Back to Journals » International Medical Case Reports Journal » Volume 10
Potential for severe airway obstruction from pediatric retropharyngeal abscess
Authors LeRiger MM, Miler V, Tobias JD , Raman VT , Elmaraghy CA, Jatana KR
Received 18 July 2017
Accepted for publication 10 October 2017
Published 23 November 2017 Volume 2017:10 Pages 381—384
DOI https://doi.org/10.2147/IMCRJ.S146661
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Michelle M LeRiger,1,2 Veronica Miler,3 Joseph D Tobias,3 Vidya T Raman,3 Charles A Elmaraghy,4,5 Kris R Jatana4,5
1Division of Pediatric Anesthesiology, Omaha Children’s Hospital & Medical Center, 2Department of Anesthesiology, University of Nebraska Medical Center, Omaha, NE, 3Department of Anesthesiology and Pain Medicine, 4Department of Pediatric Otolaryngology-Head & Neck Surgery, Nationwide Children’s Hospital, 5Department of Otolaryngology-Head and Neck Surgery, Wexner Medical Center at Ohio State University, Columbus, OH, USA
Abstract: Retropharyngeal abscesses in the pediatric population can cause severe respiratory distress. We report a rare case of significant airway obstruction in a 14-month-old patient requiring rapid, emergent tracheotomy after attempts at endotracheal intubation by an experienced airway surgeon were unsuccessful. The patient was diagnosed with streptococcal pharyngitis 9 days prior to presentation to our facility and was being treated with amoxicillin. Prompt diagnosis, communication, and appropriate multidisciplinary airway management can lead to successful outcomes even in these severe cases.
Keywords: pharyngitis, retropharyngeal abscess, emergent tracheotomy, pediatric airway obstruction, respiratory distress
Introduction
Retropharyngeal abscesses (RPAs) are deep neck space infections that have the potential to deteriorate into life-threatening airway obstruction. The peak incidence occurs between 3 and 5 years of age, before the lymph nodes in this potential space atrophy, making abscess formation much less common with age. Abscess formation is an infrequent complication of an upper respiratory tract infection, resulting from suppuration of the retropharyngeal lymph nodes, which drain the nasopharynx and oropharynx.
The retropharyngeal space is a potential space located posterior to the pharynx, larynx, and trachea. It extends superiorly from the base of the skull and inferiorly to the bifurcation of the trachea in the mediastinum. The space is bound anteriorly by the buccopharyngeal fascia, laterally by the carotid sheaths and parapharyngeal spaces, and posteriorly by the alar fascia of the deep cervical fascia. The space is fused down the midline and contains two chains of lymph nodes extending down each side. The nodes in these deep neck spaces communicate, allowing bacteria to spread to other nodes. Once infected, the nodes may progress through three progressive stages: cellulitis, phlegmon, and abscess.
Complications of RPA can result from a mass effect and compression of adjacent structures, notability the larynx and trachea. With airway compression, it is critical to have a skilled and experienced multidisciplinary team managing these children to achieve optimal outcomes. We present a 14-month-old with a recent history of streptococcal pharyngitis who subsequently developed a large RPA causing severe acute airway compromise necessitating emergent tracheostomy. Both institutional review board approval and consent from parent/legal guardian were obtained for purposes of publication.
Case presentation
A 14-month-old, 8-kg, routinely vaccinated male was transferred to a tertiary care pediatric medical center with concerns for respiratory distress. He had a 1-week history of fever, decreased neck mobility, and decreased oral intake. The patient was diagnosed with streptococcal pharyngitis 9 days prior, and he was being treated with a course of amoxicillin. Due to worsening symptoms, his parents brought him to the nearest hospital where a lateral neck film showed a large amount of retropharyngeal thickening and airway displacement (Figure 1). His white blood cell count was elevated at 33,000/mm3. He was transported by helicopter to our institution for further management. Physical examination revealed an alert child with a muffled voice. Vitals sign consisted of a respiratory rate of 25 breaths/minute, heart rate of 161 beats/minute, and temperature of 37.3°C. He was maintaining oxygen saturations of 100% on room air. Oropharyngeal examination showed significant bulging of the posterior pharynx. Further imaging was delayed until the airway was secured.
  | Figure 1 Lateral neck X-ray demonstrating significant retropharyngeal thickening with anterior displacement of airway. |
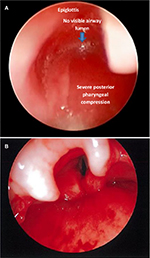
The necessary airway equipment as well as surgical instruments for tracheotomy was set up prior to the patient entering the operating room. In an attempt to keep the child calm and to avoid any unnecessary manipulation of the airway, he was transported to the operating room in his mother’s arms. Anesthesia was induced by slow, controlled inhalation of sevoflurane in nitrous oxide and oxygen with the goal of maintaining spontaneous ventilation. After ensuring an adequate depth of anesthesia and properly positioning the patient, the pediatric otolaryngology team proceeded with direct laryngoscopy. The epiglottis could be visualized, but the posterior larynx was compressed anteriorly in such a way that the vocal cords could not even be seen (Figure 2A). Attempts at placing an endotracheal tube with a stylet as well as the rigid ventilating bronchoscope through the larynx were unsuccessful. Air exchange ceased, and bag-valve-mask ventilation was not possible. There was significant upper airway obstruction from mass effect alone (never a visible lumen), and this was not believed to be due to laryngospasm. The oxygen saturation began to decline rapidly, and the decision was made to proceed with emergent tracheotomy tube placement. A vertical skin incision followed by vertical tracheotomy was performed with a scalpel, and the airway was established within 15 seconds. Oxygen saturations quickly normalized, hemostasis was achieved, and the tracheostomy tube was secured. The posterior pharyngeal bulge was very tense, and an incision and drainage was performed with the drainage of approximately 100 mL of purulent fluid. Immediately following the drainage, a grade I view of the larynx was obtained (Figure 2B). The patient was transferred to the pediatric intensive care unit in stable condition. Postoperative computed tomography scan showed there was no mediastinal component that needed further intervention. Cultures of the abscess grew beta-hemolytic streptococcus group A. Serial bedside laryngoscopy was done to confirm that there was no re-accumulation of the abscess and improvement of pharyngeal edema before initiating tracheostomy decannulation process. The tracheostomy tube was removed on postoperative day 6, and 2 weeks later the stoma was fully healed.
Discussion
The diagnosis of pediatric RPA can be difficult given a variety of nonspecific signs or symptoms including neck pain, neck stiffness, decreased oral intake, drooling, odynophagia, irritability, fever, malaise, pharyngeal swelling, and possibly external neck swelling. In a series of 73 patients, no airway symptoms were seen while awake; however, several patients had new or increased obstructive symptoms when asleep, so close monitoring is necessary.1 Signs suggesting airway compromise can include a muffled voice, stridor, respiratory distress, and obstructive sleep apnea. Dudas and Serwint stated that respiratory distress or stridor occurs less frequently than commonly believed and that most patients presenting with RPA do not necessarily have a “toxic” appearance.2 A retrospective study from Sydney Children’s Hospital reported that respiratory compromise or drooling was present in 29% of children with RPA.3 In our case, given the degree of obstruction noted intraoperatively, it was surprising that our patient did not have more severe clinical symptoms. The lack of overt airway compromise may provide a false sense of security concerning the patency of the airway. In circumstances where the airway is considered critical, the practitioner should not delay definitive management for further imaging studies. It is imperative that a surgeon experienced in pediatric airway management is directly involved in the care of these children.
In current medical practices, tracheotomy and short-term intubation (24–72 hours) are rarely required for the management of pediatric RPA. In a survey of the American Society of Pediatric Otolaryngology, a majority of surgeons reported that in their experience “a tracheotomy had never been required” for a pediatric RPA.4 Several studies have reviewed pediatric RPA, but there has been little need for tracheostomy in these series. A retrospective study from Sydney Children’s Hospital of 21 children with RPA over a 12-year time span reported that 17 of 21 patients required surgical drainage. Ten patients required endotracheal intubation postoperatively for a mean duration of 4.45 days. This series reports only one patient requiring a tracheostomy, but did not specifically mention whether it was elective or emergent.3 Montreal Children’s Hospital performed a retrospective study of pediatric RPA spanning from 1990 to 1999. In this series, 17 (25%) of 68 patients required surgical drainage. Two patients were admitted to the ICU for airway monitoring. One patient required 3 days of endotracheal intubation following the surgical procedure until the airway edema had subsided. No patients required a tracheotomy.5 Another series from Toronto included 46 retropharyngeal infections, and none required tracheotomy.6
A study from Boston Children’s Hospital reviewed 73 patients with pediatric RPA from 1989 to 1998. The presenting symptoms varied, with the most common including fever, decreased oral intake, drooling, odynophagia, malaise, and torticollis. Other symptoms included neck pain, trismus, otalgia, headache, neck swelling, and change in voice quality. Four patients had worsening of snoring or frank obstructive sleep apnea, but no patient had respiratory compromise while awake. Eighteen patients had endotracheal intubation postoperatively for an average of 1–2 days, but there was no mention of any patient requiring a tracheotomy.1 In a retrospective study from New Zealand, surgical incision and drainage was carried out in 10 of the 24 (41.6%) retropharyngeal infections. There was no mention of tracheostomy being performed in any of their patients.7
The role of medical versus surgical treatment for these infections continues to be debated. The mainstay of treatment for pediatric RPA for more than 100 years has been surgical incision and drainage. However, recent published pediatric reviews suggest that only 25–50% of patients require surgery.2 It has been proposed by some that all patients should be treated with intravenous antibiotics and that surgery be reserved for those who do not respond.1 However, it is difficult to be completely certain whether cases treated successfully with antibiotics were actually abscesses and not just cellulitis. Because the morbidity of transoral drainage is very low, it is common practice to proceed with surgical incision and drainage when a computed tomography scan suggests that a well-defined abscess is present. It is clear, however, that if any signs of airway obstruction are present, it is necessary to proceed with securing the airway and surgical drainage. Centers with a multidisciplinary team, consisting of an experienced pediatric anesthesiologist and surgical specialist in airway management, are critical to successful outcomes in these patients.
Conclusion
As seen from our case, complete airway obstruction can occur rapidly, necessitating emergent tracheotomy. Prompt diagnosis and early treatment is imperative to prevent such complications. Involvement of experienced pediatric anesthesiologists and surgeons trained in pediatric airway management, including emergent tracheotomy, is critical for optimal outcomes in severe cases. Because RPA can present with similar signs and symptoms as other upper airway infections, pediatric clinicians must always keep it in their differential diagnosis. Even in patients with no obvious airway distress, great care should be exercised before deciding to delay treatment and perform imaging studies. Management of this condition should occur in pediatric institutions with appropriate medical, surgical, and intensive care facilities.
Disclosure
The authors report no conflicts of interest in this work.
References
Kirse DJ, Roberson DW. Surgical management of retropharyngeal space infections in children. Laryngoscope. 2001;111(8):1413–1422. | ||
Dudas R, Serwint JR. In brief: retropharyngeal abscess. Pediatr Rev. 2006;27(6):e45–e46. | ||
Dawes LC, Bova R, Carter P. Retropharyngeal abscess in children. ANZ J Surg. 2002;72(6):417–420. | ||
Lalakea MI, Messner AH. Retropharyngeal abscess management in children: current practices. Otolaryngol Head Neck Surg. 1999;121(4):398–405. | ||
Al-Sabah B, Bin Salleen H, Hagr A, Choi-Rosen J, Manoukian JJ, Tewfik TL. Retropharyngeal abscess in children: 10-year study. J Otolaryngol. 2004;33(6):352–355. | ||
Daya H, Lo S, Papsin BC, et al. Retropharyngeal and parapharyngeal infections in children: the Toronto experience. Int J Pediatr Otorhinolaryngol. 2005;69(1):81–86. | ||
Courtney MJ, Mahadevan M, Miteff A. Management of paediatric retropharyngeal infections: non-surgical versus surgical. ANZ J Surg. 2007;77(11):985–987. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.