Back to Journals » Patient Preference and Adherence » Volume 9
Predictive factors for obtaining a correct therapeutic range using antivitamin K anticoagulants: a tertiary center experience of patient adherence to anticoagulant therapy
Authors Jurcuţ R , Militaru S, Geavlete O, DrăgotoiuN, Sipoş S, Roşulescu R, Ginghină C, Jurcuţ C
Received 21 April 2015
Accepted for publication 19 June 2015
Published 8 September 2015 Volume 2015:9 Pages 1271—1278
DOI https://doi.org/10.2147/PPA.S87066
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Ruxandra Jurcuţ,1 Sebastian Militaru,1 Oliviana Geavlete,1 Nic Drăgotoiu,1 Sergiu Sipoş,1 Răzvan Roşulescu,2 Carmen Ginghină,1 Ciprian Jurcuţ2
1Prof Dr CC Iliescu Emergency Institute for Cardiovascular Diseases, University of Medicine and Pharmacy, 2Dr Carol Davila Central University Emergency Military Hospital, Bucharest, Romania
Background: Patient adherence is an essential factor in obtaining efficient oral anticoagulation using vitamin K antagonists (VKAs), a situation with a narrow therapeutic window. Therefore, patient education and awareness are crucial for good management. Auditing the current situation would help to identify the magnitude of the problem and to build tailored education programs for these patients.
Methods: This study included 68 hospitalized chronically anticoagulated patients (mean age 62.6±13.1 years; males, 46%) who responded to a 26-item questionnaire to assess their knowledge on VKA therapy management. Laboratory and clinical data were used to determine the international normalized ratio (INR) at admission, as well as to calculate CHA2DS2-VASC and HAS-BLED scores for patients with atrial fibrillation.
Results: The majority of patients (62%) were receiving VKA for atrial fibrillation, the others for a mechanical prosthesis and previous thromboembolic disease or stroke. In the atrial fibrillation group, the mean CHA2DS2-VASC score was 3.1±1.5, while the average HAS-BLED score was 1.8±1.2. More than half of the patients (53%) had an INR outside of the therapeutic range at admission, with the majority (43%) having a low INR. A correct INR value was predicted by education level (higher education) and the diagnostic indication (patients with mechanical prosthesis being best managed). Patients presenting with a therapeutic INR had a trend toward longer treatment duration than those outside the therapeutic range (62±72 months versus 36±35 months, respectively, P=0.06). There was no correlation between INR at admission and the patient’s living conditions, INR monitoring frequency, and bleeding history.
Conclusion: In a tertiary cardiology center, more than half of patients receiving VKAs are admitted with an INR falling outside the therapeutic range, irrespective of the bleeding or embolic risk. Patients with a mechanical prosthesis and complex antithrombotic regimens appear to be the most careful with INR monitoring, especially if they have a higher level of education. Identifying patient groups with the lowest time interval spent in the therapeutic range could help attending physicians educate patients focusing on specific awareness issues.
Keywords: anticoagulant therapy, antivitamin K agents, patient adherence, questionnaire
Introduction
Oral anticoagulant therapy (OACT) is one of the major therapeutic classes in cardiology and probably the most challenging to manage on a long-term basis. It is prescribed for various indications, the most common being atrial fibrillation (AF) (with a prevalence estimated at 1%–2% of the general population1), followed by prosthetic heart valves and venous thromboembolic disease.
It is well known that patient adherence to treatment is one of the main causes of treatment failure. In the case of OACT this is especially true, as problems concerning compliance with treatment are also paralleled by the difficulties in obtaining a correct therapeutic range with the most widely used OACT, ie, vitamin K antagonist (VKA) anticoagulants. In this case, poor adherence to the drug regimen is associated with a lower percentage of time in therapeutic range and also with an increased risk of thromboembolic complications. Nonadherence to anticoagulation may lead to major adverse events (eg, stroke, pulmonary embolism) leading in turn to more hospital admission and residential care, and increase costs to the health care system.
Therefore, for OACT to be most effective, a bidirectional process has to be in place: patients have to comply with medical instructions, but also physicians have to understand what makes patients more likely to have consistent therapeutic international normalized ratio (INR) results and develop methods that lead in that direction. The aim of the study was to establish the determinants of patient awareness regarding OACT on the therapeutic effectiveness in a tertiary cardiology center, with the hypothesis that this can help to understand the magnitude of the problem and to build tailored education programs for these patients.
Materials and methods
Study population
This observational study was conducted during a 2-year period (2012–2014) in the cardiology department of a tertiary cardiology hospital. We included consecutive patients undergoing OACT with VKA agents irrespective of indication, who agreed to participate to the survey.
Awareness questionnaire
For the purpose of data collection, we developed a questionnaire containing 26 questions (Supplementary materials section). The questions were designed to assess patients’ background, education level, knowledge of diagnosis for which OACT was prescribed, and general knowledge about OACT, as well as assessing their compliance with treatment and periodic INR testing. The preferred method of administering the questionnaire was with the help of cardiology interns who read the questions, as this overcame barriers concerning literacy, visual impairment, or understanding of more technical questions. We also noted for each patient several variables to be included in the database: age, the INR value on admission, the CHA2DS2-VASC score (for embolic risk), and HAS-BLED (for bleeding risk) score for patients with AF. This type of observational only, non-interventional study did not require an Institutional Ethics Committee approval.
Statistical analysis
Continuous data are presented as the mean ± standard deviation. The Student’s t-test was used to test differences between two continuous datasets, whereas chi-square tests were used for differences between categorical data. Statistically significant results were considered at a two-tailed P-value <0.05. All data were analyzed using Statistical Package for the Social Sciences version 19.0 software (IBM Corporation, Armonk, NY, USA).
Results
Patient characteristics
The present study included in total 95 patients who filled in the questionnaire, but only 68 patients (44% men) could answer all questions and have a complete set of variables, this being the final study group. The mean age was 62.6±13.1 years, with a balanced sex distribution (Table 1); 27% were living in a rural area, and only 34% patients had higher education, with a balanced distribution among secondary school, high school, and college education.
The most common diagnosis for which OACT was prescribed in our center was AF (62%), followed by mechanical valve prosthesis (9%), venous thromboembolic disease (9%), and stroke (6%). Within the AF group, the mean CHA2DS2-VASC was 3.1 (showing high embolic risk), with HAS-BLED averaging 1.8 (showing low-moderate bleeding risk). No patient had a CHA2DS2-VASC score of 0, while nine patients had a score of 1. Antiplatelet therapy was commonly prescribed (37% patients), regardless of whether there was coexistent myocardial infarction or coronary artery disease.
Anticoagulation treatment
All patients were treated with the VKA medication available in our country, ie, acenocoumarol. The INR value at the index admission was outside the appropriate therapeutic range in more than half of the patients, with 43% having an INR below the lowest therapeutic level and 10% above the highest therapeutic level. Only 32 patients (47%) were inside the recommended INR range.
Most patients were prescribed OACT by a cardiologist (69%) in a hospital setting (86%, Table 2). More than 80% reported having been informed about the risks and benefits of undergoing OACT, with even more declaring compliance with the daily dose prescribed (91%). On the other hand, more than a third of the patients did not know the target INR value for their specific pathology, with more than half not knowing the emergency INR value. A quarter of the patients were not informed or did not recollect the total duration of OACT for their specific case.
  | Table 2 Oral anticoagulation treatment-related characteristics |
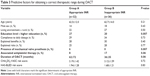
Predictive factors for obtaining a correct therapeutic range
In order to assess the determinants for obtaining a correct therapeutic range for VKA, the patients were separated into two groups: group A, having an INR appropriate for the prescription (32 patients), and group B, having an INR outside the therapeutic range (36 patients).
The only variables that proved to be significantly predictive of a correct INR value on admission were higher education level and an OACT prescription for a mechanical prosthesis (Table 3). People with high school education or higher were more likely to have appropriate an INR on admission than those with secondary school education or lower (20% versus 57%, P<0.05). All six patients with a mechanical valve prosthesis had a correct INR, compared with 41% for the rest of the patients (P<0.05). There was a trend for patients with a therapeutic INR to have a longer duration of OACT (62±72 months for correct INR versus 36±35 months for out-of-range INR, P=0.06). Also, interestingly, when antiplatelet therapy was associated with the antithrombotic regimen, INR was more often inappropriately low, maybe reflecting a more prudent approach of patients and caregivers in this instance.
The relationship between OACT-related parameters and a declared history of bleeding was also evaluated. As shown in Table 4, the declared history of bleeding was not correlated with high INR levels or antiplatelet therapy (P>0.05 chi-square for both hypothesis).
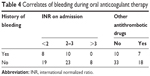  | Table 4 Correlates of bleeding during oral anticoagulant therapy |
Discussion
The main findings of the present study are that in a tertiary cardiology center more than half patients receiving VKA are admitted with an INR outside the therapeutic range, irrespective of the bleeding or embolic risk. In our study, patients with mechanical valve prosthesis regimens appear to have the most effective INR monitoring, especially those having higher education.
Most clinical data regarding patient adherence to OACT come from the field of AF, as this is the main indication for anticoagulation in terms of both prevalence and frequency of indication. In 2009, the AF AWARE group conducted an international survey2 to investigate patients’ and cardiologists’ perceptions of AF, and discovered that both patients and physicians considered AF to be life-threatening and reported the impact of AF on quality of life as moderate to high. Anticoagulation therapy is generally prescribed for AF, especially when heart failure or other cardiac disease is present, as shown by a recent publication from the EURObservational Research Programme on Atrial Fibrillation (EORP-AF) pilot survey.3 However, even from the physician’s perspective, there can be inconsistency in OACT prescriptions for guideline-driven indications. In a Danish primary care population of patients with nonvalvular AF, based on the CHA2DS2-VASC score, 75.4% of the patients were treated in adherence with the guidelines, 22.7% were undertreated, and 1.8% were overtreated.4
Lack of adherence to treatment is one of the main reasons for treatment failure in general, and especially in the case of VKA anticoagulation in particular, as patients have to strictly monitor INR levels. A recent study including 163,785 warfarin-treated patients with AF from a Swedish registry5 showed that 45% of the patients did not receive enough warfarin to last 80% of the time at risk. Moreover, between 16% and 21% of the patients discontinued OACT within the first year, followed by 8%–9% annually during the following years, especially if at high bleeding risk or with a perception of a low embolic risk. This facts are linked to the existence of various barriers in obtaining a constant therapeutic range.6,7 Proposed explanations for this reality are: demonstrated lack of patients’ awareness of the AF-associated stroke risk,8 trust in aspirin as a protective factor against stroke irrespective of AF association, concerns regarding bleeding risk during OACT, practical issues related to INR test sample collection and test interpretation, and low cognitive function or dementia leading to inappropriate drug administration.
Our study showed that age and living conditions (rural versus urban) were not linked to therapeutic range during OACT, making access to laboratory testing less of a problem when education and therapy duration were advantages in the same patient. Unlike AF patients, all patients receiving OACT for mechanical valve prosthesis in our study group had a correct INR value at admission.
The practical implication of these data results in finding the ability to prevent more embolic events by changing both physicians’ and patients’ practices regarding awareness and adherence to OACT. More than a decade ago, Barcellona et al assessed 219 patients for the time spent within the therapeutic INR range in relation to different traits and characteristics, and identified positive predictive factors, such as declared compliance, regular intake of vegetables, and concomitant use of other medication.9 The authors also administered an educational questionnaire and at the 3-month follow-up reported a significant improvement for time spent in the therapeutic range.3 Another prospective, multicenter, open randomized study (the EDUC’AVK project) divided patients with venous thromboembolic disease into two groups: an interventional group that received a 30-minute one-to-one educational session on OACT and a control group. The authors reported that at 3 months the rate of complications (both bleeding and embolic recurrence) dropped from 10.6% to 3.1% in the interventional group.10
Patient education has been considered useful for decades now in patients receiving long-term OACT. A variety of educational models have been clinically used and published (one-to-one discussions, slide shows, printed materials). Guidelines were issued in order to regulate OACT self-monitoring.11 In 2008, Wofford et al published a review of the existing studies on patient adherence to anticoagulant therapy and educational strategies. They reviewed 13 different strategies for patient education, coming to the conclusion that, while very diverse patient education methods are described in the literature, standardizing educational material for patient education is necessary for improving the quality of OACT.12 Our group has published and uses printed educational materials for patients regarding OACT, AF, and venous thrombosis in everyday clinical practice (also available online in Romanian language at www.ghidulpacientului.ro).
A more recent approach to OACT adherence involves the use of novel oral anticoagulants. The fixed-dose regimen, together with avoiding the need for periodic laboratory tests for treatment monitoring are very appealing features in this context. However, these advantages can be blunted by the higher costs supported by patients (as is the case in Eastern Europe now), fear of bleeding events, and lack of reversal with novel oral anticoagulants.13
Irrespective of the prescribed OACT, a recent study showed that patients exposed to an anticoagulation decision prefer to actively participate in the decision-making process, and have individual personal values involved in making a decision that cannot be predicted or assumed by anyone in the health care system.14
Limitations of the study
Our study sample size was limited, but we found consistency of data with previous literature reports. The small number of patients also prevented statistically significant subgroup analysis based on indication for OACT.
The present study is questionnaire-based, so we should also take into account a potential recall bias or inaccuracy for items based on the patient’s history. This is, however, a common problem for such studies or registries, and the answers reflect the patient’s perception on historical data. Also, there was no assessment tool for the time spent by patients inside the therapeutic range, which would have been a more robust parameter of adherence to treatment as well as therapeutic efficacy.
Conclusion
In a tertiary cardiology center, more than half of patients receiving chronic OACT with VKAs are admitted with an INR falling outside the therapeutic range, irrespective of the bleeding or embolic risk. Patients with a mechanical prosthesis appear as most careful with INR monitoring, especially if they have higher education. Identifying patient groups with the lowest time interval spent in the therapeutic range could help attending physicians to tailor patient education focusing on specific awareness issues.
Disclosure
The authors report no conflicts of interest in this work.
References
Camm AJ, Lip GY, De Caterina R, et al. 2012 focused update of the ESC guidelines for the management of atrial fibrillation. Eur Heart J. 2012;33:2719–2747. | ||
Aliot E, Breithardt G, Brugada J, et al. An international survey of physician and patient understanding, perception, and attitudes to atrial fibrillation and its contribution to cardiovascular disease morbidity and mortality. Europace. 2010;12:626–633. | ||
Lip YH, Laroche C, Dan GA, et al. ‘Real-world’ antithrombotic treatment in atrial fibrillation: the EORP-AF Pilot Survey. Am J Med. 2014;127:519–529. | ||
Brandes A, Overgaard M, Plauborg L, et al. Guideline adherence of antithrombotic treatment initiated by general practitioners in patients with nonvalvular atrial fibrillation: a Danish survey. Clin Cardiol. 2013;36:427–432. | ||
Skeppholm M, Friberg L. Adherence to warfarin treatment among patients with atrial fibrillation. Clin Res Cardiol. 2014;103:998–1005. | ||
Razouki Z, Ozonoff A, Zhao S, Jasuja GK, Rose AJ. Improving quality measurement for anticoagulation: adding international normalized ratio variability to percent time in therapeutic range. Circ Cardiovasc Qual Outcomes. 2014;7:664–669. | ||
Hess PI, Mirro MJ, Diener H-C, et al. Addressing barriers to optimal oral anticoagulation use and persistence among patients with atrial fibrillation: Proceedings, Washington, DC, December 3–4, 2012. Am Heart J. 2014;168:239–247.e1. | ||
Lip GY, Kamath S, Jafri M. Ethnic differences in patient perceptions of atrial fibrillation and anticoagulation therapy: the West Birmingham Atrial Fibrillation Project. Stroke. 2002;33:238–242. | ||
Barcellona D, Contu P, Marongiu F. Patient education and oral anticoagulant therapy. Haematol J. 2002;87:1081–1086. | ||
Pernod G, Labarère J, Yver J, et al. EDUC’AVK: reduction of oral anticoagulant-related adverse events after patient education: a prospective multicenter open randomized study. J Gen Intern Med. 2008;23:1441–1446. | ||
Ansell J, Jacobson A, Levy J, Voller H, Hasenkam JM. International Self-Monitoring Association for Oral Anticoagulation Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation. Int J Cardiol. 2005;99:37–45. | ||
Wofford JL, Wells MD, Singh S. Best strategies for patient education about anticoagulation with warfarin: a systematic review. BMC Health Serv Res. 2008;8:40. | ||
Di Minno A, Spadarella G, Tufano A, et al. Ensuring medication adherence with direct oral anticoagulant drugs. Lessons from adherence with vitamin K antagonists (VKAs). Thromb Res. 2014;133:699–704. | ||
Palacio AM, Kirolos I, Tamariz L. Patient values and preferences when choosing anticoagulants. Patient Prefer Adherence. 2015;9:133–138. |
Supplementary material
Patient awareness questionnaire
Surname:
Forename:
Sex: M/F Age:
1. The diagnosis for which ACT was prescribed was:
- Deep VT
- PTE
- Superficial VT
- Atrial fibrillation (paroxysmal, persistent, permanent)
- Cardiac valve prosthesis: metallic/biological
- Stroke
- Cardiac ischemic disease (what type: ...............................................)
- Cardiac failure with low EF (most recent EF being ...............................................)
- Left ventricular aneurysm
- Other...............................................
2. Level of education:
- None
- Primary school
- Secondary school
- High school
- Bachelor or above
3. Living environment:
- Rural
- Urban
4. Where was ACT prescribed?
- Ambulatory clinic
- Hospital
- General practitioner’s office
- Home consultation-visit
5. Who prescribed the ACT?
- Cardiologist
- Internal medicine doctor
- Neurologist
- General practitioner
- Other...............................................
6. What AC drug do you use?
- Sintrom
- Trombostop
- Other...............................................
7. Do you use any other antithrombotic drug?
- Aspirin; dosage...............................................
- Plavix (or other brand names for clopidogrel):Dosage...............................................
- Other...............................................
8. Were you informed about the benefits of ACT?
- Yes
- No
9. Were you informed about the risks of ACT?
- Yes
- No
10. How long have you been under ACT?
...............................................(years and months)
11. For how long have you been informed the duration of ACT is, in your case?
- The whole life
- For limited period of time ...............................................
- I haven’t been informed about the duration
12. Who administers the therapy for you?
- I do it myself
- A member of the family
- Somebody else
13. Do you know your current ACT daily dosage that you have been prescribed?
- Yes
- No
14. Do you follow this daily dosage?
- Yes
- No
- Only sometimes
15. What is the correct INR interval when undergoing ACT?
- 1.5–2
- 2–3
- 2.5–3
- 3–3.5
- 3.5–4
- I don’t know
- I haven’t been told
16. What is the time interval after which you were informed to repeat your INR dosing?
- Once a week
- Less than once a month (how many times per months...............................................?)
- Once a month
- Once every 2 months
- More than once every 2 months
- I don’t know
- I haven’t been told
17. What is the time interval after which you repeat your INR dosing?
- Once a week
- Less than once a month (how many times per months...............................................?)
- Once a month
- Once every 2 months
- More than once every 2 months
- I don’t know
- It’s not a set time interval
18. (If you answered d, e, f, and g at question 17)
Why do you repeat the INR dosing after longer time intervals?
- Financial reasons
- The long distance between where I live and the nearest laboratory
- I forgot my ACT dosage
- I don’t consider it to be important
19. Who adjusts your ACT dosage after the INR analysis, if needed?
- Cardiologist
- Internal medicine doctor
- Neurologist
- General practitioner
- Other...............................................
- I adjust it myself
20. What were you told the emergency INR is?
- Over 3
- Over 4
- Over 5
- Over 6
- I don’t know
21. Have you heard of devices for INR monitoring at home?
- Yes
- No
22. Do you own such a device?
- Yes
- No
23. Have you had any hemorrhage in the time you have been undergoing ACT?
- Yes
- No
24. If yes, what type of hemorrhage have you had?
- Epistaxis
- Digestive hemorrhage (red blood in the stool; black color stools; vomiting of red blood or blood clots)
- Hematuria
- Hematoma
- Other...............................................
25. Do you know the INR value at the moment of the hemorrhage? ...............................................
26. If you could choose between more AC drugs what would be the determining factor?
- The longer period for INR dosing (or never having to do it at all)
- The price of the drug
- The safety of the drug
INR on current admission:
For atrial fibrillation:
CHA2DS2-VASc:
HAS-BLED:
Other comments:
Abbreviations: ACT, anticoagulant therapy; AC, anticoagulant; EF, ejection fraction; INR, international normalized ratio; PTE, pulmonary thromboembolism; VT, venous thrombosis.
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.