Back to Journals » Infection and Drug Resistance » Volume 15
Predictive Value of a Quick Pitt Bacteremia Score for Prognosis of Patients with Bloodstream Infection Secondary to Urinary Tract Infection: A Retrospective Cohort Study
Authors Li C , Wang J, Wang Q , Liu B, Dang H, Li J, Hou D
Received 9 May 2022
Accepted for publication 2 August 2022
Published 10 August 2022 Volume 2022:15 Pages 4381—4391
DOI https://doi.org/10.2147/IDR.S373998
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Changxiu Li,1,* Jing Wang,2,* Qiushi Wang,3,4 Beibei Liu,4 Heqin Dang,1 Jin Li,5 Dapeng Hou4
1Department of Pharmacy, The Second Affiliated Hospital of Shandong First Medical University, Taian, People’s Republic of China; 2Department of Respiratory and Critical Care, The Second Affiliated Hospital of Shandong First Medical University, Taian, People’s Republic of China; 3Simulation Teaching Center, Capital Medical University, Beijng, People’s Republic of China; 4Department of Intensive Care Unit, The Second Affiliated Hospital of Shandong First Medical University, Taian, People’s Republic of China; 5Department of Laboratory, The Second Affiliated Hospital of Shandong First Medical University, Taian, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Dapeng Hou, Department of Intensive Care Unit, The Second Affiliated Hospital of Shandong First Medical University, Taian, People’s Republic of China, Tel +86-18505386932, Email [email protected]
Purpose: To analyze the effect of a quick Pitt bacteremia score (qpitt) on the prognosis of patients with bloodstream infection (BSI) secondary to urinary tract infection (UTI) and to further explore its use in aiding appropriate selection of initial antibiotic treatment.
Methods: Medical records of patients with BSIs secondary to UTIs who were admitted to our hospital from January 2018 to December 2020 were retrospectively collected. To screen for independent risk factors, logistic analysis was conducted on statistically significant variables. The receiver operating characteristic (ROC) curve was drawn with prognosis and death as the state variables to evaluate the predictive value. Patients were grouped by qpitt 2-point cutoff, to explore the impact of initial antimicrobial treatment regimens on poor prognosis and death in different subgroups. Poor prognosis was defined as a hospital length of stay (HLOS) ≥ 14 days or death within 28 days from BSI onset (ie, 28-day death).
Results: A total of 266 patients were included in this study. In BSIs secondary to UTIs, we observed a pathogenic composition of 77.44% Gram-negative bacteria, 19.55% Gram-positive bacteria, and 3.01% fungi. The qpitt had poor predictive value for poor prognosis [area under ROC (AUROC) = 0.653, p < 0.001], while it had a high predictive value for death (AUROC = 0.890, p < 0.001). For patients with a qpitt ≥ 2, the poor prognosis and death rates of patients who were initially treated with carbapenem antibiotics were lower (p < 0.01). In comparison, initial treatment with carbapenem antibiotics had no significant effect on prognosis and death rates in patients with qpitt < 2 (p > 0.1).
Conclusion: The qpitt is highly predictive for death in patients with BSIs secondary to UTIs and can be used to inform first-line antibiotic treatment strategy.
Keywords: bloodstream infection, urinary tract infection, a quick Pitt bacteremia score, antibiotics
Introduction
Bloodstream infections (BSIs) are associated with poor outcomes and are is among the leading causes of death in North America and Europe.1 BSIs are generally defined as the culture of pathogenic microorganisms from one or more peripheral venous blood culture specimens from patients with signs of systemic infection. Depending on the source of the pathogen, BSIs can be categorized as primary or secondary.2 Primary bloodstream infections (PBSIs) involve blood culture positive pathogenic microorganisms that are not associated with other sites of infection. In comparison, secondary bloodstream infections (SBSIs) involve a clear source of primary infection and the spread of pathogens from the primary infection into the blood.3 Common sources of SBSIs include the lungs, abdominal cavity, and genitourinary tract. One study conducted in Spain showed that the most common source of SBSIs was urinary tract infections (UTIs) (30.5%), followed by intra-abdominal infections (20.7%).4 Some scores were proposed to predict the risk of death and poor prognosis of patients with BSIs to aid early, rapid, and accurate diagnoses, which, in turn, improve treatment measures and clinical outcomes. For example, Chow and Yu5 derived the Pitt bacteremia score (PBS) in 1998, Battle et al6 derived the qpitt in 2019. The predictive value of these scores in patients with BSIs has been previously confirmed. However, there is still a lack of systematic data about the predictive effect of these scores in patients with BSIs secondary to UTIs, as well as the guiding significance for the selection of antibiotic treatments in these patients. Herein, we have analyzed the predictive value of qpitt in the prognosis of patients with BSIs secondary to UTIs. Further, we explore whether qpitt can be used to inform antibiotic treatment strategies in these patients.
Methods
Study Design and Participants
A retrospective cohort study was performed in patients over 18 years old with BSIs secondary to UTIs who were admitted to the Second Affiliated Hospital of Shandong First Medical University from January 2018 to December 2020. This study was approved by the ethics committee of the university. The committee’s reference number is 2022045. All data were anonymized to maintain the privacy of each participant.
Data Collection and Definitions
In this retrospective study, the medical records of the patients with BSIs secondary to UTIs who were hospitalized in our hospital were retrospectively collected. Diagnosis of BSIs secondary to UTIs was in accordance with the diagnostic criteria for BSI of the US CDC.3 Complete medical records of patients were collected, including age, gender, symptoms, vital signs on admission, initial antibiotic regimen, comorbidity, laboratory examinations, and microbiology. The qpitt score was calculated based on the medical records, including five scoring items: respiratory rate ≥25 times/min or mechanically assisted ventilation, systolic blood pressure ≤90 mmHg, altered mental status, temperature <36℃, and cardiac arrest.6 A positive index was 1 point, with a maximum total score of 5. For each patient, we calculated the Charlson comorbidity index (CCI) based on 17 comorbid conditions: congestive heart failure (weight = 1), myocardial infarct (weight = 1), cerebrovascular disease (weight = 1), chronic pulmonary disease (weight = 1), paraplegia (weight = 2), dementia (weight = 1), diabetes without complications (weight = 1), diabetes with complications (weight = 2), cancer (weight = 2), metastatic cancer (weight = 6), mild liver disease (weight = 1), moderate or severe liver disease (weight = 3), peptic ulcer disease (weight = 1), peripheral vascular disease (weight = 1), rheumatologic disease (weight = 1), renal disease (weight = 2), acquired immune deficiency syndrome (AIDS) (weight = 6), and for each decade over age 40 y (weight = 1).7,8 Prognostic indicators refer to two indicators, including death and hospital length of stay (HLOS). The judgment indicator of good prognosis indicates survival and hospital length of stay (HLOS) <14 days, while poor prognosis included death within 28 days from BSI onset (ie, 28-day death) or HLOS ≥14 days from BSI onset.9
BSI criteria10 were as follows: patient has a recognized pathogen cultured from one or more blood cultures and the organism cultured from blood is not related to an infection at another site; patient has at least one of the following signs or symptoms: fever (>38°C), chills, or hypotension, and signs and symptoms and positive laboratory results are not related to an infection at another site and common skin contaminant.
UTI criteria10,11 were as follows: patient has at least one of the following signs or symptoms with no other recognized cause of urinary frequency, urgency, dysuria, or costovertebral angle pain or tenderness, suprapubic tenderness, fever (>38.0°C). Based on clinical diagnosis, the etiological diagnosis conformed to one of the following criteria: (1) clean midstream urine or indwelling urine (non-indwelling catheterization) cultured Gram-positive cocci count ≥104 cfu/mL, Gram-negative Bacterial count ≥105 cfu/mL; (2) bacterial count ≥103 cfu/mL in urine cultured by bladder puncture of the suprapubic symphysis; (3) fresh urine specimens were centrifuged and examined by phase-contrast microscopy (1×400), bacteria observed in half of the 30 visual fields; (4) asymptomatic bacteriuria: although the patient was asymptomatic, they had a recent history of endoscopy or indwelling catheterization (usually 1 week), and urine cultures of gram-positive cocci 104 cfu/mL and gram-negative bacteria 105 cfu/mL should be diagnosed as a UTI.
Initial antibiotic therapy was defined as an antimicrobial agents received within the first 72 h following the collection of the first set of positive blood cultures. Initial antibiotic therapy was considered appropriate if it met all of the following criteria: (1) the initial antimicrobial agent was administered intravenously; (2) patient received at least the minimum recommended dose of an antimicrobial agent according to the medication package insert for creatinine clearance at the time of BSI; (3) bloodstream isolate was susceptible to an initial antimicrobial agent based on in vitro antimicrobial susceptibility testing results using Clinical Laboratory and Standards Institute (CLSI) guidelines. Otherwise, initial therapy was considered inadequate.
Diagnostic Criteria for BSIs Secondary to UTIs
The pathogenic bacteria cultured in blood culture specimens should be consistent with at least one pathogenic bacteria in the urinary tract culture specimens, and the time of blood culture collection is attributable to the BSI period.3
Inclusion Criteria
Patients had to be at least 18 years of age, HLOS ≥3 days, length of antibiotic treatment ≥3 days, and patients had to meet the diagnostic criteria for BSIs secondary to UTIs.
Exclusion Criteria
Patients were excluded if they were spontaneously discharged from the hospital and did not complete their antibiotic treatment.
Statistical Analysis
Enumeration data were expressed as counts (%), between-group differences were calculated using a Chi-squared test or Fisher’s exact test. Measurement data of normal distribution were expressed as mean ± standard deviation (SD), and between-group differences were calculated using one-way ANOVA. Measurement data of abnormal distribution were expressed as median (interquartile range), and between-group differences were calculated using a Mann–Whitney U-test. Logistic analysis was conducted on the statistically significant variables of univariate analysis to screen for independent risk factors. The independent risk factors were selected, and the ROC curve was drawn with prognosis and death as the state variable to evaluate the predictive value. Diagnostic consistency was checked using Kappa analysis. All analyses were completed using SPSS, version 21.0, with p-values of <0.05 (two-sided) deemed statistically significant, unless otherwise specified.
Results
Demographics and Clinical Characteristics
Initially, 268 patients were included in the study, but 2 patients were later excluded, resulting in a total of 266 enrolled patients in this study (Figure 1). This included 116 males and 150 females, ranging in age from 27 to 91 years, with an average age of 63.92 ± 14.52 years, with an average length of antibiotic treatment of 10.9 ± 5.1 days. From this cohort, 234 individuals survived while 32 people died. Patients with an HLOS <14 days were included in good prognosis group (n = 158). Further, 76 patients with an HLOSr ≥14 days and 32 patients in-hospital death were included in the poor prognosis group (n = 108). Univariate associations between baseline characteristics and prognosis are displayed in Table 1. As shown, there were significant differences in the following indicators for poor and good prognosis included admission to the intensive care unit (ICU), diabetes mellitus, blood pressure status, respiratory status, type of UTI, site of acquisition, urinary tract obstruction, urological surgery, altered mental status, age, CCI, qpitt, serum creatinine, temperature, procalcitonin (PCT), and the days at home within 30 days. The differences in the following indicators were significant between the death and survival groups: gender, admission to ICU, blood pressure status, respiratory status, site of acquisition, urinary tract obstruction, undergo urological surgery, altered mental status, CCI, qpitt, serum creatinine, temperature, peripheral WBC count, PCT, heart rate, and the days at home within 30 days. Initial appropriate antibiotic therapy had no significant effect on poor prognosis and death.
 |
Table 1 Demographics and Clinical Characteristics of Patients with Bloodstream Infections Secondary to Urinary Tract Infections |
 |
Figure 1 The flow diagram about the source of the study population. |
The Microbiology and the Initial Antibiotic Therapy
Among the 266 patients with UTIs, the etiology detected in blood cultures was mainly Gram-negative bacteria, followed by Gram-positive bacteria, and fungi. There were 206 cases of Gram-negative bacteria positive blood cultures (77.44%), including 144 cases of Escherichia coli and 38 cases of Klebsiella pneumonia. Moreover, 52 cases of Gram-positive bacteria were cultured in blood, accounting for 19.55%, including 20 Staphylococci, 18 Enterococci, and 14 Streptococci. Candida was detected in 8 cases (3.01%) in blood culture (Table 2). Among the 266 strains isolated from blood cultures, 192 strains of Enterobacteriaceae were the most prevalent (96 strains of Extended-spectrum beta-lactamases), followed by Staphylococcus (20 strains), which include 10 methicillin-resistant strains. Enterobacteriaceae bacteria mainly included E. coli (144 strains) and K. pneumoniae (38 strains). Among 144 strains of E. coli, we identified 70 strains of ESBLs, with a sensitivity of 29.2% to ciprofloxacin, 47.2% to levofloxacin, 33.3% to ampicillin/sulbactam, 61.1% to amoxicillin/clavulanate, 95.8% to piperacillin/tazobactam, and 91.6% to cefoperazone/sulbactam. We did not isolate any strains that were resistant to imipenem, meropenem, and tigecycline. Among the 38 strains of K. pneumoniae, we identified 12 strains of ESBLs, with a sensitivity of 42.1% to ciprofloxacin, 31.6% to levofloxacin, 63.1% to ampicillin/sulbactam, 73.7% to amoxicillin/clavulanate, 94.7% to piperacillin tazobactam, 84.2% to cefoperazone/sulbactam, 94.7% to imipenem and meropenem, and 89.5% to tigecycline. Among the 20 Staphylococcus strains, 10 strains were resistant to methicillin, with a sensitivity of 50.0% to ciprofloxacin and no vancomycin-resistant strains were isolated. All patients received initial antibiotic therapy upon BSI onset. However, 30 of these patients had to be switched to a different antibiotic after culture results were received. The length of antibiotic treatment for all cases was 10.9 ± 5.1 days. Moreover, the treatment length for the different parameters was as follows: death cases = 10.4 ±4.18 days; survival cases = 10.97 ± 5.21 days, cases with poor prognosis = 10.64 ± 5.18 days; and cases with good prognosis = 11.09±5.04 days.
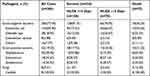 |
Table 2 Proportion of Different Pathogens in Blood Culture |
Results of Logistic Analysis and ROC Curve
Risk factors for poor prognosis and 28-day death in the multivariable logistic regression included the variables that were significant (ie, p < 0.05) in univariable analysis (Table 1). These data showed that the qpitt score, CCI, and temperature were independent risk factors for poor prognosis and death (Tables 3 and 4).
 |
Table 3 Multivariable Logistic Regression Model Results for Independent Risk Factors of Poor Prognosis |
 |
Table 4 Multivariable Logistic Regression Model Results for Independent Risk Factors of Death |
The patient’s qpitt, CCI, and temperature were used as the test variable, and the ROC curve was analyzed with poor prognosis and death as the state variables (Tables 5 and 6, Figures 2 and 3). The results showed that qpitt had a poor predictive value for poor prognosis (AUROC = 0.653, p < 0.001), while it had a high predictive value for death (AUROC = 0.890, p < 0.001), in addition, the AUROC of the qpitt score for predicting death was larger than for CCI and temperature. The best qpitt score cutoff for predicting poor prognosis and death was 1.5.
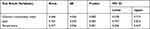 |
Table 5 Area Under ROC Curves for the Prediction of Poor Prognosis |
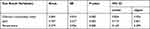 |
Table 6 Area Under ROC Curves for the Prediction of Death |
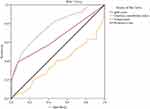 |
Figure 2 Receiver operator characteristic (ROC) curves of the independent risk factors for the prediction of poor prognosis. |
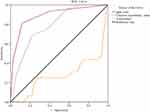 |
Figure 3 Receiver operator characteristic (ROC) curves of the independent risk factors for the prediction of death. |
Kappa Consistency
Since a qpitt score of 1.5 does not exist, both qpitt ≥1 and qpitt ≥2 were analyzed for poor prognosis and death using Kappa consistency, respectively. Results showed that qpitt ≥2 had a certain correlation with poor prognosis and death (p < 0.001), nevertheless the consistency was medium (kappa values were 0.340 and 0.534, respectively). Therefore, a qpitt ≥2 served as a definite predictor for prognosis and death. The sensitivity, specificity, positive predictive value, and negative predictive value for predicting a poor prognosis were 38.9%, 92.4%, 77.8%, and 68.9%, respectively. When a qpitt score ≥2 was used to predict death, the results of the aforementioned indicators were 81.3%, 88.0%, 48.1%, and 97.2%, respectively.
Guidance of qpitt for Antibiotic Therapy
All the cases were divided into two subgroups by a qpitt of 2 for further analysis. In the stratified analysis by acute severity of illness using qpitt, the initial application of carbapenems was associated with a lower rate of poor prognosis and death in critically ill patients with qpitt ≥2 (Table 7, p < 0.01), but not in patients with qpitt <2 (Table 7, p > 0.1).
 |
Table 7 Stratified Analysis of Carbapenems as the Initial Therapy on the Prognosis |
Discussion
The PBS was proposed in 198912 and has been revised several times.13 Many studies have confirmed that it has a good predictive value for prognosis in patients with BSIs.14–16 It has a higher discriminatory power for predicting death in patients with ICU acquired sepsis than Acute Physiology and Chronic Health Evaluation II (APACHE II).17 However, some indicators of PBS, such as mental status,13 cannot be obtained in a timely manner when patients are on admission or symptoms appear. In addition, the three degrees of altered mental status cannot be quickly distinguished, including disorientation, stupor and coma. Therefore, it is not possible to obtain a more accurate PBS score at the time of BSI onset, which affects the timely assessment of patient’s prognoses. The qpitt includes hypotension (systolic blood pressure ≤90 mmHg), respiratory rate ≥25 beats/min or mechanically ventilation, altered mental status, temperature <36°C, and cardiac arrest. All of these five indicators can be obtained on admission or symptoms appearing. According to qpitt, we can make a preliminary and rapid assessment for patients suspected of BSIs to determine the severity of the patient’s infection and predict the patient’s prognosis. Yet the qpitt contains relatively few indicators, there is some controversy about the accuracy of severity assessment and prognosis judgment.18–20 In patients with BSIs caused by Staphylococcus aureus, qpitt has a good predictive value for the 28-day mortality and 14-day mortality of these patients, and the AUROC are 0.8 and 0.81,19 respectively. For the patients with carbapenem-resistant Enterobacter infection treated with ceftazidime/avibactam, the study of Jorgensen18 showed that the predictive value of qpitt for the 30-day mortality was poor, and the AUROC was only 0.6847. However, in patients with carbapenem-resistant Enterobacter infection, Henderson’s study showed that qpitt ≥2 had a good predictive value for 14-day mortality, with a sensitivity of 91% and a specificity of 65%, even if the patient is not with BSI, qpitt ≥2 also has similar predictive value, with a sensitivity of 95% and a specificity of 64%.21 The results of our study are consistent with the above studies. Our study shows that qpitt has a certain predictive value for the prognosis of patients with BSIs secondary to UTIs, among which the predictive value for death is better, the AUROC is 0.890, the sensitivity and specificity for predicting death were 81.3% and 88%, whereas the predictive value for poor prognosis is low with an AUROC of only 0.653.
Compared with the predictive value, whether PBS or qpitt can provide a reference for the selection of antibiotics for patients with BSI is more important. Our study showed that the mortality and incidence of poor prognosis in patients with qpitt ≥2 were significantly (p < 0.01) lower in those treated with carbapenems as the first line. These data suggested that patients with BSIs secondary to UTIs with qpitt ≥2 (can also be considered as patients with relatively severe disease13) use carbapenems for initial treatment may lead to a better prognosis. However, the above-mentioned patients with qpitt <2 (that is patients with relatively mild disease) were initially treated with carbapenems, whose death and prognosis were not significantly improved, suggesting that such patients do not necessarily choose carbapenems with a high price and broad antibacterial spectrum as an initial application.
The initial empirical therapy of BSIs secondary to UTIs has been controversial. At present, the pathogenic bacteria of BSIs secondary to UTIs are mainly Gram-negative bacteria, the most common of which is E. coli, followed by K. pneumonia. This also includes Gram-positive bacteria, such as Enterococci, Staphylococcus, and Streptococcus.22–24 Up to 60% of bacteria detected in BSISs are resistant to the third-generation cephalosporins, such as ceftriaxone and ceftazidime,25 and the resistance rate of E. coli detected in UTIs resistant to fluoroquinolones (such as ciprofloxacin and levofloxacin) ranges from 25% to 50% in many European countries.26 When a drug is chosen for treatment, developing or already existing resistance to the drug is the most important factor for selecting an appropriate antibiotic, alongside pharmacodynamic, pharmacokinetic, and tolerability aspects. Hence, carbapenems, compound preparation of β-lactams and β-lactamase inhibitors, were most commonly recommended for the initial empirical treatment. A study by Lee27 and Son28 showed that the use of carbapenems as the first-line treatment may lead to a better prognosis. However, a study by Al-Hasan29 confirmed that the empirical use of combination β-lactams and fluoroquinolone antibiotics for less severely ill patients with BSIs can also achieve a better prognosis.
For this reason, special indicators or scores are needed to distinguish the severity of the disease in patients with BSIs secondary to UTIs, and then patients with different severities can be treated with different antibiotics. The BSI death risk score (BSIMRS) was used to distinguish the severity of illness in patients with Gram-negative bacilli BSI in a study by Cain.30 For patients with relatively severe diseases (BSIMRS ≥ 5), inappropriate empirical antimicrobial therapy will lead to increased death. Harris31 used the PBS to stratify patients with BSIs and the therapeutic effects of different treatment schemes on these patients were compared. The results of the randomized controlled study published in JAMA showed that the mortality of BSI caused by ceftriaxone resistant E. coli and K. pneumonia treated with meropenem in patients with relatively severe illness (PBS ≥ 4) was lower than treated with piperacillin/tazobactam, yet the difference in death was not significant for patients with relatively mild illness (PBS < 4). The results of the above studies are consistent with ours. For patients with BSIs secondary to UTIs, when their qpitt ≥2, treated carbapenems as initial therapy may lead to a better prognosis.
Our study shares the common limitations of retrospective cohorts. The results can only suggest that the qpitt has some predictive value for death in patients with BSIs secondary to UTIs, and some correlation between initial application of carbapenems and lower death and better prognosis in patients with higher qpitt. Whether the qpitt can be used as the basis for the initial selection of antibiotics needs to be further verified by well-designed prospective studies.
Conclusion
The qpitt can be calculated quickly and efficiently. It has a high predictive value for death in patients with BSIs secondary to UTIs. Patients with qpitt ≥2 treated carbapenems as initial therapy may lead to a better prognosis.
Ethics Approval
This study was approved by the ethics committee of the Second Affiliated Hospital of Shandong First Medical University. The committee’s reference number is 2022045. All data were anonymized to maintain participant’s privacy. In light of retrospective nature of the study, the Ethics Committee did not require written informed consent provided by participants. We certify that the study was performed in accordance with the 1964 Declaration of Helsinki and later amendments.
Acknowledgment
In the collection of data, this study was supported by grants from Science and Technology Development Program of Tai’an City (2021NS307).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Goto M, Al-Hasan MN. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect. 2013;19(6):501–509. doi:10.1111/1469-0691.12195
2. Laupland KB, Church DL. Population-based epidemiology and microbiology of community-onset bloodstream infections. Clin Microbiol Rev. 2014;27(4):647–664. doi:10.1128/CMR.00002-14
3. National Healthcare Safety Network. Bloodstream infection event (central line-associated bloodstream infection and non-central line associated bloodstream infection). CDC:NHSN; 2022. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/7psccauticurrent.pdf.
4. Arco AD, Olalla J, Latorre JD, et al. Results of an early intervention programme for patients with bacteraemia: analysis of prognostic factors and mortality. BMC Infect Dis. 2017;17(1):360.
5. Chow JW, Yu VL. Combination antibiotic therapy versus monotherapy for gram-negative bacteraemia: a commentary. Int J Antimicrob Agents. 1999;11(1):7–12. doi:10.1016/S0924-8579(98)00060-0
6. Battle SE, Augustine MR, Watson CM, et al. Derivation of a quick Pitt bacteremia score to predict mortality in patients with gram-negative bloodstream infection. Infection. 2019;47(4):571–578. doi:10.1007/s15010-019-01277-7
7. Koppie TM, Serio AM, Vickers AJ, et al. Age-adjusted Charlson comorbidity score is associated with treatment decisions and clinical outcomes for patients undergoing radical cystectomy for bladder cancer. Cancer. 2008;112(11):2384–2392. doi:10.1002/cncr.23462
8. Ofori-Asenso R, Zomer E, Chin KL, et al. Effect of comorbidity assessed by the Charlson comorbidity index on the length of stay, costs and mortality among older adults hospitalised for acute stroke. Int J Environ Res Public Health. 2018;15(11):11. doi:10.3390/ijerph15112532
9. Rac H, Gould AP, Bookstaver PB, et al. Evaluation of early clinical failure criteria for gram-negative bloodstream infections. Clin Microbiol Infect. 2020;26(1):73–77. doi:10.1016/j.cmi.2019.05.017
10. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–332. doi:10.1016/j.ajic.2008.03.002
11. National Healthcare Safety Network. Urinary tract infection (Catheter-Associated Urinary Tract Infection [CAUTI] and Non-Catheter-Associated Urinary Tract Infection [UTI]) Events. CDC:NHSN; 2022. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/7psccauticurrent.pdf.
12. Hilf M, Yu VL, Sharp J, et al. Antibiotic therapy for Pseudomonas aeruginosa bacteremia: outcome correlations in a prospective study of 200 patients. Am J Med. 1989;87(5):540–546. doi:10.1016/s0002-9343(89)80611-4
13. Al-Hasan MN, Baddour LM. Resilience of the Pitt Bacteremia Score: 3 decades and counting. Clin Infect Dis. 2020;70(9):1834–1836. doi:10.1093/cid/ciz535
14. Wu C-J, Lee H-C, Chang -T-T, et al. Aeromonas spontaneous bacterial peritonitis: a highly fatal infectious disease in patients with advanced liver cirrhosis. J Formos Med Assoc. 2009;108(4):293–300. doi:10.1016/S0929-6646(09)60069-3
15. Chakhtoura NGE, Saade E, Wilson BM, et al. A 17-year nationwide study of Burkholderia cepacia complex bloodstream infections among patients in the United States veterans health administration. Clin Infect Dis. 2017;65(8):1253–1259. doi:10.1093/cid/cix559
16. Shen LS, Chan L, Zhu B, et al. Bloodstream infections due to carbapenem-resistant Klebsiella pneumoniae: a single-center retrospective study on risk factors and therapy options. Microbial Drug Resist. 2021;27(2):227–233. doi:10.1089/mdr.2019.0455
17. Rhee J-Y, Kwon KT, Ki HK, et al. Scoring systems for prediction of mortality in patients with intensive care unit-acquired sepsis: a comparison of the Pitt bacteremia score and the acute physiology and chronic health evaluation II scoring systems. Shock. 2009;31(2):146–150. doi:10.1097/SHK.0b013e318182f98f
18. Jorgensen SCJ, Lagnf AM, Bhatia S, Rybak MJ. A new simplified predictive model for mortality in methicillin-resistant Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis. 2019;38(5):843–850. doi:10.1007/s10096-018-03464-0
19. Battle SE, Shuping M, Withers S, et al. Prediction of mortality in Staphylococcus aureus bloodstream infection using quick Pitt bacteremia score. J Infect. 2021;84(2):131–135. doi:10.1016/j.jinf.2021.12.002
20. Madrazo M, Piles L, López‑Cruz I, et al. Comparison of quick Pitt to quick sofa and sofa scores for scoring of severity for patients with urinary tract infection. Intern Emerg Med. 2022. doi:10.1007/s11739-022-02927-9
21. Henderson H, Luterbach CL, Cober E, et al. The Pitt Bacteremia Score predicts mortality in nonbacteremic infections. Clin Infect Dis. 2020;70(9):1826–1833. doi:10.1093/cid/ciz528
22. Fortin E, Rocher I, Frenette C, et al. Healthcare-associated bloodstream infections secondary to a urinary focus: the Quebec provincial surveillance results. Infect Control Hosp Epidemiol. 2012;33(5):456–462.
23. Fitzpatrick JM, Biswas JS, Edgeworth JD, et al. Gram-negative bacteraemia; a multi-centre prospective evaluation of empiric antibiotic therapy and outcome in English acute hospitals. Clin Microbiol Infect. 2016;22(3):244–251. doi:10.1016/j.cmi.2015.10.034
24. Diekema DJ, Hsueh PR, Mendes RE, et al. The microbiology of bloodstream infection: 20-year trends from the SENTRY antimicrobial surveillance program. Antimicrob Agents Chemother. 2019;63(7). doi:10.1128/AAC.00355-19
25. Mark DG, Hung YY, Salim Z, et al. Third-generation cephalosporin resistance and associated discordant antibiotic treatment in emergency department febrile urinary tract infections. Ann Emerg Med. 2021;78(3):357–369. doi:10.1016/j.annemergmed.2021.01.003
26. Wiedemann B, Heisig A, Heisig P. Uncomplicated urinary tract infections and antibiotic resistance-epidemiological and mechanistic aspects. Antibiotics. 2014;3(3):341–352. doi:10.3390/antibiotics3030341
27. Lee C-C, Lee C-H, Hong M-Y, et al. Timing of appropriate empirical antimicrobial administration and outcome of adults with community-onset bacteremia. Crit Care. 2017;21(1):119. doi:10.1186/s13054-017-1696-z
28. Son JS, Song J-H, Ko KS, et al. Bloodstream infections and clinical significance of healthcare-associated bacteremia: a multicenter surveillance study in Korean hospitals. J Korean Med Sci. 2010;25(7):992–998. doi:10.3346/jkms.2010.25.7.992
29. Al-Hasan MN, Wilson JW, Lahr BD, et al. Beta-lactam and fluoroquinolone combination antibiotic therapy for bacteremia caused by gram-negative bacilli. Antimicrob Agents Chemother. 2009;53(4):1386–1394. doi:10.1128/AAC.01231-08
30. Cain SE, Kohn J, Bookstaver PB, et al. Stratification of the impact of inappropriate empirical antimicrobial therapy for Gram-negative bloodstream infections by predicted prognosis. Antimicrob Agents Chemother. 2015;59(1):245–250. doi:10.1128/AAC.03935-14
31. Harris PNA, Tambyah PA, Lye DC, et al. Effect of piperacillin-tazobactam vs meropenem on 30-day mortality for patients with E coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: a randomized clinical trial. JAMA. 2018;320(10):984–994. doi:10.1001/jama.2018.12163
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
