Back to Journals » OncoTargets and Therapy » Volume 9
Postoperative radiotherapy and tumor recurrence after complete resection of stage II/III thymic tumor: a meta-analysis of cohort studies
Authors MA J, Sun X, HUANG L, XIONG Z, Yuan M, Zhang S , Han C
Received 17 January 2016
Accepted for publication 9 May 2016
Published 22 July 2016 Volume 2016:9 Pages 4517—4526
DOI https://doi.org/10.2147/OTT.S104435
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr William C. Cho
Jietao Ma, Xin Sun, Letian Huang, Zhicheng Xiong, Meng Yuan, Shuling Zhang, Cheng-Bo Han
Department of Oncology, Shengjing Hospital of China Medical University, Shenyang, People’s Republic of China
Background: Whether postoperative radiotherapy (PORT) is effective for reducing the recurrence risk in patients who received complete resection of the stage II or III thymic tumors has not been determined. A meta-analysis was performed by combining the results of all available controlled trials.
Methods: PubMed, Cochrane’s Library, and the Embase databases were searched for studies which compared the recurrence data for patients with complete resection of the stage II or III thymic tumors assigned to an observing group, or a PORT group. A random effect model was applied to combine the results.
Results: Nineteen studies, all designed as retrospective cohort studies were included. These studies included 663 patients of PORT group and 617 patients of observing group. The recurrence rate for the patients in PORT group and observing group were 12.4% and 11.5%, respectively. Results of our study indicated that PORT has no significant influence on recurrent risk in patients with stage II or III thymic tumor after complete resection (odds ratio 1.02, 95% confidence interval 0.55–1.90, P=0.96). When stratified by stages, our meta-analyses did not indicate any significant effects of PORT on recurrent outcomes in either the stage II or the stage III patients. Moreover, subsequent analysis limited to studies only including patients with thymoma or thymic carcinoma also did not support the benefits of PORT on recurrent outcomes.
Conclusion: Although derived from retrospective cohort studies, current evidence did not support any benefit of PORT on recurrent risk in patients with complete resection of the stage II or III thymic tumors.
Keywords: thymic tumor, postoperative radiotherapy, recurrence, meta-analysis
Background
Although the thymic tumors are rare clinically, they are the most common tumor of the anterior mediastinum.1–3 The treatment strategies to the thymic tumor are generally determined based on the stages of the tumor.2,4 The most accepted staging method for thymic tumor is the Masaoka stage system, which was proposed in 1981.5 This staging system takes account of the factors regarding both the local extension and the histologic characteristics of the tumors.4,6 Typically, stage I thymic tumor refers to the encapsulated lesions, and the complete resection to the patients with the stage I tumor is generally recommended, with rare postprocedure recurrence. A stage IV thymic tumor refers to the lymphogenous or hematogenous metastases of the tumor, and multimodality therapy including surgery, radiotherapy, and chemotherapy is recommended. If the tumor invades through the capsule and extend into the surrounding fat tissue within the mediastinum, either grossly or microscopically, it could be classified as stage II tumors. If the tumor has invaded into the neighboring organs, for example, pericardium, great vessels, and lung tissues, a stage III thymic tumor should be defined. Although complete resection of the tumor is preferred for patients with stage II or III thymic tumor, the recurrent risk even for these patients who received complete resection of the tumors is higher than for those with stage I tumors.7 In view of the relatively higher recurrence of the stage II or III thymic tumor after complete resection, as well as the sensitivity of the tumors to the radiotherapy,8 a postoperative radiotherapy (PORT) has been proposed as a preventative measure for the recurrence of the thymic tumors by early reports of case series and cohort studies.3,9 However, evidence for the effect of PORT on the recurrent risk in patients who have received the complete resection of stage II or III thymic tumor is generally derived from small retrospective studies. Moreover, the results of these studies were inconsistent.10–28 Inadequate statistical power may be one of the potential reasons underlying the negative results of the previous studies. Therefore, the aim of the current study was to combine the previously published data by performing a meta-analysis, which may likely demonstrate a significant effect of PORT on the recurrent outcomes in patients with complete resection of stage II or III thymic tumors.
Methods
We followed the Meta-Analysis of Observational Studies in Epidemiology protocol29 and Cochrane Handbook guidelines30 throughout the design, implementation, analysis, and reporting of this study.
Literature searching
PubMed, Embase, and Cochrane’s Library databases were searched for relevant studies, using the terms “thymic”, “thymus”, “thymoma”, in combination with “radiotherapy”, “radiation” and “adjuvant”, “postoperative”. Moreover, titles of abstracts from the websites of American Society of Clinical Oncology and the American Association of Thoracic Surgery were searched for the word “thymoma” to further include potential literature. We also analyzed the reference lists of original and review articles using a manual approach. The searching process was limited to studies in humans without restriction to publication languages. The final literature search was performed on July 5, 2015.
Study selection
Studies were included for analysis if they met the following criteria: 1) published as full-length article or abstract in any language; 2) reported as randomized or nonrandomized controlled studies (eg, cohort studies) in humans (regardless of sample size and follow-up duration); 3) included patients with stage II or III thymic tumors, in combination or separately, who received complete resection of the tumor and were assigned to the surgical procedure only (observing group), or surgical procedure with adjuvant (postoperative) radiotherapy (PORT group); and 4) documented the recurrent outcomes of the tumor (local, regional, or distant or in combination) during the follow-up, as the incidence or the number of the recurrent events in both the observing and the PORT groups.
Studies were excluded from the current meta-analysis if they met either one of the following criteria, even after the further clarification with the correspondence from the authors: 1) the Masaoka stage was not explicitly stated from the original articles; 2) data regarding the recurrent outcome in patients with complete resection of the tumor were not available; 3) the postoperative interventions were confounded by other treatment strategies, for example, chemotherapy; or 4) case reports or case series only included patients with complete resection and PORT, without the inclusion of controls (patients with complete resection and no PORT).
Data extraction and quality assessment
Two authors independently performed the literature searching, data extraction, and quality assessment according to the inclusion criteria. Discrepancies were resolved by discussion and consensus. The extracted data include: 1) the first authors and the publication years of the studies; 2) the baseline characteristics of the patients, including the mean ages and the sex distributions; 3) the number of patients with complete resection of stage II or III thymic tumors; 4) the total doses of the PORT therapy; 5) the ranges of the follow-up durations in each study; 6) the World Health Organization (WHO) histologic type of the thymic tumors;31 and 7) the incidence or the number of the recurrent events in both the observing and the PORT groups. We also tried to collect the survival data during the data extraction process. If available, a quantitative evaluation of the influence of PORT on survival outcomes in patients with stage II or III thymic tumor after complete resection would be performed.
The quality of the nonrandomized controlled trials were evaluated using the Newcastle–Ottawa Scale.32 This scale ranges from 1 to 9 stars and judges each study on three broad categories: selection of the study groups, the comparability of the groups, and the ascertainment of the outcome of interest.
Statistical analysis and data synthesis
Summary or individual data regarding the incidences or the numbers of patients with the recurrent events in both the observing and the PORT groups were used for the meta-analysis. We followed the previously published meta-analysis of the same topic33 to define and calculate the recurrence rate for the patients in the PORT group and in the observing group. Recurrence was defined as any recurrence according to the included studies, including local, regional, or distant. Recurrence rate was calculated as the ratio between the number of patients with recurrence and the total number of patients observed in each group. Odds ratio (OR) was then calculated using data from all eligible studies. The pooling of the data was performed for patients with either stage II or III thymic tumors, as well as for the patients with stage II and III separately. The Cochrane’s Q test30 and I2 test34 were used to assess heterogeneity among studies. We used a random effect model to obtain a pooled estimate of effect, since the considerable clinical heterogeneity has been noted during the data extraction process. Sensitivity analyses35 were conducted to evaluate the robustness of our results. We removed each study individually to evaluate that study’s effect on the summary estimates. Publication bias was evaluated by visually inspecting funnel plots for asymmetry.36 RevMan (Version 5.1; Cochrane Collaboration, Oxford, UK) and STATA software (Version 12.0; StataCorp LP, College Station, TX, USA) were used for the meta-analysis.
Results
Search results
The study selection process is shown in Figure 1. Overall, the database searching identified 566 citations, of which 19 studies,10–28 all designed as retrospective cohort studies, with 1,280 patients with stage II or III thymic tumor who received total resection, were included in the current meta-analysis. No randomized controlled trials were identified during the database searching process. The reasons for the exclusion of the 38 potentially relevant studies are listed in Figure 1.
  | Figure 1 Search and selection of studies included in the meta-analysis. |
Study characteristics
The characteristics of the included studies are included in Table 1. Overall, 19 studies with 663 patients with stage II or III thymic tumor assigned to the PORT group, and 617 patients assigned to the observing group were included. These studies were performed in Americans, Europeans, and Asians. Since most of the studies were presented as the retrospective review of the cases of the thymic tumor in different institutions, and the characteristics of the study population were summarized targeting the overall included cases (not limited to only stage II or III populations), most of the baseline characteristics (eg, age, sex) of the stage II or III patients for the included studies were unable to be extracted. Moreover, most of other general characteristics (eg, total dose of PORT, follow-up duration) were listed as ranges in the original literature, which prevented further quantitative analysis. Only two21,23 of the included studies provided data regarding the WHO histologic type of the thymic tumors. However, none of these studies evaluated the influence of histologic type on the effects of PORT in patients with complete resection of stage II or III thymic tumors. Briefly, we analyzed data regarding the histologic characteristics of the included studies according to whether they included only patients with thymoma, thymic carcinoma, or mixed type since thymic carcinoma has been considered to be more malignant biologically.31 It was shown that eight studies included patients with thymoma only,12,14,16,18,21–23,25 one included patients with thymic carcinoma only,28 eight with patients of both the histologic types,13,15,17,19,20,24,26,27 while the other two did not provide data regarding thymoma or thymic carcinoma.10,11
Quality assessment
The quality scores of studies included in the meta-analysis are listed in Table 1. The overall quality of the included studies varied, with only two studies scoring nine stars on the Newcastle–Ottawa scale.21,26 The other included studies did not provide information regarding whether they matched the baseline characteristics of the patients assigned to the PORT and the observing groups.
Effects of PORT on recurrent risk in patients with stage II and III thymic tumor after complete resection of the tumors
Overall, this meta-analysis included 663 patients with stage II or III thymic tumor assigned to the PORT group, and 617 patients assigned to the observing group. The recurrence rate for the patients in the PORT group was 12.4%, while the rate for those in the observing group was 11.5%. By pooling the results of the 19 studies, results of our meta-analysis with a random effect model indicated that PORT has no significant influence on recurrent risk in patients with stage II or III thymic tumor after complete resection of the tumors (OR 1.02, 95% confidence interval [CI] 0.55–1.90, P=0.96; Figure 2), and a moderate significant heterogeneity was detected (P=0.004, I2=53%). Subsequent analysis according to the stages of the tumor revealed that the recurrence rates for stage II patients in the PORT and observing groups were 7.9% and 9.5%, respectively, while the recurrent rates for those with stage III patients were 22.5% and 20.4%, respectively. Similarly, when stratified by ages, results of the meta-analyses did not indicate any significant effects of PORT on recurrent outcomes in either the stage II (16 studies with 836 patients, OR 1.04, 95% CI 0.54–2.01, P=0.91; Figure 3) or the stage III patients (ten studies with 369 patients, OR 1.04, 95% CI 0.41–2.65, P=0.93; Figure 4).
Sensitivity analysis
Results of sensitivity analysis by omitting one study at a time did not substantially change the overall results (P all >0.05) for meta-analyses for patients with stage II or III in combination, or stage II and III separately.
Effects of PORT on recurrent risk in patients with stage II or III thymic tumor according to the histologic characteristics
By pooling the data of studies which only included patients with thymoma, we found that PORT has no significant influence on recurrent risk in patients with stage II or III thymoma after complete resection of the tumors (OR 1.34, 95% CI 0.71–2.53, P=0.37; Figure 5A). Specifically, PORT has no significant influence on recurrent risk in patients with stage II (OR 1.09, 95% CI 0.53–2.25, P=0.80; Figure 5B) or stage III thymoma (OR 1.40, 95% CI 0.42–4.68, P=0.58; Figure 5C). Only one study included patients with stage II thymic carcinoma, the PORT remains lack of benefit on recurrence risk in these patients (OR 0.70, 95% CI 0.08–6.22, P=0.70).
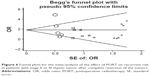
Publication bias
The funnel plot for the pooled analysis in patients with stage II or III thymic tumor after complete resection is shown in Figure 6. The plot was symmetrical on visual inspection, indicating a low probability of significant publication bias. Consistently, the results of the Egger’s regression test also indicated that the publication bias is not significant in this case (Egger’s test, P=0.21).
Effects of PORT on survival in patients with stage II and III thymic tumor after complete resection of the tumors
Although 16 studies10,12,15,17,19,21,23–28,37–40 performed a statistical analysis regarding the influence of PORT on survival outcomes in patients with stage II and III thymic tumor after complete resection, meta-analysis aiming to quantitatively evaluate the survival outcome by pooling the data from these 16 studies was impossible because individual survival data were infrequently listed, and the statistical strategies applied in these studies varied significantly. Most of these studies did not find significant effects of PORT on survival in these patients, while two found a beneficial effect of PORT on survival24,40 and one found a potential harmful effect on survival outcomes.15
Discussion
The major findings of our meta-analysis include the following: First, there is at present no high-quality prospective data regarding the impact of PORT in patients with stage II or III thymic tumors who received complete resection of the tumors. More importantly, by combing 19 available retrospective cohort studies, current evidence did not support any beneficial effects of PORT on recurrent outcomes in these patients. The results were consistent for patients with stage II or III thymic tumors after complete resection. Second, subsequent analysis limited to studies only including patients with thymoma or thymic carcinoma also did not support the benefits of PORT on recurrent outcomes. Finally, the significant heterogeneity in statistical analytic methods and clinical settings prevented a possible quantitative evaluation of PORT on survival data in these patients.
Although a previously published meta-analysis33 regarding the same topic has made effort to overcome the potential shortcomings in the lack of statistical power for the small-scale studies, and the results of our current meta-analysis were consistent with the previous ones, our study was necessary as 5 years have been passed since the last meta-analysis, and many cohort studies included in this meta-analysis were not included in the previous study. Indeed, our meta-analysis included 1,280 patients with stage II or III thymic tumor after complete resection, while the previous one only included less than half of ours (592 patients).33 However, results of our study also indicated that no significant influence of PORT on recurrent risk in patients with stage II or III thymic tumor after complete resection could be retrieved in this stage. The potential reasons for the lack of benefits of PORT on recurrent risk in these patients may include the following: First, studies regarding the recurrent pattern of patients with stage II or III thymic tumors after total resection showed that the most commonly detected recurrent sites were lungs, pleura, and diaphragm rather than the neighboring organs like pericardium or large vessels in the mediastinum.17,19,21,25 Therefore, localized PORT targeting the tissues and organs in the diaphragm may be of little effect for the prevention of the recurrence of the tumor in the chest. Moreover, the PORT was not without any adverse effect. In fact, the risks for the development of secondary malignancies41 and cardiovascular diseases42,43 have been well reported for patients receiving radiotherapy, which may adversely affect the clinical outcomes for patients assigned to PORT after complete resection of the tumors. Finally, since determination of stage III patients was made by surgeons during the surgery process, it has been proposed that sometimes it was difficult to accurately distinguish whether a complete resection is really complete. The subjective nature of the determination of stage III patients,5 as well as the subjective decision of the determination of PORT therapy in the retrospective cohort study by the surgeons may lead to the assignment of high-risk patients to the PORT group, which may further attenuate the potential beneficial effects of PORT on the clinical outcomes.
It has to be mentioned that our meta-analysis was based on the results of small-scale retrospective studies, and the quality of the included studies varies. One important implication of our study to the future is that, a high-quality prospective study, preferably a randomized controlled trial is needed to confirm our findings. However, it seemed to be difficult to be achieved because the incidence of the thymic tumor is very low. Furthermore, for studies evaluating the recurrence outcome with different observational periods, the optimal measure of effect should be hazard ratios (HRs). However, for our meta-analysis, since the recurrent data from most of the studies were extracted based on a proportion of the observed cohorts, which were seldom reported in HRs or analyzed based on the Kaplan–Meier curves, HRs could not be extracted directly or estimated based on methods by Tierney et al.44 Therefore, to avoid further loss of the information, we applied OR as the measure of effect in reference of a previously published meta-analysis of the same topic.33 Also, most of the included studies were designed as a retrospective review of the whole thymic tumor case series of their institution instead of a study exclusively on the patients with stage II or III thymic tumor after complete resection. Therefore, the baseline characteristics, and the follow-up data for this subgroup of patients were difficult to be extracted, which further prevented the quantitative evaluation of these characteristics on the clinical outcomes. Indeed, there has been report that the histologic feature of the tumor may influence the effects of PORT on clinical outcomes in patients with stage II or III thymic tumor.45 However, our study could not systematically evaluate the influence of the histologic characteristics of the tumor because only two21,23 of the included studies provided data regarding the WHO histologic type of the thymic tumors, and neither of these studies evaluated the influence of histologic type on the effects of PORT in these patients. In addition, we did not mention the type of PORT methods except for the fact that the total dose of PORT has been extracted. This is because protocols and regimens of PORT strategies were heterogeneous among the included studies, which made extraction and comparison difficult. We acknowledged that the differences of the protocols for PORT among the included studies may confer different influence on recurrent outcome. And the effect of new technique, such as intensity-modulated radiotherapy,9 on the recurrent outcome in patients with stage II/III thymic tumor after complete resection was not observed in the included studies. Moreover, studies are warranted to evaluate whether other postoperative treatment strategies, such as proton therapy, is effective to reduce the risk of recurrence in patients with stage II or III thymic tumor after complete resection, since this postoperative treatment has been considered safer than PORT.46 Finally, other potential limitations inherited to the meta-analysis of observational studies, such as considerable heterogeneity among the included studies, relative small numbers of patients included in each study, and lack of adjustment of potential confounding factors, should be considered when interpreting the results.
Conclusion
In conclusion, although derived from retrospective cohort studies, current evidence did not support any benefit of PORT on recurrent risk in patients with complete resection of the stage II or III thymic tumors. High-quality prospective studies are needed to further confirm our findings.
Acknowledgment
This work was supported by the Natural Science Foundation of China (No 81372531).
Disclosure
The authors report no conflicts of interest in this work.
References
Kondo K. Optimal therapy for thymoma. J Med Invest. 2008;55(1–2):17–28. | ||
Kondo K. Therapy for thymic epithelial tumors. Gen Thorac Cardiovasc Surg. 2014;62(8):468–474. | ||
Komaki R, Gomez DR. Radiotherapy for thymic carcinoma: adjuvant, inductive, and definitive. Front Oncol. 2014;3:330. | ||
Falkson CB, Bezjak A, Darling G, et al. The management of thymoma: a systematic review and practice guideline. J Thorac Oncol. 2009;4(7):911–919. | ||
Masaoka A, Monden Y, Nakahara K, Tanioka T. Follow-up study of thymomas with special reference to their clinical stages. Cancer. 1981;48(11):2485–2492. | ||
Masaoka A. Staging system of thymoma. J Thorac Oncol. 2010;5(10 Suppl 4):S304–S312. | ||
Gomez DR, Komaki R. Postoperative radiation therapy for non-small cell lung cancer and thymic malignancies. Cancers (Basel). 2012;4(1):307–322. | ||
Onuki T, Ishikawa S, Yamamoto T, et al. Pathologic radioresponse of preoperatively irradiated invasive thymomas. J Thorac Oncol. 2008;3(3):270–276. | ||
Giannopoulou A, Gkiozos I, Harrington KJ, Syrigos KN. Thymoma and radiation therapy: a systematic review of medical treatment. Expert Rev Anticancer Ther. 2013;13(6):759–766. | ||
Cohen DJ, Ronnigen LD, Graeber GM, et al. Management of patients with malignant thymoma. J Thorac Cardiovasc Surg. 1984;87(2):301–307. | ||
Monden Y, Nakahara K, Iioka S, et al. Recurrence of thymoma: clinicopathological features, therapy, and prognosis. Ann Thorac Surg. 1985;39(2):165–169. | ||
Curran WJ Jr, Kornstein MJ, Brooks JJ, Turrisi AT 3rd. Invasive thymoma: the role of mediastinal irradiation following complete or incomplete surgical resection. J Clin Oncol. 1988;6(11):1722–1727. | ||
Quintanilla-Martinez L, Wilkins EW Jr, Choi N, Efird J, Hug E, Harris NL. Thymoma. Histologic subclassification is an independent prognostic factor. Cancer. 1994;74(2):606–617. | ||
Haniuda M, Miyazawa M, Yoshida K, et al. Is postoperative radiotherapy for thymoma effective? Ann Surg. 1996;224(2):219–224. | ||
Ruffini E, Mancuso M, Oliaro A, et al. Recurrence of thymoma: analysis of clinicopathologic features, treatment, and outcome. J Thorac Cardiovasc Surg. 1997;113(1):55–63. | ||
Gripp S, Hilgers K, Wurm R, Schmitt G. Thymoma: prognostic factors and treatment outcomes. Cancer. 1998;83(8):1495–1503. | ||
Mangi AA, Wright CD, Allan JS, et al. Adjuvant radiation therapy for stage II thymoma. Ann Thorac Surg. 2002;74(4):1033–1037. | ||
Kondo K, Monden Y. Therapy for thymic epithelial tumors: a clinical study of 1,320 patients from Japan. Ann Thorac Surg. 2003;76(3):878–884;discussion 884–885. | ||
Singhal S, Shrager JB, Rosenthal DI, LiVolsi VA, Kaiser LR. Comparison of stages I-II thymoma treated by complete resection with or without adjuvant radiation. Ann Thorac Surg. 2003;76(5):1635–1641; discussion 1641–1642. | ||
Strobel P, Bauer A, Puppe B, et al. Tumor recurrence and survival in patients treated for thymomas and thymic squamous cell carcinomas: a retrospective analysis. J Clin Oncol. 2004;22(8):1501–1509. | ||
Rena O, Papalia E, Oliaro A, et al. Does adjuvant radiation therapy improve disease-free survival in completely resected Masaoka stage II thymoma? Eur J Cardiothorac Surg. 2007;31(1):109–113. | ||
Sousa B, Araujo A, Amaro T, Azevedo I, Soares M, Sousa O. Malignant thymomas – the experience of the Portuguese Oncological Institute, Porto, and literature review. Rev Port Pneumol. 2007;13(4):553–585. | ||
Utsumi T, Shiono H, Kadota Y, et al. Postoperative radiation therapy after complete resection of thymoma has little impact on survival. Cancer. 2009;115(23):5413–5420. | ||
Vassiliou V, Tsamandas A, Katodritis N, et al. The role of postoperative radiotherapy in the management of patients with thymic tumors – a retrospective study. In vivo (Athens, Greece). 2009;23(5):843–852. | ||
Chen YD, Feng QF, Lu HZ, et al. Role of adjuvant radiotherapy for stage II thymoma after complete tumor resection. Int J Radiat Oncol Biol Phys. 2010;78(5):1400–1406. | ||
Berman AT, Litzky L, Livolsi V, et al. Adjuvant radiotherapy for completely resected stage 2 thymoma. Cancer. 2011;117(15):3502–3508. | ||
Chang JH, Kim HJ, Wu HG, Kim JH, Kim YT. Postoperative radiotherapy for completely resected stage II or III thymoma. J Thorac Oncol. 2011;6(7):1282–1286. | ||
Song Z, Zhang Y. Adjuvant therapy in stage II thymic carcinoma. J Cancer Res Clin Oncol. 2014;140(2):349–352. | ||
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. | ||
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration; 2011. Available from: www.cochranehandbook.org. Accessed December 20, 2015. | ||
Marchevsky AM, Gupta R, McKenna RJ, et al. Evidence-based pathology and the pathologic evaluation of thymomas: the World Health Organization classification can be simplified into only 3 categories other than thymic carcinoma. Cancer. 2008;112(12):2780–2788. | ||
Wells GA, Shea BO, Connell D, Peterson J, Welch V. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; 2010. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed December 20, 2015. | ||
Korst RJ, Kansler AL, Christos PJ, Mandal S. Adjuvant radiotherapy for thymic epithelial tumors: a systematic review and meta-analysis. Ann Thorac Surg. 2009;87(5):1641–1647. | ||
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. | ||
Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37(5):1148–1157. | ||
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. | ||
Crucitti F, Doglietto GB, Bellantone R, Perri V, Tommasini O, Tonali P. Effects of surgical treatment in thymoma with myasthenia gravis: our experience in 103 patients. J Surg Oncol. 1992;50(1):43–46. | ||
Blumberg D, Port JL, Weksler B, et al. Thymoma: a multivariate analysis of factors predicting survival. Ann Thorac Surg. 1995;60(4):908–913; discussion 914. | ||
Regnard JF, Magdeleinat P, Dromer C, et al. Prognostic factors and long-term results after thymoma resection: a series of 307 patients. J Thorac Cardiovasc Surg. 1996;112(2):376–384. | ||
Eralp Y, Aydiner A, Kizir A, Kaytan E, Oral EN, Topuz E. Resectable thymoma: treatment outcome and prognostic factors in the late adolescent and adult age group. Cancer Invest. 2003;21(5):737–743. | ||
Ng J, Shuryak I. Minimizing second cancer risk following radiotherapy: current perspectives. Cancer Manag Res. 2015;7:1–11. | ||
Ong DS, Aertker RA, Clark AN, et al. Radiation-associated valvular heart disease. J Heart Valve Dis. 2013;22(6):883–892. | ||
Adams MJ, Hardenbergh PH, Constine LS, Lipshultz SE. Radiation-associated cardiovascular disease. Crit Rev Oncol Hematol. 2003;45(1):55–75. | ||
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. | ||
Omasa M, Date H, Sozu T, et al. Postoperative radiotherapy is effective for thymic carcinoma but not for thymoma in stage II and III thymic epithelial tumors: The Japanese Association for Research on the Thymus Database Study. Cancer. 2015;121(7):1008–1016. | ||
Figura N, Hoppe BS, Flampouri S, et al. Postoperative proton therapy in the management of stage III thymoma. J Thorac Oncol. 2013;8(5):e38–e40. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.