Back to Journals » International Journal of General Medicine » Volume 15
Predict the Progression of Cervical Intraepithelial Neoplasia by a Novel Marker Folate Combine with FRα, p16 and Ki-67
Authors Liu T, Chen M, Li X, Wang H
Received 20 February 2022
Accepted for publication 28 July 2022
Published 9 August 2022 Volume 2022:15 Pages 6529—6538
DOI https://doi.org/10.2147/IJGM.S362685
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Tingting Liu, Mengjie Chen, Xueqin Li, He Wang
Department of Gynecology, Guangxi Medical University Cancer Hospital, Nanning, Guangxi, People’s Republic of China
Correspondence: He Wang, Department of Gynecology, Guangxi Medical University Cancer Hospital, No. 71 Hedi Road, Nanning, Guangxi, People’s Republic of China, Email [email protected]
Purpose: To study the expression of serum folate and red blood cell (RBC) folate, folate receptor α (FRα), p16INK4a (p16), and Ki-67 at different levels of cervical intraepithelial neoplasia (CIN) and then analyze their role in the progression of CIN and their value as an early warning indicator of CIN progression.
Patients and methods: We randomly collected the data of patients at the Department of Gynecology in Guangxi Medical University Affiliated Cancer Hospital from January 2016 to December 2018: Normal controls (149 cases), CIN1 (150 cases), CIN2 (100 cases), and CIN3 (101 cases). [Ethical approval by Ethics Committee of the Second Hospital of Shanxi Medical University. (2013) No. (001– 1)]. The expression of serum folate and RBC folate was detected by the chemiluminescence method, while the expression of FRα, p16, and Ki-67 was detected by Streptavidin-Perosidase (SP) immunohistochemistry.
Results: There was no statistically significant difference in serum folate levels between different grades of CIN (P=0.784), but the RBC folate levels were statistically significant (P=0.015), and there was a negative correlation between RBC folate levels and CIN lesion grades (P< 0.05). The FRα, p16, and Ki-67 levels in the CIN group were significantly different from those in the normal control group (P < 0.01), and a positive correlation was found (P < 0.01); FRα positivity (P=0.000), Ki-67 positivity (P=0.000), and low-level RBC folate (P=0.000) were independent risk factors for the progression of CIN; these indicators were combined to establish a random forest (RF) model in which the Ki-67+FRα model was used as the early warning model of CIN progression.
Conclusion: RBC folate, FRα, p16, and Ki-67 can be used as valuable clinical test indicators for predicting the progression of CIN; the combined detection model of Ki-67+FRα can be used as an early warning model for predicting the progression of CIN.
Keywords: cervical intraepithelial neoplasia, folate, folate receptor α, p16INK4a, Ki-67
Introduction
Among female tumors, the incidence of cervical cancer is relatively high, and continuous infection with high-risk human papilloma virus (HPV) is the direct cause of cervical cancer.1 CIN is a precancerous lesion of cervical cancer, which is a dynamic process that gradually develops and usually takes a long time to progress to cervical cancer and provides sufficient time to intervene and prevent the occurrence of cervical cancer. If proper treatment of CIN is given in time, the occurrence of cervical cancer can be greatly reduced. On the other hand, since CIN can be reversed naturally, it is indeed unnecessary to perform resections for CIN that may degenerate naturally. In recent years, excessive surgeries for CIN have caused a series of adverse reactions, including infertility, miscarriage, premature delivery, and cervical insufficiency, which have caused great physical and mental stress, especially for young patients with fertility needs.2 Therefore, predicting the progress of CIN and determining ways to divert it according to its progress risk are very important.
Although a large number of current epidemiological treatments and related studies generally agree that persistent cervical infection with HPV is the main factor for the development of cervical squamous intraepithelial lesions into uterine invasive cancer, studies found that Not all SILs will progress to invasive cervical cancer,3 and simple cervical HPV infection may not necessarily cause cervical cancer. Therefore, there must be other carcinogenic factors or factors that cooperate with HPV, such as vaginal microenvironment, microbial infection, sexuality and reproductive status, immune factor, living habit and so on, which increase the susceptibility of the cervix to HPV, and makes the HPV infection persist to cause carcinogenesis.4
Folate, also known as pteroylglutamic acid, is related to the occurrence of cervical cancer5 which is a kind of water-soluble B vitamin. Dietary intake, mainly from fresh vegetables and fruits, makes it easier for the human body to lack folate.6 Folate deficiency can cause a variety of diseases, such as megaloblastic anemia, congenital defects, and cardiovascular diseases. After eating food containing folate, it is absorbed in the duodenum and proximal jejunum, and then converted into various forms of folate through various metabolic pathways, and plays various biological functions in the body. When folate is reduced to tetrahydrofolate, it is used as a 1-carbon donor for the synthesis of purine and adenosine, and homocysteine is then methylated to methionine, which is a key position in the process of DNA synthesis and DNA methylation. When deficient in folate, DNA synthesis and repair would be hindered, protein and amino acid metabolism disorders, abnormal methylation, and chromosomal aberrations would occur in DNA, thereby increasing the body’s sensitivity to carcinogenic factors.7 This study aimed to explore the serum folate, RBC folate, FRα, p16, and Ki-67 at different CIN levels. Various recent studies have demonstrated that these factors play a certain role in the progression of CIN, and we analyzed their role in the progression of CIN and their value as an early warning indicator of CIN progression.
Objects and Methods
Research Object
We randomly collected cervical tissues from patients at the Department of Gynecology in Guangxi Medical University Affiliated Cancer Hospital from January 2016 to December 2018: normal control (149 cases), CIN1 (150 cases), CIN2 (100 cases), and CIN3 (101 cases). Patients with abnormal ThinPrep cytologic test (TCT) results were further diagnosed using colposcopy and histopathological examination. Patients with nutritional megaloblastic anemia, hemolytic disease, leukemia, localized enteritis, liver disease, and other tumors as well as B vitamin users within 3 months were excluded. All research subjects entered the study with informed consent.
Methods
Serum and RBC Folate Concentration Detection
We collected 5 mL of fasting cubital venous blood from the subjects and placed it in a nonanticoagulant tube, left it at room temperature for 3 hours, centrifuged it for 15 minutes (3000 rpm), carefully collected the supernatant, and stored it in an ultralow temperature refrigerator (−80 °C) for batch testing. The sample could be kept in a frozen state for no more than 6 months before testing. The chemiluminescence method was used to determine serum folate and RBC folate levels. Instruments and reagents, including the folate assay kit, chemiluminescence substrate Lumi-Phos*530, Access Wash Buffer II, folate calibrator, and automatic luminescence analyzer, were purchased from Beckman Coulter, USA.
Detection of FRα, P16, Ki-67
The pathological HE staining slices and their corresponding tissue wax blocks for all patients in the group were selected, and the corresponding tissue wax blocks were verified and checked for integrity, which could be used for immunohistochemistry experiments. After the wax blocks were cut into thin slices for dewaxing and dehydration, the endogenous enzymes in them were removed, the antibodies were dripped in after high-pressure antigen restoration; then, hematoxylin was used for counterstaining to make immunogrouped slices. Among those, the antibody used for FRα detection was mouse anti-human FRα monoclonal antibody (ab3361) purchased from Abcam Company; the antibody used for Ki-67 detection was mouse anti-human Ki-67 monoclonal antibody (clone number: MIB-1), purchased from Fuzhou Maixin Reagent Company. In addition, the antibody used for p16 detection was mouse anti-human P16INK4a monoclonal antibody (clone number: 3G5D5), which was purchased from Beijing Zhongshan Jinqiao Biotechnology Co., Ltd, where the ready-to-use immunohistochemical hypersensitivity SP kit and DAB staining kit used for P16 detection were also purchased.
FR-α immunohistochemistry is positively expressed on the cervical epithelial cell membrane, and the positive effect product is brown–yellow particles. FR-α scoring standard: according to the comprehensive score of dyeing degree and dyeing area: the dyeing degrees for no coloring, light brown, brown, and dark brown were, respectively, 0 points, 1 point, 2 points, and 3 points; stained areas of 0, 1–25%, 26–50%, and greater than 50% were, respectively, 0, 1, 2 and 3. The two scores were added together, and 0 to 1 was considered negative (-), 2 points were rated as positive (+), 3 to 4 points were rated as weakly positive (++), and 5 to 6 points were rated as strongly positive (+++).
The results of p16 and Ki-67 were judged by using the semiquantitative method, which was in according with the proportion of positive cells in the vertical distribution of the cervical scaly epithelial. The positive marker of basal cells was marked as 1+, the lower 1/3 of the squamous epithelium was marked as 2+, the lower 2/3 was marked as 3+, and the lower 2/3 was more than the lower 2/3 to the full thickness. The coloring was marked as 4+.
Statistical Analysis
SPSS 25.0 software was used to establish a database. Nonnormal quantitative data are described by the median±interquartile range (M±Q), and the Kruskal–Wallis H-test and Spearman rank correlation were used for analysis. The rank-sum test and the rank correlation test were used for the immunohistochemical staining results of FRα, p16, and Ki-67. P<0.05 was considered statistically significant. Meaningful test indicators of the above research were analyzed by univariate analysis and multivariate logistic analysis. Based on the above results, different combinations of significant factors were selected to establish random forest models.
Results
Characteristics of Study Subjects
There were 500 subjects in this study, including 149 cases in the control group, 150 cases in the CIN1 group, 100 cases in the CIN2 group, and 101 cases in the CIN3 group. The characteristics of the research subjects, such as age, ethnicity, place of birth, smoking, drinking, vaginal secretion examination, HPV detection, etc. were shown in Table 1.
 |
Table 1 Characteristics of Study Subjects |
Serum Folate and RBC Folate in Patients with CIN
Serum Folate Test results
The serum folate level in the normal control group was 17.08±13.66 nmol/L; the serum folate levels in the CIN1, CIN2, and CIN3 groups were 16.56±12.95 nmol/L, 16.81±12.40 nmol/L, and 16.52±12.91 nmol/L, respectively. The Kruskal–Wallis H-test revealed that the overall distribution of serum folate levels in the four groups was not statistically significant (H=1.07, P=0.784) (Table 2).
 |
Table 2 The Relationship Between Serum Folate and CIN |
RBC Folate Test results
The RBC folate of the normal control group was 7.37±5.67 nmol/L; the RBC folate levels of CIN1, 2, and 3 groups were 6.59±5.16 nmol/L, 6.41±4.82 nmol/L, and 6.44±4.58 nmol/L, respectively. Kruskal–Wallis H-test indicated that the overall distribution of RBC folate levels in the four groups was statistically significant (H=10.469, P=0.015) (Table 3). Furthermore, the 50% value of the RBC folate content of the normal control group was used as the boundary, and ≤7.37 nmol/L was the low folate level for analysis. The results verified that the low folate rates were higher in the CIN 1, 2, and 3 groups than in the control group. The Mantel Haenszel chi-square test demonstrated that there was a linear relationship between the RBC folate level and the grade of CIN lesions, χ2=5.901, P=0.015<0.05. The Pearson correlation results confirmed that there was a negative correlation between RBC folate and the grade of CIN lesions, R=0.109, P=0.015<0.05. As the severity of CIN lesions worsened, the RBC folate deficiency rate gradually increased, and the RBC folate level gradually decreased.
 |
Table 3 The Relationship Between RBC Folate and CIN |
FRα, p 16, and Ki-67 Immunohistochemistry Results
The rank-sum tests of FRα, p16, and Ki-67 staining in the CIN and control groups at each level verified that there were significant differences between each group and the normal control group (CIN1: H=260.298, P<0.01; CIN2: H=373.769, P<0.01; CIN3: H=329.886, P<0.01). The Spearman rank correlation test demonstrated that there was a positive correlation between the positive expression of FRα, P16, and Ki-67 and the grade of CIN lesions (CIN1: r=0.684, P <0.01; CIN2: r=0.826, P<0.01; CIN3: r =0.778, P<0.01), indicating that the positive expression rate of FRα, p16, and Ki-67 gradually increased with an increase in CIN lesion grade (Table 4).
 |
Table 4 The Expression of FRα, p16 and Ki-67 in Each Level of CIN |
Logistic Regression Analysis
To explore the risk factors for the occurrence and progression of CIN, the four indicators FRα, P16, Ki-67, and RBC folate were included in the univariate logistic analysis (a P value less than 0.01 was considered to be statistically significant and was included in the multivariable analysis). The multivariable logistic analysis confirmed that FRα positivity (HR 9.436, 95% CI 3.569–24.945, P=0.000), Ki-67 positivity (HR 16. 389, 95% CI 5.203–51.620, P = 0.000) and low levels of RBC folate (HR 0.917, 95% CI 0.849–0.989, P = 0.000) were independent risk factors for the occurrence and progression of CIN (Table 5).
 |
Table 5 Logistic Regression of Risk Factors for CIN |
Establishment of Random Forest Models for CIN Progression
According to the results of multivariate logistic regression analysis, different combinations of significant risk factors that promote the progression of CIN were selected to establish random forest models (Table 6). According to the accuracy rate, out-of-bag (OOB) error value and Area under the curve of ROC(AUC) of each model. Among the four models of predicting CIN progression, the Ki-67+FRα model had the highest accuracy rate and the smallest OOB error value, while the AUC was relatively ideal (Figure 1). For this reason, it can be used as a candidate for an early warning model for predicting the progression of CIN.
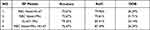 |
Table 6 Random Forest Models for Predicting CIN Progression |
 |
Figure 1 (A and B) The weight of factors in model Ki-67+ FRα. The ROC curve of model Ki-67+ FRα. |
Discussion
Folate
Folate is an essential vitamin for humans that participates in the metabolism of the one-carbon unit. The normal level of folate in the body ensures balanced DNA synthesis and DNA methylation. It plays an important role in cell proliferation and is essential for maintaining genome stability. This is due to its two functions: on the one hand, as a methyl donor of deoxythymidine monophosphate to form deoxythymidine triphosphate, which is used for DNA synthesis and repair, and on the other hand, it is synthesized with the common methyl donor S-adenosylmethionine for cytosine methylation. Therefore, a lack of folate can cause genomic DNA strand breaks, chromosomal instability, uracil mismatches, etc., disrupt DNA synthesis and repair, and affect nucleic acid and histone methylation modifications, thus increasing the risk of tumors.8
In the occurrence of cervical cancer, most scholars believe that high-risk HPV is not randomly inserted into the host genome but often integrates into the unstable and transcriptionally active regions of the cervical epithelial cell genome and inhibits its function. This integration is most likely to occur in the fragile histidine triad (FHIT) gene at the chromosomal fragile site, FRA3B. The FHIT gene is a special tumor suppressor gene, and its abnormal expression is closely related to the occurrence and development of cervical cancer. FHIT gene central pattern generator (CPG) methylation is one of the important mechanisms leading to its functional inactivation. As folate is directly involved in DNA methylation as a methyl donor in the body, its deficiency may affect chromosomal stability at the FRA3B site located in the FHIT gene, which is prone to forming gaps or breaks on metaphase chromosomes, thereby increasing the risk of high-risk HPV virus infection and leading to cancer of the cervix.9
This study revealed that the overall distribution of serum folate levels in different pathological groups was not statistically significant, while in recent years, many studies have indicated that low serum folate is related to CIN.10 Considering that serum folate only reflects the early changes in folate levels in the body that are affected by dietary and absorption factors, the possibility of error is not ruled out. On the other hand, RBC folate ought to represent the storage levels of folate in the body, which are relatively stable. Therefore, this study also analyzed the relationship between RBC folate and CIN simultaneously. After analysis, it was found that there was a negative correlation between RBC folate and the grade of CIN lesions. As the degree of CIN lesions worsened, the RBC folate deficiency rate gradually increased, and the RBC folate level gradually decreased. Univariate logistic analysis and multivariable logistic analysis were used to further determine that low RBC folate levels were an independent risk factor for the progression of CIN. In addition, related studies have pointed out that a high folate state can inhibit the possibility of viral nucleic acid integration into host cells. Appropriate folate supplementation has a protective effect on CIN. Folate supplementation has effects on cervical precancerous lesions, which may provide new strategies for cancer prevention and treatment.11
In this study, the 50% value of the normal control group was used to divide the RBC folate level. However, whether there is a more appropriate delimitation point to improve the accuracy of the RBC folate level in detecting diseases requires further analysis of a large amount of data. On the other hand, as this study failed to find a relationship between serum folate and CIN, the absorption, metabolism, and transportation of folate in the diet may be affected by various factors and should be further explored.
FRα
The immortal proliferation of malignant tumor cells requires much higher than normal levels of purines and pyrimidines. Therefore, more folate needs to be taken into the cell. Folate transport mediated by high-affinity folate receptors is the main mechanism of folate ingestion by malignant tumor cells.12
Folate receptors are synthesized by the Id protein gene family of chromosome 11 q13.3, which include primarily four subtypes of FRα, FRβ, FRδ, and FRγ. FRα is an antigen protein that is specifically and highly expressed by tumor cells. It binds to folic acid with high affinity, causing them to be endocytosed and taken into cells. FRα expression is low in nonmalignant tumor tissues but overexpressed on the surface of a variety of solid tumor cells, which is closely related to the occurrence and progression of tumors.13 Research has uncovered that FRα is an important activator of the extracellular signal-regulated kinase (ERK) pathway. Its high expression in CIN and cervical cancer could activate the ERK pathway, upregulate the expression of proto-oncogenes, and promote tumor cell proliferation and apoptosis. Downregulating the expression of FRα could reduce the uptake of folate in cells, affect DNA synthesis, break chromosomes, and arrest the cell cycle in the G0/G1 phase, thereby inhibiting the proliferation of tumor cells.14 This study also found that there were significant differences in the staining of RFα between the CIN group of each grade and the normal control group, the positive expression rate increased with an increase in the disease grade, and there was a positive correlation with the disease grade. Univariate logistic analysis and multivariable logistic analysis revealed that FRα positivity is an independent risk factor that promotes the progression of CIN.
In recent years, some researchers have developed folate receptor-mediated cervical dyeing (FRD) analysis to detect cervical cancer. When staining the cervix with FRD, the compounds of folate–deoxidized methylene blue specifically bound to the receptors on the tumor cells, and the deoxidized methylene blue was oxidized, thus changing the original brown color of the FRD and coloring the cotton swab. This study emphasized that FRD had higher sensitivity and higher specificity in screening high-grade CIN, which was higher than that of TCT and HPV. In addition, as FRD is cost-effective, it is convenient and quick to operate. Moreover, the results of FRD tests can be easily identified and can be widely used in places where there is a lack of colposcopy services and histopathology rooms.15
p16
P16 is a cyclin-dependent protein kinase inhibitor (CDKI) that is encoded by the CDKN2A2655 gene located on the short arm of chromosome 9 (9p21.3). Its production P16 protein can interact with cyclin. D competitively binds to cyclin-dependent protein kinase 4 (CDK4) or cyclin-dependent protein kinase 6 (CDK6) and specifically inhibits the activity of CDK4 or CDK6, making it unable to phosphorylate retinoblastoma protein (pRb), thereby preventing cells from entering the S phase from G1 phase and ceasing the development of the cell cycle.16 In cervical cells infected with HPV, persistent infection of the cervix can cause irreversible changes, leading to carcinoma in situ and ultimately to invasive cervical cancer. The integration of HPV DNA into the host genome can induce the expression of E6 and E7. The E7 protein competes with the cell cycle control protein pRb and induces the overexpression and accumulation of p16 in cells through a negative feedback loop by interfering with the pRb-E2F1 pathway. Therefore, p16 is considered a surrogate marker for persistent high-risk HPV infection. The overexpression of p16 has been observed in most cervical cancers and cancers.17 This study verified that there were significant differences in p16 staining between the CIN group of each grade and the normal control group, that the positive expression rate increased with increasing disease grade, and that there was a positive correlation with disease grade. However, univariate logistic analysis did not verify that p16 is an independent risk factor for CIN progression, which is inconsistent with the conclusions of other studies. At present, errors are not ruled out, and more in-depth large sample studies are needed for further verification.
Ki-67
Ki-67 is a cell proliferation marker, a nuclear nonhistone protein encoded by the MKI-67 gene, and is expressed in all stages of the cell cycle, except for the G0 segment, which plays a variety of functions in regulating cell cycle progression. During mitosis, Ki-67 participates in the formation of the chromosome perimeter, which acts as a protective sheath around the chromosome and provides a platform during the nucleolar assembly process. Ki-67 is used as a biological surfactant that can prevent the aggregation of chromosomes after mitosis and the disassembly of the nuclear envelope.18 Therefore, as a marker of cell proliferation, Ki-67 can predict the malignant potential of tumors. This study found that there were significant differences in the staining of Ki-67 between the CIN group of each grade and the normal control group, the positive expression rate increased with the increase of the disease grade, and there was a positive correlation with disease grade. Univariate logistic analysis and multivariate logistic analysis revealed that Ki-67 positivity is an independent risk factor that promotes the progression of CIN.
Liu et al19 demonstrated that the p16 test alone revealed good sensitivity, while the Ki-67 test alone showed good specificity. Combining the two tests, double positivity can be used to diagnose or monitor women receiving high-level CIN/VAIN treatment. P16/Ki-67 dual-staining cytology is of great significance in the screening and trialing of cervical cancer and precancerous lesions. It provides a good risk marker for the stratification of HPV-positive women, including normal cytological patients, and the identification of high-grade CIN from women diagnosed with ASCUS or LSIL. Compared with Pap cytology and HPV detection, it has a higher sensitivity and specificity in detecting cervical precancerous lesions and cervical cancer. However, whether p16/Ki-67 dual-staining cytology can be a method of diagnosing and following up CIN progression may require a longer follow-up time for further clinical studies.
The Predictive Models of CIN
In recent years, many prediction models of relevant CIN progress have been established from different perspectives. This study showed from the establishment of random forest models of tumor-related detection indicators that the Ki-67+FRα model could be used as a candidate for an early warning model for predicting CIN progress. Through the analysis of clinical factors related to the occurrence and progression of CIN and the core genes located in the common pathways related to CIN, Chen et al20 reported that the factors related to the progression of CIN, included older age, premenopause, and multiple parties, the significant genes of TGFBR2, FOXO1, CSKN1A1, PRKCI, and CTBP2, and the factors related to the occurrence of CIN. Including HPV infection, TCT result diagnosis of CINII+, and the significant genes of TGFBR2, FOXO1, and CTBP2. Based on the above results, different combinations of significant clinical factors and genes were selected to establish random forest models. As a result, a model (TGFBR2+ CSKN1A1+ PRKCI+ FOXO1+ CTBP2+ premenopause+ multiple parity+ older age) was selected as the model for CIN progression. Likely, the model (CTBP2+FOXO1+HPV infection,+TCT result diagnosed of CINII+) was considered the model of CIN occurrence. On the other hand, Zhou et al21 established a regression model to predict cervical squamous cell carcinoma with a backward logistic stepwise regression method and found that the combined test of hTERC gene amplification, HR-HPV viral load, and MCM5 protein could be used for prediction and evaluation of cervical lesions. The establishment of these early warning models has continuously improved the CIN detection system.
Conclusions
In summary, we selected the detection indicators of folate, FRα, P16, and Ki-67, which have been confirmed to be related to the occurrence and development of tumors. In this study, FRα positive, Ki-67 positive, and low-level RBC folate are independent risk factors for the progression of CIN. For patients with Ki-67 and FRα positive, it is necessary to be vigilant regarding the occurrence and development of CIN.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and complies with the Declaration of Helsinki.
Consent for Publication
Informed consent was obtained from all individual participants included in the study.
Funding
This subject was funded by Guangxi’s eighteenth batch of the “New Century Ten Hundred Thousand Talents Project” second-level candidate special fund (NO.2015226), Guangxi Medical High-level Backbone Talent Training “139” Program Special Fund (NO. G201903032), and Guangxi Medical and Health Appropriate Technology Development and Application Project (NO. S2018031), supported by the Guangxi Natural Science Foundation (NO.2020GXNSFAA159023).
Disclosure
Tingting Liu declares that she has no conflict of interest. Mengjie Chen declares that she has no conflict of interest. Xueqin Li declares that she has no conflict of interest. He Wang declares that she has no conflict of interest.
References
1. Miller K, Nogueira L, Devasia T, et al. Cancer treatment and survivorship statistics, 2022. CA Cancer J Clin. 2022;77. doi:10.3322/caac.21731
2. Martin C, O’leary J. Histology of cervical intraepithelial neoplasia and the role of biomarkers. Best Pract Res Clin Obstet Gynaecol. 2011;25(5):605–615. doi:10.1016/j.bpobgyn.2011.04.005
3. Zhou L, Qiu Q, Zhou Q, et al. Long-read sequencing unveils high-resolution HPV integration and its oncogenic progression in cervical cancer. Nat Commun. 2022;13(1):2563. doi:10.1038/s41467-022-30190-1
4. Yang J, Yang A, Wang Z, et al. Interactions between serum folate and human papillomavirus with cervical intraepithelial neoplasia risk in a Chinese population-based study. Am J Clin Nutr. 2018;108(5):1034–1042. doi:10.1093/ajcn/nqy160
5. Wang W, Yang A, Zhang H, et al. Associations of RBC and serum folate concentrations with cervical intraepithelial neoplasia and high-risk human papillomavirus genotypes in female Chinese adults. J Nutr. 2022;152(2):466–474. doi:10.1093/jn/nxab396
6. Barchitta M, Maugeri A, La Mastra C, et al. Dietary antioxidant intake and human papillomavirus infection: evidence from a cross-sectional study in Italy. Nutrients. 2020;12(5):1384. doi:10.3390/nu12051384
7. Nam E, Kim J, Kim S, et al. The expressions of the Rb pathway in cervical intraepithelial neoplasia; predictive and prognostic significance. Gynecol Oncol. 2007;104(1):207–211. doi:10.1016/j.ygyno.2006.07.043
8. Wang J, Ding L, Jiang S, et al. Folate deficiency and aberrant expression of DNA methyltransferase 1 were associated with cervical cancerization. Curr Pharm Des. 2014;20(11):1639–1646. doi:10.2174/13816128113199990543
9. Li Q, Ding L, Jing N, et al. Folate deficiency and aberrant DNA methylation and expression of FHIT gene were associated with cervical pathogenesis. Oncol Lett. 2018;15(2):1963–1972. doi:10.3892/ol.2017.7471
10. Hoffman S, Le T, Lockhart A, et al. Patterns of persistent HPV infection after treatment for cervical intraepithelial neoplasia (CIN): a systematic review. Int J Cancer. 2017;141(1):8–23. doi:10.1002/ijc.30623
11. Zhao W, Hao M, Wang Y, et al. Association between folate status and cervical intraepithelial neoplasia. Eur J Clin Nutr. 2016;70(7):837–842. doi:10.1038/ejcn.2016.35
12. Bai L, Ding L, Jiang S, et al. Down-regulation of FRα inhibits proliferation and promotes apoptosis of cervical cancer cells in vitro. Asian Pac J Cancer Prev. 2014;15(14):5667–5672. doi:10.7314/APJCP.2014.15.14.5667
13. Scaranti M, Cojocaru E, Banerjee S, et al. Exploiting the folate receptor α in oncology. Nat Rev Clin Oncol. 2020;17(6):349–359. doi:10.1038/s41571-020-0339-5
14. Herrero A, Pinto A, Colón-Bolea P, et al. Small molecule inhibition of ERK dimerization prevents tumorigenesis by RAS-ERK pathway oncogenes. Cancer Cell. 2015;28(2):170–182. doi:10.1016/j.ccell.2015.07.001
15. Dai Y, Wang L, Li D. Effectiveness of novel folate receptor-mediated staining solution detection (FRD) for cervical cancer screening. Medicine. 2018;97(34):e11868. doi:10.1097/MD.0000000000011868
16. Sherr C, Beach D, Shapiro G. Targeting CDK4 and CDK6: from discovery to therapy. Cancer Discov. 2016;6(4):353–367. doi:10.1158/2159-8290.CD-15-0894
17. Gashi G, Mahovlić V, Bahtiri E, et al. Assessment of the association between the frequency of micronucleus and p/Ki-67 co-expression in patients with cervical intraepithelial lesions. Biotech Histochem. 2018;93(7):496–504. doi:10.1080/10520295.2018.1462533
18. Sales Gil R, Vagnarelli P. Ki-67: more hidden behind a ‘Classic Proliferation Marker’. Trends Biochem Sci. 2018;43(10):747–748. doi:10.1016/j.tibs.2018.08.004
19. Liu W, Gong J, Xu H, et al. Good performance of p16/Ki-67 dual-stain cytology for detection and post-treatment surveillance of high-grade CIN/VAIN in a prospective, cross-sectional study. Diagn Cytopathol. 2020;48(7):635–644. doi:10.1002/dc.24427
20. Chen M, Wang H, Liang Y, et al. Establishment of multifactor predictive models for the occurrence and progression of cervical intraepithelial neoplasia. BMC Cancer. 2020;20(1):926. doi:10.1186/s12885-020-07265-7
21. Zhou Y, Fan W, Deng J, et al. Establishment and analysis of the prediction model for cervical squamous cell carcinoma. Eur Rev Med Pharmacol Sci. 2017;21(22):5042–5048. doi:10.26355/eurrev_201711_13816
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
