Back to Journals » Psychology Research and Behavior Management » Volume 16
Pre- and Post-Pandemic (COVID-19) Mental Health of International Students: Data from a Longitudinal Study
Authors Jamshaid S , Bahadar N , Jamshed K , Rashid M, Imran Afzal M, Tian L, Umar M, Feng X, Khan I , Zong M
Received 4 November 2022
Accepted for publication 23 January 2023
Published 15 February 2023 Volume 2023:16 Pages 431—446
DOI https://doi.org/10.2147/PRBM.S395035
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Samrah Jamshaid,1,2 Noor Bahadar,3 Kamran Jamshed,4 Misbah Rashid,5 Muhammad Imran Afzal,2 Lv Tian,1 Muhammad Umar,6 Xuechao Feng,7 Imtiaz Khan,8 Minru Zong1
1Department of Rehabilitation, China-Japan Union Hospital of Jilin University, Changchun, Jilin, People’s Republic of China; 2School of Psychology, Northeast Normal University, Changchun, Jilin, People’s Republic of China; 3Department of Transgenic Animals, Changchun WISH Testing Technology & Service Co, Ltd, Building E11, Beihu Science Park B, Changchun, Jilin, People’s Republic of China; 4Business School, Bahria University Islamabad, Islamabad, Pakistan; 5Department of Psychology, Institute of Southern Punjab, Multan, Pakistan; 6Department of Orthopaedics, Shenzhen University General Hospital, Shenzhen, People’s Republic of China; 7Key Laboratory of Molecular Epigenetics, Institute of Genetics and Cytology, Northeast Normal University, Changchun, Jilin, People’s Republic of China; 8Department of Weed Science and Botany, The University of Agriculture Peshawar, Peshawar, KPK, Pakistan
Correspondence: Minru Zong, Department of Rehabilitation, China-Japan Union Hospital of Jilin University, No. 126 Xiantai Street, Changchun, Jilin, 130033, People’s Republic of China, Email [email protected]
Purpose: International students are highly vulnerable to the risk of mental health worsening before and during the pandemic (COVID-19). This study investigated international students’ mental health pre- and post-pandemic (COVID-19).
Methods: It is a longitudinal study, and data were collected online, pre-pandemic (N = 470) and during the pandemic (N = 420). Using a random sampling technique, a self-administered questionnaire was used to measure mental health, including depression and anxiety.
Results: Findings show that international students’ mental health was good in pre-pandemic. Meanwhile, international students were found to be more depressed and anxious during the pandemic. Findings also investigated that in the pre-pandemic phase, young students’ and mainly females’ mental health was worsened.
Conclusion: This study concluded that students’ mental problems are alarming, so the university should provide psychological services for the student’s mental health. Post-pandemic is leaving long-lasting psychological effects and will require further investigation.
Keywords: Covid-19, anxiety, depression, international students, mental health
Introduction
Mental health refers to the state of our mental well-being which helps us to cope with life stressors, to learn and work well, and to contribute to our community.1 Mental health plays a crucial role in our sustainable development. In recent years, much attention has been paid to mental health as it increases the acknowledgment of it in achieving the sustainable global development goals.2 Similarly, a new study has explored that from 2019 to 2021, a significant increase in internet searches for mental health assistance was observed. More than 5.4 million persons completed a mental health test in 2021, an increase of 103% over 2020 and a roughly 500% increase over the number of participants in 2019. More young people are seeking online support as they struggle with their mental health.3
When the Wuhan Municipal Health Commission in China reported a cluster of pneumonia cases on December 31, 2019, the COVID-19 pandemic began gradually.4 The number of cases had risen to almost 9800 globally in less than a month, with more than 200 deaths, forcing the World Health Organization (WHO) to declare a global health emergency. COVID-19 was declared a pandemic by the World Health Organization on March 11, 2020.5 Similar to many RNA-based viruses, SARS-CoV-2 can also exhibit rapid evolution, which results in the development of such mutations that may altogether be different from the original virus. During this Pandemic, the SARS-CoV-2 virus has also shown a few other mutations, although WHO has been active in distinguishing the most threatening variant as a Variant of Concern (VOC). As per the latest update by WHO, five variants of SARS-CoV-2 have been successfully identified as of 11th December 2021.
The COVID-19 pandemic, one of the worst worldwide epidemics in decades, has had significant but far effects on health systems, economics, and civilizations. On 30th January 2020, WHO declared SARS-CoV-2 (COVID) as a global pandemic severely affecting the global population. This Pandemic has cost countless people their health, hundreds of thousands of people their lives, and billions of dollars to the people around the world.6 This Pandemic has severely affected people’s social lives and damaged the global economy. Numerous people have died or lost their jobs. Communities and families have become strained and broken. Young people have been denied the opportunity to learn and interact with others. Companies have filed for bankruptcy. Millions of individuals are now living in poverty.7 The mental health of people has been significantly impacted as a result of these health, social, and economic effects. Many of us experienced increased anxiety, but for some COVID-19 has precipitated or worsened much more severe mental health issues.8 Many individuals have reported psychological suffering as well as signs of post-traumatic stress disorder, anxiety, or depression.4 Some group of people have been impacted significantly more than others, Pandemic affected tourism industry,9 health worker,10 and economy.11
In Pre-pandemic, every industry in the globe is seeing the effects of the COVID-19 pandemic.12,13 In an effort to combat this invisible virus, the majority of social and economic activities—including those at gyms, museums, theaters, swimming pools, and locations with huge gatherings—were shut down.14 This has a significant negative impact on both the global and education sectors.15 It has imposed a global lockdown, having a highly negative impact on students’ lives, pandemic also affected educational institutes.12 Educational sectors decide to change the whole education to online system.16 Young people have been left exposed to social isolation and disconnection as a result of prolonged school and university closures.17,18 These conditions can increase experiences of anxiety, fear, and depression and result in emotional and behavioral issues.19 Since the pandemic began, students also have faced issues, mostly changing their schedules and lifestyles to adapt to their new environment. Such changes, alongside the restrictions different governments put up on their masses, have led to degrading mental health for many University students.20–27 To combat this, physical activities have been a proven strategy for dealing with degrading psychological and physical health.27,28 This makes it all the more worrying that the pandemic and its restrictions have altogether reduced the reported physical activities of many university students reported in the early months of the Pandemic.27,29–33 As expected, those reporting lesser physical activities during the pandemic also reported poorer mental health.30,34,35 While those exhibiting more physical activities reported better mental health.23,36,37 All in all, the studies point towards a decrease in overall physical activities students participate in and an increase in their mental health issues. Focusing on more physical activities has been recommended as an effective counter measure.
In Post pandemic situation, lockdowns have worsened problems like loneliness, stress, anxiety, and alcohol misuse, particularly in vulnerable populations, because of the isolation they cause, the lack of one-on-one interaction, and the feelings of isolation on major life events.7 This is not surprising, of course, as the majority of health and care systems are still entirely focused on attempting to control waves of COVID-19 infections and all the simultaneous care and hospitalizations that occur. This does not, however, excuse the failure to act quickly to prevent a growing crisis.38 COVID has also created circumstances that might worsen mental health problems, such as prolonged periods of isolation and feeling lonely. Many people were obliged to postpone or delay necessary medical visits as a result of stricter regulations and overburdened health-care systems.7,39
Several studies investigated that during pandemic, the international students were more vulnerable to psychological issues such as loneliness, anxiety, stress, depressive symptoms and post stress traumatic disorder.40–42 It was found that the international students were more vulnerable than the domestic students,43–45 because most of the students were living on campus and had to stop their all social activities. Flights were not resumed so they were not able to go back their countries, so these all factors impacted that quality of life and well-being.46
The global research regarding the psychological effects on the populous of this pandemic and the lockdown has been limited in both number and quality, mostly due to targeted sampling, improper medical sampling techniques, and lack of pre-pandemic data to compare the results against. A study showed that mental stress has increased in the US since 2018, especially in young adults (18–24 years of age).47
Similarly, some studies demonstrated that students are disturbed by pandemic as it affects their normal health. Students suffer more than the general population from insomnia, depression and stress, an average rate of 30% of depression was found in students.45 There is little evidence that throughout the early stages of the pandemic, students were adapting fairly well. According to findings from an ecological momentary assessment (EMA) study conducted in March 2020, no changes in the outcomes of mental health were noticed over a period of two weeks.48
Some of the more noticeable effects of the pandemic include its financial pressure (employment restrictions with the increased cost of living), domestic situations (students forced to live alone or people living with a young child not going to school)49 or having previously existing psychological or physical health complications. A more specific effect of the pandemic might be on those working in critical jobs (food, health) exposed to the virus.50
Higher secondary and post students are at the most risk of developing mental illnesses during COVID as their educational institutions close, their academic routine is disturbed, and the lockdown imposes new social restrictions. Many studies on post-secondary students mental health during COVID show an incredibly varied result, with clinical diagnoses of depression to have increased by anywhere from 1.3% to 100% while anxiety grew to about 1.3% to 100%.51,52 Getting more precise data on the pandemic’s effects on these young adults’ mental health is important in establishing proper coping measures. For this purpose, a meta-analysis of all the available data was conducted. Alongside this, a demographic and methodological study quality moderator analysis was conducted to see what affects the mental health of these young adults and who the ones most vulnerable to depression and anxiety are. Such studies may prove resourceful in guiding future health policymakers and may help future research on the topic.
The most common psychological issues are depression and anxiety, making up a significant portion of the world’s mental illness burden.53 Depression may be defined as a lack of motivation or happiness while feeling overwhelmed with sadness and ineptness. Depression has been shown to have physical effects on the body, including lack of appetite, insomnia, and ADHD.
Anxiety may be defined as unnecessary uneasiness, worrying, or crippling fear. A meta-analysis conducted before the pandemic showed that China and other relatively poorer countries face around 24% depression rates in their students.54,55 Furthermore, anxiety was found in one-third of the global university population.56 For Iran, the meta-analysis showed that 33% of the university population showed signs of anxiety.57 Another study in Canada regarding the mental health of university students in one year found 14.7% of them to report depression while 18.4% reported anxiety.58
Mental illnesses showing additional prominence in different academic levels can be caused by something unique to those levels, factors which the Pandemic may worsen. For instance, Undergraduates are at that point in their lives where they are forced to become more and more independent, while these years also coincide with the advent of many psychological issues.59 For graduates, most of their daily schedules are filled with either academic activities or part-time jobs limiting the time they have to spend on recreation or other protective actions.60
One source of the wide range of results regarding mental health during the pandemic may be the methodology used. For instance, with the advent of the pandemic, there was a rise in the desire to learn about the pandemic’s mental impact, which may have led to the more sloppy methodology utilized to obtain quicker results.61 The difference in cultures between countries is also attributed to the difference in mental illnesses in the population.
With the advent of the Pandemic and the global lockdown, many mental risks have arisen due to the situation, including the fear of death and disease, isolation, and financial insecurity. Furthermore, studies have been conducted to observe the impacts of the pandemic on the mental health of the masses, including emotional stability, substance use, and dietary disorders.62–64 For instance, Australians reported worse dietary self-control during the pandemic than before.65 Poland reported increased alcohol consumption.66 Furthermore, two studies conducted in the US showed more significant mental stress in the populous during the pandemic than before.8,67 As such, preliminary data points toward the Pandemic producing mental health problems for the general masses.
The Pandemic also impacted the psychological well-being of the college population. In the US, the students absconded from their colleges during the pandemic, disturbing their academics and public lives. This disturbance is of more significant concern for them due to the mentally vulnerable period of their lives. For instance, a study before the pandemic already reported an all-time high rate of reported mental issues for the past year in college students (31.1%)68 while the rate of stress, depression, anxiety, and suicidal thoughts to have constantly been increasing since 2010.69
Additionally, young adults develop three-quarters of the mental illnesses they would develop throughout their lives.53 As such, students in college are at the most vulnerable period of their mental health during the pandemic. Studies show young adults in college to have been adversely mentally impacted by the pandemic. Italy showed younger adults to report more significant anxiety and stress levels than older ones, ie, above fifty.70 Likewise, China reported college-going young adults experiencing greater anxiety than non-students of similar age.59 But, this data does not help much, mostly because of the lack of comparable data before the pandemic, due to which it cannot be said if the pandemic is to blame or if these mental issues develop due to some pre-existing factor. Proper research would have been one where the sample sizes were considerably large, and two groups were picked from immediately before the pandemic and during the pandemic and then comparing the mental health conditions of the two.71
A Greece study adopted the condition mentioned earlier and found suicidal thoughts and depression to have increased since 2012.72 However, it cannot be said whether it is due to the pandemic, or the general trend of declining mental health observed throughout the decade.49Another study in the US found alcohol consumption to have gone up in students in March 2020. However, the changes in the mental states of the students were not documented.73 As above literature state that in pre pandemic situation when world activities became online and it affects the mental health of general population and students as well. The uniqueness of the study is to explore the student’s mental health in new normal life (post-pandemic) and to compare it with pre-pandemic mental health. It was hypothesized that there will be significant differences in pre and post pandemic mental health among international students.
Materials and Methods
Research Design
It was a longitudinal study designed to investigate the pre-pandemic and post-pandemic mental health of international students in China. Data was collected online in two phases and is still ongoing. Pre-pandemic data was collected from 2019 to 2020, and post-pandemic data was collected till November 2021. A self-administered questionnaire was used to measure mental health, including depression and anxiety, via a random sampling technique.
Participants
The study was approved by the “Ethics Committee of Northeast Normal University, 20,220,621,154” and the study followed the Declaration of Helsinki. Participation in the study was voluntary, and the participants had the choice to accept, reject the participation, or withdraw at any time. Informed consent was provided to each participant and was informed about the purpose of the study. The participants agreed to get published the information for research purposes. Data was collected online from international students studying in China through Meta, Email, and WeChat. A flowchart of the students’ participation is shown in Figure 1. The study was based on two phases, ie, pre-pandemic (N = 470) and post-pandemic (N = 420). A total of 745 participants were invited to participate in this study; 120 did not complete the consent, so their responses were discarded. Fifty-eight participants did not complete the questionnaire, and missing data were found among 97 responses, so they were also discarded. Four hundred seventy participants’ responses were used for the pre-pandemic study. Twenty participants were not available again, so 450 participants were approached again for a post-pandemic survey in which 29 participants did not match previous measures, so they were discarded. Twenty-one participants refused to participate, so in the last only 420 participants’ responses were used for data analysis. In the pre-pandemic study, males (57.2%) students were more than females (42.8%), and most of them were young adults age range from 20 to 30 years old (70.4%). Most students were single (76.6%) and from Asian (69.1%) countries. 73.4% of students were urban and belonged to the middle class (81.1%). Moreover, in the post-pandemic study, males (57.6%) students were also more than females (42.4%), and most of them were young adults age range from 20 to 30 years old (70.7%). Most students were single (73.3%) and from Asian (69.5%) countries. 75.2% of students were urban and belonged to the middle class (81.7%).
 |
Figure 1 The flowchart of the study. Here, we have shown the design of the study, participants and exclusion of the students. |
Procedure
The department review board approved this study of all author’s universities. The web-based survey was made via Google doc and the link was shared through Meta, Email, and WeChat to international students in China. Population sample of the study was international students in China, so original scales based on English language were used in this study. The authors shared survey links to 745 participants for screening, and 470 true responses were screened in the pre-pandemic study from December 2019 to April 2020. For the post-pandemic study, data were collected again from 430 participants from October to December 2021. Participants were approached again by their web addresses and requested to take part again. The survey took only 5 to 10 minutes to read and mark their responses. After the screening, 420 true responses were selected for data analysis. Ethical guidelines were strictly followed to maintain the confidentiality of participants’ responses.
Measures
The Warwick Edinburgh Mental Wellbeing Scale
The mental health of international students was measured with the Warwick Edinburgh mental well-being scale, which is designed to measure the mental well-being of the general population. The mental well-being scale focuses on the positive characteristics of individual mental health to improve mental health. Positive mental health is individuals with significant values of social consequences and health.74 This scale was developed by Tennant et al,75 based on 14 items. This scale has five categories of response from 1 = none of the time to 5 = all of the time. All items of scales worded positive and measure the functioning and feeling aspects about mental health. Sample of item is, ie, I have been optimistic about the future. Alpha reliability for this scale was 0.67. A high score on scale shows good mental health, and a low score predicts poor mental health.
Depression Anxiety Stress Scale (DASS)
To measure the depression and anxiety of international students, the depression anxiety stress scale was adopted from DASS. This scale is developed by Lovibond and Lovibond in 1995,76 based on 21 items. Every seven items measure different aspects, ie, depression, anxiety, and stress. This study intended to investigate depression and anxiety, so only 14 items were adopted. This scale was based on 4 responses from 0 = did not apply to me at all to 3 = applied to me very much. The sample item of the scale is, ie, I could not seem to experience any positive feeling at all. The alpha reliability of this scale was 0.70 for depression and 0.67 for anxiety.
Analytic procedures
Different analytic procedures were applied to investigate the study hypothesis. IBM SPSS (statistical packages for social sciences) 23rd version was used for data analysis. Descriptive analysis was used to explore demographic differences (Gender, Age, Nationality, Marital status, Residence, social-economic status, etc.) for pre-pandemic and post-pandemic cohorts. For the main analysis of the study, Paired sample t-test, Multivariate analysis was used to investigate the difference in change for pre-pandemic and post-pandemic Cohort mental health.
Results
Table 1 shows the frequency and percentage of students with pre and post-pandemic mental health. In the pre-pandemic study, males (57.2%) students were more than females (42.8%), and most of them were young adults age range from 20 to 30 years old (70.4%). Most students were single (76.6%) and from Asian (69.1%) countries. 73.4% of students were urban and belonged to the middle class (81.1%). Moreover, in the post-pandemic study, males (57.6%) students were also more than females (42.4%), and most of them were young adults age range from 20 to 30 years old (70.7%). Most students were single (73.3%) and from Asian (69.5%) countries. 75.2% of students were urban and belonged to the middle class (81.7%).
 |
Table 1 Demographic Characteristics of the Participants |
Above table (see Table 2) shows that there was significant difference for pre-pandemic mental health (M = 51.41, SD = 6.93) and post-pandemic mental health (M = 33.21, SD = 3.22); t (419) = 48.78, p = 0.000. Above table shows that there was significant difference for pre-pandemic depression (M = 14.07, SD = 2.74) and post-pandemic depression (M = 14.65, SD = 4.07); t (419) = −5.39, p = 0.000, also see Figure 2. Above table shows that there was significant difference for pre-pandemic anxiety (M = 16.96, SD = 4.02) and post-pandemic mental anxiety (M = 19.46, SD = 5.91); t (419) = −16.79, p = 0.000.
 |
Table 2 Comparison Between Pre and Post Pandemic Mental Health, Depression and Anxiety by Pair Sample t-test |
 |
Figure 2 Mean differences for Pre- and post-pandemic mental health, depression, and anxiety. |
There was a significant difference (see Table 3) between male and females when considered them jointly on the variable’s pre-pandemic mental health, depression and anxiety, wilk’s Λ = 0.97, F (3466) = 3.77, p = 0.011, partial Ƞ2 = 0.02. A separate one-way ANOVA was conducted for each dependent variable, with each ANOVA evaluated at an alpha value of 0.05. There was significant difference between males and females on Anxiety, F (1468) = 9.59, p = 0.002, partialȠ2 = 0.02, with females (M = 17.63) scoring higher than males (M = 16.44). There were non-significant differences between male and females on Mental health, F (1468) = 0.35, p = 0.555, partialȠ2 = 0.00 and depression, F (1468) = 1.11, p = 0.293, partialȠ2 = 0.00 (see Figure 3). Furthermore, there was a significant difference between age groups when considered them jointly on the variable’s mental health, depression and anxiety, wilk’s Λ = 0.97, F (3466) = 4.37, p = 0.005, partial Ƞ2 = 0.03. A separate one-way ANOVA was conducted for each dependent variable, there was significant difference between age groups on depression, F (1468) = 6.79, p = 0.009, partialȠ2 = 0.01, with age of 20 to 30 years (M = 14.24) scoring higher than those whose ages were 31 to 40 years (M = 13.50). There were also significant differences between age groups on Anxiety, F (1468) = 9.98, p = 0.002, partialȠ2 = 0.02, with age of 20 to 30 years (M = 17.33) scoring higher than those whose ages were 31 to 40 years (M = 16.02). However, there was non-significant difference found on mental health, F (1468) = 2.56, p = 0.110, partialȠ2 = 0.00 (see Figure 4).
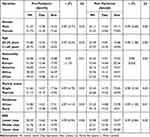 |
Table 3 Mean Differences of Pre-Pandemic and Post-Pandemic Mental Health, Depression, and Anxiety by Demographic Characteristics by MANOVA |
 |
Figure 3 Pre-pandemic (2019–2020) and post-pandemic (2021) mental health for the Gender. Abbreviations: Pre-Mh, pre-pandemic mental health; Dep, depression; Anx, anxiety; Post, post-pandemic. |
 |
Figure 4 Pre-pandemic (2019–2020) and post-pandemic (2021) mental health for age group. Abbreviations: Pre-Mh, pre-pandemic mental health; Dep, depression; Anx, anxiety; Post, post-pandemic. |
Results demonstrated that there is a significant difference between single and married students when considering them jointly on the variable’s mental health, depression, and anxiety, Wilk’s Λ = 0.97, F (3466) = 4.70, p = 0.003, partial Ƞ2 = 0.03. A separate one-way ANOVA was conducted for each dependent variable, there was significant difference between single and married on depression, F (1468) = 12.88, p = 0.000, partialȠ2 = 0.03, with single students (M = 14.27) scoring higher than married students (M = 13.19). There was also significant difference between single and married on anxiety, F (1468) = 8.96, p = 0.003, partialȠ2 = 0.02, with single students (M = 17.26) scoring higher than married students (M = 15.92). There was a non-significant difference between single and married students in mental health. There was a significant difference between urban and rural residence students when considering them jointly on the variable’s mental health, depression, and anxiety, Wilk’s Λ = 0.97, F (3466) = 4.14, p = 0.006, partial Ƞ2 = 0.03. A separate one-way ANOVA was conducted for each dependent variable, there was significant difference between urban and rural students on depression, F (1468) = 6.21, p = 0.013, partialȠ2 = 0.01, with urban students (M = 14.21) scoring higher than rural students (M = 13.48). There was also significant difference urban and rural on anxiety, F (1468) = 9.54, p = 0.002, partialȠ2 = 0.02, with urban students (M = 17.31) scoring higher than rural students (M = 15.95). There was a non-significant difference between urban and rural students in mental health. There was a non-significant difference between the lower, middle, and upper social class of students when considering them jointly on the variable’s mental health, depression, and anxiety, Wilk’s Λ = 0.99 F (3466) = 0.94, p = 0.465, partial Ƞ2 = 0.00. A separate one-way ANOVA was conducted for each dependent variable, there was also a non-significant difference between lower, middle, and upper social classes on mental health, depression, and anxiety.
Results also explored the differences in international students’ post-pandemic mental health, depression, and anxiety. There was a non-significant difference between males and females when considering them jointly on the variable’s mental health, depression, and anxiety, Wilk’s Λ = 0.99 F (3466) = 69, p = 0.559, partial Ƞ2 = 0.00. A separate one-way ANOVA was conducted for each dependent variable, there was also a non-significant difference between males and females in mental health, depression, and anxiety (see Figure 3). There was a non-significant difference between age groups when considered them jointly on the variable’s mental health, depression and anxiety, Wilk’s Λ = 0.99 F (3466) = 1.08, p = 0.355, partial Ƞ2 = 0.00. A separate one-way ANOVA was conducted for each dependent variable, there was also a non-significant difference between the age of 20–30- and 31–40-years age on mental health, depression, and anxiety (see Figure 4). There was also non-significant difference between student’s nationalities when considered them jointly on the variable’s mental health, depression and anxiety, Wilk’s Λ = 0.98 F (3466) = 0.63, p = 0.815, partial Ƞ2 = 0.00. A separate ANOVA was conducted for each dependent variable, there was also a non-significant difference between nationalities on mental health, depression, and anxiety (see Figure 5). There was a significant difference between single and married students when considering them jointly on the variable’s mental health, depression, and anxiety, Wilk’s Λ = 0.98, F (3466) = 2.34, p = 0.073, partial Ƞ2 = 0.02. A separate ANOVA was conducted for each dependent variable, with each ANOVA evaluated at an alpha value of 0.05. There was significant difference between single and married students on mental health, F (1468) = 4.72, p = 0.030, partialȠ2 = 0.01, with single (M = 33.40) scoring higher than married (M = 32.66). There were non-significant differences between single and married on depression and anxiety.
There was a significant difference between urban and rural residence-based students when considering them jointly on the variable’s mental health, depression, and anxiety, Wilk’s Λ = 0.99, F (3466) = 1.30, p = 0.273, partial Ƞ2 = 0.01. A separate one-way ANOVA was conducted for each dependent variable, with each ANOVA evaluated at an alpha value of 0.05. There was partial significant difference between urban and rural on anxiety, F (1468) = 3.62, p = 0.058, partialȠ2 = 0.01, with urban (M = 19.78) scoring higher than rural (M = 18.51). There were non-significant differences between urban and rural residence-based students on depression and mental health. There was also non-significant difference between student’s social-economic status when considered them jointly on the variable’s mental health, depression and anxiety, Wilk’s Λ = 0.99 F (3466) = 0.84, p = 0.540, partial Ƞ2 = 0.00. A separate one-way ANOVA was conducted for each dependent variable, there was also a non-significant difference between lower, middle, and upper social classes on mental health, depression, and anxiety.
Discussion
The study was devised to investigate the change in students’ mental health before and during COVID −19 pandemic in China. For this purpose, a longitudinal design was carried out online in two phases to investigate students’ mental health in China. The two distinct phases are pre-pandemic (2019–2020) and post-pandemic (till 2021) situations. This study has investigated the differences for pre-pandemic and post-pandemic mental health, depression, and anxiety. Paired sample t-test has been utilized to explore the student’s pre-pandemic and post-pandemic mental health. Furthermore, demographic differences (gender, age, nationality, marital status, residence, and social-economic status) for the pre-pandemic and post-pandemic cohort were measured. Two core domains of mental health, anxiety, and depression were aligned with mental health to assess overall mental health. One-way multivariate analysis of variance (MANOVA) was carried out to investigate the significant difference in mental health, anxiety, and depression among students during pre-pandemic and post-pandemic situations.
The paired sample t-test indicates that international students’ mental health was good in the pre-pandemic phase compared to their mental health in the post-pandemic phase. The finding is supported by a previous study that people suffer from insomnia, emotional disturbance, depression, irritability, and posttraumatic stress in the post-pandemic phase. The pandemic has caused long-term effects by causing anger, stress, depression, alcohol abuse, anxiety, and change in their behaviors. These emotional and physical disturbances are causing them to wash their hands repeatedly and avoid crowded places. However, it has been concluded that these symptoms or issues can last long, and it may take years to recover after the quarantine period.77
Another study also supports this finding, and this can also be because of the isolation effect. This study concluded that long isolation leads people to withdraw from society and could cause various social and economic crises during the pandemic. People are also afraid to go outside and might be infected by COVID-19. The government also suggests nations stay away and safe, and it causes fears of contagion virus.78 A recent study similarly investigated that mental health plays a very important role during and after this pandemic. Still, it is generating different stigmas related to it and causing severe psychological issues such as suicide and psychosis can be expected to happen in this post-pandemic time.38
In Germany, students are facing academic, emotional and financial challenges during this pandemic and it is affecting their mental health. These challenges now become the source of poor mental health. Due to pandemic all activities become online, like meeting with the friends through social application and also learning through online channels. Some students found other methods to avoid it by suspended their studies, taking a gap for one or two years and tried to enhance their social circle for good mental health. Now in 2022 many students are back to their campus but they are still stressed, depressed and anxious with campus life for post pandemic.79 Psychological discomfort among college students has reportedly grown in the United States, according to polls of students taken after March 2020. The impact of COVID-19 on college students’ mental health is much more complex than widely reported, according to CCMH evidence, which represents approximately 50,000 treatment-seeking students at 140 plus schools.80 Another study found that throughout pandemic with virtual connection and offline study, student were less likely to have poor mental health, persistent depressive or hopeless sentiments, and suicidal thoughts and behaviors.81
The result of MANOVA shows a statistically significant difference between pre and post-pandemic groups of students on the mental health scale, pointing to better scores on mental health in the pre-pandemic group compared to the post-pandemic group.
Significant differences concerning gender (male and female) of respondents were found in study outcomes on mental health, depression, and anxiety in the pre-pandemic study. The effect size is significant for both studies; still, in the post-pandemic study, the effect size was 99%. Based on the results, the COVID-19 situation has placed equal stress on students’ mental health and contributes equally to their depression and anxiety regardless of their gender. Scores of separate ANOVA highlight that mental health in pre-pandemic situations is better than mental health during COVID-19 in students. Pandemics cause poor mental health by increasing global anxiety and depression among young adults. Previous research had found that anxiety and depression during the pandemic were higher among younger members, women, those with pre-existing mental/physical health issues, and those with socioeconomic difficulty, even when pre-pandemic anxiety and despair were controlled for.82–85
Likewise, substantial differences concerning age groups (20–30) and respondents were found in study outcomes on mental health, depression, and anxiety in the pre-pandemic situation, the differences were significant and showed that students aged 20 to 30 who were females were having high depression levels. The differences were substantial and showed that students between the age of 20 to 30 had high depression levels. The findings of the study are supported by previous literature that Female students are more likely than male students to be stressed and depressed as a result of the worry of losing their educational achievements due to school closures during the COVID-19 epidemic, as well as the concern of COVID-19 having a detrimental impact on their families’ or relatives’ well-being.85 This could be because females have stronger fear-related neural network reactivity and differential conditioned skin conductance responses to stimulations than males.86
The female gender was previously proven to be a predictor of the negative psychological impact of the COVID-19 pandemic, with females enduring a stronger psychological impact and higher levels of sadness, stress, and anxiety than males, according to a study. Other studies have revealed that females were more mentally sensitive than males during the COVID-19 outbreak.87–89 During the COVID-19 pandemic in China, Liu et al (2020) looked at the prevalence and determinants of post-traumatic stress symptoms.86 According to the findings, females had higher rates of post-traumatic stress symptoms in the areas of negative thinking or emotion, re-experiencing, and high energy.
The findings of the present study also revealed that single students had a high level of depression and anxiety compared to those who were married. Results vary before and during a pandemic; levels of depression and anxiety were low post-pandemic. Their depression and anxiety level were high, maybe because of their marital status. Married students have partner support, so that was easy for them to fight the Pandemic. The results of a previous study into the immediate mental health status of the Chinese workforce during the COVID-19 pandemic revealed that respondents who were divorced, kept separate, or recently divorced had a higher impact of event, stress, anxiety, and depression scores than those who were single, and married respondents had lower scores.90,91
These findings align with an Australian population-based survey, which found that more robust relationship quality is linked to fewer depression and anxiety symptoms than poor relationship quality.92 Furthermore, a lack of good social ties has been identified as a significant risk factor for severe depression. High marital quality, on the other hand, was linked to lower anxiety and depression.93 In a recent study published in Social Science Quarterly, researchers used statistics from the Survey of Census Household Pulse to find that married people consistently reported better mental health—specifically, fewer days of depression, anxiety, worry, and loss of interest in life—than unmarried people throughout the pandemic. Furthermore, mental health among married people did not suffer nearly as much as it did among unmarried people due to the labor market and job-prospect decline.94
Furthermore, the present study’s findings investigated that students who belong to urban areas have more depression and anxiety in pre and post-pandemic states. The previous study supports findings that students in the pandemic who belong to urban areas have more depression and anxiety than those who belong to rural areas.95 Rural populations are primarily farmers who live in larger areas, and their activities and mental health may be less impacted by social separation and quarantine procedures. Furthermore, residents in isolated rural areas received less information about the epidemic because of limited media sources, which may paradoxically reduce the negative impacts of perceived stress caused by the pandemic on mental health.96,97 The advent of the pandemic has brought a new wave of problems for university students. Dealing with the newfound forced independence this age brings, university life is already riddled with mental health vulnerabilities. This new pandemic, shutting down half of the world, produces a new set of worries for people worldwide. Even though the physical aspects of the disease are being studied, the mental strains for the lockdown and the fear of the virus have not been given the proper attention. This issue has caught the university students during a vulnerable time of their lives who may become unable to organize their lives around the situation.
Limitation and Recommendation
The strength of this study was the availability of pre-pandemic data for comparative analysis. Data collection was more convenient in post-pandemic (COVID-19) compared to pre-pandemic. Students were more afraid in the pre-pandemic stage, so their response rate was low. Meanwhile, approaching the same participants for post-study analysis was complex; maybe future research researchers should choose a convenient study design. Another limitation of the study was the short sample size, and the large sample can be better for a longitudinal study to make generalizable results. The focus of this study was the mental health of international students, there are many psychological factors to be focused study during the post-pandemic.
Conclusion
This study concluded that international students’ mental health worsened in the pre-pandemic, and international students were more depressed and anxious in the pre-pandemic phase. The study also concluded that mental health worsened in the pre-pandemic phase, among young students, mainly female international students. Students whose marital status was single and those who belonged to urban areas were at risk for poor mental health. Furthermore, the study concluded that students’ mental problems are alarming, so universities should provide psychological services for the mental health of the student population. There is a need to raise awareness about psychological issues during pandemics through multiple media platforms. Covid-19 affected the mental health of international students, so this study is helpful for them to take care of their mental health and come into normal lives by getting help from supportive people, with psychological counselling/guidance. They need supportive people who can listen to their problems and try to solve their issues. This study concluded that pre and post pandemic can cause poor mental health but good habit and living style can help to cope with this; regular exercise, enough sleep, eating properly, are some factors important for mental health.
Funding
This research is supported by the College-Enterprise Collaboration Project (2017YX244) and the Natural Science Foundation of Jilin Province (YDZJ202201ZYTS062, 20200201127JC). The funders have no role in the design of the study or analysis.
Disclosure
The authors declare no conflicts of interest in this study.
References
1. Health WHODoM, Abuse S, Organization WH. Mental Health Atlas 2005. World Health Organization; 2005.
2. Moeti M, Gao GF, Herrman H. Global pandemic perspectives: public health, mental health, and lessons for the future. Lancet. 2022. doi:10.1016/S0140-6736(22)01328-9
3. Mental Health America. Mental Health and Covid-19; 2022. Available from: https://mhanational.org/mental-health-and-covid-19-two-years-after-pandemic.
4. Kumar A, Singh R, Kaur J, et al. Wuhan to world: the COVID-19 pandemic. Front Cell Infect Microbiol. 2021;2021:242.
5. Lee A. Wuhan novel coronavirus (COVID-19): why global control is challenging? Public Health. 2020;179:A1. doi:10.1016/j.puhe.2020.02.001
6. Allocati N, Petrucci AG, Di Giovanni P, Masulli M, Di Ilio C, De Laurenzi V. Bat–man disease transmission: zoonotic pathogens from wildlife reservoirs to human populations. Cell Death Dis. 2016;2(1):1–8. doi:10.1038/cddiscovery.2016.48
7. health c. Post-pandemic mental health: what you need to know for 2023; 2023. Available from: https://collectivehealth.com/blog/insights/post-pandemic-mental-health/.
8. American Psychological Association. Stress in America™ 2020; Stress in the time of COVID-19, Volume one. Available from: https://www.apa.org/news/press/releases/stress/2020/report.
9. Yang Y, Zhang H, Chen X. Coronavirus pandemic and tourism: dynamic stochastic general equilibrium modeling of infectious disease outbreak. Ann Tour Res. 2020;83:102913. doi:10.1016/j.annals.2020.102913
10. Baskin RG, Bartlett R. Healthcare worker resilience during the COVID‐19 pandemic: an integrative review. J Nurs Manag. 2021;29(8):2329–2342. doi:10.1111/jonm.13395
11. Abodunrin O, Oloye G, Adesola B. Coronavirus pandemic and its implication on global economy. Int J Arts Lag Ling Lit stud. 2020;2020:4.
12. Kedraka K, Kaltsidis C. Effects of the Covid-19 pandemic on university pedagogy: students’experiences and considerations. Euro J Educ Stud. 2020;7:8. doi:10.46827/ejes.v7i8.3176
13. Jena PK. Impact of pandemic COVID-19 on education in India. IJCR. 2020;12:5.
14. Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020;12(4). doi:10.7759/cureus.7541
15. Tarkar P. Impact of COVID-19 pandemic on education system. Int J Adv Sci Tech. 2020;29(9):3812–3814.
16. Irawan AW, Dwisona D, Lestari M. Psychological impacts of students on online learning during the pandemic COVID-19. KONSELI. 2020;7(1):53–60. doi:10.24042/kons.v7i1.6389
17. Magson NR, Freeman JY, Rapee RM, Richardson CE, Oar EL, Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50(1):44–57. doi:10.1007/s10964-020-01332-9
18. Okruszek L, Aniszewska-Stańczuk A, Piejka A, Wiśniewska M, Żurek K. Safe but lonely? Loneliness, mental health symptoms and COVID-19; 2020.
19. Groarke JM, Berry E, Graham-Wisener L, McKenna-Plumley PE, McGlinchey E, Armour C. Loneliness in the UK during the COVID-19 pandemic: cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS One. 2020;15(9):e0239698. doi:10.1371/journal.pone.0239698
20. Ahmad FB, Cisewski JA, Miniño A, Anderson RN. Provisional mortality data—United States, 2020; 2022.
21. Copeland WE, McGinnis E, Bai Y, et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. 2021;60(1):134–141. e2. doi:10.1016/j.jaac.2020.08.466
22. Elmer T, Mepham K, Stadtfeld C. Students under lockdown: comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One. 2020;15(7):e0236337. doi:10.1371/journal.pone.0236337
23. Gallego-Gómez JI, Campillo-Cano M, Carrión-Martínez A, et al. The COVID-19 pandemic and its impact on homebound nursing students. Int J Environ Res Public Health. 2020;17(20):7383. doi:10.3390/ijerph17207383
24. Li HY, Cao H, Leung DY, Mak YW. The psychological impacts of a COVID-19 outbreak on college students in China: a longitudinal study. Int J Environ Res Public Health. 2020;17(11):3933. doi:10.3390/ijerph17113933
25. Li Y, Zhao J, Ma Z, et al. Mental health among college students during the COVID-19 pandemic in China: a 2-wave longitudinal survey. J Affect Disord. 2021;281:597–604. doi:10.1016/j.jad.2020.11.109
26. Saraswathi I, Saikarthik J, Kumar KS, Srinivasan KM, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020;8:e10164. doi:10.7717/peerj.10164
27. Savage MJ, James R, Magistro D, et al. Mental health and movement behaviour during the COVID-19 pandemic in UK university students: prospective cohort study. Ment Health Phys Act. 2020;19:100357. doi:10.1016/j.mhpa.2020.100357
28. Schuch FB, Vancampfort D, Firth J, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175(7):631–648. doi:10.1176/appi.ajp.2018.17111194
29. Barkley JE, Lepp A, Glickman E, et al. The acute effects of the COVID-19 pandemic on physical activity and sedentary behavior in university students and employees. Int J Exerc Sci. 2020;13(5):1326.
30. Coughenour C, Gakh M, Pharr JR, Bungum T, Jalene S. Changes in depression and physical activity among college students on a diverse campus after a COVID-19 stay-at-home order. J Community Health. 2021;46(4):758–766. doi:10.1007/s10900-020-00918-5
31. Gallè F, Sabella EA, Ferracuti S, et al. Sedentary behaviors and physical activity of Italian undergraduate students during lockdown at the time of COVID− 19 pandemic. Int J Environ Res Public Health. 2020;17(17):6171. doi:10.3390/ijerph17176171
32. Gallo LA, Gallo TF, Young SL, Moritz KM, Akison LK. The impact of isolation measures due to COVID-19 on energy intake and physical activity levels in Australian university students. Nutrients. 2020;12(6):1865. doi:10.3390/nu12061865
33. Luciano F, Cenacchi V, Vegro V, Pavei G. COVID-19 lockdown: physical activity, sedentary behaviour and sleep in Italian medicine students. Eur J Sport Sci. 2021;21(10):1459–1468. doi:10.1080/17461391.2020.1842910
34. Lin J, Guo T, Becker B, et al. Depression is associated with moderate-intensity physical activity among college students during the COVID-19 pandemic: differs by activity level, gender and gender role. Psychol Res Behav Manag. 2020;13:1123. doi:10.2147/PRBM.S277435
35. Maher JP, Hevel DJ, Reifsteck EJ, Drollette ES. Physical activity is positively associated with college students’ positive affect regardless of stressful life events during the COVID-19 pandemic. Psychol Sport Exerc. 2021;52:101826. doi:10.1016/j.psychsport.2020.101826
36. Xiang M-Q, Tan X-M, Sun J, et al. Relationship of physical activity with anxiety and depression symptoms in Chinese college students during the COVID-19 outbreak. Front Psychol. 2020;11:582436. doi:10.3389/fpsyg.2020.582436
37. Zhang Y, Zhang H, Ma X, Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int J Environ Res Public Health. 2020;17(10):3722. doi:10.3390/ijerph17103722
38. Kathirvel N. Post COVID-19 pandemic mental health challenges. Asian J Psychiatr. 2020;53:102430. doi:10.1016/j.ajp.2020.102430
39. Khanna A, Jones GB. Envisioning post-pandemic digital neurological, psychiatric and mental health care. Front Digit Health. 2021;3. doi:10.3389/fdgth.2021.803315
40. Maleku A, Kim YK, Kirsch J, et al. The hidden minority: discrimination and mental health among international students in the US during the COVID‐19 pandemic. Health Soc Care Community. 2022;30(5):. doi:10.1111/hsc.13683
41. Labrague LJ, De Los Santos JAA, Falguera C. Social and emotional loneliness among college students during the COVID-19 pandemic: the predictive role of coping behaviours, social support, and personal resilience; 2021.
42. Manyeruke G, Ergün D. Mental health, loneliness and social support during covid-19 pandemic among International University Students in North Cyprus. Kibris Türk Psikiyatri ve Psikoloji Dergisi. 2022;4(3):211–221.
43. Girmay M, Singh GK. Social isolation, loneliness, and mental and emotional well-being among international students in the United States. IJTMRPH. 2019;3(2):75–82. doi:10.21106/ijtmrph.82
44. Dodd RH, Dadaczynski K, Okan O, McCaffery KJ, Pickles K. Psychological wellbeing and academic experience of university students in Australia during COVID-19. Int J Environ Res Public Health. 2021;18(3):866. doi:10.3390/ijerph18030866
45. Kivelä L, Mouthaan J, van der Does W, Antypa N. Student mental health during the COVID-19 pandemic: are international students more affected? J Am Coll Health. 2022;2022:1–9.
46. Antwi CO, Belle MA, Ntim SY, et al. COVID-19 pandemic and international students’ mental health in China: age, gender, chronic health condition and having infected relative as risk factors. Int J Environ Res Public Health. 2022;19(13):7916. doi:10.3390/ijerph19137916
47. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324(1):93–94. doi:10.1001/jama.2020.9740
48. Fried EI, Papanikolaou F, Epskamp S. Mental health and social contact during the COVID-19 pandemic: an ecological momentary assessment study. Clin Psychol Sci. 2022;10(2):340–354. doi:10.1177/21677026211017839
49. Sevilla A, Phimister A, Krutikova S, et al. How are mothers and fathers balancing work and family under lockdown?; 2020.
50. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368. doi:10.1136/bmj.m1211
51. Deng C-H, Wang J-Q, Zhu L-M, et al. Association of web-based physical education with mental health of college students in Wuhan during the COVID-19 outbreak: cross-sectional survey study. J Med Internet Res. 2020;22(10):e21301. doi:10.2196/21301
52. Vahedian-Azimi A, Moayed MS, Rahimibashar F, Shojaei S, Ashtari S, Pourhoseingholi MA. Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic. BMC Psychiatry. 2020;20(1):1–7. doi:10.1186/s12888-020-02804-9
53. Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi:10.1001/archpsyc.1994.03950010008002
54. Akhtar P, Ma L, Waqas A, et al. Prevalence of depression among university students in low and middle income countries (LMICs): a systematic review and meta-analysis. J Affect Disord. 2020;274:911–919. doi:10.1016/j.jad.2020.03.183
55. Lei X-Y, Xiao L-M, Liu Y-N, Li Y-M. Prevalence of depression among Chinese University students: a meta-analysis. PLoS One. 2016;11(4):e0153454. doi:10.1371/journal.pone.0153454
56. Hiramura H, Shono M, Tanaka N, Nagata T, Kitamura T. Prospective study on suicidal ideation among Japanese undergraduate students: correlation with stressful life events, depression, and depressogenic cognitive patterns. Arch Suicide Res. 2008;12(3):238–250. doi:10.1080/13811110802100924
57. Rahmani A, Sayehmiri K, Asadollahi K, Sarokhani D, Islami F, Sarokhani M. Investigation of the prevalence of obesity in Iran: a systematic review and meta-analysis study. Acta Medica Iranica. 2015;27:596–607.
58. Esmaeelzadeh S, Moraros J, Thorpe L, Bird Y. The association between depression, anxiety and substance use among Canadian post-secondary students. Neuropsychiatr Dis Treat. 2018;14:3241. doi:10.2147/NDT.S187419
59. Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–640. doi:10.1001/archpsyc.62.6.629
60. Wyatt T, Oswalt SB. Comparing mental health issues among undergraduate and graduate students. Am J Health Educ. 2013;44(2):96–107. doi:10.1080/19325037.2013.764248
61. Pierce M, McManus S, Jessop C, et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7(7):567–568. doi:10.1016/S2215-0366(20)30237-6
62. Unützer J, Kimmel RJ, Snowden M. Psychiatry in the age of COVID‐19. World Psychiatry. 2020;19(2):130. doi:10.1002/wps.20766
63. Clay JM, Parker MO. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Public Health. 2020;5(5):e259. doi:10.1016/S2468-2667(20)30088-8
64. Fernández‐Aranda F, Casas M, Claes L, et al. COVID‐19 and implications for eating disorders. Eur Eat Disord Rev. 2020;28(3):239. doi:10.1002/erv.2738
65. Phillipou A, Meyer D, Neill E, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: initial results from the COLLATE project. Int J Eat Dis. 2020;53(7):1158–1165. doi:10.1002/eat.23317
66. Sidor A, Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. 2020;12(6):1657. doi:10.3390/nu12061657
67. Twenge JM, Joiner TE. Mental distress among US adults during the COVID‐19 pandemic. J Clin Psychol. 2020;76(12):2170–2182. doi:10.1002/jclp.23064
68. Auerbach RP, Mortier P, Bruffaerts R, et al. WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623. doi:10.1037/abn0000362
69. Duffy ME, Twenge JM, Joiner TE. Trends in mood and anxiety symptoms and suicide-related outcomes among US undergraduates, 2007–2018: evidence from two national surveys. J Adolesc Health. 2019;65(5):590–598. doi:10.1016/j.jadohealth.2019.04.033
70. Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi:10.1016/j.sleep.2020.05.011
71. Busfield J. Challenging claims that mental illness has been increasing and mental well-being declining. Soc Sci Med. 2012;75(3):581–588. doi:10.1016/j.socscimed.2012.02.053
72. Kaparounaki CK, Patsali ME, Mousa D-PV, Papadopoulou EV, Papadopoulou KK, Fountoulakis KN. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020;290:113111. doi:10.1016/j.psychres.2020.113111
73. Lechner WV, Laurene KR, Patel S, Anderson M, Grega C, Kenne DR. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav. 2020;110:106527.
74. Linley PA, Joseph S. Applied positive psychology: a new perspective for professional practice. Posit Psychol Pract. 2004;2004:3–12.
75. Tennant R, Hiller L, Fishwick R, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. 2007;5. doi:10.1186/1477-7525-5-63
76. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343. doi:10.1016/0005-7967(94)00075-u
77. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/s0140-6736(20)30460-8
78. Kato TA, Sartorius N, Shinfuku N. Forced social isolation due to COVID-19 and consequent mental health problems: lessons from hikikomori. Psychiatry Clin Neurosci. 2020;74(9):506–507. doi:10.1111/pcn.13112
79. Kohls E, Baldofski S, Moeller R, Klemm S-L, Rummel-Kluge C. Mental health, social and emotional well-being, and perceived burdens of university students during COVID-19 pandemic lockdown in Germany. Front Psychiatry. 2021;12:643957. doi:10.3389/fpsyt.2021.643957
80. Minds A, Aida J, Osaka K, Rozier RG. COVID-19 impact on college student mental health. Int J Envir Res Public Health. 2020;17:2020. doi:10.3390/ijerph17062020
81. Jones SE, Ethier KA, Hertz M, et al. Mental health, suicidality, and connectedness among high school students during the COVID-19 pandemic—adolescent behaviors and experiences survey, United States, January–June 2021. MMWR Supplements. 2022;71(3):16. doi:10.15585/mmwr.su7103a3
82. Kwong AS, Pearson RM, Adams MJ, et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br J Psychiatry. 2021;218(6):334–343. doi:10.1192/bjp.2020.242
83. Ramiz L, Contrand B, Rojas Castro MY, et al. A longitudinal study of mental health before and during COVID-19 lockdown in the French population. Global Health. 2021;17(1):1–16. doi:10.1186/s12992-021-00682-8
84. Henry RS, Kwakkenbos L, Carrier M-E, et al. Mental health before and during the pandemic in people with systemic sclerosis. Lancet Rheumatol. 2022;4(2):e82–e85. doi:10.1016/S2665-9913(21)00363-5
85. Al Dhaheri AS, Bataineh M, Mohamad MN, et al. Impact of COVID-19 on mental health and quality of life: is there any effect? A cross-sectional study of the MENA region. PLoS One. 2021;16(3):e0249107. doi:10.1371/journal.pone.0249107
86. Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi:10.1016/j.psychres.2020.112921
87. Broche-Pérez Y, Fernández-Fleites Z, Jiménez-Puig E, Fernández-Castillo E, Rodríguez-Martin BC. Gender and fear of COVID-19 in a Cuban population sample. Int J Ment Health Addict. 2020;1–9. doi:10.1007/s11469-020-00377-y
88. Radwan E, Radwan A, Radwan W. The role of social media in spreading panic among primary and secondary school students during the COVID-19 pandemic: an online questionnaire study from the Gaza Strip, Palestine. Heliyon. 2020;6(12):e05807. doi:10.1016/j.heliyon.2020.e05807
89. Rossi R, Socci V, Talevi D, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry. 2020;11:790. doi:10.3389/fpsyt.2020.00790
90. Tan W, Hao F, McIntyre RS, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. doi:10.1016/j.bbi.2020.04.055
91. Nkire N, Nwachukwu I, Shalaby R, et al. COVID-19 pandemic: influence of relationship status on stress, anxiety, and depression in Canada. Ir J Psychol Med. 2021;39:1–12.
92. Leach LS, Butterworth P, Olesen SC, Mackinnon A. Relationship quality and levels of depression and anxiety in a large population-based survey. Soc Psychiatry Psychiatr Epidemiol. 2013;48(3):417–425. doi:10.1007/s00127-012-0559-9
93. Teo AR, Choi H, Valenstein M. Social relationships and depression: ten-year follow-up from a nationally representative study. PLoS One. 2013;8(4):e62396. doi:10.1371/journal.pone.0062396
94. Lafortune J, Low C. Collateralized Marriage. National Bureau of Economic Research; 2020.
95. Islam MA, Barna SD, Raihan H, Khan MNA, Hossain MT. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS One. 2020;15(8):e0238162. doi:10.1371/journal.pone.0238162
96. Liu L, Xue P, Li SX, Zhang J, Zhou J, Zhang W. Urban-rural disparities in mental health problems related to COVID-19 in China. Gen Hosp Psychiatry. 2021;69:119. doi:10.1016/j.genhosppsych.2020.07.011
97. Zhang J, Zhu L, Li S, et al. Rural–urban disparities in knowledge, behaviors, and mental health during COVID-19 pandemic: a community-based cross-sectional survey. Medicine. 2021;100:13.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.