Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Pre-Existing Diabetes Limits Survival Rate After Immune Checkpoint Inhibitor Treatment for Advanced Lung Cancer: A Retrospective Study in Japan
Authors Hisanaga K, Uchino H , Kakisu N, Miyagi M , Yoshikawa F, Sato G, Isobe K, Kishi K, Homma S, Hirose T
Received 29 October 2020
Accepted for publication 11 January 2021
Published 22 February 2021 Volume 2021:14 Pages 773—781
DOI https://doi.org/10.2147/DMSO.S289446
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Kaori Hisanaga, 1 Hiroshi Uchino, 1 Naoko Kakisu, 1 Masahiko Miyagi, 1 Fukumi Yoshikawa, 1 Genki Sato, 1 Kazutoshi Isobe, 2 Kazuma Kishi, 2 Sakae Homma, 3 Takahisa Hirose 1
1Division of Diabetes, Metabolism and Endocrinology, Department of Medicine, Toho University Graduate School of Medicine, Tokyo, Japan; 2Department of Respiratory Medicine, Toho University Graduate School of Medicine, Tokyo, Japan; 3Department of Advanced and Integrated Interstitial Lung Disease Research, School of Medicine, Toho University, Tokyo, Japan
Correspondence: Hiroshi Uchino
Division of Diabetes, Metabolism and Endocrinology, Department of Medicine, Toho University Graduate School of Medicine, 6-11-1 Omori-Nishi, Ota-Ku, Tokyo, 143-8541, Japan
Tel +81-3-3762-4151
Fax +81-3-3765-6488
Email [email protected]
Background: Although immune checkpoint inhibitors (ICIs) are promising in the treatment of advanced cancer, their use is associated with immune-related adverse events (irAEs) that affect endocrine organ systems. Although development of irAEs was associated with improved cancer-specific survival, the risk of irAEs is unclear. We investigated the association of pre-ICI comorbidities—including diabetes—with irAEs, overall survival (OS), and progression-free survival (PFS) in advanced lung cancer.
Methods: Patients with lung cancer who were treated with ICIs during the period from September 1, 2015 through July 31, 2018 were retrospectively enrolled. All data were collected from the NEPTUNE database of university patients. Hazard ratios were estimated by using Cox regression weighted for propensity scores. Odds ratios were calculated by logistic regression and adjusted for unbalanced variables. The Kaplan–Meier method was used to compare OS, and the generalized Wilcoxon test was used to compare median survival.
Results: Among the 88 patients identified, 22 (25.0%) had diabetes (DM) before ICI treatment and 57 (75.0%) did not (non-DM); irAEs developed in 12.2% of patients with DM and in 9.1% of patients in non-DM (p=0.87). Diabetes status was not associated with irAE risk in relation to baseline characteristics (age, sex, TNM staging, thyroid and renal function) or in propensity score–matched analysis (age, TNM staging). During a mean follow-up of 30 months, OS and cancer-specific PFS were significantly higher in patients who developed irAEs (Kaplan–Meier estimates, p=0· 04 and 0· 03, respectively). In propensity score–matched analysis, diabetes was significantly associated with lower OS (multivariate hazard ratio, 0· 36; 95% CI, 0· 13– 0· 98) unrelated to irAEs. Irrespective of irAEs, PFS was also lower among patients with DM than among non-DM patients (Kaplan–Meier estimate, p=0· 04).
Conclusion: Pre-existing diabetes was associated with higher mortality in advanced lung cancer, regardless of irAE development during treatment with ICI.
Keywords: immune checkpoint inhibitor, diabetes, overall survival, progression-free survival
Corrigendum for this paper has been published
Article Summary
- Although immune checkpoint inhibitor (ICI) treatment yields satisfactory outcomes for advanced cancer, immune-related adverse events (irAEs) are still concern.
- Development of irAEs was associated with better cancer-specific survival outcomes; however, the risk factors are not well understood.
- This study investigated pre-ICI comorbidities, including diabetes, that are potentially associated with irAE rates. However, pre-existing diabetes has shorter overall and progression-free survival in advanced lung cancer, despite no relation to irAEs.
Introduction
The development of immune checkpoint inhibitors (ICIs) is an important milestone in cancer therapy. In a randomised controlled trial of cancer adjuvants for NSCLC patients, response duration and overall survival were longer for nivolumab than for docetaxel.1 There are three types of ICIs, and six products have been approved in Japan (ipilimumab, nivolumab, pembrolizumab, avelumab, atezolizumab, and durvalumab). Nivolumab and pembrolizumab—monoclonal antibodies that target the programmed cell death 1 (PD-1) protein on cell surfaces—have been approved for treatment of metastatic non–small cell lung cancer (NSCLC) since 2015.
The superior effectiveness of nivolumab is now reflected in the development and revision of guidelines for NSCLC and other solid cancers.2–5 New classes of drugs (eg, ICIs) that improve patient outcomes in advanced NSCLC are expected to be more widely used in the future.1,6
ICI can trigger autoimmune-related reactions in organ systems. Such reactions are referred as immune-related adverse events (irAEs). irAEs are among the most frequent toxicities (around 10% of irAEs) including thyroid disorders, hypophysitis, diabetes mellitus, and adrenalitis. Treatment is based on the replacement of specific hormone deficits, accompanied by immunosuppression (with corticosteroids or other drugs), depending on irAEs’ grade, often without the need of ICI withdrawal, except in more severe forms.7–10
Development of irAEs was found to be positively associated with survival,11,12 and risk factors associated with irAEs, including age, sex, gene mutations, and smoking status, are currently being investigated worldwide.13,14 However, antecedent factors related to irAEs and the precise mechanisms involved are unknown. Therefore, we investigated comorbidities associated with irAEs, as such comorbidities might be related to overall survival (OS) and progression-free survival (PFS).
Lung cancer mortality rates are lower for patients with diabetes than for normoglycemic patients.15–17 Diabetes might therefore have some effect on chemotherapeutic agents used to treat cancer. To our knowledge, no study has examined the association between diabetes status before ICI treatment and outcomes of treatment for advanced lung cancer. Our primary hypothesis is that glucose tolerance inversely correlate to the rate of irAEs, that of limited efficacy in ICI treatment, resulting in the poor cancer-specific OS and PFS with pre-treatment diabetes.
Methods
Patients and Public Involvement
This study was conducted in the Division of Diabetes, Metabolism, and Endocrinology, Department of Internal Medicine, at Toho University School of Medicine, Tokyo, Japan. The participants were patients with lung cancer or mediastinal tumours that were treated with nivolumab or pembrolizumab in the department of respiratory medicine during the period from January 2015 through February 2019.
Study Design
The first anti–PD-1 antibody treatment was approved in Japan in 2014, and all data for patients at our centre who received anti–PD-1 antibodies for lung cancer were collected from the NEPTUNE database in which all the patients were registered in our university hospital. Using propensity-score matching, we conducted a 1:1 (diabetes/non-diabetes) matched case–control analysis18 and a comprehensive comparison of cofounding factors affecting lung cancer outcomes for patients with and without diabetes.
The study protocol and all procedures were in accordance with the ethical standards of the Ethics Committee of Toho University Omori Medical Center and the1964 Helsinki Declaration and its amendments and were approved by the Ethics Committee of Toho University Omori Medical Center (M19129). This trial was registered with the University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) as JPRN-UMIN 000037931. For further details of propensity-score matching, see Supplementary Appendix 1–3. All supplementary data are available upon reasonable request to the corresponding author.
Statistical Analysis
We used multiple logistic regression to calculate adjusted odds ratios (ORs) to compare OS and PFS in patients with and without diabetes who had advanced lung cancer.
Because patients with diabetes before ICI treatment were more likely to have risk factors (including age, sex, year of diagnosis, comorbidity, cancer type, and TNM staging) related to shorter OS,15–17 we attempted to reduce selection bias by using propensity scoring to match age, sex, and TNM staging. For the matched and unmatched groups, no factors significantly differed in relation to diabetes status.
After the propensity score was estimated, patients with diabetes were matched in a 1:1 ratio to those without diabetes. For multiple comparisons of normally distributed variables between more than two groups, one-way analysis of variance was used with the post-hoc t-test. For time-to-event variables, survival functions were estimated with the Kaplan–Meier method and compared with the Log rank test. Cox proportional hazards regression was used to obtain hazard ratios.
Univariate Cox proportional-hazards models were performed for both PFS and OS for three predicted variables, age, sex, TMN staging. Statistically significant predictor variables (p<0.5) on univariate analysis were then included in multivariate Cox proportional hazards models, which were performed to compare the effects of DM on PFS and OS when controlling for potential confounding variables.19–22
Role of the Funding Source
The authors received no external funding. All the authors had full access to all data in the study and consented to publication of the manuscript.
Results
Baseline Cohorts
Baseline and disease characteristics for propensity score matched and unmatched cohorts are summarized in Table 1. Propensity-score matching was used to mitigate the effect of potential selection bias. In matched-pair samples, the mean distance in the estimated propensity score was 0.2. Overall, both groups were well balanced. In unmatched analysis, factors in pretreatment DM and non DM were, age (yr) (66.58±9.86 vs 66.17±9.85, p=0.86), gender (M/F %) (87.5/12.5 vs 79.7/20.3, p=0.22), tumor type (adenomatous/squamous/others/unknown %)(45.8/37.5/8.3/8.3 vs 65.6/21.9/6.3/6.3, p=0.16), TMN staging (I/II/III/IV %, 8.3/12.5/29.2/50 vs 9.4/9.4/25.0/56.3, p=0.16), %-PD1 expression (0.48±0.20 vs0.35±0.40, p=0.22), Cre (mg/dL) (0.70±0.18 vs 0.77±0.20, p=0.08), BS (mg/dl) (159.8±98.6 vs 11.3±20.8, p=0.03), FT3 (pg/mL) (2.71±0.55 vs 2.84±0.55, p=0.33), FT4 (ng/mL) (1.30±0.19 vs 1.29±0.18, p=0.53), TSH (μIU/mL) (1.20±1.40 vs 2.18±2.30, p=0.51), C-peptide (ng/mL) (2.68±1.83 vs 3.30±2.90, p=0.23), cortisol (μg/dl) (8.53±0.16 vs 10.13±6.05, p=0.28), irAEs (%) (p=0.39), OS (12.30±10.00 vs 14.4±9.73, p=0.38), and Tx number (9.17±11.90 vs 11.34±11.90, p=0.45). In matched analysis, factors in pretreatment DM and non DM were age (yr) (64.91±10.32 vs 65.7±10.02, p=0.7), gender (%) (p=0.10), tumor type (%) (p=0.13), TMN stageing (%) (p=0.084), %-PD1 (0.26±0.38 vs0.32±0.39, p=0.52), Cre (mg/dL) (0.76±0.19 vs 0.77±0.19, p=0.24), BS (mg/dl) (113.9±22.0 vs 113.27±21.21, p=0.87), FT3 (pg/mL) (2.89±0.57 vs 2.87±0.56, p=0.91), FT4 (ng/mL) (1.30±0.17 vs 1.29±0.19, p=0.21), TSH (μIU/mL) (2.23±2.28 vs 2.25±2.39, p=0.54), C-peptide (ng/mL) (3.04±2.45 vs 3.33±3.0, p=0.63), cortisol (μg/dl) (9.70±6.11 vs 9.75±6.19, p=0.81), irAEs (%) (p=0.18), OS (14.14±10.25 vs 14.75±10.31, p=0.744), and Tx number (10.83±11.78 vs 11.41±12.31, p=0.731).
 |
Table 1 Baseline Characteristics of the Patients |
irAEs
Patients treated with other ICIs were excluded, and only endocrine irAEs were selected. Among 88 patients, 27% (n=24) had diabetes before ICI treatment and 73% (n=64) did not. They were followed during February 2019, and development of irAEs (thyroid dysfunction, hypopituitarism, adrenal insufficiency, and insulin-deficient diabetes) was investigated and recorded.
Of the 88 patients who were treated with ICI during the study period, 4.5% (n=1) of those with diabetes and 10.6% (n=7) of those without diabetes developed irAEs. All the patients who developed irAEs of thyroid disorders, and two of them had adrenalitis. Treatment is based on the replacement of specific hormone deficits, accompanied by immunosuppression. Eight of three people have to take levothyroxine sodium hydrate and amount is average of 50 μg/day. Three patients of adrenalitis take Hydrocortisone of 15 mg/day. The patients with diabetes had worse control of blood sugar lever after developing irAEs.
Survival Rates
OS and PFS were estimated in the two groups. Figure 1A shows Kaplan–Meier curves for OS, and Figure 1B shows cancer-specific PFS, with and without irAEs. As was noted in previous studies,11,12 outcomes were better in patients with irAEs than in those without irAEs (OS, p=0.02; PFS, p=0.04). Figure 2A shows the Kaplan–Meier curves for cancer-specific PFS, and Figure 3 shows the Kaplan–Meier curves for OS for all patients. PFS was shorter for patients with diabetes (n=24) than for those without diabetes (n=64) (p<0.05). In addition, PFS was significantly shorter in patients with diabetes. PFS was affected only by lung cancer, which indicates that diabetes directly affects survival rate in lung cancer patients. Table 2 shows the multivariate Cox proportional hazards regression model for cancer-specific PFS and OS. In univariate and multivariate analyses, diabetes status was not significantly associated with OS or PFS in the entire, unmatched cohort; however, after propensity-score matching, OS was significantly shorter (p=0.04) in patients with diabetes.
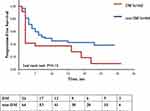 |
Figure 2 Kaplan–Meier curves for cancer-specific progression-free survival in the DM and non-DM groups (red line, DM group; blue line, non-DM group). |
 |
Figure 3 Kaplan–Meier curves for overall survival in the DM and non-DM groups (red line, DM group; blue line, non-DM group). |
 |
Table 2 Multivariate Cox Proportional Hazards Regression Model of Cancer-Specific Progression-Free Survival and Overall Survival in the Unmatched and Matched Cohorts |
Discussion
We hypothesized that the presence of diabetes before ICI treatment would be associated with fewer irAEs in patients receiving treatment for advanced lung cancer. However, diabetes status was not associated with irAE rate but was associated with shorter PFS in DM patients. The structural and conformational dynamics of the immune-related cancer agents nivolumab and pembrolizumab are referred to as anti–PD-1 antibody.1 Tumour cells express programmed death-ligand 1 (PD-L1) on their surface, to avoid attack from the immune system. However, PD-L1 binds to PD-1, which is expressed on the surface of T cells, thereby suppressing the immune system. Anti–PD-1 antibody binds to PD-1, thus inhibiting the interaction of cancer cells and immune cells.23 These are the key mechanism in the ICI treatment and the magnitude of glucose tolerance before the treatment is unclear. Of greatest interest is, this immunotherapeutic approach is often associated with immune-mediated toxic events, known as irAEs. Interestingly, irAEs were found to be associated with improved OS and cancer-specific PFS in several advanced cancers.11,12 Unfortunately, in patients with pre-existing diabetes, our results failed to elucidate the relationship between decreased post-ICI treatment OS/PFS with the rate of irAEs an advanced cancer.
Diabetes and Immune Reactivity
The state of diabetes might affect immune activity. During ICI treatment, its cognate antigen triggers an immune response by which several T cell clones target cancer cells.24 A recent study reported that diabetes is a chronic, low-grade inflammatory disease in which expression or activation of immune-related molecules is altered.25 T cells differentiate into various types of immune cells by specific stimulation and in relation to the source of energetic nutrient transport. Under conditions of normoglycemia, naive T cells use lipids as their predominant energy substrate to differentiate regulatory T cells. However, under conditions of hyperglycaemia, glucose is mainly used as the energy substrate to differentiate to Th17.26 Furthermore, PD-1 expression on tumour cell surfaces is diminished in diabetes, which blunts the response to activated T cells.27 Although hyperglycaemia, including diabetes, is known to alter immune T cell activity, the response to ICI in the context of advanced cancer treatment is not well understood. Our findings showed no association between diabetes before ICI and irAEs incidence, which was associated with subsequent OS and PFS. The results were similar in the PFS-matched cohort and overall, ie, in the unmatched cohort.
Diabetes and Cancer-Specific Outcomes
Ten percent of the world population will develop diabetes during their life,28 and 55% of persons with diabetes will receive a cancer diagnosis. The mechanisms underlie diabetes and cancer may play a role in the developing of both disease activity; that is, the increase in body weight, the increases risk of diabetes and cancer.29 The link between the two diseases (diabetes and cancer) results in worse outcomes for both.30,31 However, “obesity paradox” has been reported in several advanced cancer. The patients with obesity may have better outcome in treating with ICI, in which the impact of body adiposity might be related to the irAEs development.32 A nutritional status has a pleiotropic effect on an individual patient background, both synergically acting in producing cancer treatment outcomes. Because of such complex interactions, a clear cause-effect relationship between BMI and cancer treatment survival seems to be difficult to carry out, we avoid to simply compare the body weight in this study.
PFS was poor in the present patients with diabetes. Diabetes before ICI treatment was associated with worse PFS in lung cancer patients, and pre-treatment diabetes was associated with poor outcomes after chemotherapy for other cancers.33,34
Diabetes and cancer share several intrinsic risk factors (obesity, poor diet, and aging),33 and our results indicate that diabetes was associated with worse OS and PFS, regardless of irAEs development. Although the underlying biological mechanisms are unclear, several hypotheses have been suggested. First, hyperinsulinemia and hyperglycaemia associated with diabetes may increase tumour cell proliferation and metastasis.33 Adipose tissue inflammation may have a role, and insulin resistance might further enhance production of inflammatory cytokines, which could alter the immune system.33 Secondly, patients with diabetes are more likely to develop adverse effects during chemotherapy, which decreases the effectiveness of such treatments.33,34 Although ICI clearly improve outcomes in patients with advanced lung cancer, they are costly and associated with irAEs. In our current health care environment, policymakers, providers, and patients need more evidence in order to determine the value of therapeutic alternatives to ICI treatment. Covariates that could affect ICI effectiveness should be examined. Inappropriate ICI treatment results in detrimental risks, both in social health costs and patient selection bias. Our results shed light on the positive effects of ICI on OS and PFS in patients without diabetes before ICI treatment.
Limitations
The present study has limitations. It was retrospective and enrolled only a small number of Japanese patients at a single centre. In addition, it does not reflect the entire lifespan, namely, time to onset and to disease resolution. Therefore, research encompassing more of the patient’s lifetime might elicit different findings. Large-scale, multicentre and multiple cancer types with prospective studies are needed.
Conclusions
Pre-treatment diabetes status was not associated with subsequent risk of irAEs. However, patients with advanced lung cancer who developed irAEs after ICI treatment had better OS and PFS. The unforeseen risks of irAEs during ICI treatment are an important consideration in improving cancer outcomes. To optimise selection of patients likely to benefit from ICI treatment, future studies should attempt to identify predictors of irAEs. Moreover, tumor genetic profiling in the context of clinical research protocols might allow future studies to identify matched targeted therapy to ICIs, assess the clinical impact of a precision medical approach for cancer, and make additional sequencing data from patients with diabetes available to the research community.
Data Sharing Statement
Data on the findings of the current study are available from the corresponding author.
Ethics Approval
The study protocol and all procedures were in accordance with the ethical standards of the Ethics Committee of the Toho University Omori Medical Center Hospital and the 1964 Helsinki Declaration and its amendments and were approved by the Ethics Committee of Toho University Omori Medical Center (M19129). This trial was registered with the University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) as JPRN-UMIN 000037931.
Acknowledgment
We are grateful to all the individuals who participated in this study. The authors thank Dr. Chiaki Nishimura for assistance with statistical analysis.
Author Contributions
HU coordinated the study, and KH, KN, MM, FY, GS, KI, and SH codesigned the study. KH, HU, and TH were responsible for screening and enrolling participants, arranging informed consent from participants, and providing patient care. KH, HU, and TH wrote the report. FY, GS, and KI contributed to data analysis, including the statistical analyses. SH designed and implemented the clinical variables. HU, KH, MM, FY, GS, KI, SH, and TH contributed to the interpretation of the results. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study received no external funding.
Disclosure
Takahisa Hirose received research support from Ono, speaker honoraria from Sanofi, Eli Lilly, Novo Nordisk, Merck (MSD), Dainippon-Sumitomo, AstraZeneca, Tanabe-Mitsubishi and Kowa Company and research support from AstraZeneca, Tanabe and Novo Nordisk. The authors report no other potential conflicts of interest for this work.
References
1. Horn L, Spigel DR, Vokes EE, et al. Nivolumab versus docetaxel in previously treated patients with advanced non-small-cell lung cancer: two-year outcomes from two randomized, open-label, Phase III trials. J Clin Oncol. 2017;35(35):3924–3933. doi:10.1200/JCO.2017.74.3062
2. Bironzo P, Di MM. A review of guidelines for lung cancer. J Thorac Dis. 2018;10(Suppl S13):S1556–S1563. doi:10.21037/jtd.2018.03.54
3. Umeweni N, Knight H, McVeigh G. NICE guidance on necitumumab for untreated advanced or metastatic squamous non-small-cell lung cancer. Lancet Oncol. 2016;17(11):1483–1484. doi:10.1016/S1470-2045(16)30488-0
4. Hallz CJ, Umeweni N, Knight H, Smith L. NICE guidance on ramucirumab for previously treated locally advanced or metastatic non-small-cell lung cancer. Lancet Oncol. 2016;17(10):1357–1358. doi:10.1016/S1470-2045(16)30435-1
5. Hadoux J, Pacini F, Tuttle RM, et al. Management of advanced medullary thyroid cancer. Lancet Diabetes Endocrinol. 2016;4(1):64–71. doi:10.1016/S2213-8587(15)00337-X
6. Kato K, Cho BC, Takahashi M, et al. Nivolumab versus chemotherapy in patients with advanced oesophageal squamous cell carcinoma refractory or intolerant to previous chemotherapy (ATTRACTION-3): a multicentre, randomised, open-label, Phase 3 trial. Lancet Oncol. 2019;20(11):1506–1517. doi:10.1016/S1470-2045(19)30626-6
7. Baxi S, Yang A, Gennarelli RL, et al. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: systematic review and meta-analysis. BMJ. 2018;360:k793. doi:10.1136/bmj.k793
8. Byun DJ, Wolchok JD, Rosenberg LM, et al. Cancer immunotherapy—immune checkpoint blockade and associated endocrinopathies. Nat Rev Endocrinol. 2017;13(4):195–207. doi:10.1038/nrendo.2016.205
9. Romualdo B-S, WillBarry T, Garrido-Castro AC, et al. Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens. JAMA Oncol. 2018;4(2):173–182. doi:10.1001/jamaoncol.2017.3064
10. Ruggeri RM, Campennì A, Giuffrida G, et al. Endocrine and metabolic adverse effects of immune checkpoint inhibitors: an overview (what endocrinologists should know). J Endocrinol Invest. 2019;42(7):745–756. doi:10.1007/s40618-018-0984-z
11. Haratani K, Hayashi H, Chiba Y, et al. Association of immune-related adverse events with nivolumab efficacy in non–small cell lung cancer. JAMA Oncol. 2018;4(3):374–378. doi:10.1001/jamaoncol.2017.2925
12. Ricciuti B, Genova C, De GA, et al. Impact of immune-related adverse events on survival in patients with advanced non-small cell lung cancer treated nivolmab: long-term outcomes from a multi-institutional analysis. J Cancer Res Clin Oncol. 2019;145(2):479–485. doi:10.1007/s00432-018-2805-3
13. Nakamura Y. Biomarkers for immune checkpoint inhibitor-mediated tumor response and adverse events. Front Med (Lausanne). 2019;6(119).
14. Kartolo A, Sattar J, Sahai V, et al. Predictors of immunotherapy-induced immune-related adverse events. Oncology. 2018;25(5):e403–e410.
15. Zhu L, Cao H, Zhang T, et al. The effect of diabetes mellitus on lung cancer prognosis. Medicine. 2016;95(17):e3528. doi:10.1097/MD.0000000000003528
16. Luo J, hendryx M, Qi L, et al. Pre-existing diabetes and lung cancer prognosis. Br J Cancer. 2016;115(1):76–79. doi:10.1038/bjc.2016.141
17. Kurishima K, Watanabe H, Ishikawa H, et al. Survival of patients with lung cancer and diabetes mellitus. Mol Clin Oncol. 2017;6(6):907–910. doi:10.3892/mco.2017.1224
18. Drake C, Fisher L. Prognostic models and the propensity score. Int J Epidemiol. 1995;24(1):183–187. doi:10.1093/ije/24.1.183
19. Alssab HO, Sau S, Alzhrani R, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8:561. doi:10.3389/fphar.2017.00561
20. Paz-Ares L, Tan E-H, O’Byrne K, et al. Afatinib versus gefitinib in patients with EGFR mutation-positive advanced non-small-cell lung cancer: overall survival data from the phase IIb LUX-Lung 7 trial. Ann Oncol. 2017;28(2):270–277. doi:10.1093/annonc/mdw611
21. Wang Y, Guan S, Bi Y, et al. Survival impact of delaying postoperative radiotherapy in patients with esophageal cancer. Transl Oncol. 2018;11(6):1358–1363. doi:10.1016/j.tranon.2018.08.007
22. Xu LT, Funchain PF, Bena JF, et al. Uveal melanoma metastatic to the liver: treatment trends and outcomes. Ocul Oncol Pathol. 2019;5(5):323–332. doi:10.1159/000495113
23. Georgakis MK, Tsivgoulis G, Spinos D, et al. Prognostic factors and survival of gliomatosis cerebri: a systematic review and meta-analysis. World Neurosurg. 2018;120:e818–e854. doi:10.1016/j.wneu.2018.08.173
24. Chaplin DD. Overview of the immune response. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S3–23. doi:10.1016/j.jaci.2009.12.980
25. Tsalamandris S, Antonopoulos AS, Oikonomou E, et al. The role of inflammation in diabetes: current concepts and future perspectives. Eur Cardiol. 2019;14(1):50–59. doi:10.15420/ecr.2018.33.1
26. Berod L, Friedrich C, Nandan A, et al. De novo fatty acid synthesis controls the fate between regulatory T and T helper 17 cells. Nat Med. 2014;20(11):1327–1333. doi:10.1038/nm.3704
27. Jia Y, Zhao Y, Li C, et al. Unlike PD-L1, PD-1 is downregulated on partial immune cells in type 2 diabetes. J Diabetes Res. 2019;5035261.
28. Goto A, Noda M, Inoue M, et al. Increasing number of people with diabetes in Japan: is this trend real? Intern Med. 2016;55(14):1827–1830. doi:10.2169/internalmedicine.55.6475
29. Eibl G, Cruz-Monserrate Z, Korc M, et al. Diabetes mellitus and obesity as risk factors for pancreatic cancer. J Acad Nutr Diet. 2018;118(4):555–567. doi:10.1016/j.jand.2017.07.005
30. Bray GA, Heisel WE, Afshin A, et al. The science of obesity management: an endocrine society scientific statement. Endocr Rev. 2018;39(2):79–132.
31. Vigneri P, Frasca F, Sciacca L, et al. Diabetes and cancer. Endocr Relat Cancer. 2009;16(4):1103–1123. doi:10.1677/ERC-09-0087
32. Gallo M, Adinolfi V, Barucca V, et al. Expected and paradoxical effects of obesity on cancer treatment response. Rev Endocr Metab Disord. 2020. doi:10.1007/s11154-020-09597-y
33. Shlomai G, Neel B, LeRoith D, et al. Type 2 diabetes mellitus and cancer: the role of pharmacotherapy. J Clin Oncol. 2016;34(35):4261–4269. doi:10.1200/JCO.2016.67.4044
34. Edward G, David M, Michael C, et al. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33(7):1674–1685. doi:10.2337/dc10-0666
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

