Back to Journals » International Journal of General Medicine » Volume 15
Predicting New-Onset Postoperative Atrial Fibrillation Following Isolated Coronary Artery Bypass Grafting: Development and Validation of a Novel Nomogram
Authors Fan K, Chen L, Liu F, Ding X, Yan P , Gao M, Yu W, Liu H, Yu Y
Received 9 November 2021
Accepted for publication 7 January 2022
Published 26 January 2022 Volume 2022:15 Pages 937—948
DOI https://doi.org/10.2147/IJGM.S346339
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Kangjun Fan,1 Liang Chen,1 Fei Liu,2 Xiaohang Ding,1 Pengyun Yan,1 Mingxin Gao,1 Wenyuan Yu,1 Hongli Liu,1 Yang Yu1
1Department of Cardiac Surgery, Beijing Anzhen Hospital, Capital Medical University, Beijing, 100029, People’s Republic of China; 2Department of Biology, Faculty of Science, Hong Kong Baptist College, Kowloon Tong, Hong Kong, People’s Republic of China
Correspondence: Yang Yu, Tel +86-10-64456868, Fax +86-10-84005030, Email [email protected]
Objective: To select variables associated with new-onset postoperative atrial fibrillation (POAF) following isolated coronary artery bypass grafting (CABG) and develop a nomogram for risk prediction in a Chinese population.
Methods: The study retrospectively enrolled 4854 consecutive patients undergoing isolated CABG from February 2018 to September 2019, they were divided into derivation cohort and validation cohort with a 3:1 ratio according to the order of operation date. In the derivation cohort, significant variables were selected by use of the multivariate logistic backward stepwise regression analysis and a nomogram model was built on the strength of the results. The model performance was assessed in terms of discrimination and calibration. Besides, we compared the discriminative ability for POAF of the nomogram with established prediction models (CHA2DS2-VASc and HATCH scores) in the two cohorts.
Results: POAF occurred in 1025 (28.2%) out of 3641 patients in the derivation cohort, and in 337 (27.8%) out of 1213 patients in the validation cohort. A nomogram, composed of eight prognostic variables, namely age, sex, heart rate, hypertension, left ventricular ejection fraction (LVEF) < 50%, left atrial diameter (LAD) > 40mm, estimated glomerular filtration rate (eGFR) level, and on-pump surgery, was constructed from the derivation cohort. The nomogram had substantial discriminative ability in derivation and validation cohorts with the area under the receiver operating characteristic curves (AUCs) of 0.661 (95% confidence interval, 0.642– 0.681) and 0.665 (95% confidence interval, 0.631– 0.699), respectively, and showed well-fitted calibration curves. Compared with CHA2DS2-VASc, HATCH and POAF scores, respectively, the nomogram had superior discrimination performance.
Conclusion: We constructed a novel nomogram with improved accuracy for predicting the risk of POAF following isolated CABG, which might help clinicians predict individual probability of POAF and achieve effective prophylaxis.
Keywords: coronary artery bypass grafting, atrial fibrillation, high-risk patients, prediction, nomogram
Introduction
New-onset postoperative atrial fibrillation (POAF), a common complication with an incidence of 18% to 33%, typically develops within 4 days after isolated coronary artery bypass grafting (CABG), and lasts several hours.1–3 Considerable evidence has confirmed that POAF following CABG is an independent predictor of worse outcomes, including early outcomes such as renal failure, infective complications, a prolonged ventilation,4 and long-term outcomes such as mortality (6 years, hazard ratio: 1.21, 95% confidence interval: 1.12–1.32),3 stroke (10 years, hazard ratio: 1.53, 95% confidence interval: 1.06–2.23).2 Therefore, effective prophylaxis may reduce associated risks of adverse outcomes. However, the majority of patients undergoing CABG remain in sinus rhythm, administering prophylactic medication to patients routinely might expose most patients without indications to the risk of drug side effects and unnecessary expenses.5,6
Consequently, identifying patients prone to develop POAF and making targeted prevention could be cost-effective. Existing risk models, such as CHA2DS2-VASc, HATCH and POAF scores, have been verified useful in predicting new-onset POAF by studies including patients undergoing different types of cardiac surgery (which carry different risks of POAF).7–9 Unfortunately, a simple, convenient and effective tool to predict POAF following isolated CABG has not yet been identified.
The nomogram has been proved to be a reliable predictive tool with the ability to generate an individual probability of a clinical event by graphically representing the effect of each predictor on the outcome.10 The present study aimed to identify the combination of variables that resulted in a highly accurate prediction of POAF and derive an efficient and reliable nomogram to predict POAF in patients undergoing isolated CABG.
Methods
Study Population
Data of consecutive patients undergoing isolated CABG at Beijing Anzhen Hospital, Capital Medical University from February 2018 to September 2019, were collected retrospectively. The inclusion criteria were as follows: patients with coronary artery disease (CAD) confirmed by coronary angiography undergoing elective first CABG; patients aged >18 years. The exclusion criteria were as follows: patients with incomplete clinical data; patients with previous AF; patients complicated with moderate or more severe valve disease, primary myocardiopathy, congenital heart disease, or other cardiac diseases; patients undergoing any other major cardiac procedure with the exception of coronary endarterectomy.
In total, 4854 eligible patients were enrolled, then they were divided into derivation cohort and validation cohort with a 3:1 ratio according to the order of operation date. The derivation cohort was used to develop the model, while the validation cohort was applied to validate the model. This study was conducted following the Declaration of Helsinki of the World Medical Association and ethical approval was obtained from the Institutional Ethics Committee of Beijing Anzhen Hospital (Approval No. 2021101X). Given the retrospective nature and anonymity of the present study, no informed consent was required. All patients’ identifiable information were hidden, and anyone’s identity cannot be deduced from the context.
Outcome and Definitions
The primary outcome was the development of new-onset POAF during hospitalization. POAF was defined as any documented AF episode lasting >30 seconds captured on a standard 12-lead electrocardiogram or cardiac telemetry, or that required medical treatment. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation: eGFR = 141 × min (Scr/κ, 1)α × max (Scr/κ, 1)−1.209 × 0.993Age × 1.018 [if female], where Scr is serum creatinine, κ is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, min indicates the minimum of Scr/κ or 1, and max indicates the maximum of Scr/κ or 1. CHA2DS2-VASc score (age ≥75 years, 2 points; 65 to 74 years, 1 point; female sex, 1 point; history of heart failure, 1 point; hypertension, 1 point; stroke/transient ischemic attack, 2 points; diabetes, 1 point; and peripheral vascular disease, 1 point), HATCH score (hypertension, 1 point; age ≥75 years, 1 point; stroke or transient ischemic attack, 2 points; chronic obstructive pulmonary disease, 1 point; and heart failure, 2 points) and POAF score (age, 60 to 69 years, 1 point; 70 to 79 years, 2 points; ≥80 years, 3 points; chronic obstructive pulmonary disease, 1 point; eGFR <15 mL/min/1.73 m2 or dialysis, 1 point; emergency operation, 1 point; preoperative intra-aortic balloon pump, 1 point; left ventricular ejection fraction <30%, 1 point; and any heart valve surgery, 1 point) were calculated for each patient.
Constructing the Nomogram
Data of patients with and without POAF were compared in the derivation cohort, and the screening criterion for risk factors for POAF was P value <0.1 in univariable analysis. All potential variables included in the multivariable analysis were subjected to a correlation matrix for analysis of multicollinearity, afterwards multivariate logistic backward stepwise regression (likelihood ratio) analysis was performed to further screen out the significant risk factors for POAF on a criterion of P value <0.05. A nomogram model was built on the strength of the results of multivariate analysis in the derivation cohort by the package of rms in R.
Calibration and Validation
In the derivation cohort, the calibration curves of the predicted and the actual probability of POAF were drawn. The bar chart further assessed model calibration: predicted probabilities for POAF were calculated and divided into deciles, compared with observed frequencies. The area under the receiver operating characteristic (ROC) curve (AUC) was estimated to assess the discriminative ability of the nomogram. With respect to calibration and discrimination, the performance of the model was evaluated by the same methods in the validation cohort. Besides, DeLong’s test, net reclassification index (NRI) and integrated discrimination improvement (IDI) were used to compare the discriminative ability for POAF of the nomogram with established prediction models (CHA2DS2-VASc, HATCH and POAF scores) in the two cohorts.
Statistical Analysis
Continuous variables were shown as mean ± standard deviation (SD) or median (25th, 75th percentiles) in case of normal or non-normal distribution, and the differences between two groups were compared by using Student’s t-test or the Mann–Whitney U-test. Categorical variables were presented as counts (percentage) and compared by Pearson chi-square test or Fisher exact test. All analyses were performed with SPSS software, version 26.0 (SPSS Inc., Chicago, IL, USA) and R software, version 4.0.2 with the following packages: rms for nomogram model and riskRegression for ROC curve analyses. A two-sided P value <0.05 indicated statistical significance.
Results
Demographics and Clinical Characteristics
A total of 4854 eligible patients were enrolled (Figure 1). The derivation cohort and the validation cohort enrolled 3641 (mean age, 62.6 ± 8.6 years; 76.2% male) as well as 1213 (mean age, 62.9 ± 8.7 years; 73.8% male) patients undergoing isolated CABG, respectively. As shown in Table 1, no significant difference regarding incidence of POAF was found between derivation cohort and the validation cohort (28.2% vs 27.8%, P = 0.804), CHA2DS2-VASc, HATCH and POAF scores did not differ between the two groups (P = 0.063, 0.120 and 0.100, respectively). Patients in the derivation cohort exhibited higher heart rate, left ventricular ejection fraction (LVEF), level of hemoglobin and percentage of preoperative statin therapy. Percentage of previous percutaneous coronary intervention (PCI) and LVEF <50%, left ventricular end-diastolic diameter (LVEDD), and level of white blood cell count were lower in the derivation cohort.
 |
Table 1 Characteristics of the Patients in the Derivation Cohort and Validation Cohort |
 |
Figure 1 The consort diagram showing the inclusion and exclusion of patients. Abbreviations: CAD, coronary artery disease; CABG, coronary artery bypass grafting; AF, atrial fibrillation. |
Screening Potential Variables
Characteristics of the patients with and without POAF in the derivation cohort are exhibited in Table 2. The univariate analysis identified the following factors potentially associated with POAF (P < 0.1): age, sex, body mass index (BMI), heart rate, hypertension, peripheral vascular disease (PVD), LVEF, LVEF < 50%, LVEDD, left atrial diameter (LAD), LAD > 40mm, eGFR, platelet count LIMA, left internal mammary artery (LIMA) graft + saphenous vein graft (SVG) and on-pump surgery. In addition, patients with POAF had higher CHA2DS2-VASc, HATCH and POAF scores, as well as longer hospital stay (Table 2). At multivariable analysis, age (OR, 1.049; 95% CI, 1.038–1.060; P < 0.001), male (OR, 1.488; 95% CI, 1.236–1.790; P < 0.001), heart rate (81–100: OR, 1.394; 95% CI, 1.042–1.865; P = 0.025. > 120: OR, 2.565; 95% CI, 1.465–4.492; P = 0.001), hypertension (OR, 1.339; 95% CI, 1.134–1.582; P = 0.001), LVEF < 50% (OR, 1.726; 95% CI, 1.358–2.194; P < 0.001), LAD > 40mm (OR, 1.616; 95% CI, 1.318–1.982; P < 0.001), eGFR (OR, 0.993; 95% CI, 0.988–0.997; P = 0.003) and on-pump surgery (OR, 1.298; 95% CI, 1.090–1.546; P = 0.003) were independent predictive factors of POAF in the derivation cohort (Table 3).
 |
Table 2 Characteristics of the Patients with and without Postoperative Atrial Fibrillation in the Derivation Cohort |
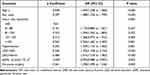 |
Table 3 Multivariate Logistic Regression Analysis for Predicting Postoperative Atrial Fibrillation in the Derivation Cohort |
Developing the Nomogram
A nomogram was established by independent predictors for POAF in the derivation cohort (Figure 2). In the nomogram, each variable was assigned to a point ranging from 0 to 100, and the higher the total score, the higher the probability of new-onset POAF following CABG.
Calibration and Validation of the Nomogram
Calibration curves of the nomogram, which are presented in Figure 3, provided accordant agreements between nomogram prediction and actual observation of POAF in the derivation cohort (Figure 3A) as well as the validation cohort (Figure 3B). Figure 4 further verified the model calibration by comparing the predicted and observed risks across predicted risk deciles, and revealed marked predictive accuracy of the nomogram to predict POAF both in the derivation (Figure 4A) and validation cohorts (Figure 4B). The nomogram had discriminative ability in derivation (Figure 5A) and validation cohorts (Figure 5B) with AUCs of 0.661 (95% CI, 0.642–0.681) and 0.665 (95% CI, 0.631–0.699), respectively. In comparison, the DeLong’s test indicated that the CHA2DS2-VASc, HATCH and POAF scores had inferior discrimination performance for predicting POAF in the same two cohorts with significantly lower (all P < 0.05) AUCs (0.578, 0.576 and 0.596 in the derivation cohort, respectively; 0.592, 0.583 and 0.632 in the validation cohort, respectively) (Figure 5). The performance of nomogram, CHA2DS2-VASc, HATCH and POAF scores in the entire cohort was as follows: the AUCs were 0.662, 0.581, 0.578 and 0.607, respectively, the best cut-off points to predict POAF were >98, >2, >1 and >1, with sensitivity/specificity of 61%/63%, 60%/53%, 34%/77% and 33%/80%, and positive/negative predictive values were 39%/81%, 33%/77%, 37%/75%, and 39%/76%, respectively. The changes in NRI, and IDI were used to compare the accuracy between the nomogram and established prediction models (CHA2DS2-VASc, HATCH and POAF scores). While using the nomogram in the derivation cohort, the NRI values were 0.436 (95% CI = 0.365–0.506, P < 0.01), 0.386 (95% CI = 0.315–0.457, P < 0.01) and 0.378 (95% CI = 0.307–0.449, P < 0.01), respectively, the IDI values were 0.056 (95% CI = 0.048–0.064, P < 0.01), 0.055 (95% CI = 0.047–0.063, P < 0.01) and 0.042 (95% CI = 0.035–0.050, P < 0.01), respectively. In the validation cohort, the NRI values were 0.388 (95% CI = 0.266–0.511, P < 0.01), 0.417 (95% CI = 0.295–0.539, P < 0.01) and 0.157 (95% CI = 0.032–0.282, P = 0.01), respectively, the IDI values were 0.051 (95% CI = 0.037–0.066, P < 0.01), 0.052 (95% CI = 0.038–0.066, P < 0.01) and 0.022 (95% CI = 0.008–0.037, P < 0.01), respectively.
 |
Figure 4 Predicted and observed risks of postoperative atrial fibrillation based on decile grouping of predicted risk in derivation (A) and validation (B) cohorts. |
Discussion
A method for effectively identifying patients at high risk of POAF could enable targeted preventive strategies, and avoid exposing the overall isolated CABG population to the risk of drug side effects and additional costs. In this setting, the present study developed an intuitive nomogram as a bedside predictive tool that quantified the risk of POAF following isolated CABG. By incorporating eight preoperative variables, namely age, sex, heart rate, hypertension, LVEF < 50%, LAD > 40mm, eGFR level, and on-pump surgery, the current nomogram demonstrated improved accuracy compared with established prediction models.
A Bayesian analysis from an observational study of 1481 patients showed that CHA2DS2-VASc score, severe obesity, renal failure, preoperative β-blocker and antiplatelet therapy were independent predictors of POAF after isolated CABG with cardiopulmonary bypass (CPB).11 In a prospective study of 1851 patients, Amar et al presented a prediction rule to estimate the risk of POAF following CABG with CPB using four independent predictors: greater age, history of AF, P-wave duration >110 ms, and postoperative low cardiac output.12 Previous studies have confirmed the utility of CHA2DS2-VASc, HATCH and POAF scores for predicting POAF; however, the population of these studies concentrated on inhomogeneous patients undergoing different types of cardiac surgery.7,8 Notably, considerable evidence has confirmed that the occurrence and prognosis of POAF following CABG are ethnically different.2,3 In China, the annual CABG volume exceeds 46,000 and off-pump (without CPB) CABG has become a common practice.13 To our knowledge, as of the writing of this article, this study was the first to construct a quantitative nomogram to predict the probability of POAF in a Chinese population undergoing isolated CABG with or without CPB.
Recently, Filardo et al reported that approximately 800,000 people worldwide undergo CABG each year, and the incidence of POAF is greater than 33%,1 which is significantly higher than our study (28%). A reasonable explanation for this might be that most of surgeries (77% in the entire cohort) included in our study were performed without CPB, and CPB increased the risk of POAF (OR = 1.298; P = 0.003). A meta-analysis involving 16,261 participants showed that compared with on-pump CABG, CABG without CPB yielded a lower incidence of POAF (OR = 0.87; P = 0.01).14 Studies have shown that systemic inflammation induced by CPB can potentially alter atrial conduction, facilitating multiple re-entry wavelets, and then predisposing to the development of POAF.15,16
Advanced age has become a well-established risk factor for AF whether in the general or cardiac surgery population.17,18 Degeneration of the atrial myocardium with aging may lead to a loss of side-to-side electrical coupling between muscle fibers, slowing down electrical conduction of the sinoatrial and atrioventricular nodes and atria, thereby providing an anatomic or electrophysiologic substrate for arrhythmogenesis.19 Left atrial (LA) enlargement is a manifestation of potentially fibrosis and adverse atrial remodeling,20 in addition to age, it can also be exacerbated by atrial ischemia in the presence of stenosis of coronary artery supplying to the atria.21 On the basis of varying degrees of changes in the atria, inflammation and activation of the autonomic nervous system are the principal transient factors associated with CABG that trigger POAF.22 Hakala et al prospectively evaluated whether atrial enlargement and increased level of atrial natriuretic peptide (ANP), N-terminal atrial natriuretic peptide (N-ANP) and brain natriuretic peptide (BNP) could predict POAF following CABG, and found that only age and LA area were independent predictors.23 However, the above three scores did not include size of LA as a scoring item. In the current study, LA enlargement was defined as an LA diameter of >40 mm, age and LA enlargement were independent risk factors for POAF, with odds ratios of 1.049 (for each increasing year) and 1.616, respectively. In addition, the weight of age in this nomogram was greater than that in the HATCH score, which might lead to a better discriminative ability for POAF of the nomogram to a certain extent.
Recent studies with relatively large sample size have found an increased incidence of POAF following CABG among males.24,25 In terms of the sex-specific characteristics and effect on survival, a study of 9203 consecutive isolated CABG patients showed that POAF occurred in 2157 (32.3%) men and 739 (29.4%) women (p < 0.001), increased risk of five-year mortality was found in both men and women who experienced ≥2 AF episodes, while men’s risk increased as number of in-hospital AF episodes rose, women’s peaked at 2 AF episodes.26 Another study of the same population showed women had lower adjusted risk of POAF and experienced shorter duration of AF episodes.27 In consistent to previous studies, we identified male sex as an independent predictor of POAF following CABG. However, CHA2DS2-VASc score, which was developed to predict risk of stroke in individuals diagnosed with AF and was proved to have reasonable discrimination for the prediction of AF,7,28 includes female sex as a high-risk factor. This partly explains why the present nomogram could provide a superior discriminatory ability to that of CHA2DS2-VASc score.
The role of the sympathetic nervous in initiating and maintaining AF has been studied extensively. Increased atrial ectopic electrical activity and sinus rate, which point to an increased sympathetic tone, usually precede onset of POAF.22,29 A dose–response meta-analysis demonstrated a significant J-shaped association between the resting heart rate and AF, compared with a modest resting heart rate of 68 to 80 bpm, both lower and higher resting heart rate increased the risk of AF.30 However, an analysis from the Multi Ethnic Study of Atherosclerosis (MESA) enrolling 6261 participants revealed that higher (but not lower) resting heart rate (>76 bpm) was associated with increased risk of AF in fully adjusted models.31 The results of this study on the relationship between sinus rate and POAF were consistent with the latter, related mechanisms in the CABG population deserve further detailed study in the future. Easy-to-measure electrocardiographic variables of P-wave, which represents atrial depolarization, would be of great value to predict the risk of AF. Recently, a new score system composed of P-wave morphology in inferior leads, voltage in lead I and P-wave duration has proven to be valuable in in-hospital and long-term AF diagnosis following acute ischemic stroke. Further improvement of this nomogram based on such indicators can be achieved.32
Hypertension and reduced LVEF may induce atrial stretch and cardiomyopathy, which ultimately lead to structural and electrophysiological remodeling conducive to onset of AF.33,34 Hypertension, fluid overload, pathological activation of the renin-angiotensin-aldosterone system (RAAS) with subsequent enhanced myocardial fibrosis may be the underlying mechanisms by which renal dysfunction increases the likelihood of AF.35 The predictive model constructed in this study further showed that the presence of hypertension, reduced LVEF and a decline in eGFR increased the risk of POAF following isolated CABG. In addition to being related to POAF, LVEF was lower in the intra-aortic balloon pump (IABP) group compared with the non-IABP group in the entire cohort of this study (56.6±10.9 vs 59.6±8.2, P = 0.001), and previous study has further pointed out that LVEF is an independent predictor of in-hospital mortality in patients treated with IABP.36
A wide range of therapies targeting autonomic alterations and inflammation have been used to prevent POAF following cardiac surgery, of which β-blocker prophylaxis, recommended by current guidelines (class I), is the best established.17,37,38 Furthermore, identifying patients at high risk for developing POAF may allow modification of risk factors to reduce POAF burden. The current nomogram, composed of eight preoperative variables, was a simple, accurate bedside tool to predict POAF in patients undergoing isolated CABG.
The present study has several limitations. Firstly, this was a single-center retrospective study, although internal validation of a cohort with 33% of the total sample size yielded satisfactory discrimination and calibration performance, the generalizability of this nomogram still requires external validation through a larger, multicenter sample. Secondly, in consistent to the previous studies,11,35 patients with history of AF, which is an important risk factor for cardiac surgery POAF,22 were excluded in order to avoid referral bias. In addition, although complete medical histories were collected, patients with prior paroxysmal or asymptomatic AF could not be completely excluded. Thirdly, in the present study, POAF was defined as captured AF that occurred before discharge, undiagnosed post-discharge AF might lead to underestimation of the incidence. However, previous study showed that the risk of POAF was highest immediately postoperatively and at 48 hours, the risk returned to near baseline by postoperative day 6.39 Finally, the predictive ability of the nomogram was moderate (AUC=0.66), which shared with other similar studies,9,12,40 and this is likely due to the multifactorial nature of AF.
Conclusions
We developed a novel nomogram with improved accuracy for predicting the risk of POAF following isolated CABG. This nomogram might help clinicians predict individual probability of POAF and achieve effective prophylaxis.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
This study was approved by the Institutional Ethics Committee of Beijing Anzhen Hospital of Capital Medical University (Approval No: 2021101X). Given the retrospective nature and anonymity of the present study, no informed consent was required. All patients’ identifiable information were hidden and anyone’s identity cannot be deduced from the context.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (82070364) and Beijing Municipal Health Commission Capital Health Development Scientific Research Project (shoufa 2020-1-2061).
Disclosure
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
References
1. Filardo G, Damiano RJ
2. Benedetto U, Gaudino MF, Dimagli A, et al. Postoperative atrial fibrillation and long-term risk of stroke after isolated coronary artery bypass graft surgery. Circulation. 2020;142(14):1320–1329. doi:10.1161/CIRCULATIONAHA.120.046940
3. El-Chami MF, Kilgo P, Thourani V, et al. New-onset atrial fibrillation predicts long-term mortality after coronary artery bypass graft. J Am Coll Cardiol. 2010;55(13):1370–1376. doi:10.1016/j.jacc.2009.10.058
4. Saxena A, Dinh DT, Smith JA, Shardey GC, Reid CM, Newcomb AE. Usefulness of postoperative atrial fibrillation as an independent predictor for worse early and late outcomes after isolated coronary artery bypass grafting (multicenter Australian study of 19,497 patients). Am J Cardiol. 2012;109(2):219–225. doi:10.1016/j.amjcard.2011.08.033
5. Mahoney EM, Thompson TD, Veledar E, Williams J, Weintraub WS. Cost-effectiveness of targeting patients undergoing cardiac surgery for therapy with intravenous amiodarone to prevent atrial fibrillation. J Am Coll Cardiol. 2002;40(4):737–745. doi:10.1016/s0735-1097(02)02003-x
6. Mariscalco G, Cederlund B, Engström KG. The clinical noncompliance of oral sotalol/magnesium for prophylactic treatment of atrial fibrillation after coronary artery bypass grafting. J Card Surg. 2007;22(4):281–286. doi:10.1111/j.1540-8191.2007.00408.x
7. Burgos LM, Seoane L, Parodi JB, et al. Postoperative atrial fibrillation is associated with higher scores on predictive indices. J Thorac Cardiovasc Surg. 2019;157(6):2279–2286. doi:10.1016/j.jtcvs.2018.10.091
8. Selvi M, Gungor H, Zencir C, et al. A new predictor of atrial fibrillation after coronary artery bypass graft surgery: HATCH score. J Investig Med. 2018;66(3):648–652. doi:10.1136/jim-2017-000525
9. Mariscalco G, Biancari F, Zanobini M, et al. Bedside tool for predicting the risk of postoperative atrial fibrillation after cardiac surgery: the POAF score. J Am Heart Assoc. 2014;3(2):e000752. doi:10.1161/JAHA.113.000752
10. Tang Y, Chen Q, Zha L, et al. Development and validation of nomogram to predict long-term prognosis of critically ill patients with acute myocardial infarction. Int J Gen Med. 2021;14:4247–4257. doi:10.2147/IJGM.S310740
11. Perrier S, Meyer N, Hoang Minh T, et al. Predictors of atrial fibrillation after coronary artery bypass grafting: a bayesian analysis. Ann Thorac Surg. 2017;103(1):92–97. doi:10.1016/j.athoracsur.2016.05.115
12. Amar D, Shi W, Hogue CW
13. Chinese Society of Extracorporeal Circulation. White book of Chinese cardiovascular surgery and extracorporeal circulation in 2019. Chin J ECC. 2020;18:193–196. doi:10.13498/j.cnki.chin.j.ecc.2020.04.01
14. Dieberg G, Smart NA, King N. On- vs. off-pump coronary artery bypass grafting: a systematic review and meta-analysis. Int J Cardiol. 2016;223:201–211. doi:10.1016/j.ijcard.2016.08.250
15. Zhang W, Liu W, Chew ST, Shen L, Ti LK. A clinical prediction model for postcardiac surgery atrial fibrillation in an Asian population. Anesth Analg. 2016;123(2):283–289. doi:10.1213/ANE.0000000000001384
16. Echahidi N, Pibarot P, O’Hara G, Mathieu P. Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol. 2008;51(8):793–801. doi:10.1016/j.jacc.2007.10.043
17. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force On Practice Guidelines And The Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1–e76. doi:10.1016/j.jacc.2014.03.022
18. Mitchell LB; CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society atrial fibrillation guidelines 2010: prevention and treatment of atrial fibrillation following cardiac surgery. Can J Cardiol. 2011;27(1):91–97. doi:10.1016/j.cjca.2010.11.005
19. Zaman AG, Archbold RA, Helft G, Paul EA, Curzen NP, Mills PG. Atrial fibrillation after coronary artery bypass surgery: a model for preoperative risk stratification. Circulation. 2000;101(12):1403–1408. doi:10.1161/01.cir.101.12.1403
20. Koshy AN, Enyati A, Weinberg L, et al. Postoperative atrial fibrillation and long-term risk of stroke in patients undergoing liver transplantation. Stroke. 2021;52(1):111–120. doi:10.1161/STROKEAHA.120.031454
21. Boyd AC, Ng AC, Tran DT, et al. Left atrial enlargement and phasic function in patients following non-ST elevation myocardial infarction. J Am Soc Echocardiogr. 2010;23(12):1251–1258. doi:10.1016/j.echo.2010.09.010
22. Dobrev D, Aguilar M, Heijman J, Guichard JB, Nattel S. Postoperative atrial fibrillation: mechanisms, manifestations and management. Nat Rev Cardiol. 2019;16(7):417–436. doi:10.1038/s41569-019-0166-5
23. Hakala T, Hedman A, Turpeinen A, Kettunen R, Vuolteenaho O, Hippeläinen M. Prediction of atrial fibrillation after coronary artery bypass grafting by measuring atrial peptide levels and preoperative atrial dimensions. Eur J Cardiothorac Surg. 2002;22(6):939–943. doi:10.1016/s1010-7940(02)00565-1
24. Pollock BD, Filardo G, da Graca B, et al. Predicting new-onset post-coronary artery bypass graft atrial fibrillation with existing risk scores. Ann Thorac Surg. 2018;105(1):115–121. doi:10.1016/j.athoracsur.2017.06.075
25. Taha A, Nielsen SJ, Bergfeldt L, et al. New-onset atrial fibrillation after coronary artery bypass grafting and long-term outcome: a population-based nationwide study from the SWEDEHEART registry. J Am Heart Assoc. 2021;10(1):e017966. doi:10.1161/JAHA.120.017966
26. Filardo G, Pollock BD, da Graca B, et al. Postcoronary artery bypass graft atrial fibrillation event count and survival: differences by sex. Ann Thorac Surg. 2020;109(5):1362–1369. doi:10.1016/j.athoracsur.2019.08.098
27. Filardo G, Ailawadi G, Pollock BD, et al. Postoperative atrial fibrillation: sex-specific characteristics and effect on survival. J Thorac Cardiovasc Surg. 2020;159(4):1419–1425.e1. doi:10.1016/j.jtcvs.2019.04.097
28. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi:10.1378/chest.09-1584
29. Dimmer C, Tavernier R, Gjorgov N, Van Nooten G, Clement DL, Jordaens L. Variations of autonomic tone preceding onset of atrial fibrillation after coronary artery bypass grafting. Am J Cardiol. 1998;82(1):22–25. doi:10.1016/s0002-9149(98)00231-8
30. Liu X, Guo N, Zhu W, et al. Resting heart rate and the risk of atrial fibrillation. Int Heart J. 2019;60(4):805–811. doi:10.1536/ihj.18-470
31. Habibi M, Chahal H, Greenland P, et al. Resting heart rate, short-term heart rate variability and incident atrial fibrillation (from the multi-ethnic study of atherosclerosis (Mesa)). Am J Cardiol. 2019;124(11):1684–1689. doi:10.1016/j.amjcard.2019.08.025
32. Hayıroğlu Mİ, Çınar T, Selçuk M, et al. The significance of the morphology-voltage-P-wave duration (MVP) ECG score for prediction of in-hospital and long-term atrial fibrillation in ischemic stroke. J Electrocardiol. 2021;69:44–50. doi:10.1016/j.jelectrocard.2021.09.006
33. Fialová M, Dlugošová K, Okruhlicová L, Kristek F, Manoach M, Tribulová N. Adaptation of the heart to hypertension is associated with maladaptive gap junction connexin-43 remodeling. Physiol Res. 2008;57(1):7–11. doi:10.33549/physiolres.931101
34. Carlisle MA, Fudim M, DeVore AD, Piccini JP. Heart failure and atrial fibrillation, like fire and fury. JACC Heart Fail. 2019;7(6):447–456. doi:10.1016/j.jchf.2019.03.005
35. Chua SK, Shyu KG, Lu MJ, et al. Renal dysfunction and the risk of postoperative atrial fibrillation after cardiac surgery: role beyond the CHA2DS2-VASc score. Europace. 2015;17(9):1363–1370. doi:10.1093/europace/euu360
36. Hayıroğlu Mİ, Çanga Y, Yıldırımtürk Ö, et al. Clinical characteristics and outcomes of acute coronary syndrome patients with intra-aortic balloon pump inserted in intensive cardiac care unit of a tertiary clinic. Turk Kardiyol Dern Ars. 2018;46(1):10–17. doi:10.5543/tkda.2017.11126
37. Sousa-Uva M, Head SJ, Milojevic M, et al. 2017 EACTS guidelines on perioperative medication in adult cardiac surgery. Eur J Cardiothorac Surg. 2018;53(1):5–33. doi:10.1093/ejcts/ezx314
38. Andrade JG, Verma A, Mitchell LB, et al. 2018 focused update of the Canadian cardiovascular society guidelines for the management of atrial fibrillation. Can J Cardiol. 2018;34(11):1371–1392. doi:10.1016/j.cjca.2018.08.026
39. Melby SJ, George JF, Picone DJ, et al. A time-related parametric risk factor analysis for postoperative atrial fibrillation after heart surgery. J Thorac Cardiovasc Surg. 2015;149(3):886–892. doi:10.1016/j.jtcvs.2014.11.032
40. Thorén E, Hellgren L, Jidéus L, Ståhle E. Prediction of postoperative atrial fibrillation in a large coronary artery bypass grafting cohort. Interact Cardiovasc Thorac Surg. 2012;14(5):588–593. doi:10.1093/icvts/ivr162
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



