Back to Journals » International Journal of Women's Health » Volume 14
POTS and Pregnancy: A Review of Literature and Recommendations for Evaluation and Treatment
Authors Morgan K , Smith A, Blitshteyn S
Received 1 August 2022
Accepted for publication 6 December 2022
Published 24 December 2022 Volume 2022:14 Pages 1831—1847
DOI https://doi.org/10.2147/IJWH.S366667
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Kate Morgan,1 Angela Smith,2 Svetlana Blitshteyn3,4
1School of Medicine and Public Health, Faculty of Health, The University of Newcastle, Newcastle, New South Wales, Australia; 2HNE Health Libraries, Hunter New England Local Health District, Newcastle, New South Wales, Australia; 3Department of Neurology, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, Buffalo, NY, USA; 4Dysautonomia Clinic, Williamsville, NY, USA
Correspondence: Svetlana Blitshteyn, 300 International Drive, Suite 100, Williamsville, NY, 14221, USA, Tel +1-716-531-4598, Fax +1-716-478-6917, Email [email protected]
Abstract: Postural Orthostatic Tachycardia Syndrome (POTS) is a disorder of the autonomic nervous system most commonly affecting women of reproductive age. Studies on POTS and pregnancy are limited, and there is a lack of clinical guidelines regarding assessment and management of pregnant women with POTS. The purpose of this review is to summarize data from the available studies on the topic of pregnancy in POTS and common comorbid conditions and to provide the clinical recommendations regarding evaluation and treatment of POTS in pregnant women, based on the available studies and clinical experience. We conclude that pregnancy appears to be safe for women with POTS and is best managed by a multi-disciplinary team with knowledge of POTS and its various comorbidities. Importantly, large, prospective studies are needed to better delineate the course and outcomes of pregnancy, as well as possible pregnancy-related complications in women with POTS. Clinicians should be aware of the clinical presentation, diagnostic criteria, and treatment options in pregnant women with POTS to optimize outcomes and improve medical care during pregnancy and post-partum period.
Keywords: POTS, pregnancy, Ehlers-Danlos syndrome, migraine, post-partum
Introduction
Postural orthostatic tachycardia syndrome (POTS) is a disorder of the autonomic nervous system characterized by symptoms of orthostatic intolerance, such as palpitations, tachycardia, pre-syncope, syncope, and non-orthostatic symptoms, such as fatigue, cognitive complaints, also known as “brain fog”, headache, and gastrointestinal symptoms. POTS is four times more prevalent in females, particularly of childbearing age, which raises a number of issues surrounding pregnancy and post-partum health.1,2 It is estimated that up to 3 million people in the United States may have had POTS before the pandemic but the prevalence is now significantly higher due to post-COVID POTS that may follow a SARS-CoV-2 infection as part of the post-acute sequelae of the virus.3 In addition to being precipitated by a viral or bacterial infection, POTS may also occur following a pregnancy, surgery, menarche, or trauma.2
The diagnostic criteria for POTS include 1) an increase in heart rate of at least 30 beats per minute in adults and at least 40 beats per minute in teens up to 19 years of age within 10 minutes of standing or a tilt table test; 2) absence of orthostatic hypotension; and 3) symptoms of orthostatic intolerance present for at least six months.4 Other conditions that can mimic POTS, such as infection, dehydration, severe anemia, prolonged bed rest, hyperthyroidism, pheochromocytoma, and anorexia nervosa, need to be excluded. Treatment and management is symptomatic, consisting of both pharmacologic and non-pharmacologic therapies, and a multidisciplinary approach is often necessary to reduce symptoms and functional impairment.1,2,5
Normal Maternal Physiology in Pregnancy
Normal physiological changes in pregnancy may mimic or exacerbate the symptoms of POTS. There are significant changes in maternal cardiovascular physiology: the three main physiological changes are an increase in maternal blood volume, an increase in maternal cardiac output, and a reduction in maternal blood pressure.6,7
Maternal blood volume starts to increase in the first trimester, with the total volume increasing up to 45% from baseline; both plasma and red cells are increased.7 This supports the growing fetus as well as prepares for blood loss during labor and delivery.7 In the first and second trimester, the increase in maternal blood volume causes the heart rate and stroke volume to increase, leading to an increase in cardiac output. Maternal cardiac output varies in the third trimester and returns to baseline post-partum.7 Maternal heart rate steadily increases over the course of the pregnancy, normally by 10 to 20 beats per minute.7 Blood pressure is reduced during pregnancy due to peripheral vasodilation. This systemic vasodilation occurs due to increased levels of estrogen, progesterone and relaxin.7 The renin-angiotensin-aldosterone system is activated and increases blood volume to mitigate the vasodilatory effects of the hormones.7
Methods
Sources
A search of the available literature was conducted in May 2022. The electronic databases CINAHL, Medline, PsycINFO, The Cochrane Library, and Embase were searched for relevant articles. Search strategies were developed by a research librarian (AS). An initial strategy was developed in Medline before being translated to other databases. Databases were selected based on their coverage of a wide range of health disciplines and include both qualitative and quantitative literature. There were no limitations on date range in the POTS search due to a paucity of published data available.
Inclusion Criteria
Studies were included for review if they were full text, published in English, and discussed pregnancy in relation to pre-existing Postural Orthostatic Tachycardia Syndrome (POTS), hypermobile Ehlers-Danlos Syndrome (hEDS), chronic fatigue syndrome (CFS), mast cell activation syndrome (MCAS), syncope, common autoimmune disorders, or migraine.
Exclusion Criteria
Studies were excluded if they were not available in full text or not published in English.
Included Studies
We identified and included in this review 12 studies, including case reports, and 3 reviews on the topic of POTS and pregnancy (Table 1).
 |  |  |  |
Table 1 Overview of Included Literature |
Results
POTS and Pregnancy
Symptoms During Pregnancy
Symptoms of POTS appear to be variable throughout the pregnancy with a tendency toward improvement during pregnancy.8–12 Women who reported severe POTS symptoms at the time of conception were more likely to experience a worsening of symptoms during the pregnancy,8,9 whereas women who had mild to moderate POTS symptoms or did not require medication at the time of conception tended to experience stability or improvement in symptoms during their pregnancy.10 Autonomic function tests did not differ between women with POTS who had children and those who did not. Overall, there was a reported trend toward improvement in the autonomic dysfunction in the short-term post-partum period.13
In the first trimester, POTS symptoms were often exacerbated, but in the second trimester, there was an overall improvement in POTS symptoms.8,13–15 The third trimester was variable with some women reporting a worsening of symptoms while other women maintained the feeling of wellness.10,12,14,15 The improvement in symptoms, particularly in the second and third trimester, is thought to be due to the increase in blood and plasma volumes during pregnancy, which increases blood pressure and cardiac output.10,13,14,16 Studies have reported either stable or improved symptoms in 60–68% of pregnant women, with 30–40% experiencing worsening of symptoms.10,12,15
Labor and Delivery
POTS may present a challenge during labor and delivery in some women with POTS due to the potential for tachycardia and hemodynamic instability. Early utilization of anesthetic management during labor is recommended for pregnant women with POTS since pain is a major trigger of the autonomic instability.12,21–23 Epidural anesthesia placed early can decrease pain and avoid blood pressure and heart rate changes in response to pain. Natural birth without pain control is not recommended and should probably be avoided, despite a case series describing 2 women with POTS who have gone through labor and delivery without anesthetic interventions.9 Hydration with IV saline or Lactated Ringer’s solution prior to epidural catheter placement should be considered to counteract possible hypotension induced by epidural anesthesia.19,22–24 If vasoconstrictors are needed, phenylephrine may be utilized since it can help prevent reactive tachycardia caused by peripheral vasodilation, which may lead to hypotension.9,19–23 Additionally, we do not recommend a home birth for women with POTS due to a pre-existing medical condition that may require close monitoring of the vital signs.
Vaginal delivery appears to be safe for the majority of women with POTS and is the preferred mode of delivery.6,8,9,12,14,15,23 With that in mind, decisions regarding delivery should be based on obstetric and surgical considerations rather than POTS. The risk of complications and adverse events during labor and delivery appear to be the same as the general population, and none were attributed directly to POTS in small studies and case reports. Large prospective studies are needed to verify these findings.12,15,19,23
Post-Partum
Post-partum symptoms of POTS remained variable, with half of women reporting their symptoms to be stable, particularly while the mother was still breastfeeding.8,12,13,16 This may be due, in part, to physical reconditioning and incidental upper body resistance training that naturally occurs when looking after an infant.6,9,13 One study reported that 50% of women felt either the same or better compared to before pregnancy, and 50% felt that their symptoms had worsened.12 However, to date, no longitudinal studies have been conducted to determine the course of POTS following a pregnancy and whether there is a higher prevalence of post-partum complications, including post-partum mood disorders, in women with POTS. Given that maternal chronic illness is one of the risk factors for post-partum depression and that increased sympathetic activation may underlie pregnancy-induced hypertension, it’s possible that the prevalence of both is increased in women with POTS.17,18
Complications and Adverse Effects
Based on several available studies conducted to date, complications and adverse events to the mother and infant do not appear to be increased in women with POTS than in the general population; those complications that did occur were thought to be unrelated to POTS.13,20 One study found an increased risk of hyperemesis gravidarum in women with pre-existing POTS; the reason for this finding is unclear, although it may be related to a higher rate of migraine in POTS patients, which can be associated with hyperemesis gravidarum.12 Women experiencing hyperemesis gravidarum require close monitoring of their hemodynamic status, anti-emetics, fluid replacement therapy, and consideration of thrombotic risk.9 Further research regarding complications and adverse events for pregnant POTS patients is warranted via pregnancy registries and large prospective studies.
Breastfeeding
Breastfeeding is safe and should be encouraged. It may be beneficial in reducing symptoms due to the antidiuresis effect caused by the release of oxytocin in the bloodstream, and it obviously has enormous benefits for the infant.6 However, some women with POTS may find breastfeeding challenging due to plasma volume shifts, higher requirements for fluids and salt intake, and interrupted sleep schedule, which may result in an overall worsening of POTS symptoms. In some cases, breastfeeding may become detrimental to maternal physical and/or mental health,17 and accommodations with breast pumps and accumulating milk supply that may be given in a bottle by another caretaker could be implemented. Ultimately, these authors emphasize the need to maintain physical and mental health of the mother as a priority in addition to providing nutrition and adequate caloric intake for the baby, whether feeding takes on the form of breastfeeding or bottle-feeding with breastmilk or formula.
POTS Co-Morbidities and Pregnancy
At least 80% of patients with POTS have one or more comorbidities, which may present an additional challenge in pregnancy. There are several common comorbid conditions that are highly prevalent in POTS, including migraine, hypermobile Ehlers-Danlos Syndrome (EDS), chronic fatigue syndrome (CFS), syncope, mast cell activation syndrome (MCAS) and autoimmune disorders.1,25 Clinicians caring for pregnant POTS patients need to be aware of the common comorbid conditions and their special considerations in pregnancy to ensure the best maternal and fetal outcomes.
Migraine
It is estimated that 40% of POTS patients also experience migraine, making migraine a significant consideration when caring for pregnant women with POTS.1,2 Migraine is a neurological disorder characterized by recurrent severe headache and a range of associated symptoms, many of which are autonomic. The pathophysiology of migraine is complex and involves the central nervous system, central and peripheral autonomic networks, central sensitization, neuroinflammation and other mechanisms, with shared and overlapping mechanisms noted in both POTS and migraine.29,30 Many factors can affect the type and duration of migraine experienced, including hormonal changes.31,32
During pregnancy, migraine often goes into remission, and during the first trimester, there may be some improvement in the quality and intensity of symptoms. The second and third trimesters often have the greatest improvement or complete remission.31–34 Rates of improvement are higher in those who experience migraine without aura compared to those who experience aura before migraine.32,33 The intensity and quality of the migraine often improve, possibly due to rising levels in estrogen and its positive effect on pain levels.33 Women who do not experience improvement by the end of the first trimester will often continue experiencing migraine throughout the pregnancy. These women may also experience migraine with higher intensity in subsequent pregnancies.33 Migraine during pregnancy has been shown to be associated with increased risk of hypertensive disorders, low birth weight, preeclampsia, and miscarriage.32,34,35 Migraine does not appear to have any effect on labor and delivery.33 During the first week post-partum, women may experience severe migraine, possibly due to the sudden drop in estrogen levels. This usually normalizes after the first week, and rates of migraine will usually return to the pattern of migraine during pregnancy.33
Nonpharmacological treatments for migraine are in many ways similar to those used in POTS. Ensuring adequate hydration, nutrition, sleep, and exercise is recommended for both patients with migraine and patients with POTS.1,32 Medications to treat migraine should be used sparingly and in consultation with a specialist due to the potential harm of some medications on the developing fetus.31,33 The use of propranolol as a preventative treatment for migraine also overlaps with the treatment for POTS and may help to reduce the incidence and severity of both conditions.15,31,32 It remains unclear if breastfeeding is protective for migraine.33 Close monitoring and consultation with a neurologist specializing in headache medicine is recommended to manage pregnant patients with migraine and POTS. 31,33
Hypermobile Ehlers-Danlos Syndrome and Hypermobility Spectrum Disorders
Ehlers-Danlos syndromes are genetic disorders involving collagen, which commonly affect the connective tissue, including joints and skin. The most common type is hEDS, but hypermobility spectrum disorders (HSD) that encompass patients who do not qualify for a diagnosis of hEDS are also common among patients with POTS.36,37 The prevalence of hEDS/HSD in POTS is high, with reports of 31% of POTS patients meeting the criteria for hEDS and a further 24% for non-hEDS generalized joint hypermobility.36,37 Both hEDS and HSD can complicate pregnancy and need to be considered in pregnant women with POTS and EDS/HSD. Early consultation with a multidisciplinary team is encouraged to support and manage pregnant women with POTS and hEDS/HSD. Hormonal changes during pregnancy can exacerbate hEDS/HSD symptoms and increase maternal and fetal risks during pregnancy, labor and delivery.36
During pregnancy women may experience increased pain due to the increased laxity and instability of the joints. Pelvic girdle pain is common, and in some severe cases may result in women utilizing wheelchairs for mobility.25,36 Other symptoms during pregnancy include back pain, heartburn, headache, heart palpitations, varicosities, edema, tinnitus, sleep disturbance, nausea, and vomiting. Regular early physiotherapy is recommended to aid in joint strengthening, stability, and pain relief.25,36
There are some special considerations for women with hEDS/HSD during labor that the treating team must be aware of. Pre-labor spontaneous rupture of membranes is more common in women with hEDS/HSD due to the fragility of the membranes.25,36 Early review of anesthetic agents by an anesthesiologist is recommended as hEDS/HSD patients have a higher incidence of responding poorly to lidocaine.25,36 Due to increased laxity in the vessels and when co-morbid dysautonomia is present, anesthesia may cause significant hypotension.36
In the active labor phase, women with hEDS/HSD are prone to a precipitous labor, which can increase physiological risks to both the mother and the infant as well as exacerbate POTS symptoms. Healthcare staff must be aware of this risk and be prepared to assist women in the event of a fast labour.25,36 Women with hEDS/HSD are more likely to birth without instrument assistance due to the increased laxity of the connective tissue in the pelvis. This laxity in the joints and connective tissue may also cause the baby to be delivered in an unusual position, without the need for intervention.25,36 hEDS/HSD can cause alterations in bleeding due to the tissue fragility; pregnancy in women with vascular EDS may be contraindicated.36 While most women with hEDS/HSD will not experience major hemorrhage, it is imperative that the delivery team is aware of the possibility for major hemorrhage and that they monitor blood loss closely.25,36 Wound healing is often impaired with hEDS/HSD due to the fragility of the skin, and as such, any surgical interventions, including episiotomy, need to be carefully considered.25,36
New mothers with hEDS/HSD will benefit from consultation with a lactation consultant and physiotherapist to provide strategies to aid in the care of the infant while minimizing joint dislocations or increased pain for the mother.36
Women with POTS and co-morbid hEDS/HSD may experience significant challenges during pregnancy, labor and delivery. Consensus guidelines for the management of pregnancy, birth and post-natal recovery in the context of hEDS, HSD and vascular EDS are currently in progress.38 In the meantime, with careful planning and a multidisciplinary approach consisting of specialists with extensive knowledge of POTS and EDS, these challenges can be minimized, with many women experiencing successful pregnancy, labor and delivery.
Mast Cell Activation Syndrome
MCAS is a common co-morbidity with both POTS and EDS and is a multi-systemic disorder of mast cell hyperactivity that typically manifests with allergic symptoms, gastrointestinal dysfunction, dysautonomia and various genito-urinary and gynecologic manifestations.26–28 Scientific literature on MCAS and pregnancy is extremely limited, consisting of one review article,27 and as such, there is a great need to further delineate the various potential pregnancy complications that could be associated with MCAS via well-designed studies and pregnancy registeries.
Chronic Fatigue Syndrome
CFS is a common co-morbidity of POTS, with many patients qualifying for a diagnosis of CFS due to chronic fatigue and post-exertional malaise that are highly prevalent in patients with POTS. It has been estimated that at least 21% of POTS patients have concurrent CFS.1,2 There is limited research regarding CFS and pregnancy; however, the available evidence suggests that pregnancy is generally safe for women with CFS.39
It is advisable for women to discuss their health and options with the treating team prior to conceiving. Women who have stable symptoms are more likely to have a relatively smooth pregnancy. During pregnancy, approximately 71% of women with CFS experience either stable or improved symptoms, slightly higher than what has been found in women with POTS.39 It is thought that hormonal shifts and immunosuppression to protect the fetus may assist in the relief of symptoms. The remaining 29% of women with CFS may experience a worsening of symptoms during pregnancy.39 This is more likely to occur in women who are still in the early stages of CFS, have unstable symptoms, or who experience a significant number of infectious symptoms, such as temperature dysregulation or flu-like symptoms.39 One study concluded that pregnancy in women with CFS should be managed in the same way as pregnancy for healthy women, but large longitudinal studies are needed to verify this conclusion.39
Labor and delivery appear to be safe and have no contraindications. Early review of anesthetic agents is recommended. Pain relief during labor should be considered to conserve energy as appropriate pain management can reduce energy depletion during labor and delivery.39 Women may experience a significant relapse of symptoms during delivery and immediately afterwards so it is imperative that the obstetrician is aware of CFS to ensure appropriate management.39 In women with CFS, symptoms in the post-partum period remained stable in 30% of women, improved in 20% and worsened in 50% of women. The authors suggest that this may be due to the hormonal changes and physical challenges of caring for a newborn.39
There is no literature available regarding complications and adverse outcomes in women with CFS compared to the general population. One study found no significant difference in the rates of complications when comparing pregnancies before and after the onset of CFS.39 The authors did note a higher rate of miscarriage, which may be due to maternal age or parity.39 Higher rate of miscarriage in pregnant POTS patients was also noted. This suggests that an increased risk of miscarriage in women with POTS and CFS is unlikely to be an incidental finding. Shared pathophysiology between the two conditions as well as other comorbidities that may be present, such as anti-phospholipid syndrome (APS) or another autoimmune disorder, may be a possible factor.12,39,40
Syncope
While presyncope is a common manifestation of POTS, syncope can occur in approximately 30% of patients.41,42 Syncope during pregnancy is linked with adverse events in both the mother and the infant.42 A large population-based study examining rates and outcomes of syncopal episodes in pregnancy found that approximately one percent of the population experiences a syncopal event during pregnancy.42 Of these women, 32% experienced syncope in the first trimester, 44% in the second trimester, and approximately 24% in the third trimester. Eight percent of women experience more than one episode of syncope.42 Compared to pregnancies without syncope, women who experienced syncope were more likely to be younger (age <25 years; 34.7% versus 20.8%), have higher rates of pre-existing medical conditions (1.8% verses 1%), have a history of syncopal events (11.5% verses 3.2%), primiparous (52.1% verses 42.4%), and less likely to be married (57.7% verses 69.8%).42 Preterm birth was higher in women who had previously experienced a syncopal event (16.3%) when compared to women who had never experienced a syncopal event (15%). The first trimester was shown to be the most dangerous time to experience syncope leading to the highest rates of preterm birth (18.3%) compared to second trimester (15.8%) and third trimester (14.2%).42 Low birth weight and babies small for gestational age (SGA) were higher in pregnancies with syncope compared to pregnancies without syncope.42 Congenital abnormalities were significantly higher for children who experienced multiple syncopal events during pregnancy compared to only a single syncopal event (4.9% verses 2.9%).42 Increased maternal risks include cardiac arrhythmias and further syncopal events within a year post birth.42 Clinicians caring for pregnant women with POTS must be aware of the patient’s history of syncope and closely monitor both the mother and the baby during pregnancy and the post-partum period.
Autoimmmune Disorders
Approximately 20% of patients with POTS have comorbid autoimmune disorders, including Hashimoto’s thyroiditis, rheumatoid arthritis, lupus, APS, Sjogren’s syndrome and celiac disease.43,44 Some of the special complications and considerations in pregnancy associated with autoimmune disorders may include a higher miscarriage and stillbirth rate, a possible need for anti-platelet and/or anti-coagulation agents in women with lupus or APS, and monitoring for a possibility of fetal congenital heart block in pregnant women with positive anti-SSA and anti-SSB antibodies.40,45 It’s important to note that a significant number of women will not be diagnosed with an autoimmune disorder until pregnancy or post-partum, and therefore, screening women with POTS with a serum autoimmune panel, including anti-phospholipid, anti-SSA and anti-SSB antibodies, might be prudent to identify women with undiagnosed autoimmune disorders or positive autoimmune markers who are at risk for various pregnancy-related and postpartum maternal or fetal complications.
Discussion
Preconception Considerations
There are no consensus guidelines or randomized studies available on the evaluation or management of pregnant patients with POTS. In women with pre-existing POTS contemplating pregnancy, a multi-disciplinary team consisting of a POTS specialist, an obstetrician-gynecologist, and a maternal-fetal medicine specialist is recommended. This is of particular relevance to pregnant women with POTS who are of advanced maternal age and those women with common POTS comorbidities, such as EDS, chronic migraine, MCAS, or autoimmune disorders. Due to pre-existing chronic illness and the medications that may be involved in managing POTS and comorbidities, a planned pregnancy is obviously preferred to an unplanned pregnancy. A pre-conception discussion and review of medications and their FDA pregnancy categories are important aspects of prenatal care and should convene as early as possible prior to conception.
It may take anywhere from a few weeks to a few months for certain medications, such as stimulants or benzodiazepines, to be discontinued prior to conception. It was previously suggested by some POTS specialists that pregnancy is best to take place when the patient has stable or improved symptoms of POTS for 6–12 months, and while this may be achievable for a subset of POTS patients, others will not be able to have a symptom-free period. It’s been our experience that even women with moderate-to-severe POTS can go through pregnancy and labor safely with certain precautions and a good multi-disciplinary healthcare team. At Dysautonomia Clinic, we have been encouraging women to consider pregnancy before age 35, even if they are symptomatic, and not wait to undertake pregnancy until they are in the late thirties or early forties; this recommendation is encouraged in order to decrease infertility, miscarriage rate, and pregnancy-related complications inherent to advanced maternal age.
Pre-conception counseling should also focus on psychological, social, and financial impacts of pregnancy in the context of a pre-existing chronic medical condition that may be exacerbated by pregnancy and/or post-partum period. Expectations, obligations, and childcare may need to be considered and adjusted accordingly to assist a pregnant woman or a new mother with POTS to care for her infant and herself. While many women with POTS go on to have uneventful pregnancies and deliveries, some will experience pregnancy-related and/or POTS-related complications that may require certain interventions and a change in management. These complications may include hyperemesis gravidarum, which can exacerbate POTS as a result of volume depletion; anemia of pregnancy and resultant exacerbation of POTS via a reduction of red blood cells’ capacity for oxygen delivery; pregnancy-induced hypertension that may also worsen POTS, and pregnancy-related insomnia and mood disorders that may lead to increased fatigue and cognitive impairment. Since migraine is one the most common comorbidities of POTS, migraine assessment and management during pregnancy apply to many pregnant patients with POTS.33 Similarly, various musculoskeletal complications, including joint pain, back pain, sacroiliac joint dysfunction, carpal tunnel syndrome, and joint subluxation and dislocations, may occur in pregnant patients with POTS and EDS, likely at a higher rate than would be expected in healthy pregnant women. A referral to a physiatrist, physical therapist, and/or pain management specialist with knowledge of hereditary connective tissue disorders would be indicated for evaluation and management of these musculoskeletal conditions . Although women with well-controlled POTS who are otherwise fairly healthy and functional may not typically be considered “high-risk” for pregnancy, it’s been our experience that women with more severe POTS symptoms, those who are of advanced maternal age, and those with multiple POTS comorbidities should be considered “high-risk” and should be followed by a maternal-fetal specialist in addition to an obstetrician.
While at this time, there are no data that show an association between POTS and pre-eclampsia, eclampsia, pregnancy-induced hypertension, or post-partum hypertension, clinical experience of the author (SB) suggests that a possible association may exist, and to this end, close monitoring of blood pressure during pregnancy, labor, delivery, and in the post-partum period may be warranted. Furthermore, pregnancy complications associated with EDS must be considered, which may include premature rupture of membranes, fast labor, and alteration in bleeding diathesis and healing after vaginal birth or a C-section. These complications need to be evaluated and managed, where appropriate, by an obstetrician and maternal-fetal medicine specialist.
Evaluation of Pregnant Patient with POTS
Evaluation of pregnant patients with new-onset symptoms suggestive of POTS and without a pre-existing POTS diagnosis should include a thorough history of current symptoms, pre-pregnancy symptoms and disorders, medications, dietary habits, possible caffeine intake, and fluid intake that may have preceded the onset of symptoms and any other triggers that may be associated with new-onset POTS, such as a viral illness, trauma, or immunization (Table 2). Pregnancy is one of the well-described triggers of POTS that was reported to be associated with the onset of POTS in 9% of patients.2 Many women may experience a delayed diagnosis of POTS months to years into the post-partum period, since both patients and physicians often attribute symptoms of presyncope, syncope, tachycardia, and fatigue to pregnancy or common pregnancy complications, such as anemia, hypotension, and pregnancy-related mood disorders. A timely diagnosis of POTS during pregnancy is obviously preferred to a delayed diagnosis because treatment for POTS may lead to improved symptoms and functional status during and after pregnancy and avoid unnecessary diagnostic tests and poor treatment choices.
 |
Table 2 Evaluation Overview for the Pregnant Patient with New Onset POTS Symptoms |
Following a thorough history, physical exam should be performed by a healthcare professional that documents blood pressure and heart rate in the supine and standing position (Table 2). In addition to the vital signs, symptoms during standing, if present, should be noted. Thorough cardiovascular and neurologic exams with sensory examination should be performed to determine if there is any evidence of a heart murmur, cardiomegaly, pupillary dysfunction, or a loss of temperature and pain sensation in the extremities that may suggest small fiber neuropathy, one of the common comorbidities of POTS (Table 2). Since a tilt table test is not recommended for pregnant patients, diagnosis should rely on a 10-min stand test, which is included in the diagnostic criteria for POTS.4 Data from the patient’s personal wearable devices, such as a FitBit or AppleWatch, can be reviewed and utilized as an aid to diagnosis. Laboratory tests may include complete blood cell count, comprehensive metabolic panel, thyroid function tests, free T4, ferritin, morning cortisol, vitamin B12, and brain natriuretic peptide. Other tests may be indicated depending on the clinical picture, such as a serum autoimmune panel and a more comprehensive vitamin and nutrient panel. (Table 2). Additionally, diagnostic tests such as an electrocardiogram, two-dimensional cardiac echocardiogram and a 24-hr Holter monitor, may be obtained to rule out cardiomyopathy, valvular disease and cardiac arrhythmia, and longer cardiac monitoring may be necessary in patients with POTS and intermittent palpitations or episodic tachycardia or syncope (Table 2). If headaches are prominent, different or new compared to pre-pregnancy headaches or accompanied by focal neurologic deficits, abnormal neurologic exam, or associated with blood pressure elevation, MRI of the brain without contrast should be considered to rule out the secondary causes of headache.46
Non-Pharmacologic Management in Pregnancy
Non-pharmacologic therapies are strongly encouraged in women with POTS, are preferable to pharmacotherapy during pregnancy due to their safety profile and should be maximized before initiation of pharmacotherapy is considered (Table 3). Increased fluid intake of at least 2.5L per day and salt (sodium chloride) intake of at least 7 grams per day is recommended, but may be difficult for women with significant nausea, vomiting or hyperemesis gravidarum.47 To this end, intravenous hydration with normal saline can be employed on an as-needed basis for patients who are unable to maintain a desirable fluid intake or those whose clinical features (syncope, pre-syncope, hypotension, or tachycardia) are refractory to standard pharmacologic and non-pharmacologic therapies (Table 3). Intravenous fluids, 1–2 L of normal saline, may be administered over 1–2 hours through a peripheral venous access. Central lines should be generally avoided and placed only as a last resort and after careful consideration due to an increased risk of thrombosis and infection in pregnancy and post-partum period. Waist-high maternity compression stockings can be utilized, and light exercise, such as swimming or recumbent bike, is advisable. Supine exercise in the 2nd and 3rd trimester while lying flat on the back is not recommended due to a growing uterus that can compress both the inferior vena cava and aorta. Similarly, sleeping or napping on the back is not recommended due to a possibility of compression of the inferior vena cava, and patients with POTS need to be instructed to avoid this position and lie on the left side instead. If postural and exertional tachycardia is of concern, consultation with a cardiologist is advisable to discuss the maximum target heart rate, duration, and intensity of exercise in a pregnant woman with POTS. While there are no studies on the benefits of any particular diet in pregnant POTS patients, it’s been our experience that patients with POTS experience significant reduction in various autonomic symptoms with the implementation of a gluten-free diet.48 This may present an effective and safe non-pharmacologic treatment strategy in pregnant women. A consultation with a dietician or nutritionist may be helpful to ensure that nutritional requirements are being met. Finally, psychological and social support is essential for women with POTS who may be particularly vulnerable to pregnancy-related mood disorders as a result of the psychological stress and physiologic changes associated with both pregnancy and POTS. Cognitive behavioral therapy, group therapy, biofeedback, meditation and counseling may be preferred to pharmacotherapy. Anti-depressants, such as escitalopram or sertraline, can be utilized if non-pharmacologic therapies are ineffective and symptoms of depression or anxiety are moderate-to-severe.49 Treatment of anxiety disorders in pregnant patients with POTS may include the same non-pharmacologic therapies as for depression and/or addition of propranolol at a low dose, especially if anxiety is accompanied by tachycardia.
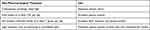 |
Table 3 Non-Pharmacologic Management in Pregnancy |
Pharmacotherapy in Pregnancy
It has been our experience that was reflected in one study that women who take medications for POTS during pregnancy appear to report improved symptoms of POTS compared to those who did not.12 As such, although the ideal scenario is to discontinue all medications pre-conception, this goal will not be achievable for many patients with moderate to severe POTS. Therefore, continuing pre-pregnancy medication or initiating a new or different medication for POTS during pregnancy may be necessary to reduce the symptom burden and disability.
Medications that may be continued during pregnancy usually fall into the pregnancy category B or C and could be necessary in women with more severe POTS who rely on medications for symptomatic control and improved functional status (Table 4). As in pregnant women with other chronic medical disorders, the risks and benefits of each medication should be reviewed, and the lowest number and dose of the safest medications for the fetus should be used during pregnancy. Preferably, one medication at the lowest possible dose should be used and may include a low dose of metoprolol 12.5 mg to 25 mg daily or twice a day, propranolol 5 mg twice a day, fludrocortisone 0.05 mg to 0.1 mg daily, or midodrine 2.5 mg to 5 mg three times a day. If there is concurrent pregnancy-induced hypertension in addition to POTS symptoms, labetalol 100 mg twice a day can be utilized. Pyridostigmine, the only medication used to treat POTS that is pregnancy class B, has been used safely in pregnant women with myasthenia gravis for many decades and may, therefore, present a valuable treatment option in women with pre-existing POTS with worsening of symptoms during pregnancy or in women with new-onset POTS during pregnancy (Table 4). A low dose of pyridostigmine 30 mg twice a day is recommended, but can be increased to a higher dose if warranted by the symptoms. Rarely, a patient with severe POTS and comorbidities, such as a systemic autoimmune disorder or small fiber neuropathy, may be managed via immunotherapy, such as intravenous or subcutaneous immunoglobulin.50,51 These therapies may be continued throughout pregnancy and can be managed for possible dose adjustment by a rheumatologist, immunologist with knowledge of immunotherapies pre- and antepartum, or maternal-fetal medicine specialist.
 |
Table 4 Pharmacologic Therapies for POTS With Pregnancy and Breastfeeding Classification |
Future Direction
There is a significant need for pregnancy registries and multi-center prospective studies that are designed to assess the clinical course, prognosis, possible risk factors, and both obstetrical and POTS managements in order to guide clinicians in their understanding and treatment of pregnant patients with POTS. The available case series and small retrospective studies are undoubtedly insufficient to capture the possible risks – and potential benefits – associated with pregnancy in women with POTS. In the meantime, based on the available literature and personal experience of clinicians specializing in POTS, women with pre-existing POTS may be reassured that to date, it appears that there are no overt contraindications to pregnancy or vaginal delivery secondary to POTS. Whether POTS is associated with increased miscarriage rate, infertility, gestational diabetes, pre-eclampsia, pregnancy-induced hypertension, or post-partum hypertension is unknown at this time and should be further examined in large, prospective well-designed studies. Understanding and awareness of the clinical presentation, diagnostic criteria, and treatment options in patients with POTS, including pregnant women with POTS, are essential to improving medical care and outcomes of pregnancy and post-partum period.
Conclusion
POTS, a common autonomic disorder, is not a contraindication to pregnancy, but may necessitate special considerations, monitoring and management via a multi-disciplinary team, including an obstetrician, a maternal-fetal medicine specialist and a clinician with knowledge of POTS and its various comorbidities, to optimize outcomes and improve maternal and fetal medical care during pregnancy and the post-partum period. Physicians specializing in women’s health and primary care should be aware of the clinical presentation, diagnostic criteria, and treatment options in pregnant women with POTS and women who develop POTS during pregnancy and post-partum period.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vernino S, Bourne KM, Stiles LE, et al. Postural orthostatic tachycardia syndrome (POTS): state of the science and clinical care from a 2019 national institutes of health expert consensus meeting - part 1. Auton Neurosci. 2021;235:102828. doi:10.1016/j.autneu.2021.102828
2. Shaw BH, Stiles LE, Bourne K, et al. The face of postural tachycardia syndrome - insights from a large cross-sectional online community-based survey. J Intern Med. 2019;286(4):438–448. doi:10.1111/joim.12895
3. Jamal SM, Landers DB, Hollenberg SM, et al. Prospective evaluation of autonomic dysfunction in post-acute sequela of COVID-19. J Am Coll Cardiol. 2022;79(23):2325–2330. doi:10.1016/j.jacc.2022.03.357
4. Sheldon RS, Grubb BP, Olshanksky B, et al. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015;12(6):e41–63. doi:10.1016/j.hrthm.2015.03.029
5. Thieben MJ, Sandroni P, Sletten DM, et al. Postural orthostatic tachycardia syndrome: the mayo clinic experience. Mayo Clin Proc. 2007;82(3):308–313. doi:10.4065/82.3.308
6. Ruzieh M, Grubb BP. Overview of the management of postural tachycardia syndrome in pregnant patients. Auton Neurosci. 2018;215:102–105. doi:10.1016/j.autneu.2018.02.002
7. Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014;130(12):1003–1008. doi:10.1161/CIRCULATIONAHA.114.009029
8. Bhatia M, Kavi L, Nelson-Piercy C. Postural tachycardia syndrome and pregnancy. Obstet Gynaecol. 2018;20(2):119–123. doi:10.1111/tog.12478
9. Powless CA, Harms RW, Watson WJ. Postural tachycardia syndrome complicating pregnancy. J Matern Fetal Neonatal Med. 2010;23(8):850–853. doi:10.3109/14767050903265089
10. Morgan K, Chojenta C, Tavener M, et al. Postural orthostatic tachycardia syndrome during pregnancy: a systematic review of the literature. Auton Neurosci. 2018;215:106–118. doi:10.1016/j.autneu.2018.05.003
11. Ruzieh M, Batizy L, Dasa O, et al. The role of autoantibodies in the syndromes of orthostatic intolerance: a systematic review. Scand Cariovasc J. 2017;51(5):243–247. doi:10.1080/14017431.2017.1355068
12. Blitshteyn S, Poya H, Bett GC. Pregnancy in postural tachycardia syndrome: clinical course and maternal and fetal outcomes. J Matern Fetal Neonatal Med. 2012;25(9):1631–1634. doi:10.3109/14767058.2011.648671
13. Kanjwal K, Kanjwal Y, Karabin B, et al. Outcomes from pregnancy in patients with preexisting postural orthostatic tachycardia syndrome. Heart Rhythm. 2009;1:S371.
14. Kimpinski K, Iodice V, Sandroni P, et al. Effect of pregnancy on postural tachycardia syndrome. Mayo Clin Proc. 2010;85(7):639–644. doi:10.4065/mcp.2009.0672
15. Lide B, Haeri S. A case report and review of postural orthostatic tachycardia syndrome in pregnancy. AJP Rep. 2015;5(1):e033. doi:10.1055/s-0034-1544106
16. Glatter KA, Tuteja D, Chiamvimonvat N, et al. Pregnancy in postural orthostatic tachycardia syndrome. Pacing Clin Electrophysiol. 2005;28(6):591–593. doi:10.1111/j.1540-8159.2005.50026.x
17. Brown HK, Wilton AS, Ray JG, et al. Chronic physical conditions and risk for perinatal mental illness: a population-based retrospective cohort study. PLoS Med. 2019;16(8):e1002864. doi:10.1371/journal.pmed.1002864
18. Jarvis SS, Shibata S, Bivens TB, et al. Sympathetic activation during early pregnancy in humans. J Physiol. 2012;590(15):3535–3543. doi:10.1113/jphysiol.2012.228262
19. McEvoy MD, Low PA, Hebbar L. Postural orthostatic tachycardia syndrome: anesthetic implications in the obstetric patient. Anes Analg. 2007;104(1):166–167. doi:10.1213/01.ane.0000246815.39197.2b
20. Pramya N, Puliyathinkal S, Sagili H, et al. Postural orthostatic tachycardia syndrome complicating pregnancy: a case report with review of literature. Obstet Med. 2012;5(2):83–85. doi:10.1258/om.2011.110012
21. Corbett WL, Reiter CM, Schultz JR, et al. Anaesthetic management of a parturient with the postural orthostatic tachycardia syndrome: a case report. Br J Anaesth. 2006;97(2):196–199. doi:10.1093/bja/ael105
22. James CF, Burnett EH. Multiple anesthetic and obstetric challenges in a laboring patient with postural orthostatic tachycardia syndrome (POTS): acquired hemophilia and a rare seizure disorder. Acta Anaesthesiol Belg. 2019;70(2):85–89.
23. Kodakkattil S, Das S. Pregnancy in woman with postural orthostatic tachycardia syndrome (POTS). J Obstet Gynaecol. 2009;29(8):764–765. doi:10.3109/01443610903165529
24. Jones TL, Ng C. Anaesthesia for caesarean section in a patient with Ehlers-Danlos syndrome associated with postural orthostatic tachycardia syndrome. Int J Obstet Anesth. 2008;17(4):365–369. doi:10.1016/j.ijoa.2008.04.003
25. Karthikeyan A, Venkat-Raman N. Hypermobile Ehlers-Danlos syndrome and pregnancy. Obstet Med. 2018;11(3):104–109. doi:10.1177/1753495X18754577
26. Kohn A, Chang C. The relationship between hypermobile Ehlers-Danlos syndrome (hEDS), postural orthostatic tachycardia syndrome (POTS), and mast cell activation syndrome (MCAS). Clin Rev in Allergy Immun. 2020;58(3):273–297. doi:10.1007/s12016-019-08755-8
27. Dorff SR, Afrin LB. Mast cell activation syndrome in pregnancy, delivery, postpartum and lactation: a narrative review. J Obstet Gynaecol. 2020;40(7):889–901. doi:10.1080/01443615.2019.1674259
28. Afrin LB, Dempsey TT, Rosenthal LS, et al. Successful mast-cell-targeted treatment of chronic dyspareunia, vaginitis, and dysfunctional uterine bleeding. J Obstet Gynaecol. 2019;39(5):664–669. doi:10.1080/01443615.2018.1550475
29. Blitshteyn S. Is postural orthostatic tachycardia syndrome (POTS) a central nervous system disorder? J Neurol. 2022;269(2):725–732. doi:10.1007/s00415-021-10502-z
30. Blitshteyn S. Headache in dysautonomia and “long Covid”/PASC. Prac Neurol. 2022;22:35–61.
31. Eigenbrodt AK, Ashina H, Khan S, et al. Diagnosis and management of migraine in ten steps. Nat Rev Neurol. 2021;17(8):501–514. doi:10.1038/s41582-021-00509-5
32. Burch R. Epidemiology and treatment of menstrual migraine and migraine during pregnancy and lactation: a narrative review. Headache. 2020;60(1):200–216. doi:10.1111/head.13665
33. Parikh SK. Unique populations with episodic migraine: pregnant and lactating women. Curr Pain and Headache Rep. 2018;22(12):80. doi:10.1007/s11916-018-0737-x
34. Tanos V, Raad EA, Berry KE, et al. Review of migraine incidence and management in obstetrics and gynaecology. Eur J Obstet Gynecol Reprod Biol. 2019;240:248–255. doi:10.1016/j.ejogrb.2019.07.021
35. Skajaa N, Szépligeti SK, Xue F, et al. Pregnancy, birth, neonatal, and postnatal neurological outcomes after pregnancy with migraine. Headache. 2019;59(6):869–879. doi:10.1111/head.13536
36. Pezaro S, Pearce G, Reinhold E. A clinical update on hypermobile Ehlers-Danlos syndrome during pregnancy, birth and beyond. Br J Midwifery. 2021;29(9):492–500. doi:10.12968/bjom.2021.29.9.492
37. Miller AJ, Stiles LE, Sheehan T, et al. Prevalence of hypermobile Ehlers-Danlos syndrome in postural orthostatic tachycardia syndrome. Auton Neurosci. 2020;224:102637. doi:10.1016/j.autneu.2020.102637
38. Simons E. Pregnancy, childbirth, and postnatal care in EDS and HSD. The Ehlers-Danlos Society; 2022. Available from: https://www.ehlers-danlos.com/pregnancy-childbirth-and-postnatal-care-in-eds-and-hsd/.
39. Schacterle RS, Komaroff AL. A comparison of pregnancies that occur before and after the onset of chronic fatigue syndrome. Arch Intern Med. 2004;164(4):401–404. doi:10.1001/archinte.164.4.401
40. Mavragani CP, Ioannidis JP, Tzioufas AG, et al. Recurrent pregnancy loss and autoantibody profile in autoimmune diseases. Rheumatology. 1999;38(12):1228–1233. doi:10.1093/rheumatology/38.12.1228
41. Nwazue VC, Raj SR. Confounders of vasovagal syncope: postural tachycardia syndrome. Cardiol Clin. 2013;31(1):101–109. doi:10.1016/j.ccl.2012.09.004
42. Chatur S, Islam S, Moore LE, et al. Incidence of syncope during pregnancy: temporal trends and outcomes. J Am Heart Assoc. 2019;8(10):e011608. doi:10.1161/JAHA.118.011608
43. Blitshteyn S. Autoimmune markers and autoimmune disorders in patients with postural tachycardia syndrome (POTS). Lupus. 2015;24(13):1364–1369. doi:10.1177/0961203315587566
44. Schofield JR, Blitshteyn S, Shoenfeld Y, et al. Postural tachycardia syndrome (POTS) and other autonomic disorders in antiphospholipid (Hughes) syndrome (APS). Lupus. 2014;23(7):697–702. doi:10.1177/0961203314524468
45. De Carolis S, Garufi C, Garufi E, et al. Autoimmune congenital heart block: a review of biomarkers and management of pregnancy. Front Pediatr. 2020;8:607515. doi:10.3389/fped.2020.607515
46. Chansakul T, Young GS. Neuroimaging in pregnant women. Semin Neurol. 2017;37(6):712–723. doi:10.1055/s-0037-1608939
47. Garland E, Gamboa A, Nwazue V, et al. Effect of high dietary sodium intake in patients with postural tachycardia syndrome. J Am Coll Cardiol. 2021;77(17):2174–2184. doi:10.1016/j.jacc.2021.03.005
48. Zha K, Brook J, McLaughlin A, Blitshteyn S. Gluten-free diet in postural orthostatic tachycardia syndrome (POTS). Chronic Illn. 2022;174239532210769. doi:10.1177/17423953221076984
49. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77:1246–1255. doi:10.1001/jamapsychiatry.2020.2453
50. Schofield JR, Chemali KR. Intravenous immunoglobulin therapy in refractory autoimmune dysautonomias: a retrospective analysis of 38 patients. Am J Ther. 2019;26(5):570–582. doi:10.1097/MJT.0000000000000778
51. Kesterson K, Schofield J, Blitshteyn S. Immunotherapy with subcutaneous immunoglobulin or plasmapheresis in patients with postural orthostatic tachycardia syndrome (POTS). J Neurol. 2022. doi:10.1007/s00415-022-11344-z
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
