Back to Journals » Cancer Management and Research » Volume 13
Practices and Hindrances in Cancer Pain Management: Results of a National Multi-Cancer Center Survey Among Healthcare Professionals in China
Authors Su C, Chen M, Chen G, Li Y, Li N , Hu Z, Hu X, Zhao Y , Yu Q , Jiang W
Received 4 November 2020
Accepted for publication 22 January 2021
Published 18 February 2021 Volume 2021:13 Pages 1709—1717
DOI https://doi.org/10.2147/CMAR.S290470
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eileen O'Reilly
Cuiyun Su,1,* Maojian Chen,1,* Guanxuan Chen,2,* Yajun Li,3 Ning Li,4 Zhihuang Hu,5 Xiao Hu,6,7 Yuanyuan Zhao,8– 10 Qitao Yu,1 Wei Jiang1
1Department of Respiratory Oncology, Guangxi Medical University Cancer Hospital, Nanning, Guangxi, 530021, People’s Republic of China; 2Department of Intensive Care Unit, Shandong Cancer Hospital Affiliated to Shandong University, Jinan, Shandong, 250117, People’s Republic of China; 3Department of Lymphoma and Hematology, Hunan Cancer Hospital & the Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University, Changsha, Hunan, 410013, People’s Republic of China; 4Department of Oncology, Henan Cancer Hospital & the Affiliated Cancer Hospital of Zhengzhou University, Zhengzhou, Henan, 450008, People’s Republic of China; 5Department of Medical Oncology, Fudan University Shanghai Cancer Center, Shanghai, 200032, People’s Republic of China; 6Department of Radiation Oncology, Cancer Hospital of the University of Chinese Academy of Sciences & Zhejiang Cancer Hospital, Hangzhou, Zhejiang, 310022, People’s Republic of China; 7Department of Radiation Oncology, Institute of Cancer Research and Basic Medical Sciences, Chinese Academy of Sciences, Hangzhou, Zhejiang, 310022, People’s Republic of China; 8Department of Medical Oncology, Sun Yat-Sen University Cancer Center, Guangzhou, Guangdong, 510060, People’s Republic of China; 9State Key Laboratory of Oncology in South China, Guangzhou, Guangdong, 510060, People’s Republic of China; 10Collaborative Innovation Center for Cancer Medicine, Guangzhou, Guangdong, 510060, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wei Jiang; Qitao Yu Department of Respiratory Oncology
Guangxi Medical University Cancer Hospital, No. 71, Hedi Road, Qingxiu District, Nanning, Guangxi, 530021, People’s Republic of China
Tel/Fax +86 0771 5334953
Email [email protected]; [email protected]
Background: Inadequate control of cancer-related pain in China is an ongoing problem. This study investigated the practices of cancer pain (CP) management at major cancer centers in China and perceived hindrances and knowledge of CP management among health professionals.
Methods: From September to October 2019, a survey was conducted using electronic questionnaires via the internet to investigate the practices, and perceived hindrances and knowledge in managing CP among healthcare professionals from 7 provincial cancer centers in China. The questionnaire included demographic data, the professionals’ practices among their own patients, their opinions regarding hindrances to CP management, and knowledge of CP management.
Results: We gathered validated responses from 411 anonymous healthcare professionals, with 82.2% (411/500) of response rate. Based on the analysis of these 411 questionnaires, the results demonstrated that CP was prevalent among patients with cancer, while moderate-to-severe pain took a great proportion. CP management was inadequate for a significant proportion of the patients with CP. Pain assessment, analgesic treatment, attention to adverse effects of analgesic, and multidisciplinary management were usually ineffectual in many cases. The duration of work experience did not significantly affect CP management. The respondents considered that both patients and healthcare professionals were responsible for the undermanagement of CP. Only 26 (6.3%) respondents were able to answer correctly all 10 of the professional questions regarding CP.
Conclusion: CP is commonly undermanaged in China. Effective pain control requires the implementation of standards, and the sufficient attention and training of healthcare professionals.
Keywords: cancer pain, pain control, pain treatment, quality of life, electronic questionnaire
Introduction
Cancer-related pain is one of the most common symptoms among patients with cancer and is often moderate to severe. A population-based study in the Netherlands with 1429 respondents reported that 55% of these patients with cancer had suffered pain in the previous week, and the pain was moderate-to-severe in 44%.1 According to a nationwide survey in China, there are more than 1.8 million patients with newly diagnosed cancer annually, and 61.6% suffer cancer pain (CP). In 50%, CP is moderate to severe; and in 30%, CP is severe.2 More recently, a national survey in the United States found that the prevalence of chronic pain was higher in patients with cancer (30.8%) than in the general population (15.7%).3
With increased attention, there have been substantial improvements in the management of CP,4 and updated guidelines, educational interventions, and patient education have resulted in a gradual decline in undertreatment. Greco et al5 reported that from 2007 to 2013, the rate of undertreatment of CP decreased from 43.4% to 31.8%, and in the Asian population the decrease was from 59.1% to 45.2%.
However, the undermanagement of CP in China remains prevalent. A survey of 477 patients with cancer in Beijing revealed that 78.8% had experienced moderate to severe pain during the previous 24 hours (42.4% and 36.3% for moderate and severe, respectively). Rates of patient dissatisfaction with analgesic treatment were mild (10.0%), moderate (7.9%), and strong (1.4%).6 Xia et al7 reported that 43.8% of patients in several tertiary hospitals in China complained of inadequate control of CP.
The three barriers to adequate CP management are healthcare professionals, patients, and the healthcare system.8 A worldwide, regional, and national study faulted especially the absence of training and awareness of medical professionals, but also the fear of dependence and restricted financial resources of the patients.9
Clarifying the deficiencies in CP management that can be controlled by healthcare professionals may help promote effective control of CP. We surveyed the practices, perceived barriers, and knowledge of CP management among healthcare professionals from 7 provincial cancer centers across China.
Methods
Respondent Eligibility
We chose 7 cancer centers from different regions with differing economic development in China. The institutional review board of the following 7 hospitals approved this study: Guangxi Medical University Cancer Hospital; Shandong Cancer Hospital Affiliated to Shandong University; Hunan Cancer Hospital & The Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University; Henan Cancer Hospital & The Affiliated Cancer Hospital of Zhengzhou University; Fudan University Shanghai Cancer Center; Cancer Hospital of the University of Chinese Academy of Sciences & Zhejiang Cancer Hospital; and Sun Yat-sen University Cancer Center.
Healthcare professionals from the above 7 provincial cancer centers in China were surveyed from September to October 2019. The participants were informed about the purpose of this survey, and that it was conducted in accordance with the Declaration of Helsinki. The respondents deemed eligible comprised physicians and nurses who were actively providing analgesic treatment for patients with CP; had worked in the 7 investigated cancer centers for at least one year; and willingly participated in this study. Written consent was obtained from all the included participants.
Study Design
The questionnaire (completed in 8–10 min) was designed by a panel of 6 experts (including two medical oncologists, a surgical oncologist, a radiologist, a pain specialist and a nurse) with up to 10 years of experience in cancer management. Information including demographic data of respondents, practice of CP management among their own patients, their opinions regarding obstacles to pain management, and their basic knowledge of CP management was collected (see Supplementary material). Questions regarding barriers to CP management was developed based on literature reviews10–13 summarized as healthcare professionals, patients, and the healthcare system. Ten questions regarding CP-related professional knowledge were designed through the discussion of our experts panel based on the review of literatures11,14 and National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines of Adult Cancer Pain to assess the knowledge of pain assessment, pharmacy, analgesia therapy, and characters of cancer pain. Pilot-testing was conducted and the questionnaire was revised by researchers accordingly.
For a recovery of 400 questionnaires as our plan, we delivered 500 pieces, with an estimation of 20% no response. CP occurrence in the department of medical oncology was approximate three times compared to the department of surgery or other departments (including department of radiotherapy and department of interventional therapy) based on pilot-tested. We presumed that higher proportion of advanced disease in the department of medical oncology may contribute to higher CP occurrence. Therefore, we delivered the questionnaires randomly, in a 3:1:1 ratio, in the department of medical oncology (300 pieces), the department of surgery (100 pieces), and other departments (100 pieces). The healthcare professionals responded anonymously to questionnaires via the internet. Each responder received 10 RMB in compensation.
Statistical Analysis
Statistical differences were determined by Mann–Whitney test or chi-squared test. P values less than 0.05 were considered statistically significant. All analyses were conducted using SPSS v17.0 software (SPSS, Chicago, USA).
Results
General Characteristics of the Respondents
With a total of 500 questionnaires sent out, 411 healthcare professionals responded. Response rate was 82.2%. The respondents included 186 physicians (45.3%) and 225 nurses (54.7%); 79 (19.2%) men and 332 (80.8%) women (Table 1). The median age was 32 years (20–60 y), and the median duration of work experience was 8 years (1–44 y). Among the respondents, 207 (50.4%), 154 (37.5), and 50 (12.2) held junior (residents or junior nurses), intermediate (attendings or senior nurses), and senior (chief physician or chief nurse) academic titles, respectively. The majority of physicians (90.3%) and nurses (83.1%) had ever attended any form of CP training.
 |
Table 1 Demographics of the Respondents* |
Prevalence of CP Among the Patients of the Respondents
A percentage of 31.4% respondents reported a range of 10–30% of their patients had experienced CP in the previous month, while 38.0% of respondents reported 30–50% (Table 2). Moderate to severe CP was prevalent among patients with CP, with 45.0% of respondents reporting 10–30% incidence of moderate to severe CP, and 33.1% of respondents reporting 30–50%. Only 58.9% of respondents reported that undermanagement of CP occurred in <10% of patients with CP treated with analgesics. A percentage of 74.7% respondents reported incidence of refractory CP was <10%.
 |
Table 2 Status of CP Among the Patients of the Respondents* |
Respondents’ Management of CP
Table 3 presents the management of CP among respondents. Fewer than half (46.2%) of the respondents reported that >90% of their patients were routinely screened for CP; while 56.9% performed a comprehensive assessment of CP within 8 hours of admission among >90% of their patients. Standardized pain assessment tools, including the Numerical Rating Scale and Visual Analog Scale, were limitedly used for CP assessment, with 52.1% of respondents using among >90% of their patients.
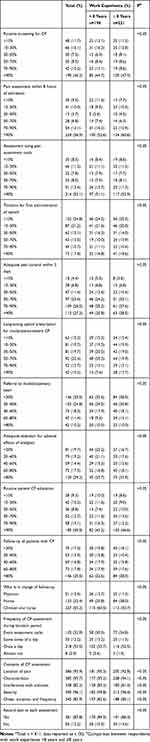 |
Table 3 Management Rates of Patients with CP* |
Surprisingly, the proportion of titration for patients receiving opioid for the first time was low, with 24.8% of respondents rarely (<10% of their patients) performing titration for first administration of opioid. During titration, 53.0% of the respondents performed assessment only once daily; while only 32.9% performed a stabilized assessment in every assessment cycle. Among patients with moderate-to-severe CP, the prescription of long-acting opioids was not satisfactory, with only 10.2% of respondents prescribing long-acting opioids for >90% of their patients. Only 27.3% of respondents reported that >90% of their patients were given adequate pain control within 3 days since CP presentation. Multidisciplinary involvement in the management of CP was insufficient, with 35.5% of respondents rarely (<20% of their patients) referred to a multidisciplinary team. Quite a few patients were not paid attention for adverse effects associated with analgesic treatment, with only 29.2% of respondents concerning about the assessment, prevention and management of adverse effects for >80% of their patients.
We divided the included respondents into two groups based on the median of the work experience duration. Overall, the practice of CP management was not remarkably different between respondents with duration of work experience <8 years and ≥8 years, indicating that the duration of work experience did not significantly affect CP management.
Barriers and Obstacles of CP Management
Among the respondents, 71.3% believed that undermanagement of CP by healthcare professionals was due to poor drug efficacy against refractory CP in a complex condition; 63.8% stated that empiric prescription without personalized treatment was a problem; and for 50.6%, lack of knowledge about CP was a deciding factor (Table 4). The participants reported 3 main factors of undermanagement of CP attributed to patients: according to 80.5%, 72.0%, and 63.0%, these factors were, respectively, low opioid adherence and random medication, misconceptions about CP treatment, and a fear of opioid addiction. Furthermore, 76.9%, 59.4%, and 57.7% attributed obstacles to patient use of opioids as, respectively, patients’ concerns about drug addiction, healthcare professionals’ concerns regarding adverse effects, and patients’ rejection of opioids.
 |
Table 4 Barriers to CP Managementa |
Knowledge of CP Management
Among the 411 respondents, only 26 (6.3%) could correctly answer all of the 10 questions concerning professional knowledge of CP (Table 5). The percentage of physicians who achieved a perfect score (7.5%) was slightly higher but statistically comparable to that of the nurses (5.3%).
 |
Table 5 Rates of Correct Response Regarding CP-Related Professional Knowledgea |
Notably, regarding the timing of assessment after oral short-acting morphine sulfate, only 40.9% of the respondents provided a correct response, which was significantly higher among nurses (46.2%) than physicians (34.4%). For moderate CP, 44.2% of respondents preferred low-dose strong opioids to weak opioids such as tramadol for moderate cancer pain; physicians were significantly more favorable (51.1%) than nurses (38.7%). Only 54.5% of the respondents answered correctly that patients with CP should not be given pethidine; a significantly higher percentage of physicians (64.5%) answered correctly than did the nurses (46.2%). For 6 questions regarding analgesic drugs, a significantly higher percentage of physicians answered correctly, but for one question regarding CP assessment, the percentage of nurses with the correct response was significantly higher than the physicians.
The majority of the respondents (74.8%, 71.4%, and 70.4%) wished to learn more, respectively, about the management of refractory CP; developments in CP and palliative care; and opioid titration protocol, dose adjustment, and adverse event management.
Discussion
The most widely accepted algorithm for CP treatment is the 3-tiered CP ladder developed by the World Health Organization (WHO) in 1982. Since 1990 when this algorithm was promoted in China, CP treatment has gradually received more attention and become standard. However, the control of pain is still inadequate for numerous patients.7 In the present study, results revealed that the healthcare professionals in China remain face the prevalence of CP among patients with cancer. Noteworthily, moderate-to-severe pain took a great proportion of CP. This survey was conducted in provincial cancer hospitals that constitute the highest level of oncologic expertise in China, yet the issue of CP undermanagement has confronted us. Many patients experience CP that was not effectively and quickly controlled. This study found that assessment of CP, prescription of analgesic drugs, and attention to adverse effects of analgesic drugs remains far from satisfactory, and there is much room for improvement. Moreover, most patients did not receive multidisciplinary CP management, although all included cancer centers have multidisciplinary teams for CP management recruiting experts in medical oncology, radiation oncology, surgery, intervention, anesthesiology, and/or nursing (based on the results of pre-investigation). With emphasis on multidisciplinary management of CP from the recommendation of major guidelines, multidisciplinary teams were increasingly built at many cancer centers in China. However, we are still at the beginning of multidisciplinary pain management and multidisciplinary involvement is still absent or a mere formality in many cases.
Many studies have shown that failure to make an accurate assessment of CP is a common obstacle to CP control.15,16 As we known, scientific and accurate CP assessment is the cornerstone of management. However, in the present study, standardized pain assessment tools were limitedly used for CP assessment, and only 32.9% of the respondents performed a standardized CP assessment for every assessment cycle. We attribute the deficiency of CP assessment to lack of knowledge of protocol, inadequate appreciation of its importance, busy clinical work, and the tediousness of repeated assessment. For example, only 40.9% of the respondents knew the correct timing of assessment after administration of oral short-acting morphine sulfate. Performing incorrect assessment, or even no assessment, results in poor CP management. Therefore, correct assessment requires basic knowledge by professionals, and meticulous work. Assessment should not only be routine, quantitative, and comprehensive, but employed throughout CP management, and is crucial for CP management.
In this study, 44.2% of the respondents preferred to prescribe weak opioids rather than low-dose strong opioids for moderate CP, which was in line with insufficient prescription of long-acting opioids for patients with moderate to severe CP. In the past 30 years, the 3-tiered CP ladder algorithm has proved greatly effective for CP control and has been widely applied. Yet, over time its shortcomings have also become salient. Since 1994, the role of weak opioids in moderate CP has raised considerable controversy. Many studies have shown that weak opioids have short analgesic duration and poor analgesic effect, but are accompanied by adverse events.17–19 Accumulating evidence supports that early administration of strong opioids can prevent central sensitization and development to refractory CP.19–23 A prospective study revealed that patients with terminal cancer given strong opioids had better pain relief and greater satisfaction with treatment when compared with patients given the three-tiered CP ladder regime.9 Since 2012, practice guidelines in CP have been revised by the European Association for Palliative Care (EAPC), European Society for Medical Oncology (ESMO), and National Comprehensive Cancer Network (NCCN). The new guidelines recommend that strong rather than weak opioids should be prescribed during the second step of the 3-tiered CP ladder. Patients with moderate and severe CP should be prescribed strong opioids, but instead the traditional CP ladder is often adhered to, due to lack of updated training in CP management.
The present study determined that a major factor related to undermanagement of CP was due to healthcare professionals. The poor scores of the respondents for professional knowledge of CP management is unsatisfactory, and reflect deviations from standard protocol in provincial tumor hospitals that include CP assessment, treatment, and attitude toward adverse effects. Inaccurate assessment, lack of knowledge regarding analgesic drugs, and concerns about adverse events from healthcare professionals may impede the prescription of analgesic drugs, result in non-standard use of analgesic drugs, and application of empirical rather than personalized CP management. Given these dilemmas, healthcare professionals struggle to develop a reasonable and effective analgesic regimen, and undermanagement of CP is common.
The physicians’ scores for basic knowledge of analgesic drugs in CP management were significantly higher than that of the nurses. This may be because physicians prescribe drugs, but nurses sometimes simply implement orders without understanding or thinking about them. However, the scores of the nurses regarding CP assessment were higher than that of the physicians. This indicates that nurses may be more aware and in better communication with patients’ CP than physicians.
Previous study indicated that patients also contribute to the undermanagement of CP.10 In this survey, the respondents usually attributed undermanagement of CP regarding patients to low opioid adherence, especially because of fear of addiction. As we known, this fear may lead to concealing pain, poor adherence with analgesic treatment, and rejection of opioid or random medication. To address this problem, healthcare professionals must pay more attention to patient education and follow-up. It is encouraging that a great proportion of patients were given routine education and follow-up from respondents concerning CP. Nevertheless, educational interventions targeting patients as well as professionals, have been shown to improve pain outcomes.24
The respondents of the present study reported the wish to learn more about advances in CP management, management of refractory CP, and therapeutic strategies including opioid titration, dose adjustment, and adverse event management. Supplemental education based on these weaknesses could help further standardize CP management, enhance the efficacy of CP treatment, and improve patients’ quality of life.
There were several limitations of this study. First, with respect to our choice of 7 included institutes, selection bias was existing; Nevertheless, the included cancer centers were chosen from different regions with differing economic development, and our survey at these centers maybe representative in China. Second, this study did not include patient-reported outcome and not demonstrate the real deficiencies in patient with cancer pain, which need our further investigation in future. Last, the absence of the definition regarding “cancer pain training” in Question 8 and the frequency of follow-up regarding cancer pain in Question 22 in this questionnaire may affect the reliability of these issues.
Conclusion
In conclusion, the undermanagement of CP remains a substantial problem. Yet, sufficient attention, greater professional knowledge, and particular emphasis on adequate pain treatment from healthcare professionals can promote effective pain control. Educational interventions and CP management standards are urgently needed to improve the efficacy of CP management.
Funding
This work was carried out with the supports of Beijing Xisike Clinical Oncology Research Foundation (No. Y-2019AZQN-04532), the International Communication of Guangxi Medical University Graduate Education and the Innovation Project of Guangxi Graduate Education (No. YCSW2017108).
Disclosure
The authors declare that there are no conflicts of interest.
References
1. van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. High prevalence of pain in patients with cancer in a large population-based study in The Netherlands. Pain. 2007;132(3):312–320. doi:10.1016/j.pain.2007.08.022
2. Liu Z, Lian Z, Zhou W, et al. National survey on prevalence of cancer pain. Chin Med Sci J. 2001;16(3):175–178.
3. Sanford NN, Sher DJ, Butler SS, et al. Prevalence of chronic pain among cancer survivors in the United States, 2010–2017. Cancer. 2019;125(23):4310–4318. doi:10.1002/cncr.32450
4. van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage. 2016;51(6):1070–1090 e1079.
5. Greco MT, Roberto A, Corli O, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32(36):4149–4154. doi:10.1200/JCO.2014.56.0383
6. Wei W, Bangwei C, Xiaohong N, et al. Progress and challenges in pain management in Beijing in last 20 years——multicenter investigation of cancer pain management in Beijing (FENPAI4090). Chin J Pain Med. 2014;20(1):5–12.
7. Xia Z. Cancer pain management in China: current status and practice implications based on the ACHEON survey. J Pain Res. 2017;10:1943–1952. doi:10.2147/JPR.S128533
8. Deandrea S, Montanari M, Moja L, Apolone G. Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol. 2008;19(12):1985–1991. doi:10.1093/annonc/mdn419
9. Berterame S, Erthal J, Thomas J, et al. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet. 2016;387(10028):1644–1656. doi:10.1016/S0140-6736(16)00161-6
10. Kwon JH. Overcoming barriers in cancer pain management. J Clin Oncol. 2014;32(16):1727–1733. doi:10.1200/JCO.2013.52.4827
11. Jho HJ, Kim Y, Kong KA, et al. Knowledge, practices, and perceived barriers regarding cancer pain management among physicians and nurses in Korea: a nationwide multicenter survey. PLoS One. 2014;9(8):e105900. doi:10.1371/journal.pone.0105900
12. Scarborough BM, Smith CB. Optimal pain management for patients with cancer in the modern era. CA Cancer J Clin. 2018;68(3):182–196. doi:10.3322/caac.21453
13. Gunnarsdottir S, Sigurdardottir V, Kloke M, et al. A multicenter study of attitudinal barriers to cancer pain management. Support Care Cancer. 2017;25(11):3595–3602. doi:10.1007/s00520-017-3791-8
14. García-Mata J, Álamo C, de Castro J, et al. A survey of perceptions, attitudes, knowledge and practices of medical oncologists about cancer pain management in Spain. Clin Transl Oncol. 2018;20(8):1061–1071. doi:10.1007/s12094-017-1826-8
15. Breuer B, Fleishman SB, Cruciani RA, Portenoy RK. Medical oncologists’ attitudes and practice in cancer pain management: a national survey. J Clin Oncol. 2011;29(36):4769–4775. doi:10.1200/JCO.2011.35.0561
16. Silvoniemi M, Vasankari T, Vahlberg T, Vuorinen E, Clemens KE, Salminen E. Physicians’ self-assessment of cancer pain treatment skills–more training required. Support Care Cancer. 2012;20(11):2747–2753. doi:10.1007/s00520-012-1396-9
17. Ventafridda V, Tamburini M, Caraceni A, De Conno F, Naldi F. A validation study of the WHO method for cancer pain relief. Cancer. 1987;59(4):850–856. doi:10.1002/1097-0142(19870215)59:4<850::AID-CNCR2820590432>3.0.CO;2-1
18. Straube C, Derry S, Jackson KC, et al.Codeine, alone and with paracetamol (acetaminophen), for cancer pain. Cochrane Database Syst Rev. 2014;(9):CD006601. doi:10.1002/14651858.CD006601.pub4
19. Bandieri E, Romero M, Ripamonti CI, et al. Randomized trial of low-dose morphine versus weak opioids in moderate cancer pain. J Clin Oncol. 2016;34(5):436–442. doi:10.1200/JCO.2015.61.0733
20. Marinangeli F, Ciccozzi A, Leonardis M, et al. Use of strong opioids in advanced cancer pain: a randomized trial. J Pain Symptom Manage. 2004;27(5):409–416. doi:10.1016/j.jpainsymman.2003.10.006
21. Chapman EJ, Edwards Z, Boland JW, et al. Practice review: evidence-based and effective management of pain in patients with advanced cancer. Palliat Med. 2020;34(4):444–453. doi:10.1177/0269216319896955
22. Wiffen PJ, Wee B, Derry S, Bell RF, Moore RA. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;7:CD012592.
23. Corli O, Floriani I, Roberto A, et al. Are strong opioids equally effective and safe in the treatment of chronic cancer pain? A multicenter randomized Phase IV ‘real life’ trial on the variability of response to opioids. Ann Oncol. 2016;27(6):1107–1115. doi:10.1093/annonc/mdw097
24. Adam R, Bond C, Murchie P. Educational interventions for cancer pain. A systematic review of systematic reviews with nested narrative review of randomized controlled trials. Patient Educ Couns. 2015;98(3):269–282. doi:10.1016/j.pec.2014.11.003
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
