Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Pre-Procedure Blood Sugar Levels in Diabetic and High-Risk Patients Visiting King Abdulaziz University Dental Hospital: The Role of the Dentist in Diabetes Screening
Authors Al-Sebaei MO , Bamashmous M , Bassyoni L , Alsubaie R , Alnahdi DO
Received 22 January 2023
Accepted for publication 28 March 2023
Published 12 April 2023 Volume 2023:16 Pages 1021—1027
DOI https://doi.org/10.2147/DMSO.S405676
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Maisa O Al-Sebaei,1 Mohamed Bamashmous,2 Lojain Bassyoni,1 Rasha Alsubaie,3 Dania O Alnahdi4
1Department of Oral and Maxillofacial Surgery, King Abdulaziz University, Faculty of Dentistry, Jeddah, Saudi Arabia; 2Department of Public Health, King Abdulaziz University, Faculty of Dentistry, Jeddah, Saudi Arabia; 3Private Practice, Jeddah, Saudi Arabia; 4Taif Specialty Dental Centre MOH, Taif, Saudi Arabia
Correspondence: Maisa O Al-Sebaei, King Abdulaziz University, Faculty of Dentistry, PO Box 80209, Jeddah, 21589, Saudi Arabia, Tel +966553358482, Fax +966126404166, Email [email protected]
Aim: Diabetes mellitus (DM) is a widespread problem. Satisfactory control of DM is essential for maintaining oral health and optimizing the outcomes of dental treatment; DM patients with poor glycaemic control have a high risk of dental treatment-related complications. Furthermore, the dentist and dental office can play an important role in DM screening. Therefore, this study aimed at measuring random blood glucose (RBG) levels in patients with established DM or high risk of DM seeking dental treatment at the King Abdulaziz University Dental Hospital to avoid treatment complications and execute an immediate physician referral.
Methods and Material: This cross-sectional study included patients presenting to our institution for dental treatment, who were categorized as diabetic (established diagnosis) or at high risk of DM according to the American Diabetes Association criteria. Participants’ pre-procedure RBG level was assessed via a glucometer. High-risk participants were classified as per their blood glucose level into two groups (< 200 mg/dL and > 200 mg/dL), while the diabetic participants were placed into four groups (< 140 mg/dL; 140 to < 200 mg/dL; 200– 300 mg/dL; and > 300 mg/dL).
Results: This study included 695 patients (361 females and 334 males), of which 354 (52%) had established DM and 341 (48%) were high-risk patients. Around 31% of patients in the high-risk group were potentially diabetic but unaware of it; 46% of the diabetic patients had RBG levels > 200 mg/dL. For the high-risk participants, age had a statistically significant association (P-value 0.03) with the RBG level.
Conclusion: Pre-procedure RBG measurement in diabetic and high-risk patients undergoing dental treatment is crucial for the prevention of DM-related complications. Dental health-care professionals have a vital role in screening, early detection, and referral of these patients.
Keywords: blood glucose, dentists, diabetes complications, diabetes mellitus, screening
Introduction
Diabetes mellitus (DM) is a chronic disease and major global epidemic that affects the health and economy of individuals, families, and societies. The International Diabetes Federation (IDF) has determined that 9.3% of people worldwide are currently affected, which is estimated to increase to 10.2% by 2030 and 10.9% by 2045.1 Similarly, the American Diabetes Association (ADA) reported in 2019 that 1 out of 11 adults have DM.2
According to the World Health Organization (WHO), the Eastern Mediterranean region has the second-highest prevalence of DM among all WHO regions.3 According to the IDF, the Middle East and North Africa regions have the highest regional prevalence of DM (16.2%) among people aged 20–79 years, with approximately 1 in 3 adults living with DM remaining undiagnosed.4,5
In Saudi Arabia, the age-adjusted prevalence of DM was 18.7% in 2021; this number was estimated to increase to 20.4% by 2030 and 21.4% by 2045.6 This increase is expected due to urbanization, changes in lifestyle (unhealthy food, obesity, lack of physical activity), and ageing. Al-Rubeaan et al in 2015 reported that 6.2% of the Saudi population remained unaware of their DM.7 Makkah, Aljouf, Eastern region, Madinah, and Qassim were revealed to be the top five regions in Saudi Arabia in terms of DM prevalence with the respective prevalence of 43.4%, 41.7%, 37.2%, 35.4%, and 33.7%.8
A majority of the population visits a dental office each year in advanced economies. An Australian nationwide study of adult oral health has stated that more than half (56%) of adults saw a dentist in the last 12 months, and that 58% of adults reported that they usually visit the dentist at least once a year.9 In Canada, 75% of Canadians reported visiting the dental office in the past year.10 A cross-sectional study, which included participants from all over the Saudi kingdom, reported that 67.5% of the population are considered average visitors.11
The glucometer-based random blood glucose (RBG) test is an easy, non-invasive, and readily available tool to use in the dental setting. At the dental office, DM monitoring in general, and pre-procedure RBG monitoring in particular, are extremely important for all DM patients and those who are at risk of developing diabetes. Abnormal glucose levels can negatively affect the success of dental treatment and the ability of the body to heal after oral surgical procedures. Hence, RBG monitoring should be incorporated into the protocols of all dental offices, especially dental teaching institutions.
Therefore, the dental office offers an opportunity for the identification of high-risk individuals and undiagnosed diabetic patients who are unaware of their condition. The screening test of the RBG level can be easily utilized in dental clinics facilitating early medical intervention, thereby potentially limiting the burden of the disease and its complications on the community and the healthcare system.
Hence, this study aimed to report the mean RBG level of DM patients who are dental patients at the King Abdulaziz University Dental Hospital, and to demonstrate the importance of the role played by dental professionals in identifying potentially undiagnosed diabetic patients and high-risk individuals who could develop the disease in the future.
Materials and Methods
An observational cross-sectional study was conducted at King Abdulaziz University Dental Hospital between March 2019 and Dec 2019. All diabetic adult patients (18 years and older) and high-risk individuals for developing DM (according to the ADA criteria for testing for DM and prediabetes in asymptomatic adults) (Box 1) who presented for routine dental care were included in this study.12 The study sample was collected as a convenience sample from a total of 125,800 patient visits at the institution in the 10-month study period. The inclusion criteria for this study were as follows: patients voluntarily seeking dental treatment at King Abdulaziz University Dental Hospital during the study duration who are diagnosed with DM, or those deemed high-risk according to the ADA classification of patients at high risk for DM, who are aged between 18 and above, both with and without comorbidities. The exclusion criteria included non-diabetic patients, paediatric patients <18-years-old, and those who refused fingerstick testing for any reason.
 |
Box 1 ADA Criteria for Screening for Diabetes or Prediabetes in Asymptomatic Adults |
Collected parameters included: demographics (age, sex), past medical history, and RBG level. The blood sample was acquired from the capillary blood from the fingertip via a blood glucose meter OneTouch Select plus® (Lifescan Inc., Malvern, PA, USA), using the following protocol; the test strip was inserted into the glucometer, the finger-tip was prepared with an alcohol wipe, the fingertip was pricked with a lancing device, the blood sample was applied to the test strip and the result was read and recorded. Measurements were obtained by two trained and calibrated nurses.
The high-risk group was classified into two groups; <200 mg/dL and >200mg/dL since the ADA uses 200 mg/dL as the cut-off for diagnosis of DM based on random blood sugar in patients with classic symptoms of hyperglycaemia.12 The diabetic patients were classified into four groups according to their blood glucose level results as a distribution range of this sample (<140 mg/dL; 140 to <200 mg/dL; 200–300 mg/dL; and >300 mg/dL).
Statistical Analysis
All data were recorded in a data sheet utilizing Microsoft Office Excel 2013. Participants’ demographics and characteristics were expressed as counts and percentages. Logistic regression was performed for the high-risk participants to assess the predictors of age and gender with the outcome (above 200 mg/dL). Statistical significance was set at P < 0.05. All data were analysed using Statistical Package for the Social Science (SPSS Inc., Chicago, Illinois, USA) version 24 software.
This study was approved by the research ethics committee at King Abdulaziz University Faculty of Dentistry (IRB 115-10-15). Written informed consent was obtained from all the participating patients.
Results
This study had 695 participants of which 354 were diabetic patients with a previously established diagnosis and 341 had high risk for developing diabetes. The females slightly outnumbered the males (361 females, 334 males). The age of the participants ranged from 18 to 87 years with a mean age of 49.36 ± 14.95 years for all participants. The demographics and characteristics of both the high-risk and diabetic groups are shown in Table 1.
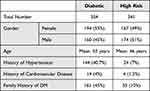 |
Table 1 Demographics and Characteristics of the Study Sample |
The results of the RBG for the high-risk and diabetic groups are shown in Table 2 and Table 3, respectively. Approximately 46% of the diabetic patients showed a blood glucose level of higher than 200 mg/dL, while approximately one-third (31%) of high-risk patients revealed a blood glucose level of higher than 200 mg/dL.
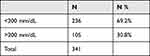 |
Table 2 Random Glucose Levels for High-Risk Participants |
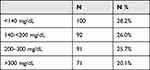 |
Table 3 Random Glucose Levels for the Diabetic Participants |
The outcome of RBG level (above 200mg /dL) in the high-risk group was tested for the predictors age and gender. Our regression model showed that gender was not statistically significant, whereas, for every one-year increase in age, the odds of having a RBG reading above 200 among individuals at high risk of DM increased by a factor of 2%, holding all other factors constant (OR = 1.02, 95% CI 1.00–1.03, P = 0.03) (Table 4).
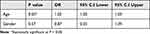 |
Table 4 Logistic Regression for Random Blood Glucose Level (<200 and >200) in the High-Risk Group |
All patients with RBG levels above 200 mg/dL were referred to the public medical centres that serve the neighbourhoods of these patients, either to establish a diagnosis of DM or prediabetes or ensure proper DM control and regular follow-up in already diagnosed patients. In total, 267 patients were referred. Dental treatment was deferred or modified until the patient was under the supervision of a physician, remained compliant with medication, and reached glycated haemoglobin (HbA1C) of less than 7% to ensure that the DM was well-controlled at treatment.13–15
Discussion
This study from a large academic centre in Saudi Arabia reaffirmed the undisputable role of dental offices and professionals in diabetes screening. In addition, it highlighted the need to reach satisfactory glycaemic control to improve dental treatment outcomes. The population in this study consisted of dental patients visiting our teaching institution. There was a diverse social and economic representation in our sample because of its location and free dental health services rendered. In the high-risk populations, one-third of the tested participants had a RBG of >200 which is suggestive of DM.
Few studies have demonstrated the role of dental professionals in opportunistic diabetes screening in Saudi Arabia. Alqurashi et al reported a similar result to ours in terms of diabetes prevalence, ie, 30% of the patients attending primary care clinics.16 Yet, other studies conducted in Saudi Arabia have reported lower prevalence; Zaini et al reported 8% of their sample to have DM;17 that their numbers fall short of ours could be attributed to their study being conducted in public locations like malls or women clubs and not in dental clinics. Patients visit dental clinics to address issues related to their oral health such as periodontal disease and teeth loss which are known to be strongly associated with DM.18–20 Al Ghamdi et al reported a prevalence of 16.45% and 15.8% for DM and prediabetes, respectively.21 Differing from ours, their study only included patients who were 40 years old and above. This might explain the higher prevalence of potential new cases in our study. However, our results reaffirmed the King Saud University 2017 study;22 the authors reported 10.2% of their participants to be at risk of DM and (63%) of them had a family history of DM.
Our results suggest that the measurement of pre-procedure RBG levels at the dental office would yield valuable information to the patient about their medical condition and alarm them to seek professional help. In addition to helping the dentists to determine the dental treatment plan and prevent oral diseases, as there is a strong correlation between glycaemic control and oral health.18
Our data also showed that 31% of the high-risk group had readings above 200 mg/dL with readings reaching 379.25 mg/dL. This group is at high risk of having undiagnosed DM that is not treated or under the care of a physician. This subjects them to the risk of microvascular and macrovascular complications if they remain undiagnosed and untreated. Additionally, approximately half (46%) of the Diabetic participants have a RGB of >200 mg/dL, which is not indicative of poor glycaemic control per se, but warrants further testing with HbA1C and fasting blood sugar for establishing glycaemic control which is vital to avoid complications during dental treatment.12
In this study, the percentage of diabetic patients who had RBG reading above 200 mg/dL was almost half of the diabetic sample (46%), which could indicate poor compliance with drugs, diet, or physician care. According to the ADA Standards of Medical Care in Diabetes,12 the target HbA1C of a diabetic patient should be <7%. Although the RBG in this sample does not reflect the true glycaemic control of the individual, as HbA1C and fasting blood glucose are indicated for diagnosis and to assess control,12 the ADA generally recommends that the target blood sugar levels be 80–130 mg/dL fasting and <180 mg/dL 2 hours post-prandial.
Moreover, the ADA states that RBG of more than 200 mg/dL is suggestive of DM. Therefore, our study supports the feasibility of RBG in the dental clinic as a screening method for abnormal blood glucose levels and potential DM diagnosis; the process was well accepted by patients and practitioners. In addition, Rosedale et al,23 Barasch et al,24 Estrich et al,25 Al Ghamdi et al21 and others26–28 have also supported the use of community dental practices as opportunistic venue for DM screening; they claimed it would result in improving DM diagnosis and control and that the screening method used (fingerstick) is well accepted by the patients.
Furthermore, our results suggest that individuals should be made more aware of the possibility of having DM when one or more of the risk factors are present, especially non-modifiable risk factors including family history. Patient education through brochures and community campaigns can play a role in addressing that issue. The dentist is a pivotal health-care advocate who needs to educate the patient about the importance of following up with their primary physicians to establish a diagnosis and/or have their blood glucose levels controlled.
However, his study had several limitations. This was a single-centre study from an academic centre and the findings may need to be confirmed in a multi-centre study representing different geographical locations in Saudi Arabia. This study might not be reflective of the situation in non-academic centres, especially small dental offices in Saudi Arabia. The results of this study should be cautiously interpreted for populations residing in other countries outside the Arabian Peninsula and especially those comprising non-Mediterranean populations. In addition, the results of this study were based only on a single pre-procedure measurement of glucometer measured RBG. Ideally, diabetes screening may require more measurements and types of tests, such as HbA1C, or fasting and post-prandial samples. Moreover, this study could not analyse the impact of screening as only limited data were collected in this study. Future studies could assess the health and economic impact of diabetes screening in dental offices in Saudi Arabia.
Conclusion
In conclusion, our findings suggest that dental practitioners have a crucial role in the screening, early detection, and referral of diabetic and pre-diabetic patients in Saudi Arabia. Diabetic progression contributes to comorbid complications, which further contribute to a decline in quality of life. Screening for an undiagnosed systemic disease, such as DM in the dental setting can be viewed a highly valuable service to the public health because early detection offers several benefits, such as reduction in the long-term comorbidities, mortalities, and high costs on the health systems associated with the DM.
Abbreviations
ADA, American Diabetes Association; DM, Diabetes mellitus; HbA1C, Glycated haemoglobin; IDF, International Diabetes Federation; RBG, Random blood glucose; WHO, World Health Organization.
Data Sharing Statement
The data set used in the current study is available upon request from author: Maisa O. Al-Sebaei, [email protected].
Ethical Policy and Institutional Review Board Statement
This study was approved by the Research Ethical Committee at King Abdulaziz University Faculty of Dentistry (REC-FD), approval #115-10-18, on 13/2/2019. All the procedures have been performed as per the ethical guidelines laid down by the Declaration of Helsinki.
Patient Declaration of Consent Statement
All the procedures have been performed as per the ethical guidelines laid down by the Declaration of Helsinki.
Acknowledgments
The manuscript adheres to the STROBE reporting guidelines for observational studies.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study has not received a grant or funding from any source.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
2. American Diabetes Association. Statistics about diabetes. Available from: https://diabetes.org/about-us/statistics/about-diabetes.
3. World Health Organization. Diabetes factsheet. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes.
4. International Diabetes Federation. Diabetes estimates (20–79 y): age-adjusted comparative prevalence of diabetes, %. Available from: https://diabetesatlas.org/data/en/indicators/2/.
5. International Diabetes Federation Middle East and North Africa diabetes report 2000 — 2045. Available from: https://diabetesatlas.org/data/en/region/4/mena.html.
6. International Diabetes Federation. IDF diabetes atlas, Tenth Edition. Available from: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf.
7. Al-Rubeaan K, Al-Manaa H, Khoja T, et al. The Saudi abnormal glucose metabolism and diabetes impact study (Saudi-DM). Ann Saudi Med. 2014;34:465–475. doi:10.5144/0256-4947.2014.465
8. Alotaibi A, Perry L, Gholizadeh L, Al-Ganmi A. Incidence and prevalence rates of diabetes mellitus in Saudi Arabia: an overview. J Epidemiol Glob Health. 2017;7:211–218. doi:10.1016/j.jegh.2017.10.001
9. Chrisopoulos S, Ellershaw A, Luzzi L. National study of adult oral health 2017–18: study design and methods. Aust Dent J. 2020;65(Suppl 1):S5–S10. doi:10.1111/adj.12758
10. Statistics Canada. Health factsheets, dental care; 2018. Available from: https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00010-eng.htm.
11. Linjawi AI, Bahaziq AM, Qari AH, et al. Impact of dental visits on oral health awareness in Saudi Arabia. J Contemp Dent Pract. 2019;20:783–788. doi:10.5005/jp-journals-10024-2597
12. ElSayed NA, Aleppo G, Aroda VR, et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. 2023;46:S19–S40. doi:10.2337/dc23-S002
13. Miller A, Ouanounou A. Diagnosis, management, and dental considerations for the diabetic patient. J Can Dent Assoc. 2020;86:k8.
14. Patton L, Glick M. The ADA practical guide to patients with medical conditions, 2nd Edition. Available from: https://www.wiley.com/en-gb/The+ADA+Practical+Guide+to+Patients+with+Medical+Conditions%2C+2nd+Edition-p-9781118924402.
15. American Diabetes Association. Diabetes: dental considerations for people with diabetes. Available from: https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/diabetes.
16. Alqurashi KA, Aljabri KS, Bokhari SA. Prevalence of diabetes mellitus in a Saudi community. Ann Saudi Med. 2011;31:19–23. doi:10.4103/0256-4947.75773
17. Zaini RG, Abdulsatar S. Detection of undiagnosed diabetes among Saudi female at four campaigns in Taif City, Saudi Arabia. Available from: https://www.researchgate.net/publication/305654026_Detection_of_Undiagnosed_Diabetes_among_Saudi_Female_at_Four_Campaigns_in_Taif_City_Saudi_Arabia.
18. Lamster IB, Lalla E, Borgnakke WS, Taylor GW. The relationship between oral health and diabetes mellitus. J Am Dent Assoc. 2008;139:19S–24S. doi:10.14219/jada.archive.2008.0363
19. Liljestrand JM, Havulinna AS, Paju S, et al. Missing teeth predict incident cardiovascular events, diabetes, and death. J Dent Res. 2015;94:1055–1062. doi:10.1177/0022034515586352
20. Luo H, Pan W, Sloan F, Feinglos M, Wu B. Forty-year trends in tooth loss among American adults with and without diabetes mellitus: an age-period-cohort analysis. Prev Chronic Dis. 2015;12. doi:10.5888/pcd12.150309
21. AlGhamdi AST, Bukhari SMN, Elias WY, et al. Dental clinics as potent sources for screening undiagnosed diabetes and prediabetes. Am J Med Sci. 2013;345:331–334. doi:10.1097/MAJ.0b013e318287c96c
22. Hadlaq EM, Faraj ZT, Al Gamdi FM, et al. Early screening of diabetes and hypertension in primary care dental clinics at King Saud University in Riyadh, Kingdom of Saudi Arabia. J Contemp Dent Pract. 2017;18:652–659. doi:10.5005/jp-journals-10024-2101
23. Rosedale MT, Strauss SM. Diabetes screening at the periodontal visit: patient and provider experiences with two screening approaches. Int J Dent Hyg. 2012;10:250–258. doi:10.1111/j.1601-5037.2011.00542.x
24. Barasch A, Safford MM, Qvist V, et al. Random blood glucose testing in dental practice: a community-based feasibility study from The Dental Practice-Based Research Network. J Am Dent Assoc. 2012;143:262–269. doi:10.14219/jada.archive.2012.0151
25. Estrich CG, Araujo MWB, Lipman RD. Prediabetes and diabetes screening in dental care settings: NHANES 2013 to 2016. JDR Clin Transl Res. 2019;4:76–85. doi:10.1177/2380084418798818
26. Herman WH, Taylor GW, Jacobson JJ, et al. Screening for prediabetes and type 2 diabetes in dental offices. J Public Health Dent. 2015;75:175–182. doi:10.1111/jphd.12082
27. Glurich I, Bartkowiak B, Berg RL, Acharya A. Screening for dysglycaemia in dental primary care practice settings: systematic review of the evidence. Int Dent J. 2018;68:369–377. doi:10.1111/idj.12405
28. Harase T, Nishida W, Hamakawa T, et al. Clinical implication of blood glucose monitoring in general dental offices: the Ehime Dental Diabetes Study. BMJ Open Diabetes Res Care. 2015;3:e000151. doi:10.1136/bmjdrc-2015-000151
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
