Back to Journals » Neuropsychiatric Disease and Treatment » Volume 13
Predicting treatment outcomes of major depressive disorder by early improvement in painful physical symptoms: a pooled analysis of double-blind, placebo-controlled trials of duloxetine
Authors Tokuoka H , Nishihara M, Fujikoshi S, Yoshikawa A, Kuga A
Received 2 June 2017
Accepted for publication 21 August 2017
Published 25 September 2017 Volume 2017:13 Pages 2457—2467
DOI https://doi.org/10.2147/NDT.S143093
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Hirofumi Tokuoka,1 Makoto Nishihara,2 Shinji Fujikoshi,3 Aki Yoshikawa,4 Atsushi Kuga1
1Bio-Medicine, Medicines Development Unit Japan, Eli Lilly Japan K.K., Kobe, 2Multidisciplinary Pain Center, Aichi Medical University, Nagakute, Aichi, 3Statistical Science, 4Scientific Communications, Medicines Development Unit Japan, Eli Lilly Japan K.K., Kobe, Japan
Objective: We determined if early improvement in painful physical symptoms (PPS) can be a predictor of remission in the treatment of major depressive disorder (MDD).
Methods: We included randomized, double-blind, parallel-group clinical trials of duloxetine (40–60 mg/day) versus placebo for the acute treatment of MDD with associated PPS. Only those studies using the Montgomery–Åsberg Depression Rating Scale (MADRS) and the Brief Pain Inventory – Short Form (BPI-SF) were included. Three studies met all criteria and included male or female outpatients aged ≥18 years who met the diagnostic criteria for MDD, had a MADRS total score ≥20, and had at least moderate pain (BPI-SF average pain score ≥3). Positive predictive values (PPVs) and negative predictive values (NPVs) of early improvement in PPS for remission were analyzed. PPVs were the proportion of patients with remission (MADRS total score ≤10) at week 8 out of patients who experienced early improvement in BPI-SF average pain score (≥30% decrease from baseline at week 1, 2, or 4). NPVs were the proportion of patients without remission (MADRS total score >10) at week 8 out of patients who did not experience early improvement in PPS.
Results: Data from 1,320 patients were analyzed (duloxetine N=641 and placebo N=679). The overall remission (MADRS total score ≤10 at week 8) rate for the duloxetine group was significantly higher than the placebo group (38.5% vs 21.8%; P<0.0001). For both treatment groups, PPVs of early improvement in BPI-SF (30% improvement from baseline) were higher than the overall remission rate for all weeks examined (weeks 1, 2, and 4); in general, NPVs of early improvement in BPI-SF for nonremission were higher than the overall nonremission rate.
Conclusion: Early improvement in PPS can be a useful clinical indicator of subsequent treatment outcome for MDD patients with associated PPS.
Keywords: Brief Pain Inventory, Montgomery–Åsberg Depression Rating Scale, pain, predictor, remission
Introduction
Although major depressive disorder (MDD) is one of the leading causes of years lived with disability,1 the remission rate of MDD remains low.2 To guide efforts to achieve a higher rate of remission in clinical practice, many different aspects of predicting treatment outcome in MDD have been studied. Some baseline characteristics have been demonstrated to be associated with the treatment outcome. In the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study,3 subjects who were Caucasian, female, and/or employed had higher remission rates, as assessed by the Hamilton Depression Rating Scale (HAM-D). Subjects who had more education and/or larger incomes also had higher remission rates. Lower remission rates were associated with longer episodes of depression, more general medical and psychiatric disorders (especially, anxiety disorders or drug abuse), more impairment in work and social adjustment, and lower quality of life.3
More recently, prediction of MDD treatment outcome by early response has been extensively investigated. It has been reported that early improvement in the HAM-D total score or subscale scores during the first 2 weeks of treatment could contribute to the correct prediction of remission later in treatment.4–6 A recent report suggests that improvement in the HAM-D retardation subscale even during the first week could help predict subsequent remission.7
Patients with MDD commonly experience painful physical symptoms (PPS).8 Unfortunately, in addition to the burden of the pain itself, PPS appear to have a negative impact on MDD. PPS severity is closely associated with depression severity at baseline.9 The presence of PPS prior to treatment and the severity of PPS are both associated with poorer treatment outcomes.8,10–14 In addition, an association has been found between PPS improvement and depression improvement in cohort studies11,15,16 and case–control studies.17 Pain can negatively affect efforts to treat MDD with antidepressants, reducing the probability of achieving depression remission/response.18
Fava et al19 reported that a ≥50% reduction in pain scores 2 weeks after treatment initiation was associated with a higher probability of remission (HAM-D total score ≤7) at the end point. This result implies that the early improvement (within 2 weeks) in PPS is associated with subsequent remission of MDD. However, not all patients included in the analysis experienced pain at baseline, thus compromising the sensitivity of evaluating the association. In addition, Fava et al19 used a visual analog scale (VAS) for assessing PPS, which is a simple tool to administer but can be highly subjective. Currently, many other scales for assessment of pain are available,20,21 and more developed scales such as the Brief Pain Inventory – Short Form (BPI-SF) may better capture the severity of PPS and its improvement.
Duloxetine, a potent and selective inhibitor of serotonin and norepinephrine reuptake in the central nervous system in vitro and in vivo,22 has been approved for the treatment of MDD and various types of pain (diabetic peripheral neuropathic pain, fibromyalgia, and chronic musculoskeletal pain) in the US and other countries. Duloxetine showed effectiveness on PPS in acute treatment phases of double-blind, placebo-controlled trials.23,24 In addition, Harada et al,25 in a pooled analysis of patients with MDD and PPS, found that duloxetine would directly improve PPS early in treatment. However, this result is not direct evidence that early improvement in PPS increases the likelihood of MDD remission.
Therefore, the purpose of the present analysis was to determine if early improvement in PPS, as measured using the BPI-SF, can be a predictor of remission when MDD patients with PPS are treated with duloxetine.
Methods
Data sources, study selection, and patients
The studies used in the present pooled analysis have been previously described.25 Briefly, we screened the Eli Lilly and Company clinical trial database to identify studies that met the following criteria: 1) randomized, double-blind, parallel-group clinical trials of duloxetine (40–60 mg/day) versus placebo for the acute treatment of MDD with associated PPS and 2) use of the Montgomery–Åsberg Depression Rating Scale (MADRS) for depressive symptoms and the BPI-SF for pain symptoms. As a result of database screening, three studies were identified that met all criteria,15,26,27 and we included these studies for the pooled analysis. In each of these studies, data were collected at baseline and on post-baseline weeks 1, 2, 4, and 8 at minimum. Each study included male or female outpatients aged ≥18 years who met the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition, Text Revision28 criteria for MDD and had a MADRS total score ≥20, at least moderate pain (based on BPI-SF average pain score ≥3), and a Clinical Global Impression of Severity score ≥4. Exclusion criteria included a current diagnosis of an Axis I disorder (other than MDD); history of bipolar disorder, schizophrenia, or other psychotic disorders; and any diagnosed pain syndrome as per medical history26 or presence of pain of a known origin except MDD.14,27 The protocols for these studies were approved by the appropriate ethical review boards for each of the study centers. Patients gave written informed consent before participating in the studies. The studies were all conducted in accordance with the regulatory standards in each country and conformed to the standards dictated by Good Clinical Practice and the Declaration of Helsinki.29 The studies were registered at ClinicalTrials.gov (NCT00191919, NCT01070329, and NCT01000805).
Treatment
Enrolled patients in all three studies were randomized to an oral dose of duloxetine 60 mg/day or placebo. Patients assigned to duloxetine were started on 30 mg/day for 1 week and then were titrated up to duloxetine 60 mg/day for 7 weeks.
Assessments
Depression severity was assessed using the MADRS total score.30 The MADRS measures 10 core symptoms of depression on a scale of 0–6 for a maximum total score of 60. Remission of MDD was defined as an MADRS total score ≤10 at week 8. Response to treatment was defined as a ≥50% decrease in MADRS total score from baseline at week 8.
PPS were evaluated using the BPI-SF, which was designed to assess pain intensity and its interference with activities of daily living. The questionnaire uses a 0 (no pain or does not interfere) to 10 (pain as severe as you can imagine or completely interferes) scale.31 For the purposes of the present investigation, responses to BPI-SF item 5, 24-hour average pain score, were used, since this was the primary outcome measure for pain used in the three studies.15,26,27 Moreover, the single-item, average pain score is commonly used in randomized clinical trials for the assessment of pain relief,32–36 and its use is supported by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) recommendations for clinical pain trials.20,37,38
Early improvement in PPS was defined as a ≥30% decrease in the 24-hour average pain item on the BPI-SF at week 1, 2, or 4 compared to baseline. We used 30% improvement in BPI-SF from baseline because 30% reduction was reported to be a clinically important difference in an 11-point pain intensity numerical rating scale37,39 and 30% is often used in clinical trials of chronic pain disorders.32,35 As a comparison, early improvement in depressive symptoms (at week 1, 2, or 4 post baseline) was defined as a decrease in MADRS total score of 30% from baseline.40
Statistical methods
All randomized patients with MADRS total score ≥20 and with BPI-SF average pain score ≥3 who received placebo or duloxetine (40–60 mg/day) were included in the analyses. Patients with no baseline MADRS or BPI-SF data or no post-baseline MADRS or BPI-SF data were excluded from the analyses.
For the predictor analysis, positive predictive values (PPVs) and negative predictive values (NPVs) were calculated. PPV is the proportion of patients with a positive outcome (remission or response) out of those patients with early improvement on the BPI-SF. NPV is the proportion of patients without a positive outcome out of those patients without early improvement on the BPI-SF.
PPVs and NPVs based on early improvement in MADRS scores were also calculated. A predictor analysis was conducted for both treatment groups separately. Last observation carried forward was used for missing week 8 data. All analyses were post hoc.
Subgroup analysis on depression severity was carried out by dividing patients into three groups based on MADRS total scores at baseline: mild depression (≤24), moderate depression (25–30), and severe depression (≥31).41 Note that one of the inclusion criteria for these three studies was having a MADRS score ≥20; therefore, the mild depression group had MADRS score ≥20 and ≤24.
Results
Patient demographics, baseline characteristics, and patient disposition
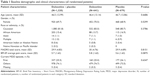
Data from a total of 1,320 patients were analyzed (duloxetine N=641 and placebo N=679). Patient demographics and baseline characteristics are presented in Table 1. Patients were mostly female (69.7%) and Caucasian (81.8%), and the mean age was 46.5 years. Mean baseline MADRS total score (standard deviation [SD]) was 29.9 (4.83) and BPI-SF average pain score (SD) was 5.7 (1.63); 25.5% of patients were experiencing their first MDD episode. Demographic and baseline characteristics were similar for the treatment groups (Table 1). The dispositions of patients in the duloxetine and placebo groups are shown in Table 2. At the end of treatment, early discontinuations were similar for the two groups (duloxetine 15.9% and placebo 16.2%; Table 2).
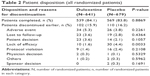  | Table 2 Patient disposition (all randomized patients) |
Predictability of remission by early improvement in PPS and depressive symptoms
The overall remission rate for the duloxetine group was significantly higher than that for the placebo group (duloxetine 38.5% and placebo 21.8%; P<0.0001). To assess how early improvement in PPS or MADRS is useful for the prediction of achieving remission at week 8, PPVs and NPVs were assessed (Figure 1). PPVs (Figure 1A) and NPVs (Figure 1B) of early improvement in PPS for remission (defined as a MADRS score ≤10 at week 8) in the duloxetine group are determined by ≥30% decrease in BPI-SF and MADRS scores at week 1, 2, or 4.
PPVs of early improvement in BPI-SF scores for remission were higher than the overall remission rate (38.5%) by >10%. PPVs of early improvement in BPI-SF scores were, as expected, generally lower than those of the MADRS. Note that the number of patients with early improvement increased over time. PPVs for remission in the duloxetine group changed relatively little between weeks 1, 2, and 4. The NPV of early improvement in BPI-SF scores for remission at week 1 was similar to the overall nonremission rate (61.5%) but increased at later time points.
PPVs and NPVs of early improvement in PPS for remission in the placebo group are shown in Figure 1C and D, respectively. As with the duloxetine group, PPVs were higher for the MADRS than for the BPI-SF, but both were higher than the overall remission rate (21.8%). NPVs at week 1 were nearly the same as the nonremission rate (78.2%) but improved in later weeks.
Thus, early improvement in PPS even from week 1 can be used for prediction of remission in both treatment groups. In addition, lack of improvement in PPS at week 2 or 4 can also be useful for predicting nonremission.
Predictability of treatment response by early improvement in PPS and depressive symptoms
The overall treatment response rate for the duloxetine group was significantly higher than that for the placebo group (duloxetine 53.4% and placebo 33.6%; P<0.0001). The PPVs and NPVs for treatment response (defined as a ≥50% decrease from baseline MADRS score at week 8) are shown in Figure 2. Overall, predictability scores for treatment response mirrored those for remission. PPVs of early improvement in BPI-SF scores for treatment response were higher than the overall treatment response rate (53.4%) by >10% (Figure 2A). PPVs of early improvement in BPI-SF scores for treatment response were, as expected, generally lower than those of the MADRS. The NPV for the BPI-SF at week 1 was similar to the overall treatment nonresponse rate (46.6%) but was higher at later time points, indicating that predictability was improving over time (Figure 2B). The same tendency in PPV and NPV was observed in the placebo group (Figure 2C and D). These data suggest that early improvement in PPS can also be useful for the prediction of treatment response.
Depression severity and prediction of remission by early improvement in PPS
The PPVs and NPVs for remission by early improvement in BPI-SF and MADRS scores were further analyzed by stratification based on baseline depression severity in the duloxetine group (Figure 3). Patients were divided into three groups, based on MADRS total scores: mild depression (≤24), moderate depression (25–30), and severe depression (≥31) at baseline. The overall remission rate in each group was 62.0%, 34.5%, and 38.4% for mild, moderate, and severe groups, respectively, as estimated from the analysis set at week 1. Compared to the overall remission rate for each subgroup, PPVs of early improvement in BPI-SF were higher at all time points in moderate and severe groups, while in the mild group, PPVs were higher at weeks 2 and 4 (Figure 3A).
The nonremission rate in each group was 38.0%, 65.5%, and 61.6% for mild, moderate, and severe groups, respectively. Compared to the overall nonremission rate for each subgroup, NPVs of early improvement in BPI-SF were not significantly different at week 1 but were higher at later time points (Figure 3B). PPVs and NPVs of the MADRS were mostly higher than those of the BPI-SF in all severity groups as observed in the whole group (Figure 3C and D). Collectively, the predictive usefulness of the BPI-SF was generally confirmed across the range of depression severities studied.
Discussion
We have demonstrated that early improvement in PPS can be a predictor for remission and response in MDD. Our data not only support the idea that PPS and depression are closely related but also suggest that PPS improvement could be a sign of subsequent depression state improvement in MDD patients with PPS.
The usefulness of this measure is evident as early as week 1, when the 50% PPV for remission and 69% PPV for response observed with early improvement in PPS were better than the overall remission rate (38.5%) and response rate (53.4%) in the duloxetine group. Although early improvement in the MADRS was found to be better for prediction, this was expected as the same scale was used for both predictive value and outcome measurement. It is striking that improvement in PPS as early as week 1 was associated with subsequent remission, even though PPS is not one of the 10 items of the MADRS.
The PPVs of early improvement in the BPI-SF scores for response and remission did not change very much from week 1 to 4, while the number of patients experiencing early improvement in BPI-SF increased. NPV was not evidently superior to overall nonremission rate at week 1, but, in general, the value increased over time. These changes in PPV and NPV suggest that early improvement in PPS, regardless of timing, can be a sign of positive outcome. However, when treating with duloxetine, it is worth waiting at least 4 weeks to see if PPS improves before predicting a negative outcome based on a lack of improvement.
Our results regarding the predictability of remission by early improvement in PPS are partly consistent with a previous report by Fava et al,19 where it was reported that 35.4% of early responders (≥50% improvement in VAS score within 2 weeks) achieved remission of depressive symptoms, compared with 20.9% of patients without early pain response. These values are lower than those found in our study, most likely because their study population was not selective for patients with PPS, while our study population was restricted to patients with associated PPS. In addition, their estimation was based on a mixture of patients who were treated with duloxetine and placebo.
Another reason for the slight discrepancy between our results and those of Fava et al19 could be the difference in assessment scales. Fava et al19 used the VAS to measure PPS and the HAM-D to measure MDD symptoms. We used the BPI-SF to assess PPS because it is a more specialized scale for pain and is now commonly used for evaluation of PPS.15,26,27,42 Because of the focus on PPS in the present analysis, the PPVs and NPVs we demonstrated should be more appropriate estimations for patients with MDD having PPS and being treated with duloxetine.
Notably, early improvement in BPI-SF score even at week 1, which is earlier than reported in Fava et al,19 can predict duloxetine treatment outcome. This treatment period in our study is quite early even compared with recent reports on early prediction using HAM-D scores at week 2.5,6
At least one observational study supports the relationship between early improvement in PPS and remission. Schneider et al16 showed that in patients treated with duloxetine, a 50% reduction in VAS overall pain score after 2 or 4 weeks was associated with greater improvement in depressive symptoms (as measured using the Kurz-Skala Stimmung/Aktivierung [KUSTA]) after 6 months. This finding partly complements our study by showing that the association between early improvement in PPS and remission of depression can be as long as 6 months.
Results of PPV and NPV derived from the placebo group showed the association of early improvement in PPS with remission and response, even in the absence of an active drug. Although the remission rate was lower in the placebo group than in the duloxetine group, PPV for remission at week 1 (40%) was much higher than the placebo remission rate (21.8%). Provided that the placebo response is thought to be a manifestation of resilience,43 our data imply that early improvement in PPS can be a part of the natural process of recovery from depression.
When patients were subgrouped by severity of MDD symptoms by baseline MADRS score, patients with mild MDD showed a somewhat different pattern of PPV and NPV (higher PPV and lower NPV) from those of the moderate and severe subgroups. These differences are most likely because the overall remission rate in the mild subgroup was higher than other subgroups. In the moderate and severe subgroups, PPVs and NPVs were consistently better than the overall remission rate and overall nonremission rate, respectively. This tendency was also observed in the mild group, except at week 1. The apparently weaker association in the mild groups than in the moderate and severe groups may be due to a relatively smaller sample size or lower mean baseline BPI-SF scores. Alternatively, it may be because PPS in the mild depression group is not as closely coupled with other depression symptoms as in the moderate or severe depression groups. Even though there is some variation depending on baseline severity of depression, PPV and NPV can be useful for assessing treatment outcome across a broad range of depression severity.
Depressive disorders show many different types of symptoms. We recently reported that the improvement in many depression symptoms assessed by HAM-D can be useful in predicting the outcome of depressive disorder.44 Our results indicate that early improvement in PPS can be one of the useful signs for predicting subsequent remission. This sign is clinically relevant, given that PPS is often observed in MDD patients8 and pain severity is higher in patients with MDD than in healthy controls.45 Thus, PPS should be one of the symptoms that is routinely given attention during the treatment of MDD.
There are limitations to the present analysis that should be considered. First, our patient sample was mostly Caucasian (81.8%) and female (69.7%). Potential differences due to gender, ethnicity, or cultural considerations may be underrepresented in this sample. Second, BPI-SF average pain may not fully represent the complex character and severity of PPS, although it is commonly used for evaluation of PPS. Third, we only examined data from the acute phase of treatment and long-term results may differ. Fourth, because this is a post hoc analysis, results must be interpreted with caution. Fifth, only patients treated with duloxetine 60 mg/day or placebo were included in this analysis. Higher or lower doses of duloxetine and other antidepressants may have different effects on both PPS and symptoms of depression. Finally, the integrated database we used included only studies that were conducted by Eli Lilly and Company or its partners outside Japan; therefore, sponsorship bias may not be completely ruled out.
Conclusion
We recently reported that duloxetine directly improves PPS during the early treatment phase, while other depressive symptoms are improved partly by indirect effect through PPS improvement in MDD patients treated with duloxetine.25 Together with this report, the present results suggest that early improvement in PPS can be a positive sign for remission of depression, and close attention can be paid to PPS from the earliest phase of treatment. PPS improvement can be a useful early clinical indicator in assessing treatment effectiveness for remission in MDD patients.
Acknowledgments
This study was sponsored by Eli Lilly Japan K.K., manufacturer/licensee of Cymbalta®, which was involved in the preparation of the manuscript. Medical writing assistance was provided by Leah Hains, PhD, and Rodney Moore, PhD, of in Ventiv Health Clinical, LLC, funded by Eli Lilly Japan K.K. Statistical support was provided by Ralf Jaeger, PhD, a full-time employee of Accovion GmbH.
Author contributions
All authors (HT, MN, SF, AY, AK) contributed to the conception of the study, interpretation of the data, and drafting and critical revision of the manuscript and provided final approval of the manuscript.
Disclosure
HT, SF, AY, and AK are employees of Eli Lilly Japan K.K. MN has received speaker’s honoraria from Eli Lilly Japan K.K.; Pfizer Inc.; Shionogi & Co., Ltd.; Otsuka Pharmaceutical Co., Ltd.; Nippon Zoki Pharmaceutical Co., Ltd.; Meiji Seika Pharma Co., Ltd.; Hisamitsu Pharmaceutical Co., Inc.; Mochida Pharmaceutical Co., Ltd.; Mitsubishi Tanabe Pharma Corporation; and Yoshitomiyakuhin Corporation and grant/research support from Astellas Pharma Inc.; Eisai Co., Ltd.; Shionogi & Co., Ltd.; Daiichi Sankyo Co., Ltd.; St Jude Medical Japan Co., Ltd.; Hisamitsu Pharmaceutical Co., Inc.; Medtronic Japan, Inc.; Pfizer Inc.; Kyowa Hakko Kirin Co., Ltd.; Taisho Toyama Pharmaceutical Co., Ltd.; and Tsumura & Co. The authors report no other conflicts of interest in this work.
References
Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. | ||
Rush AJ. Limitations in efficacy of antidepressant monotherapy. J Clin Psychiatry. 2007;68(suppl 10):8–10. | ||
Trivedi MH, Rush AJ, Wisniewski SR, et al; STAR*D Study Team. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28–40. | ||
Henkel V, Seemüller F, Obermeier M, et al. Does early improvement triggered by antidepressants predict response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J Affect Disord. 2009;115(3):439–449. | ||
Katz MM, Meyers AL, Prakash A, Gaynor PJ, Houston JP. Early symptom change prediction of remission in depression treatment. Psychopharmacol Bull. 2009;42(1):94–107. | ||
Szegedi A, Jansen WT, van Willigenburg AP, van der Meulen E, Stassen HH, Thase ME. Early improvement in the first 2 weeks as a predictor of treatment outcome in patients with major depressive disorder: a meta-analysis including 6562 patients. J Clin Psychiatry. 2009;70(3):344–353. | ||
Harada E, Kato M, Fujikoshi S, Wohlreich MM, Berggren L, Tokuoka H. Changes in energy during treatment of depression: an analysis of duloxetine in double-blind placebo-controlled trials. Int J Clin Pract. 2015;69(10):1139–1148. | ||
Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66(1):17–22. | ||
Brnabic A, Lin C, Monkul ES, Dueñas H, Raskin J. Major depressive disorder severity and the frequency of painful physical symptoms: a pooled analysis of observational studies. Curr Med Res Opin. 2012; 28(12):1891–1897. | ||
Karp JF, Scott J, Houck P, Reynolds CF 3rd, Kupfer DJ, Frank E. Pain predicts longer time to remission during treatment of recurrent depression. J Clin Psychiatry. 2005;66(5):591–597. | ||
Kroenke K, Shen J, Oxman TE, Williams JW Jr, Dietrich AJ. Impact of pain on the outcomes of depression treatment: results from the RESPECT trial. Pain. 2008;134(1–2):209–215. | ||
Ang QQ, Wing YK, He Y, et al. Association between painful physical symptoms and clinical outcomes in East Asian patients with major depressive disorder: a 3-month prospective observational study. Int J Clin Pract. 2009;63(7):1041–1049. | ||
Leuchter AF, Husain MM, Cook IA, et al. Painful physical symptoms and treatment outcome in major depressive disorder: a STAR*D (sequenced treatment alternatives to relieve depression) report. Psychol Med. 2010;40(2):239–251. | ||
Lin CH, Lane HY, Chen CC, Juo SH, Yen CF. Pain has a strong negative impact on the fluoxetine response in hospitalized patients with major depressive disorder. Clin J Pain. 2011;27(9):805–810. | ||
Gaynor PJ, Gopal M, Zheng W, Martinez JM, Robinson MJ, Marangell LB. A randomized placebo-controlled trial of duloxetine in patients with major depressive disorder and associated painful physical symptoms. Curr Med Res Opin. 2011;27(10):1849–1858. | ||
Schneider E, Linden M, Weigmann H, et al. Early reduction in painful physical symptoms is associated with improvements in long-term depression outcomes in patients treated with duloxetine. BMC Psychiatry. 2011;11:150. | ||
Arnold LM, Meyers AL, Sunderajan P, et al. The effect of pain on outcomes in a trial of duloxetine treatment of major depressive disorder. Ann Clin Psychiatry. 2008;20(4):187–193. | ||
Fishbain DA, Cole B, Lewis JE, Gao J. Does pain interfere with antidepressant depression treatment response and remission in patients with depression and pain? An evidence-based structured review. Pain Med. 2014;15(9):1522–1539. | ||
Fava M, Mallinckrodt CH, Detke MJ, Watkin JG, Wohlreich MM. The effect of duloxetine on painful physical symptoms in depressed patients: do improvements in these symptoms result in higher remission rates? J Clin Psychiatry. 2004;65(4):521–530. | ||
Dworkin RH, Turk DC, Farrar JT, et al; IMMPACT. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1–2):9–19. | ||
Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17–24. | ||
Bymaster FP, Lee TC, Knadler MP, Detke MJ, Iyengar S. The dual transporter inhibitor duloxetine: a review of its preclinical pharmacology, pharmacokinetic profile, and clinical results in depression. Curr Pharm Des. 2005;11(12):1475–1493. | ||
Ball SG, Desaiah D, Spann ME, et al. Efficacy of duloxetine on painful physical symptoms in major depressive disorder for patients with clinically significant painful physical symptoms at baseline: a meta-analysis of 11 double-blind, placebo-controlled clinical trials. Prim Care Companion CNS Disord. 2011;13(6):CC.11r01181. | ||
Ball SG, Desaiah D, Zhang Q, Thase ME, Perahia DG. Efficacy and safety of duloxetine 60 mg once daily in major depressive disorder: a review with expert commentary. Drugs Context. 2013;2013:212245. | ||
Harada E, Tokuoka H, Fujikoshi S, et al. Is duloxetine’s effect on painful physical symptoms in depression an indirect result of improvement of depressive symptoms? Pooled analyses of three randomized controlled trials. Pain. 2016;157(3):577–584. | ||
Brecht S, Courtecuisse C, Debieuvre C, et al. Efficacy and safety of duloxetine 60 mg once daily in the treatment of pain in patients with major depressive disorder and at least moderate pain of unknown etiology: a randomized controlled trial. J Clin Psychiatry. 2007;68(11): 1707–1716. | ||
Gaynor PJ, Gopal M, Zheng W, et al. Duloxetine versus placebo in the treatment of major depressive disorder and associated painful physical symptoms: a replication study. Curr Med Res Opin. 2011;27(10): 1859–1867. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. | ||
World Medical Association General Assembly. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Int Bioethique. 2004;15(1):124–129. | ||
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. | ||
Cleeland CS. Measurement of pain by subjective report. In: Chapmen CR, Loeser JD, editors. Issues in Pain Measurement, Advances in Pain Research and Therapy. Vol. 12. New York: Raven Press; 1989:391–403. | ||
Arnold LM, Rosen A, Pritchett YL, et al. A randomized, double-blind, placebo-controlled trial of duloxetine in the treatment of women with fibromyalgia with or without major depressive disorder. Pain. 2005;119(1–3):5–15. | ||
Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs placebo in patients with painful diabetic neuropathy. Pain. 2005;116(1–2): 109–118. | ||
Russell IJ, Mease PJ, Smith TR, et al. Efficacy and safety of duloxetine for treatment of fibromyalgia in patients with or without major depressive disorder: results from a 6-month, randomized, double-blind, placebo-controlled, fixed-dose trial. Pain. 2008;136(3):432–444. | ||
Skljarevski V, Zhang S, Desaiah D, et al. Duloxetine versus placebo in patients with chronic low back pain: a 12-week, fixed-dose, randomized, double-blind trial. J Pain. 2010;11(12):1282–1290. | ||
Tesfaye S, Wilhelm S, Lledo A, et al. Duloxetine and pregabalin: high-dose monotherapy or their combination? The “COMBO-DN study” – a multinational, randomized, double-blind, parallel-group study in patients with diabetic peripheral neuropathic pain. Pain. 2013;154(12):2616–2625. | ||
Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–121. | ||
Turk DC, Dworkin RH, Burke LB, et al; Initiative on Methods, Measurement and Pain Assessment in Clinical Trials. Developing patient-reported outcome measures for pain clinical trials: IMMPACT recommendations. Pain. 2006;125(3):208–215. | ||
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. | ||
Nakajima S, Uchida H, Suzuki T, et al. Is switching antidepressants following early nonresponse more beneficial in acute-phase treatment of depression? A randomized open-label trial. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(8):1983–1989. | ||
Stewart TD, Hatch A, Largay K, et al. Effect of symptom severity on efficacy and safety of aripiprazole adjunctive to antidepressant monotherapy in major depressive disorder: a pooled analysis. J Affect Disord. 2014;162:20–25. | ||
Brannan SK, Mallinckrodt CH, Brown EB, Wohlreich MM, Watkin JG, Schatzberg AF. Duloxetine 60 mg once-daily in the treatment of painful physical symptoms in patients with major depressive disorder. J Psychiatr Res. 2005;39(1):43–53. | ||
Stassen HH, Angst J, Hell D, Scharfetter C, Szegedi A. Is there a common resilience mechanism underlying antidepressant drug response? Evidence from 2848 patients. J Clin Psychiatry. 2007;68(8):1195–1205. | ||
Tokuoka H, Takahashi H, Ozeki A, et al. Trajectories of depression symptom improvement and associated predictor analysis: an analysis of duloxetine in double-blind placebo-controlled trials. J Affect Disord. 2016;196:171–180. | ||
Kishi T, Matsuda Y, Mukai T, et al. A cross-sectional survey to investigate the prevalence of pain in Japanese patients with major depressive disorder and schizophrenia. Compr Psychiatry. 2015;59:91–97. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.