Back to Journals » International Journal of General Medicine » Volume 15
Potential of Omega 3 Supplementation for Coronavirus Disease 2019 (COVID-19): A Scoping Review
Authors Nursyifa Fadiyah N, Megawati G , Erlangga Luftimas D
Received 12 January 2022
Accepted for publication 31 March 2022
Published 11 April 2022 Volume 2022:15 Pages 3915—3922
DOI https://doi.org/10.2147/IJGM.S357460
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nanda Nursyifa Fadiyah,1 Ginna Megawati,2 Dimas Erlangga Luftimas2,3
1Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia; 2Department of Public Health, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia; 3Nutrition Working Group (NWG), SKIP-NAKES Study Center, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
Correspondence: Ginna Megawati, Department of Public Health, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia, Tel +62 81312349351, Email [email protected]
Abstract: COVID-19 can cause fever, cough, headache, and shortness of breath but patients with comorbidities can experience worsening and death. An action is needed to treat this condition in COVID-19 patients. Omega 3 fatty acids may be one possibility associated with COVID-19 prevention, management, and treatment. Therefore, this review aimed to identify the existing studies on potency of omega 3 fatty acid supplementation on COVID-19. We searched studies from PubMed, Google Scholar, Springer Link, and Emerald Insight databases published on January 31, 2020, to September 1, 2021. The studies selected were the full-text, non-review ones which focused on the omega 3 fatty acid intervention in COVID-19 with COVID-19 patients and people affected by COVID-19 as their subjects and clinical manifestations or the results of supporting examinations as their outcomes. No quality assessment was performed in this review. Of the 211, there were 4 studies selected for this review. They showed that severe COVID-19 patients have low levels of omega 3 in their blood. Omega 3 was considered to reduce the risk of positive for SARS-CoV-infection and the duration of symptoms, overcome the renal and respiratory dysfunction, and increase survival rate in COVID-19 patients. Omega 3 fatty acid supplementations were thought to have a potential effect in preventing and treating COVID-19. This can be a reference for further research about omega 3 fatty acid supplementation and COVID-19.
Keywords: COVID-19, omega 3 fatty acid, EPA, DHA, inflammation
Introduction
Coronavirus Disease 2019 (COVID-19) was officially reported for the first time on December 31, 2019.1 It occurs in patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This virus can be transmitted through direct contact with infected people through droplets or indirectly through contaminated objects and airborne.2,3
The most common symptoms were fever, shortness of breath, malaise, anosmia, and headache with bilateral ground-glass opacities on chest CT scan.4–7 Patients with certain conditions, including old age with or without comorbidities such as hypertension, diabetes, obesity and other chronic diseases, or young patients who have comorbidities, tend to have a poor inflammatory response that can lead to worsening.8 Patients with this condition can experience pneumonia, ARDS, pulmonary edema, and multiple organ failure. This can worsen the patient’s condition and require intensive care in the ICU. If not treated properly, it can lead to death in COVID-19 cases.5,9 It becomes a further concern for analyzing various potentials to prevent the deterioration in the condition of the patient and overcome multiple organ failure.
One potential that might be a solution is omega 3 fatty acid supplementation. Omega 3 is one type of long-chain polyunsaturated fatty acid (LCPUFA) which is classified as an essential fatty acid. It consists of eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA).10 Because it is an essential fatty acid, omega 3 can only be obtained from food sources, such as canola oil, seeds, green vegetables, and nuts containing ALA and marine fish and fish oil that consume microalgae containing EPA and DHA. Besides, omega 3 can be obtained from supplements.11 Omega 3 fatty acids have many health benefits. EPA and DHA are important components that play a role in modulating immune function and regulating the inflammatory response.12,13 Its involvement in regulating inflammation has been shown to provide various benefits, including lowering the risk of cardiovascular disease, reducing the risk of cancer, reducing symptoms of metabolic syndrome, and treating rheumatoid arthritis, Crohn’s disease, ulcerative colitis, and other diseases caused by inflammation.14–16 A narrative review from several studies had shown that EPA and DHA-derived mediators such as resolvin, protectin, and lipoxin act as specialized proresolving mediators (SPM) that can regulate the inflammatory process that occurs due to infection.17
Several studies have stated that one of the markers of worsening in COVID-19 is the increased production of inflammatory mediators, especially interleukin-6 (IL-6).18–20 Panigrahy et al considered that omega 3 fatty acids, through SPM, could regulate inflammation in COVID-19 by increasing phagocytosis of viruses and debris by macrophages, suppressing the production of eicosanoids, proinflammatory cytokines, and leukocyte infiltration, and increasing the production of anti-SARS-CoV-2 antibodies.21
There was a systematic narrative review study on anti-inflammatory diet that was effective in preventing or treating viral respiratory disease. Omega 3 fatty acids were included in the food items in the review besides turmeric, ginger, garlic, onion, saffron, vitamin C, vitamin D, and zinc. However, the review was more general in viral respiratory disease and is not specific to COVID-19.17 Omega 3 fatty acid is thought to be a potential solution in COVID-19 treatment. Therefore, this scoping review aimed to identify the various studies that have been done on the effects of omega 3 supplementation in COVID-19 and identify gaps and opportunities for further research.
Materials and Methods
Search Strategy
Our review focused on identifying the studies on the potential for omega 3 fatty acid supplementation in COVID-19, key concepts, gaps in existing studies, and the types and sources of evidence to inform the studies presented in a scoping review. The stages of the framework for this scoping review were adapted from Arksey and O’Malley: (1) identifying the research question, (2) identifying relevant studies, (3) study selection, (4) charting the data, and (5) collating, summarising, and reporting the results.22
Our scoping review followed the Preferred Reporting Items for Systematic Review and Meta-Analyses extension (PRISMA).23,24 The process consisted of article searching, screening duplicate articles and adjusting to titles and abstracts, assessing the eligibility of screened full-text articles based on inclusion and exclusion criteria, and reviewing articles that have been included.
Search strategy was done from June 28 to September 1, 2021. The reference used in this review were obtained through article searching process on four databases: PubMed, Google Scholar, Emerald Insight, and Springer Link. The keywords used were (omega 3 fatty acids) AND (inflammation) AND (COVID-19) and we used other words from key terms by using OR. Other key terms for “omega 3 fatty acids” were (n 3 Oil) OR (n-3 Fatty Acids) OR (n 3 PUFA) OR (n 3 Fatty Acid) OR (n-3 Polyunsaturated Fatty Acid). Other key terms for “inflammation” were (Inflammations) OR (Innate Inflammatory Response) OR (Innate Inflammatory Responses). Other key terms for “COVID-19” were (COVID 19) OR (COVID-19 Virus Disease) OR (COVID-19 Virus Infection) OR (COVID-19 Virus Infections) OR (2019-nCoV Infection) OR (Coronavirus Disease 19) OR (2019 Novel Coronavirus Disease) OR (2019 Novel Coronavirus Infection) OR (Coronavirus Disease 2019) OR (SARS Coronavirus 2 Infection) OR (SARS-CoV-2 Infection) OR (COVID-19 Pandemic).
Inclusion and Exclusion Criteria
The searching process used specific clinical questions with reference to population, concept, and context (PCC). In this review, the population was people affected by the COVID-19 pandemic, especially COVID-19 patients; the concept was the omega 3 fatty acid intervention in COVID-19; and the context was the patient’s condition during the COVID-19 pandemic, based on the clinical manifestations and the results of supporting examinations.
The studies were included in our review if they met the following eligibility criteria: (1) full-text articles published from January 31, 2020 to September 1, 2021, (2) article was not a review, (3) available in English or Indonesian language, (4) their subjects were COVID-19 patients and people affected by COVID-19, (5) focused on the omega 3 fatty acid intervention in COVID-19, and (6) their outcomes were clinical manifestations or the results of supporting examinations.
Data Extraction
In this review, eligible papers were extracted to identify the author, year of publication, country of origin, type of study design, population, purpose, omega 3 supplement supplementation and dose, as well as important findings. No quality assessment and critical appraisal was performed in this review.
Results
Search Outcome
The study selection based on the PRISMA flowchart is presented in Figure 1. In the initial search with the keywords (omega 3 fatty acids) AND (inflammation) AND (COVID-19) and several other key terms, there were 211 studies: 42 studies from PubMed, 52 studies from Springer Link, 3 studies from Emerald Insight, and 114 studies from Google Scholar. After screening for duplicate studies, 30 studies were excluded. We continued screening 181 studies by observing their title and abstract. In this stage, we excluded 140 studies because they did not fit the research question. 41 full-text studies were reviewed by assessing their eligibility. 37 studies were excluded because they were review articles, editorial material, letters to editors, the study population was not COVID-19 patients, did not include omega 3 fatty acid data, and their outcomes were neither clinical manifestation nor the result of supporting examinations. At the final stage, we included 4 studies that met the eligibility criteria for our scoping review.
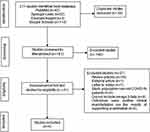 |
Figure 1 Flow diagram of literature searching and screening process. |
Characteristic of the Studies
The characteristics of the studies included in this review are reported in Table 1. All studies included were published between 2020 and 2021, with 75% (3/4) published in 2021. The countries of origin of the research consisted of Iran, the United States of America, United Kingdom, Sweden, and Chile.25–28
 |
Table 1 The Characteristics of the Studies Included |
Study designs of four articles included in this review were randomized controlled trial, case report, cross-sectional study, and app-based community survey. In general, the focus of the studies included was to analyze the relationship of omega 3 fatty acids with COVID-19.25–27 An article provided an overview of omega 3 fatty acid levels and clinical outcomes of patients with severe COVID-19.28
Most of the population were COVID-19 patients.25,26,28 The study population Louca et al were subscribers of the COVID-19 Symptom Study application who performed self-reports regarding identity, COVID-19 symptoms, healthcare visits, SARS-CoV-2 test results using RT-PCR or serological tests, age, gender, body mass index (BMI), smoking habit, ethnicity, status of health workers and the presence of comorbidities (cancer, diabetes, eczema, heart disease, lung disease, kidney disease and hay fever), and supplements that were routinely taken during the last 3 months.27
Potential of Omega 3 Supplementation for COVID-19
Summary of the included studies are showed in Table 2. Three articles involved giving oral omega 3 supplements with various doses and frequencies and evaluating their effect on COVID-19.25–27 Meanwhile, an article by Zapata et al described omega 3 index and clinical outcome of severe COVID-19 patients.28
 |
Table 2 Summary of the Included Studies |
The results presented in the studies showed that there was a relationship between omega 3 fatty acids and COVID-19. Patients with severe COVID-19 had the low omega 3 index levels.28 However, as described by Louca et al that people who took omega 3 fatty acid supplements more than 3 times a week for at least 3 months had a 12% lower risk of SARS-CoV-2 infection.27 Besides, it was demonstrated that patients who consumed omega 3 supplement had higher levels of parameters of respiratory and renal function and shorter symptom duration compared to those who did not consume them.25,26
Discussion
Omega 3 Fatty Acids and Reducing Risk of SARS-CoV-2 Infection
Omega 3 fatty acids were thought to have potential in reducing the risk of SARS-CoV-2 infection. Based on study by Louca et al, users of the COVID-19 Symptom Study app who reported taking omega 3 fatty acid supplements more than 3 times a week for at least 3 had a 12% lower risk of getting a positive result of SARS-CoV-2 infection in the UK, 21% in the United States, and 16% in Sweden.27 This is considered to be related to the mechanism of omega 3 fatty acids in suppressing and inhibiting the progress of viral infections. Supporting this study, Morita et al reported that protectin D1, DHA-derived mediators are thought to inhibit viral RNA replication, one of which is influenza virus.29 However, another study concluded that the effect of omega 3 fatty acid supplementation on infection depends on the pathogen, dose and frequency of supplementation.30 Therefore, research on the potential of omega 3 fatty acids against SARS-CoV-2 infection along with its exact dose needs to be tested further.
Omega 3 Fatty Acid and Accelerating Symptom Days
Berger et al in their case report showed that the consumption of Icosapent Ethyl (IPE) 2g twice daily can have an impact on accelerating the symptoms duration in COVID-19 patients. IPE is an omega 3 fatty acid derivative containing EPA ethyl ester which is given to hypertriglyceridemia patients and has been shown to reduce cardiovascular risk with treatment targeted at inflammation.31 Among the two COVID-19 patients with the same background, the patient who took IPE 2g twice daily experienced a shorter symptom day than the one who did not.26 Omega 3 fatty acids had been reported to modulate immunity and activate inflammatory resolution processes.32,33 It was through eicosanoids derived from omega 3 fatty acids EPA and DHA such as resolvin, maresin, lipoxin, and protectin, which could inhibit the synthesis of pro-inflammatory cytokines through downregulation of the NFkB pathway, inhibit leukocyte infiltration to the site of inflammation, and stimulate macrophages and neutrophils to resolve inflammation so that it did not lead to a longer duration of symptoms.34,35 The short duration of symptoms in patients taking IPE was thought to be affected by the regulation of inflammation and modulation of immunity by omega 3 fatty acids. This finding could be a reference for further research to determine the right dose of omega 3 fatty acids on the effect of regulating inflammation and immunity in COVID-19.
Omega 3 Fatty Acid and Overcoming the Deterioration of Health
Patients with severe COVID-19 generally have a more severe inflammatory response accompanied by worsening manifestations, such as ARDS, metabolic disorders, sepsis, septic shock, heart failure, acute myocardium, acute kidney damage, multiple organ failure, etc.5,36
Severe COVID-19 patients may experience metabolic acidosis and respiratory acidosis.37–39 They can occur due to dysregulation of the inflammatory response that causes multiorgan failure, respiratory failure, and hypoxia resulting in increased production of lactic acid as a result of anaerobic metabolism.40,41 In critical conditions, SARS-CoV-2 infection was thought to cause kidney dysfunction. This results in decreased bicarbonate reabsorption and impaired pH regulation by the kidneys and causes acidosis.42–44
Doaei et al reported that critically ill COVID-19 patients who took 1000 mg of omega 3 fatty acids enterally every day for 14 days showed higher arterial pH, HCO3, and Be levels and lower BUN, Cr, and K than the control group. Omega 3 fatty acids were reported to improve endothelial function and microcirculation and optimize blood flow and tissue perfusion to prevent the progression of hypoxia and organ dysfunction.25 They have a role in increasing blood flow to tissues and microvascular function by increasing vasodilation mechanisms, increasing endothelial relaxation, and decreasing the vasoconstrictive response.45 Here, omega 3 may prevent the renal and respiratory impairment manifested by higher level of pH, HCO3, and Be and lower level of BUN, Cr, and K than the control group. Besides, this study showed that patients with omega 3 supplementation had a higher one-month survival rate compared to those who did not consume omega 3 fatty acids.25 It was supported by several studies reporting that omega 3 fatty acids can reduce mortality rates in critically ill patients.46,47 However, another study concluded that the evidence for omega 3 benefits in the survival of hospitalized critically ill patients is still weak.13
Cross-sectional study by Zapata et al supported previous evidence and reported that patients with severe COVID-19 had a low omega 3 index, consistent with a lower intake of fish and omega 3 supplements. Higher O3I reduced risk of mechanical ventilation and risk of death; this relationship became significant after adjusting for age and sex and remained significant when adjusted for other factors.28 Omega 3 index is the EPA and DHA content of red blood cells expressed as a percentage of the total weight of fatty acids in red blood cell membranes.48 Short-term fish oil supplementation with high doses can increase O3I.49
Conclusion
The existing studies considered that omega 3 fatty acid has potential in COVID-19 by reducing the risk of positive SARS-CoV-2 infection, speeding up the duration of symptoms, decreasing the risk of renal and respiratory dysfunction, and increasing patient survival rate.
Acknowledgments
This review was conducted at the Faculty of Medicine, Universitas Padjadjaran. The authors would like to thank Lika Apriani, Dr., M.Sc. PhD, and Dr. Siti Nur Fatimah, Dr. MS., SpGK for their help. We also thank the Faculty of Medicine, Universitas Padjadjaran for their support.
Disclosure
The authors report that there they have no conflicts of interest for this work.
References
1. Di Gennaro F, Pizzol D, Marotta C, et al. Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int J Environ Res Public Health. 2020;17(8):2690. doi:10.3390/ijerph17082690
2. Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508(April):254–266. doi:10.1016/j.cca.2020.05.044
3. Morawska L, Tang JW, Bahnfleth W, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020;142(April):105832. doi:10.1016/j.envint.2020.105832
4. Du Y, Tu L, Zhu P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med. 2020;201(11):1372–1379. doi:10.1164/rccm.202003-0543OC
5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
6. Hassan SA, Sheikh FN, Jamal S, Ezeh JK, Akhtar A. Coronavirus (COVID-19): a review of clinical features, diagnosis, and treatment. Cureus. 2020;977(3):2–6. doi:10.7759/cureus.7355
7. Vetter P, Vu DL, L’Huillier AG, Schibler M, Kaiser L, Jacquerioz F. Clinical features of covid-19. BMJ. 2020;369(April):1–2. doi:10.1136/bmj.m1470
8. Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20(6):363–374. doi:10.1038/s41577-020-0311-8
9. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
10. Shahidi F, Ambigaipalan P. 37 The annual review of food science and technology is online at food. Annu Rev Food Sci Technol. 2018;9(January):16–17. doi:10.1146/annurev-food-111317-
11. Vonshak A. Recent advances in microalgal biotechnology. Biotechnol Adv. 1990;8(4):709–727. doi:10.1016/0734-9750(90
12. Norris PC, Skulas-Ray AC, Riley I, et al. Identification of specialized pro-resolving mediator clusters from healthy adults after intravenous low-dose endotoxin and omega-3 supplementation: a methodological validation. Sci Rep. 2018;8(1):1–13. doi:10.1038/s41598-018-36679-4
13. Koekkoek W, Panteleon V, van Zanten AR. Current evidence on ω-3 fatty acids in enteral nutrition in the critically ill: a systematic review and meta-analysis. Nutrition. 2019;59:56–68. doi:10.1016/j.nut.2018.07.013
14. Rogero MM, Calder PC. Obesity, inflammation, toll-like receptor 4 and fatty acids. Nutrients. 2018;10(4):1–19. doi:10.3390/nu10040432
15. Manson JE, Cook NR, Lee I-M, et al. Marine n−3 fatty acids and prevention of cardiovascular disease and cancer. N Engl J Med. 2019;380(1):23–32. doi:10.1056/nejmoa1811403
16. Swanson D, Block R, Mousa SA. Omega-3 fatty acids EPA and DHA: health benefits throughout life. Adv Nutr. 2012;3(1):1–7. doi:10.3945/an.111.000893
17. Vahid F, Rahmani D. Can an anti-inflammatory diet be effective in preventing or treating viral respiratory diseases? A systematic narrative review. Clin Nutr ESPEN. 2021;43:9–15. doi:10.1016/j.clnesp.2021.04.009
18. Petrey AC, Qeadan F, Middleton EA, Pinchuk IV, Campbell RA, Beswick EJ. Cytokine release syndrome in COVID-19: innate immune, vascular, and platelet pathogenic factors differ in severity of disease and sex. J Leukoc Biol. 2021;109(1):55–66. doi:10.1002/JLB.3COVA0820-410RRR
19. Gorham J, Moreau A, Corazza F, et al. Interleukine-6 in critically ill COVID-19 patients: a retrospective analysis. PLoS One. 2020;15(12 12):1–11. doi:10.1371/journal.pone.0244628
20. Santa Cruz A, Mendes-Frias A, Oliveira AI, et al. Interleukin-6 is a biomarker for the development of fatal severe acute respiratory syndrome coronavirus 2 Pneumonia. Front Immunol. 2021;12(February):1–10. doi:10.3389/fimmu.2021.613422
21. Panigrahy D, Gilligan MM, Huang S, et al. Inflammation resolution: a dual-pronged approach to averting cytokine storms in COVID-19? Cancer Metastasis Rev. 2020;39(2):337–340. doi:10.1007/s10555-020-09889-4
22. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi:10.1080/1364557032000119616
23. Title ST. Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews (PRISMA-ScR) checklist. Ann Intern Med. 2018;169:11–12. doi:10.7326/M18-0850.2
24. Pham MT, Rajić A, Greig,JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5. doi:10.1002/jrsm.1123
25. Doaei S, Gholami S, Rastgoo S, Gholamalizadeh M, Bourbour F. The effect of omega ‑ 3 fatty acid supplementation on clinical and biochemical parameters of critically ill patients with COVID ‑ 19: a randomized clinical trial. J Transl Med. 2021;1–9. doi:10.1186/s12967-021-02795-5
26. Berger AA, Sherburne R, Urits I, Patel H, Eskander J. Icosapent Ethyl – a successful treatment for symptomatic COVID-19 infection. Cureus. 2020;12(9):12–15. doi:10.7759/cureus.10211
27. Louca P, Murray B, Klaser K, et al. Modest effects of dietary supplements during the COVID-19 pandemic: insights from 445 850 users of the COVID-19 symptom Study app. BMJ Nutr Prev Health. 2021:1–9. doi:10.1136/bmjnph-2021-000250
28. Zapata BR, Müller M, Enrique J, et al. Omega-3 index and clinical outcomes of severe COVID-19: preliminary results of a cross-sectional study. Int J Environ Res Public Health. 2021;18:13–15.
29. Morita M, Kuba K, Ichikawa A, et al. The lipid mediator protectin D1 inhibits influenza virus replication and improves severe influenza. Cell. 2013;153(1):112–125. doi:10.1016/j.cell.2013.02.027
30. Husson M-O, Ley D, Portal C, et al. Modulation of host defence against bacterial and viral infections by omega-3 polyunsaturated fatty acids. J Infect. 2016;73(6):523–535. doi:10.1016/j.jinf.2016.10.001
31. Bhatt DL, Steg PG, Miller M, et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380(1):11–22. doi:10.1056/nejmoa1812792
32. Calder PC. Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology? Br J Clin Pharmacol. 2013;75(3):645–662. doi:10.1111/j.1365-2125.2012.04374.x
33. Ortega-Gómez A, Perretti M, Soehnlein O. Resolution of inflammation: an integrated view. EMBO Mol Med. 2013;5(5):661–674. doi:10.1002/emmm.201202382
34. Basil MC, Levy BD. Specialized pro-resolving mediators: endogenous regulators of infection and inflammation. Nat Rev Immunol. 2016;16(1):51–67. doi:10.1038/nri.2015.4
35. Krishnamoorthy N, Abdulnour REE, Walker KH, Engstrom BD, Levy BD. Specialized proresolving mediators in innate and adaptive immune responses in airway diseases. Physiol Rev. 2018;98(3):1335–1370. doi:10.1152/physrev.00026.2017
36. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
37. Chhetri S, Khamis F, Pandak N, Al Khalili H, Said E, Petersen E. A fatal case of COVID-19 due to metabolic acidosis following dysregulate inflammatory response (cytokine storm). IDCases. 2020;21:e00829. doi:10.1016/j.idcr.2020.e00829
38. Behzad S, Aghaghazvini L, Radmard AR, Gholamrezanezhad A. Extrapulmonary manifestations of COVID-19: radiologic and clinical overview. Clin Imaging. 2020;66:35–41. doi:10.1016/j.clinimag.2020.05.013
39. Shevel E. Conditions favoring increased COVID-19 morbidity and mortality: their common denominator and treatment. Isr Med Assoc J. 2020;22(11):680.
40. Nechipurenko YD, Semyonov DA, Lavrinenko IA, et al. The role of acidosis in the pathogenesis of severe forms of COVID-19. Biology. 2021;10(9). doi:10.3390/biology10090852
41. Wan-hui L, Gee-gwo Y, De HM. The renin-angiotensin-aldosterone system inhibitors in COVID-19: from acidosis to ventilation and immunity. Swiss Med Weekly. 2020;(December):1–7. doi:10.4414/smw.2020.20444
42. Kunutsor SK, Laukkanen JA. Renal complications in COVID-19: a systematic review and meta-analysis. Ann Med. 2020;52(7):345–353. doi:10.1080/07853890.2020.1790643
43. Nogueira SÁR, de Oliveira SCS, de Carvalho AFM, et al. Renal changes and acute kidney injury in COVID-19: a systematic review. Rev Assoc Med Bras. 2020;66(Suppl 2):112–117. doi:10.1590/1806-9282.66.S2.112
44. Liu YF, Zhang Z, Pan XL, et al. The chronic kidney disease and acute kidney injury involvement in COVID-19 pandemic: a systematic review and meta-analysis. PLoS One. 2021;16(1 January):1–13. doi:10.1371/journal.pone.0244779
45. Mori TA, Watts GF, Burke V, Hilme E, Puddey IB, Beilin LJ. Differential effects of eicosapentaenoic acid and docosahexaenoic acid on vascular reactivity of the forearm microcirculation in hyperlipidemic, overweight men. Circulation. 2000;102(11):1264–1269. doi:10.1161/01.CIR.102.11.1264
46. Mozaffarian D, Lemaitre RN, King IB, et al. Plasma phospholipid long-chain Omega-3 fatty acids and total and cause-specific mortality in older adults: the cardiovascular health study. Ann Intern Med. 2013;158(7):515–525. doi:10.7326/0003-4819-158-7-201304020-00003.Plasma
47. Eide IA, Jenssen T, Hartmann A, et al. The association between marine n-3 polyunsaturated fatty acid levels and survival after renal transplantation. Clin J Am Soc Nephrol. 2015;10(7):1246–1256. doi:10.2215/CJN.11931214
48. Walker RE, Jackson KH, Tintle NL, et al. Predicting the effects of supplemental EPA and DHA on the omega-3 index. Am J Clin Nutr. 2019;110(4):1034–1040. doi:10.1093/ajcn/nqz161
49. Drudi LM, Schaller MS, Hiramoto J, et al. Predictors of change in omega-3 index with fish oil supplementation in peripheral artery disease. J Surg Res. 2017;210:124–131. doi:10.1016/j.jss.2016.11.011
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
