–5 T2DM is not only associated with the early onset of atherosclerotic cardiovascular disease (ASCVD),6,7 but also with the severity8 and poor prognosis of ASCVD.9 Diabetes mellitus was previously regarded as a “CAD risk equivalent”.10 However, many studies, including meta-analysis, have reached different conclusions, indicating that although diabetes is an important risk factor for the development of cardiovascular disease (CVD), it cannot be regarded as the “CAD risk equivalent” of all diabetes patients.11,12 That is, T2DM patients may have a heterogeneous risk for CVD, so further stratification of patients improves the accuracy of subclinical CAD and future CVD predictions.
Although various non-invasive methods, which can be used to detect the presence and severity of extracoronary atherosclerotic disease, are commonly used to estimate cardiovascular risk in real clinical practice.8,13,14 The usefulness of systematic CVD screening in asymptomatic patients with T2DM for cardiovascular risk reclassification remains controversial, and most guidelines do not recommend routine evaluation in asymptomatic patients due to the ultimate balance of benefits, costs, and risks.15 Therefore, we reappraised several noninvasive measures of peripheral atherosclerosis and their predictive value in the presence and severity of coronary artery disease in long-term T2DM patients. To the best of our knowledge, there have been no studies on the predictive value of various noninvasive peripheral atherosclerosis measures for coronary atherosclerosis in this specific population.
Materials and Methods
Study Population
Patients with T2DM who underwent first coronary angiography and carotid ultrasound and lower extremity vascular ultrasound in the Affiliated Hospital of Medical School, Ningbo University from January 2020 to June 2022 were retrospectively enrolled in this study. T2DM was defined according to the current American Diabetes Association guidelines.16 Inclusion criteria were age≥18 years, T2DM duration≥5 years and absence of known CAD (ie, no history of angina pectoris, acute coronary syndrome). This study was approved by the medical ethics committee of Affiliated Hospital of Medical College of Ningbo University and was performed following the Declaration of Helsinki guidelines, including any relevant details. Due to the retrospective nature of the study, the requirement for informed consent was waived.
Clinical Characteristics and Laboratory Data
Clinical data were obtained from the electronic medical record system during the hospital stay in which coronary angiography was performed. Weight and height were measured using a standardized approach, followed by the calculation of body mass index (BMI) in kg/m2. Blood pressure was obtained as the mean of 3 consecutive measurements with an OMRON M10-IT automatic oscillometric sphygmomanometer (OMRON Healthcare Co. Ltd., Kyoto, Japan), with the individuals resting in a seated position for 5 min between readings. Use of antihypertensive medication or average blood pressure levels greater or equal to 140/90 mmHg defined the presence of arterial hypertension according to the latest ESH/ESC guidelines.17 Blood samples were collected between 8.00 and 10.00 a.m. after an overnight (>8 h) fast were processed for laboratory analyses the same day. Fasting serum glucose, triglycerides (TG), total cholesterol (TC), and high-density lipoprotein cholesterol (HDL-C) were measured by spectrophotometry. Low-density lipoprotein cholesterol (LDL-C) was calculated. Current smoking was defined as smoking in the present or having smoked in the last year. Being a former smoker was defined as a subject having smoked at least 50 cigarettes in his lifetime, but not having smoked in the last year.
Femoral and Carotid Atherosclerosis Assessment by Ultrasound and Carotid Plaque Score
Femoral and carotid ultrasound was conducted by an experienced imaging technician within 7days of coronary angiography. The sonographer and the interpreting cardiologist were blinded to the angiographic findings. The maximum distal common carotid intima-media thickness (C-IMT) was determined and the average of left and right maximum common C-IMT was computed. Plaque was defined using the Mannheim criteria as a focal structure that protruded into the arterial lumen by 50% of the surrounding intima-media thickness or that was≥1.5 mm in thickness from the media-adventitia border to the intima-lumen border.18 In all cases, plaques were recorded in both longitudinal and transverse planes to account for circumferential asymmetry.
We also measured the carotid plaque score (CPS) for the common and internal carotid arteries.8 The CPS was computed by adding the maximal thickness in millimeters of plaques in each segment on both sides (A + B + C + thickness of the contralateral carotid artery plaques) (Figure 1). Segment 1 (S1) was the region of the internal carotid arteries (ICA) that was <15 mm distal to its bifurcation from common carotid artery (CCA). Segment 2 (S2) was the region of the ICA and the CCA that was <15 mm proximal to the bifurcation. Segment 3 (S3) was the region of the CCA that was >15 mm and <30 mm proximal to the bifurcation. The length of individual plaques was not considered in determining the CPS (Figure 1).
 |
Figure 1 The measurement of the carotid plaque score. Abbreviations: BIF, bifurcation; CCA, common carotid artery; ECA, external carotid artery; ICA, internal carotid artery. |
The Gensini Score and Angiographic Analysis
Two of the five experienced physicians evaluated the patient’s coronary condition according to the guidelines for coronary angiography of the American College of Cardiology and the American Heart Association.19,20 Due to the inability to accurately obtain collateral adjustment factors from the available data, the modified Gensini score (GS) system was used to measure CAD severity.21 These scores were expressed as the sum of the positional score of each lesion multiplied by the obstruction severity score, which emphasizes the severity of the disease. The calculation of the modified Gensini score system is shown in Table 1. The lesion score of each segment was calculated as stenosis score × weight coefficient. The cumulative score of each segment lesion was the total score of the degree of coronary artery lesion of the patient.
 |
Table 1 Modified Gensini Score System |
Statistical Analysis
All statistical analyses were performed using SPSS 26.0 for Mac (IBM Corp., Armonk, New York, USA) and GraphPad Prism version 9.0 for Mac (GraphPad Software, San Diego, California, USA). Data were checked for normality with the Kolmogorov–Smirnov test as well as visually by Q–Q plots and shown as mean± SD or median [P25-P75] depending on the distribution. Categorical variables are displayed as percentages and absolute numbers. Independent samples t-test and one-way ANOVA were used to compare normally distributed continuous variables between two or more independent groups, respectively. Homogeneity of variance was evaluated by Levene’s test. For comparisons of non-normally distributed variables between two or more groups, the non-parametric Mann–Whitney U-test and Kruskal–Wallis test were used, respectively. Post-hoc testing with Bonferroni correction (parametric) or the Dunn’s test (non-parametric) was used for multiple comparisons. Categorical variables were compared using the chi- squared. Univariate and multivariate logistic regression analysis was used to explore the possible risk factors for CAD. Receiver operating characteristic (ROC) curves were created to determine the most accurate assessment for detecting significant CAD (≥50% stenosis). Weighted Youden indices were used to determine optimal threshold values for identifying significant CAD. Level of significance was set at p<0.05.
Results
Study Population Characteristics
Characteristics of the examined population are displayed in Table 2. 245 patients (137 male) aged 68.21±9.5 years (range: 36–95 years), with T2DM duration 12.04± 6.17 years (range: 5–34 years) were included. CAD was diagnosed in 165 patients (67.3%). Those with CAD were more often smoking, had femoral artery plaque, and had higher CPS and Gensini score, compared to those without CAD (p<0.05). In addition, compared with non-CAD patients, CAD patients tended to be older, have a longer duration of T2DM, higher total cholesterol, lower HDL-C and higher C-IMT values, but the differences were not statistically significant (p>0.05). However, there were no differences in gender, BMI, hypertension, fasting blood glucose, triglyceride, or LDL-C between participants with or without CAD (p>0.05).
 |
Table 2 Patient Characteristics |
Risk Factors of Coronary Artery Disease
To further explore the possible risk factors for coronary artery stenosis, univariate and multivariate logistic regression analyses were applied (Table 3). Univariate logistic regression analyses showed that risk factors associated with CAD included smoking, femoral plaques, C-IMT and CPS (all p<0.05). Additionally, after adjusting for all traditional risk covariates, multiple regression analyses showed that smoking, femoral plaques, and CPS significantly correlated with CAD.
 |
Table 3 Logistic Regression Analysis of Factors Associated with the Presence of CAD |
Predictive Values of Arterial Measures for CAD
To better evaluate the predictive value of peripheral arterial measurements for CAD, we developed a traditional model that included all covariates: gender, age, BMI, alcohol consumption history, mean systolic and diastolic blood pressure, TG, TC, HDL-C, LDL-C, fasting blood glucose, duration of diabetes, hypertension, and smoking status. The ROC area under the curve (AUC) curve for identifying CAD were compared between traditional model, femoral plaques, C-IMT, and CPS measurements (Figure 2). Carotid plaque score yielded the highest AUC for identifying participants with CAD (AUC=0.7323), higher than the traditional model (AUC=0.6677). The AUC values of femoral artery plaque and C-IMT for CAD prediction were comparable and lower than 0.7, which was at a low level.
The ROC analysis displayed that the cut-off value of CPS was 2.45, 61.82% of sensitivity, 81.25% of Specificity and 0.4307 of Yoden index could predict CAD, and the area under the ROC curve was 0.7323 (95% CI 0.665–0.8, p<0.001, Figure 2).
Associations of Peripheral Atherosclerosis Measurement with the Severity of CAD
For analyze the relationship between carotid plaque score, femoral plaque and CAD severity, patients were further divided into three subgroups according to the tertiles of Gensini score, including no or mild (n=73), moderate (n=89) and severe (n=83). Calculated CPS values had significant difference among three groups with the increasing of Gensini score, 0 [0–2.1] for no or mild group, 2.1 [0–4.4] for the moderate group and 4.7 [2.8–6.6] for the severe group, expressed as the median [25–75%] (Figure 3A). Moderate group and severe group of CPS calculation value was significantly higher than no or mild group (adjusted p<0.05 and adjusted p<0.001, respectively). Compared with the moderate group, the calculated CPS values of the severe group were significantly higher (adjusted p<0.001) (Figure 3A).
The mean C-IMT values were 0.8 [0.75–0.9] for no or mild group, 0.8 [0.8–1.1] for the moderate group and 0.9 [0.8–1.1] for the severe group, respectively, expressed as the median [25–75%] (Figure 3B). Figure 3B indicate that the mean C-IMT among the three groups grouped according to CAD severity, only the difference between no or mild group and severe group was statistically significant (adjusted p<0.001).
As shown in Figure 3C, with the increasing of Gensini score, a stepwise upward trend was observed in the proportion of femoral plaque, 42.5% for no or mild group, 71.9% for the moderate group and 79.5%for the severe group. The differences between no or mild and severe groups and between no or mild and severe groups were statistically significant (all p<0.001). Although the prevalence of femoral artery plaque in the severe group was higher than that in the moderate group, there was no statistical significance (p>0.05).
Discussion
The novelty of this study lies in the combination of the duration of diabetes, that is, in patients with more than 5 years of illness, re-valuate the ability of different peripheral atherosclerosis measurement methods in predicting the existence of CAD and correlation with the severity of CAD. It was found that femoral plaque and carotid plaque score were independent predictors of CAD in this specific population. We also found that the carotid plaque score was correlated with the severity of CAD, and the femoral plaque had a higher positive rate in patients with moderate to severe CAD, which suggests that it has unique value in identifying moderate to severe CAD.
Our data show the association of traditional cardiovascular risk factors and noninvasive atherosclerosis measures with coronary artery disease. In addition to smoking, other risk factors such as sex, age, blood pressure, various lipid metabolism, BMI, etc. have lost their relationship with CAD. The reason may be that these factors themselves are also risk factors for diabetes. However, non-invasive peripheral arterial measures, including femoral plaque, C-IMT, and carotid plaque scores were all associated with the presence of CAD. The associations of femoral plaque and carotid scores remained, after adjustment for traditional risk factors. This may suggest that non-invasive measurement of peripheral atherosclerosis has a certain value in predicting CAD. In patients with long-term T2DM, this value may exceed the traditional risk factors.
Among the three non-invasive measurement methods, femoral plaque has the strongest correlation with CAD. This is the same as the conclusion that in the autopsy studies, the presence of femoral artery plaques was much more strongly correlated with coronary artery plaques and coronary artery death than plaques in the common carotid artery.22,23 However, the AUC of the carotid plaque score was much higher than that of the femoral plaque in identifying patients with CAD. The reason may be that we used the carotid plaque score to further measure the severity of carotid plaque, rather than defining presence or absence roughly. In a study of 501 patients who completed carotid ultrasonography and first coronary angiography, Nobutaka Ikeda et al demonstrated that CPS was an excellent predictor of the presence of CAD, the areas under the ROC curves for CPS to predict the presence of coronary artery disease was 0.756 (95% CI: 0.713–0.798; p <0.0001).8 Similarly, in the present study we found that CPS was useful in identifying CAD, the AUC values of CPS for CAD prediction was 0.7323 (95% CI 0.665–0.8, p <0.001), which was close to their result. The present study demonstrates the comparatively increased utility of calculated CPS over femoral plaque for identifying patients with significant CAD. CPS demonstrated a high specificity (81.25%) but relatively low sensitivity (61.82%) for CAD detection.
The predictive value of carotid intima-media thickness for CAD is controversial.24 Although some prospective studies have shown that it increases the predictive power of traditional risk prediction models,8,25,26 others cannot confirm this.27 Therefore, the 2013 American College of Cardiology (ACC) / American Heart Association (AHA) guidelines for CVD risk prediction no longer recommend this method.28 Our results suggest that C-IMT is not an independent risk factor for CAD in patients with long-term diabetes and has the lowest ability to predict CAD.
Many previous studies have demonstrated the relationship between noninvasive atherosclerosis measurements and the prevalence or severity of coronary artery disease. However, the assessment of disease severity was limited to the number of coronary artery stenosis, and failed to take into account the complexity of coronary artery disease.29 The Gensini score considers three main parameters of each coronary artery lesion: severity score, region multiplying factor and collateral adjustment factor to characterize the complexity of coronary heart disease, which was first described by Goffredo G. Gensini in 1975.21 It is a widely used angiographic scoring system. We divided the subjects into no or mild group, moderate group, and severe group according to the third quartile of Gensini score. We found that with the increase of severity of coronary stenosis, there was a significant difference in the calculated value of CPS in each group. It suggests that the calculated value of CPS has a good correlation with the severity of coronary artery, which can be used as a predictor of the severity of CAD.30 In addition, some recent studies have demonstrated that CPS has a higher value than C-IMT in predicting stroke and is associated with white matter lesions.31,32
Some previous studies have shown that femoral artery plaques are associated with advanced or severe CAD, which can be used as a surrogate index for coronary atherosclerosis research.33,34 In our study, 71.9% and 79.5% of the moderate CAD group and the severe CAD group showed positive femoral artery plaque, compared with 42.5% in the no or mild CAD group. This suggests that femoral artery plaque is more correlated with moderate to severe CAD, which is also consistent with previous findings in the general population.35 Importantly, this measurement is based on a relatively rough but direct assessment of the presence or absence of atherosclerotic plaques, which is easier to obtain than the carotid plaque score.
Our study had several limitations. First, since the participants in our study are all hospitalized patients, the cardiovascular risk of these subjects may be relatively higher than that of the healthy population. Therefore, it is not clear whether our results are useful for screening long-term T2DM patients who are generally asymptomatic. In addition, age, lipid metabolism disorder, hypertension and other risk factors have lost their correlation with CAD, which may be affected by this selection bias. Second, the modified Gensini score is used, which actually does not take into account the compensation of collateral circulation, so it can be biased in the assessment of the severity of CAD. However, the essential purpose of this study was to evaluate the relationship between extracoronary atherosclerosis and coronary atherosclerosis, so ignoring collateral circulation compensation may not affect our final results.
Conclusion
In conclusion, both carotid plaque score and femoral plaque were independent predictors of CAD. In patients with long-term T2DM, compared with femoral plaque and C-IMT, CPS has a higher ability to predict the occurrence and severity of CAD. However, femoral artery plaque has its special value in predicting moderate to severe CAD.
Data Sharing Statement
The datasets generated and analyzed during this study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the medical ethics committee of Affiliated Hospital of Medical College of Ningbo University. Due to the retrospective nature of this study the ethics committee waived the need for written informed consent of the included patients. However, we de-identified and anonymized patient records/information prior to analysis to protect the patients’ privacy.
Funding
This work was supported by the Science and Technique Plans of Ningbo City (Grant No. 2019C50080).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323. doi:10.1093/eurheartj/ehz486
2. Sarwar N, Gao P, Seshasai SR, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–2222. doi:10.1016/s0140-6736(10)60484-9
3. Bessueille L, Magne D. Inflammation: a culprit for vascular calcification in atherosclerosis and diabetes. Cell Mol Life Sci. 2015;72(13):2475–2489. doi:10.1007/s00018-015-1876-4
4. Rhee SY, Kim YS. The role of advanced glycation end products in diabetic vascular complications. Diabetes Metab J. 2018;42(3):188–195. doi:10.4093/dmj.2017.0105
5. Shi Y, Vanhoutte PM. Macro- and microvascular endothelial dysfunction in diabetes. J Diabetes. 2017;9(5):434–449. doi:10.1111/1753-0407.12521
6. Ul Amin R, Ahmedani MAM, Karim M, Raheem A. Correlation between gensini score and duration of diabetes in patients undergoing coronary angiography. Cureus. 2019;11(2):e4010. doi:10.7759/cureus.4010
7. Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006;368(9529):29–36. doi:10.1016/s0140-6736(06)68967-8
8. Ikeda N, Kogame N, Iijima R, Nakamura M, Sugi K. Carotid artery intima-media thickness and plaque score can predict the SYNTAX score. Eur Heart J. 2012;33(1):113–119. doi:10.1093/eurheartj/ehr399
9. Zhang HW, Jin JL, Cao YX, et al. Association of diabetes mellitus with clinical outcomes in patients with different coronary artery stenosis. Cardiovasc Diabetol. 2021;20(1):214. doi:10.1186/s12933-021-01403-6
10. Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339(4):229–234. doi:10.1056/nejm199807233390404
11. Rana JS, Liu JY, Moffet HH, Jaffe M, Karter AJ. Diabetes and prior coronary heart disease are not necessarily risk equivalent for future coronary heart disease events. J Gen Intern Med. 2016;31(4):387–393. doi:10.1007/s11606-015-3556-3
12. Bulugahapitiya U, Siyambalapitiya S, Sithole J, Idris I. Is diabetes a coronary risk equivalent? Systematic review and meta-analysis. Diabet Med. 2009;26(2):142–148. doi:10.1111/j.1464-5491.2008.02640.x
13. Naqvi TZ, Lee M-S. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging. 2014;7(10):1025–1038. doi:10.1016/j.jcmg.2013.11.014
14. Laclaustra M, Casasnovas JA, Fernández-Ortiz A, et al. Femoral and carotid subclinical atherosclerosis association with risk factors and coronary calcium. J Am Coll Cardiol. 2016;67(11):1263–1274. doi:10.1016/j.jacc.2015.12.056
15. American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl1):S111–s134. doi:10.2337/dc20-S010
16. Chamberlain JJ, Rhinehart AS, Shaefer CF, Neuman A. Diagnosis and management of diabetes: synopsis of the 2016 American Diabetes Association standards of medical care in diabetes. Ann Intern Med. 2016;164(8):542–552. doi:10.7326/m15-3016
17. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281–1357. doi:10.1097/01.hjh.0000431740.32696.cc
18. Touboul PJ, Hennerici MG, Meairs S, et al. Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012;34(4):290–296. doi:10.1159/000343145
19. Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation. 1999;99(17):2345–2357. doi:10.1161/01.cir.99.17.2345
20. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation. 2016;134(10):e123–55. doi:10.1161/cir.0000000000000404
21. Rampidis GP, Benetos G, Benz DC, Giannopoulos AA, Buechel RR. A guide for gensini score calculation. Atherosclerosis. 2019;287:181–183. doi:10.1016/j.atherosclerosis.2019.05.012
22. Dalager S, Falk E, Kristensen IB, Paaske WP. Plaque in superficial femoral arteries indicates generalized atherosclerosis and vulnerability to coronary death: an autopsy study. J Vasc Surg. 2008;47(2):296–302. doi:10.1016/j.jvs.2007.10.037
23. Molnár S, Kerényi L, Ritter MA, et al. Correlations between the atherosclerotic changes of femoral, carotid and coronary arteries: a post mortem study. J Neurol Sci. 2009;287(1–2):241–245. doi:10.1016/j.jns.2009.06.001
24. Poredoš P, Cífková R, Marie Maier JA, et al. Preclinical atherosclerosis and cardiovascular events: do we have a consensus about the role of preclinical atherosclerosis in the prediction of cardiovascular events? Atherosclerosis. 2022;348:25–35. doi:10.1016/j.atherosclerosis.2022.03.030
25. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115(4):459–467. doi:10.1161/circulationaha.106.628875
26. Nambi V, Chambless L, Folsom AR, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. 2010;55(15):1600–1607. doi:10.1016/j.jacc.2009.11.075
27. van den Oord SC, Sijbrands EJ, ten Kate GL, et al. Carotid intima-media thickness for cardiovascular risk assessment: systematic review and meta-analysis. Atherosclerosis. 2013;228(1):1–11. doi:10.1016/j.atherosclerosis.2013.01.025
28. Den Ruijter HM, Peters SA, Anderson TJ, et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA. 2012;308(8):796–803. doi:10.1001/jama.2012.9630
29. Kablak-Ziembicka A, Tracz W, Przewlocki T, Pieniazek P, Sokolowski A, Konieczynska M. Association of increased carotid intima-media thickness with the extent of coronary artery disease. Heart. 2004;90(11):1286–1290. doi:10.1136/hrt.2003.025080
30. Gepner AD, Young R, Delaney JA, et al. Comparison of carotid plaque score and coronary artery calcium score for predicting cardiovascular disease events: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2017;6(2):Feb. doi:10.1161/jaha.116.005179
31. Kawai T, Ohishi M, Takeya Y, et al. Carotid plaque score and intima media thickness as predictors of stroke and mortality in hypertensive patients. Hypertens Res. 2013;36(10):902–909. doi:10.1038/hr.2013.61
32. Zhang X, Li J, Zeng JJ. The association between white matter lesions and carotid plaque score: a retrospective study based on real-world populations. Eur Rev Med Pharmacol Sci. 2022;26(24):9365–9371. doi:10.26355/eurrev_202212_30687
33. Geng B, Cao T, Duan Y. 外周动脉超声检查预测冠状动脉粥样硬化性心脏病的探讨 [Predictive value of peripheral artery ultrasonography for coronary artery disease]. Zhonghua Yi Xue Za Zhi. 2001;81(11):651–654. Chinese.
34. Nicolaides AN, Panayiotou AG, Griffin M, et al. Arterial ultrasound testing to predict atherosclerotic cardiovascular events. J Am Coll Cardiol. 2022;79(20):1969–1982. doi:10.1016/j.jacc.2022.03.352
35. Sosnowski C, Pasierski T, Janeczko-Sosnowska E, et al. Femoral rather than carotid artery ultrasound imaging predicts extent and severity of coronary artery disease. Kardiol Pol. 2007;65(7):760–6;discussion 767–8.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.