Back to Journals » Journal of Pain Research » Volume 12
Postoperative pain control after the use of dexmedetomidine and propofol to sedate patients undergoing ankle surgery under spinal anesthesia: a randomized controlled trial
Authors Kim D, Jeong JS , Park H, Sung KS, Choi SJ, Gwak MS, Kim GS, Hahm TS, Ko JS
Received 23 November 2018
Accepted for publication 26 March 2019
Published 13 May 2019 Volume 2019:12 Pages 1479—1487
DOI https://doi.org/10.2147/JPR.S195745
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor E Alfonso Romero-Sandoval
Doyeon Kim,1,* Ji Seon Jeong,1* Huigyeong Park,1 Ki-Sun Sung,2 Soo Joo Choi,1 Mi Sook Gwak,1 Gaab Soo Kim,1 Tae Soo Hahm,1 Justin Sangwook Ko1
1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 2Department of Orthopedics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
*These authors contributed equally to this work
Background: Dexmedetomidine is widely used for conscious sedation in patients undergoing lower-extremity surgery under regional anesthesia. We evaluated the postoperative analgesic effects of intravenous dexmedetomidine given during ankle surgery under spinal anesthesia.
Methods: Forty-three participants underwent repair of lateral angle ligaments under spinal anesthesia. For sedation during surgery, participants were allocated to a dexmedetomidine group (n=22) that received a loading dose of 1 mcg.kg−1, over 10 min, followed by a maintenance dose of 0.2–0.7 μg.kg−1,.h−1,; and a propofol group (n=21) that received an effective site concentration of 0.5–2.0 μg.mL−1, via target-controlled infusion. The primary outcome was the postoperative, cumulative, intravenous (IV) morphine equivalent dose delivered via IV patient-controlled anesthesia (PCA) and rescue analgesic consumption in the first 24 h after surgery. We recorded sensory and motor block durations.
Results: The postoperative IV morphine equivalent dose was 14.5 mg (0.75–31.75 mg) in the dexmedetomidine group compared to 48.0 mg (31.5–92.5 mg) in the propofol group (median difference, 33.2 mg; 95% confidence interval, 21.0–54.8 mg; P<0.001). The time to the first complaint of surgical site pain was significantly prolonged in the dexmedetomidine group (P<0.001), but the duration of motor block was comparable between the two groups (P=0.55).
Conclusion: IV dexmedetomidine given as a sedative during ankle surgery under spinal anesthesia reduced postoperative opioid consumption in the first 24 h. Thus, intraoperative dexmedetomidine is a versatile sedative adjunct.
Level of evidence: Level I, prospective randomized trial.
Keywords: ankle surgery, dexmedetomidine, postoperative analgesia, spinal anesthesia
Introduction
Dexmedetomidine is a selective α2-adrenergic agonist with sedative, anxiolytic, and analgesic effects.1 Most sedatives (eg, propofol) act on the gamma-aminobutyric acid (GABA) or N-methyl-D-aspartate (NMDA) receptors, but systemic dexmedetomidine activates α2-receptors in the locus coeruleus of the brain stem, triggering an unconsciousness similar to that of natural sleep.2 Because of this unique property, patients remain easily rousable, cooperative, and most importantly, at minimal risk for respiratory depression. Therefore, in the time since the drug was introduced in the 1990s, it has been widely used to sedate patients during a variety of surgical and nonsurgical procedures.3
The analgesic efficacies of both perineural and intravenous (IV) dexmedetomidine given as adjuncts to local anesthetics have been investigated in various contexts including neuraxial anesthesia and peripheral nerve blocks.4–7 Perineural dexmedetomidine prolongs both sensory and motor blocks; the latter block may be disadvantageous in clinical settings, delaying rehabilitation and possibly hospital discharge.7 IV dexmedetomidine sedation during spinal anesthesia significantly reduces postoperative pain and opioid consumption.8 In particular, a recent meta-analysis showed that IV dexmedetomidine significantly prolongs the duration of sensory block and the time to the first analgesic request after spinal anesthesia.4 Motor block duration is also prolonged, but less so than the sensory block, emphasizing the utility of IV dexmedetomidine in the context of regional anesthesia. However, most studies that have evaluated the postoperative analgesic effects of IV dexmedetomidine after spinal anesthesia have been performed in patients undergoing urological, lower abdominal, and lower extremity surgeries such as total knee replacement surgery.9–13 Therefore, we compared the postoperative analgesic effects of IV dexmedetomidine and propofol, another popular sedative, in patients undergoing ankle surgery under spinal anesthesia. We hypothesized that intraoperative dexmedetomidine sedation would decrease postoperative opioid consumption during the first 24 h after surgery.
Methods
This single-center, prospective, parallel-group, randomized control trial was conducted in accordance with the Declaration of Helsinki. In addition, this study was approved by the Institutional Review Board (IRB) of Samsung medical center, Seoul, Republic of Korea (IRB no. 2016–11-002–002) and written informed consent was obtained from all participants. The trial was registered with the Clinical Research Information Service prior to recruitment of the first participant (registration no. KCT0002246).
Patients scheduled for elective repair of the ankle lateral ligament (Brostrom’s operation) under spinal anesthesia were assessed in terms of eligibility from February 2017 to June 2018. Written informed consent was obtained from all patients who participated in the study. Inclusion criteria were 20–70 years of age and American Society of Anesthesiologists (ASA) physical status I–II. Exclusion criteria included contraindications for spinal anesthesia (eg, coagulopathy, pre-existing neurological deficits in the lower extremities, infection of the puncture site, and refusal to undergo such anesthesia); prolonged preoperative use of opioids or sedatives; any known allergy to study agents including dexmedetomidine and propofol; arrhythmia; heart failure; and/or severe hepatic or renal disease.
Randomization
After enrollment, all participants were randomly allocated to one of the two study groups using Allocation Software Version 1.0 running the random, permuted block method. Group assignments were placed in consecutively numbered, opaque sealed envelopes and patients received envelopes given to them by one of the authors not involved in either anesthetic management or outcome assessment. Propofol and dexmedetomidine differ in color and injection method; the anesthesiologist involved in ankle surgery thus knew the group assignment. A blinded investigator not involved in either spinal anesthesia or sedation collected all postoperative data.
Anesthesia protocols
After a patient entered the operating theatre, a standard electrocardiographic monitor and noninvasive devices measuring blood pressure and peripheral oxygen saturation were attached. The forehead was cleaned with a 70% alcohol swab and a bispectral index (BIS) quadrant sensor was attached according to the manufacturer’s guidelines. Intraoperative BIS values were monitored using a BIS Vista monitor (2013; BISx Revision 1.15; BIS Engine 4.1). After obtaining baseline data on vital signs, the patient was placed in the lateral decubitus position (depending on the surgical site) and IV midazolam 1–1.5 mg was administered as premedication. Each patient received oxygen at 4 L/min via a facial mask during spinal anesthesia, which was established via the L 3–4 or L 4–5 interspace (using a midline approach and a 25-G Whitacre needle; Vygon, UK). After free flow of cerebrospinal fluid was confirmed, 0.5% (w/v) hyperbaric bupivacaine 10 or 12 mg (depending on sex), with 200 μg morphine sulfate, was injected into the intrathecal space. Each patient was placed in the supine position immediately after intrathecal injection and an anesthesiologist blinded to group assessed the extent of sensory block using the pin prick test with a blunt 27 G needle. The extent of motor block was assessed using the modified Bromage scale (0= the ability to raise the extended leg against gravity; 1= an inability to raise the extended leg, but an ability to bend the knee; 2= an inability to bend the knee, but an ability to flex the ankle; and 3= complete motor block) at 5 min intervals for up to 30 min.
After confirming the establishment of appropriate spinal anesthesia, the study drugs were administered. The dexmedetomidine group received dexmedetomidine at 1 μg.kg−1 over 10 min (loading dose) and then 0.2–0.7 μg.kg−1.h−1 for maintenance; the propofol group received propofol at an effective site concentration of 0.5–2.0 μg.mL−1 via target-controlled infusion (Orchestra®; Fresenius Vial, Brezins, France). The drug levels were adjusted to maintain BIS values of 60–80 (thus ensuring sedation during the operative period); continuous end-tidal CO2 monitoring via a facial mask was performed during sedation. All surgeries were performed by a single experienced surgeon.
Hypotension (a mean blood pressure decrease of more than 20% from the pre-induction value) was treated via injection of 5 mg ephedrine or 100 μg phenylephrine; bradycardia (a heart rate less than 50 beats per min) was treated with 0.5 mg atropine. When the respiratory rate was lower than 8/min or when the oxygen saturation was lower than 90%, we considered that these reductions were side effects of the sedative, and the drug level was adjusted to maintain respiration, oxygen saturation, and the end-tidal CO2 level within the normal ranges. After arrival in the post-anesthetic care unit (PACU), all patients were assessed in terms of the extents of sensory and motor blocks; they were also scored on the OAA/S scale and adverse effects such as nausea and vomiting were recorded every 30 min. When the Aldrete score exceeded 9, the patient was transferred to the general ward.14
Postoperative supplemental analgesia was standardized. Pain severity using a numeric rating scale (NRS, ranging from 0 [no pain] to 10 [the worst pain]); if a patient scored the surgical site pain as over 3, IV PCA (delivered via an Abbott Hospira Gemstar pain management infusion pump) was commenced; this featured 0.9% normal saline with fentanyl 15 µg.mL−1 running at 1 mL.h−1 with a 1 mL bolus dose and a 15 min lockout time. The time to the first complaint of pain was recorded and patients with NRS scores over 3 despite IV PCA were given a rescue analgesic (IV pethidine 50 mg or morphine 10 mg). Once oral intake was tolerated, all patients received oral Cetamadol 325 mg/37.5 mg (acetaminophen 325 mg/tramadol HCl 37.5 mg) every 8 hrs. Despite of this analgesic protocol, if the patient complained pain greater than NRS 4, rescue analgesia with IV propacetamol 1 g was given. The cumulative opioid levels were converted into IV morphine equivalents,15 and the blinded assessor visited each patient at 8, 16 and 24 hrs after surgery and tabulated postoperative pain at rest in each time point. In addition, we educated patients to comment if the NRS scores was greater than 3 at the surgical site at other times throughout the first 24 hrs. If postoperative nausea and vomiting developed, metochlopramide 10 mg was administered; if the symptoms were not relieved, lamosetron 0.075 mg was given. If pruritus developed, chlorpheniramine 4 mg was administered. At 24 h after surgery, patient satisfaction in terms of intraoperative sedation and postoperative analgesia was measured using a Likert scale (1 to 5; 1= strongly dissatisfied, 2= dissatisfied, 3= neither satisfied nor dissatisfied, 4= satisfied, and 5= very satisfied).16 All patients were discharged on postoperative day (POD) 3 and were followed-up at the outpatient clinic on POD 14. Adverse effects associated with spinal anesthesia or intraoperative sedation were evaluated on PODs 3 and 14.
The primary outcome was the cumulative opioid consumption (IV morphine equivalent) in the first 24 h following surgery. Secondary outcomes included the time to the first complaint of pain at the surgical site, the durations of sensory and motor nerve blocks, and postoperative resting NRS scores.
Statistical analyses
Sample size calculation was based on a previous study12 and the mean 24 h morphine consumption after knee arthroplasty was 61.2 mg (standard deviation [SD] 11.2 mg). When a 20% reduction in opioid consumption associated with the use of intraoperative dexmedetomidine was considered clinically significant, use of the two-sided Student’s t-test with an alpha of 0.05 and a power of 0.9 indicated that 19 participants/group were required. Assuming a potential drop-out rate of 10%, the number of participants required to exhibit a clinically meaningful difference totaled 44 (22 in each group).
Continuous variables were compared using Student’s t-test or the Mann–Whitney U test, as appropriate, and adjusted by reference to the Bonferroni correction if multiple comparisons were in play. The normalities of continuous variable distributions were explored using the Shapiro–Wilk test. The chi-square test or Fisher’s exact test was used to analyze categorical variables. Kaplan–Meier survival analyses were performed (using the log-rank test) to compare the times to the first complaints of pain at surgical sites. Data are presented as means (with SDs), medians (with interquartile ranges [IQRs]), or median differences (with 95% confidence intervals [CIs]) for continuous variables; and as numbers (with percentages) for categorical variables.
All statistical analyses were performed using SAS version 9.4 software (SAS Institute Inc., Cary, NC, USA) and SPSS version 22.0 software (IBM Corporation, Armonk, NY, USA). A P-value <0.05 was considered to reflect statistical significance.
Results
A total of 45 patients were recruited; 1 who refused to participate was excluded. Thus, 44 participants were allocated to the two study groups; 43 completed the study (Figure 1). Patient characteristics were comparable between the two groups (Table 1).
 | Table 1 Patient’s Characteristics |
 | Figure 1 The CONSORT diagram. |
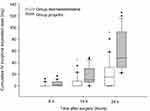
The postoperative, cumulative, IV morphine equivalent dose (median [IQR]) was significantly lower in the dexmedetomidine group (0.0 mg [0.0–8.0 mg]) than the propofol group (10.5 mg [6.6–29.7 mg]) at 16 h (median difference, 7.95 mg; 95% CI, 4.2–13.5 mg; P=0.005) and 24 h (14.7 mg [0.5–31.8 mg] and 48.0 mg [31.4–92.6 mg], respectively; median difference, 33.2 mg; 95% CI, 21.0–54.8 mg; P=0.0006) (Figure 2). However, there were no significant between-group differences at 8 h (P=0.06). Postoperative consumption of non-opioid analgesics was comparable between two groups (P=0.648). The postoperative NRS scores did not differ significantly at 8, 16, or 24 h (P=0.26, P=0.05, and P>0.99, respectively) (Figure 3).
The time to the first complaint of pain (median [IQR]) at the surgical site was 594 min (488–857 min) in the dexmedetomidine group and 449 min (418–522 min) in the propofol group (median difference: 150 min, 95% CI: 62–285 min; P<0.001). Kaplan–Meier survival analyses performed using the log-rank test showed that the time to first pain at the surgical site was longer in the dexmedetomidine than the propofol group (P<0.001) (Figure 4).
 | Figure 4 Kaplan–Meier survival plots showing the durations of postoperative analgesia in the two study groups. P<0.001 (log-rank test). |
The highest levels of sensory block, the times to two-level regression of the sensory block, and the durations of motor block were comparable in the two groups (P=0.74, P=0.23, and P=0.55, respectively) (Table 2).
 | Table 2 Duration of spinal anesthesia |
The total amounts (mean [SD]) of agents used for intraoperative sedation were 99.36 (87.44) μg in the dexmedetomidine group and 194.24 (92.82) mg in the propofol group. Table 3 lists the intra- and postoperative data. Intraoperative bradycardia was more frequent in the dexmedetomidine group than the propofol group (7/22 [31.8%] and 1/21 [4.8%], respectively; P=0.046). The incidence of overall postoperative complications did not differ significantly between the two groups. No spinal anesthesia- or sedation-related complications were evident on POD 3 or 14.
 | Table 3 Perioperative data |
Discussion
Patients who received the sedative dexmedetomidine during ankle surgery under spinal anesthesia required significantly less opioids during the first 24 h after surgery and the time to first pain at the surgical site was prolonged.
Ankle surgery can be performed under spinal anesthesia, affording both surgical anesthesia for up to 3 h and postoperative analgesia for up to 4 h.17 Once the analgesic wears off, ankle surgery is usually associated with moderate to severe pain a few days in duration; inadequate pain management can cause negative outcomes such as pulmonary function impairment, cardiac overload, and vascular resistance in turn triggering ventricular arrhythmia or major cardiac events.18–20 Clinically, IV opioids are the first-line agents used to control postoperative pain, but can be associated with various side effects such as nausea, vomiting, sedation, and respiratory depression. Therefore, pain management regimens featuring adjunct analgesia should be applied during ankle surgery to afford adequate pain relief and reduce opioid consumption.
Recently, many studies have shown that intraoperative IV dexmedetomidine significantly reduces postoperative opioid consumption and prolongs both peripheral and neuraxial blocks.21,22 The analgesic effects of dexmedetomidine are not fully understood but may feature binding of the drug to α2-receptors of the central nervous system, probably those of the locus coeruleus and spinal cord, blocking pain signal propagation and inducing analgesic effects.23,24 As neuronal α2-receptors may contribute to analgesic effects by inhibiting norepinephrine release,23 dexmedetomidine may enhance the actions of local anesthetics (LAs) and afford intraoperative sedation during spinal anesthesia.4 A previous study found that the α2-adrenergic receptors of the locus coeruleus mediated an antinociceptive effect after dexmedetomidine injection into rats.25 In line with this result, we found that sedation via IV dexmedetomidine significantly reduced postoperative opioid consumption and prolonged the duration of analgesia compared to propofol. Therefore, dexmedetomidine may afford effective postoperative pain control.
In a previous study, IV dexmedetomidine, compared to midazolam, combined with spinal anesthesia, prolonged the sensory block time, increased block level, and was associated with slower sensory regession.26 By contrast, we found no between-group differences in either the highest sensory block level attained or the time to two-level block regression. The differences between the two studies may be attributable to differences in the injection times and doses of the study drugs. The effects of dexmedetomidine peak about 10 min after injection;27 thus, drug administration after completion of spinal anesthesia might not affect the sensory block level. The biological half-life of dexmedetomidine is about 2 h28,29 and the dose used in the present study was approximately 1.3 mcg.kg−1, thus twice that of the cited work.26 IV dexmedetomidine increased the duration of spinal anesthesia, prolonged the time to first pain at the surgical site, and reduced postoperative opioid consumption.
An ideal intraoperative sedation agent should alleviate anxiety and ensure safety by preserving airway tone and preventing respiratory suppression. During spinal anesthesia, dexmedetomidine may be a better sedative than propofol because the cardiorespiratory profile is more stable, patient satisfaction is higher, and the analgesia afforded is more potent.30 Here, neither propofol nor dexmedetomidine was associated with respiratory depression. The hypotension rates and the numbers of patients requiring inotropics were similar in the two groups. However, the incidence of bradycardia was higher in the dexmedetomidine group (31.8 vs 4.8%). Dexmedetomidine does not directly affect the heart, and the cardiovascular response is biphasic.31 Within 1 min after bolus injection of dexmedetomidine, the high concentration in serum transiently increases blood pressure, triggering baroreceptor-reflex bradycardia via stimulation of the α2-adrenoceptors of vascular smooth muscle. After this initial phase, reduced drug concentrations in plasma may inhibit sympathetic outflow, reducing blood pressure.2 A previous meta-analysis showed that rapid infusion (within 10 min) of the initial dexmedetomidine loading dose was associated with a higher incidence of bradycardia than injection over 20 min.1,12 In our study, the incidence of bradycardia was high because of rapid infusion of the dexmedetomidine loading dose; slower infusion may be preferable. In addition, although dexmedetomidine-induced bradycardia is transient and can easily be treated with anticholinergics, patients on medications that can cause hemodynamic instability should be carefully reviewed prior to dexmedetomidine administration.
Study limitations
Our study had several limitations. First, postoperative analgesic effects vary by the intraoperative dexmedetomidine dose in patients who receive peripheral nerve blocks such as interscalene brachial plexus blocks;21 we did not evaluate the postoperative analgesic effects of dexmedetomidine. The effects of different dexmedetomidine doses on postoperative pain intensity require further study. Second, as morphine sulfate (200 μg) was injected together with LAs to afford additional analgesic effects (as dictated by our institutional, multimodal analgesic protocol),32 the true effects of IV dexmedetomidine on LA-only spinal anesthesia could not be assessed. Thus, our results should be interpreted with caution. Lastly, the cost increase due to the use of dexmedetomidine could become an issue. However, intraoperative dexmedetomidine may reduce the total amount of analgesics used for postoperative pain control. Thus, the amount of medical cost might not be expected to increase significantly.
Conclusion
In conclusion, we found that IV dexmedetomidine significantly reduced postoperative opioid use over the first 24 h after operation and increased the duration of postoperative analgesia after spinal anesthesia in patients undergoing ankle surgery. Dexmedetomidine not only maintains stable sedation during surgery but also effectively controls postoperative pain.
Data sharing statements
The authors intend to share, if requested by the journal:
• All the deidentified participant individual data.
• The initial protocol.
• Approval by the ethics committee.
The data can be accessible by contacting the corresponding author. These will be sent by means of attached files.
Acknowledgments
This trial had no funding source. The authors thank Dr. Insuk Sohn and Dr. Heewon Han who povided statistical advice. DK and JSJ are co-first authors for this study.
Author contributions
DK conducted the study and participated in data collection, data analysis, writing the manuscript, and manuscript preparation. JSJ contributed to protocol design, data collection, analysis and writing the manuscript. KSS contributed to the acquisition of data. HP participated to protocol design and contributed to the acquisition of data. SJC and MSG contributed to the analysis of data. GSK contributed to the interpretation of data. TSH contributed to the conception and design of the manuscript. JSK contributed to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data and drafting the article. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflict of interest in this work.
References
1. Chrysostomou C, Schmitt CG. Dexmedetomidine: sedation, analgesia and beyond. Expert Opin Drug Metab Toxicol. 2008;4(5):619–627. doi:10.1517/17425255.4.5.619
2. Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000;90(3):699–705.
3. Lobo FA, Wagemakers M, Absalom AR. Anaesthesia for awake craniotomy. Br J Anaesth. 2016;116(6):740–744. doi:10.1093/bja/aew113
4. Abdallah FW, Abrishami A, Brull R. The facilitatory effects of intravenous dexmedetomidine on the duration of spinal anesthesia: a systematic review and meta-analysis. Anesth Analg. 2013;117(1):271–278. doi:10.1213/ANE.0b013e318290c566
5. Abdallah FW, Dwyer T, Chan VW, et al. IV and perineural dexmedetomidine similarly prolong the duration of analgesia after interscalene brachial plexus block: a randomized, three-arm, triple-masked, placebo-controlled trial. Anesthesiology. 2016;124(3):683–695. doi:10.1097/aln.0000000000000983
6. Bharti N, Sardana DK, Bala I. The analgesic efficacy of dexmedetomidine as an adjunct to local anesthetics in supraclavicular brachial plexus block: a randomized controlled trial. Anesth Analg. 2015;121(6):1655–1660. doi:10.1213/ane.0000000000001006
7. Vorobeichik L, Brull R, Abdallah FW. Evidence basis for using perineural dexmedetomidine to enhance the quality of brachial plexus nerve blocks: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2017;118(2):167–181. doi:10.1093/bja/aew411
8. Gurbet A, Basagan-Mogol E, Turker G, et al. Intraoperative infusion of dexmedetomidine reduces perioperative analgesic requirements. Can J Anaesth. 2006;53(7):646–652. doi:10.1007/bf03021622
9. Al-Mustafa MM, Badran IZ, Abu-Ali HM, et al. Intravenous dexmedetomidine prolongs bupivacaine spinal analgesia. Middle East J Anaesthesiol. 2009;20(2):225–231.
10. Arain SR, Ebert TJ. The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth Analg. 2002;95(2):461–466. table of contents.
11. Chan IA, Maslany JG, Gorman KJ, O‘Brien JM, McKay WP. Dexmedetomidine during total knee arthroplasty performed under spinal anesthesia decreases opioid use: a randomized-controlled trial. Can J Anaesth. 2016;63(5):569–576. doi:10.1007/s12630-016-0597-y
12. Elcicek K, Tekin M, Kati I. The effects of intravenous dexmedetomidine on spinal hyperbaric ropivacaine anesthesia. J Anesth. 2010;24(4):544–548. doi:10.1007/s00540-010-0939-9
13. Hong JY, Kim WO, Yoon Y, et al. Effects of intravenous dexmedetomidine on low-dose bupivacaine spinal anaesthesia in elderly patients. Acta Anaesthesiol Scand. 2012;56(3):382–387. doi:10.1111/j.1399-6576.2011.02614.x
14. Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49(6):924–934. doi:10.1213/00000539-197011000-00020
15. Fishman SM. Bonica‘S Management of Pain. Philadelphia: Lippincott Williams & Wilkins; 2012.
16. Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;22(140):55.
17. Urfalioglu A, Gokdemir O, Hanbeyoglu O, et al. A comparison of ankle block and spinal anesthesia for foot surgery. Int J Clin Exp Med. 2015;8(10):19388–19393.
18. Filos KS, Lehmann KA. Current concepts and practice in postoperative pain management: need for a change? Eur Surg Res. 1999;31(2):97–107. doi:10.1159/000008627
19. Mangano DT, Wong MG, London MJ, Tubau JF, Rapp JA. Perioperative myocardial ischemia in patients undergoing noncardiac surgery–II: incidence and severity during the 1st week after surgery. The Study of Perioperative Ischemia (SPI) Research Group. J Am Coll Cardiol. 1991;17(4):851–857.
20. Rosenberg J, Kehlet H. Does effective postoperative pain management influence surgical morbidity? Eur Surg Res. 1999;31(2):133–137. doi:10.1159/000008631
21. Kang R, Jeong JS, Yoo JC, et al. Effective dose of intravenous dexmedetomidine to prolong the analgesic duration of interscalene brachial plexus block: a single-center, prospective, double-blind, randomized controlled trial. Reg Anesth Pain Med. 2018;43(5):488–495. doi:10.1097/aap.0000000000000773
22. Shin HJ, Do SH, Lee JS, Kim TK, Na HS. Comparison of intraoperative sedation with dexmedetomidine versus propofol on acute postoperative pain in total knee arthroplasty under spinal anesthesia: a randomized trial. Anesth Analg. 2018. doi:10.1213/ane.0000000000003315
23. Jaakola ML, Salonen M, Lehtinen R, Scheinin H. The analgesic action of dexmedetomidine–a novel alpha 2-adrenoceptor agonist–in healthy volunteers. Pain. 1991;46(3):281–285. doi:10.1016/0304-3959(91)90111-A
24. Liu L, Ji F, Liang J, He H, Fu Y, Cao M. Inhibition by dexmedetomidine of the activation of spinal dorsal horn glias and the intracellular ERK signaling pathway induced by nerve injury. Brain Res. 2012;1427:1–9. doi:10.1016/j.brainres.2011.08.019
25. Guo TZ, Jiang JY, Buttermann AE, Maze M. Dexmedetomidine injection into the locus ceruleus produces antinociception. Anesthesiology. 1996;84(4):873–881.
26. Kaya FN, Yavascaoglu B, Turker G, et al. Intravenous dexmedetomidine, but not midazolam, prolongs bupivacaine spinal anesthesia. Can J Anaesth. 2010;57(1):39–45. doi:10.1007/s12630-009-9231-6
27. Hsu YW, Cortinez LI, Robertson KM, et al. Dexmedetomidine pharmacodynamics: part I: crossover comparison of the respiratory effects of dexmedetomidine and remifentanil in healthy volunteers. Anesthesiology. 2004;101(5):1066–1076.
28. Ohtani N, Yasui Y, Watanabe D, Kitamura M, Shoji K, Masaki E. Perioperative infusion of dexmedetomidine at a high dose reduces postoperative analgesic requirements: a randomized control trial. J Anesth. 2011;25(6):872–878. doi:10.1007/s00540-011-1239-8
29. Weerink MAS, Struys M, Hannivoort LN, et al. Clinical pharmacokinetics and pharmacodynamics of dexmedetomidine. Clin Pharmacokinet. 2017;56(8):893–913. doi:10.1007/s40262-017-0507-7
30. Shah PJ, Dubey KP, Sahare KK, Agrawal A. Intravenous dexmedetomidine versus propofol for intraoperative moderate sedation during spinal anesthesia: A comparative study. J Anaesthesiol Clin Pharmacol. 2016;32(2):245–249. doi:10.4103/0970-9185.168172
31. Housmans PR. Effects of dexmedetomidine on contractility, relaxation, and intracellular calcium transients of isolated ventricular myocardium. Anesthesiology. 1990;73(5):919–922.
32. Souron V, Delaunay L, Schifrine P. Intrathecal morphine provides better postoperative analgesia than psoas compartment block after primary hip arthroplasty. Can J Anaesth. 2003;50(6):574–579. doi:10.1007/bf03018643
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.