Back to Journals » Cancer Management and Research » Volume 12
Postoperative Concurrent Chemoradiotherapy versus Postoperative Radiotherapy Alone for Larynx Squamous Cell Carcinoma Patients with Lymphovascular Invasion: A Propensity Score Matching Study
Authors Yu S, Zhu Y, Shi X, Hu K, Bai C, Diao W, Zhu X, Gao Z, Chen X
Received 20 February 2020
Accepted for publication 9 May 2020
Published 29 May 2020 Volume 2020:12 Pages 4063—4071
DOI https://doi.org/10.2147/CMAR.S250621
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Shuting Yu,1 Yingying Zhu,1 Xiaohua Shi,2 Ke Hu,3 Chunmei Bai,4 Wenwen Diao,1 Xiaoli Zhu,1 Zhiqiang Gao,1 Xingming Chen1
1Department of Otolaryngology-Head and Neck Surgery, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, People’s Republic of China; 2Department of Pathology, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, People’s Republic of China; 3Department of Radiotherapy, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, People’s Republic of China; 4Department of Oncology, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, People’s Republic of China
Correspondence: Xingming Chen
Tel +86 13901077778
Email [email protected]
Purpose: To date, no guidelines have been proposed for the ideal treatment of postoperative larynx squamous cell carcinoma (LSCC) patients with lymphovascular invasion due to a lack of similar studies. The present study was conducted to compare the survival and toxicity in LSCC patients with lymphovascular invasion receiving either postoperative radiotherapy (PORT) or postoperative chemoradiotherapy (POCRT). The results can be applied for more appropriate treatment of these patients.
Patients and Methods: Three hundred eighty-eight eligible LSCC patients with lymphovascular invasion were enrolled in this retrospective study. Survival and treatment-related toxicities were compared in the POCRT and PORT group using propensity score matching (PSM) methodology (1:1).
Results: Five-year overall survival (OS), disease-specific survival (DSS), and recurrence-free survival (RFS) of all patients were 48.7%, 58.2%, and 56.0%, respectively. Significantly, higher RFS rates (P=0.040) were found in the POCRT group than the PORT group in the PSM cohort. In the multivariate analysis, higher OS, DSS, and RFS rates were observed in the POCRT group than the PORT group (P=0.049, 0.024, and 0.011 respectively). Patients in the POCRT group presented more acute toxicities than those in the PORT group such as hematological toxicities (25.0% vs 0.9%, P< 0.001) and mucositis (35.0% vs 19.1%, P=0.002).
Conclusion: In the context of no ideal treatment for LSCC patients with lymphovascular invasion, the present study proposes POCRT as a preferable modality compared with PORT, as POCRT was associated with higher RFS rates. Higher RFS, DFS, and OS rates were also observed in the POCRT group in the multivariate analysis.
Keywords: head and neck carcinoma, larynx carcinoma, lymphovascular invasion, propensity score, chemoradiotherapy, survival
Introduction
The incidence rate of laryngeal squamous cell carcinoma (LSCC) ranks second among all respiratory system carcinomas after lung cancer.1–3 LSCC is also a common malignant tumor in the head and neck region.4 In China, the incidence rate and mortality have been increasing in recent years.5 Most patients with laryngeal cancer have developed advanced disease (stage III or IV) at diagnosis.6,7 For these patients, regional recurrence and distant metastases are prevalent after surgical resection. The risk is especially high in patients with adverse features, including extranodal extension, positive margins, lymphovascular invasion, perineural invasion, pT3 or pT4 primary, and pN2 or pN3 nodal disease.8
For patients with adverse features, surgery is frequently followed by concurrent chemoradiotherapy (CCRT) or radiotherapy alone, as proposed in the NCCN Guidelines for head and neck cancer. CCRT is recommended for patients with extranodal extension and/or positive margins, but for patients with other risk features such as lymphovascular invasion, there are no guidelines regarding whether postoperative chemotherapy should be applied. Several studies have shown that combining chemotherapy with postoperative radiotherapy significantly improved local or regional control of locally advanced head and neck squamous cell carcinoma (HNSCC),9–11 but these studies defined “locally advanced” differently, and patients with lymphovascular invasion were not studied alone. Additionally, chemotherapy also increased the incidence of anemia, granulocytopenia, thrombocytopenia, functional mucosal reactions, and acute skin toxicity. Therefore, for patients with lymphovascular invasion, whether to apply chemotherapy should be considered deliberately.
Currently, no studies have addressed the impact of combining chemotherapy with postoperative radiotherapy among patients with lymphovascular invasion of LSCC. Therefore, herein we performed a propensity score matching (PSM) analysis in these patients to compare postoperative radiotherapy (PORT) to postoperative chemoradiotherapy (POCRT).
Patients and Methods
Patient Population
A total of 388 patients were consecutively enrolled in this study at Peking Union Medical College Hospital (PUMCH) from January 2007 to December 2017. Eligible patients should meet all the following criteria: (i) pathologically confirmed, previously untreated LSCC undergoing radical resection; (ii) had at least one of the following adverse features: vascular invasion, lymphatic invasion (iii) received PORT or POCRT. The exclusion criteria were as follows: (i) extranodal extension or positive margin; (ii) loss during follow-up; (iii) presence of other malignant tumors. TNM stages of all participants were identified according to the American Joint Committee on Cancer (AJCC) in 2017. Clinical information such as age, sex, overall stage, differentiation grade, comorbidity score, treatment, tumor site, and tobacco and alcohol consumption were obtained from the medical history of the participants. HPV16 (human papillomavirus 16) DNA was detected by quantitative real-time PCR (qRT-PCR) as previously indicated.12
“Smokers” were defined as patients who had smoked >100 cigarettes during their lifetime; otherwise, they were defined as “never smokers”. “Drinkers” were defined as those who drank alcohol at least once a week for a year or longer; whereas “never drinkers” had drunk less. The adult comorbidity score was graded by the Adult Comorbidity Evaluation 27 index (a disease-specific comorbidity index), which is a reliable predictor of survival in patients with laryngeal squamous cell carcinoma.13
Surgical Procedures
All patients in the study received curative surgery. Primary tumor resection and neck dissection were performed following accepted criteria for adequate resection depending on the location and extent of the tumor. Resection margins were also evaluated by frozen section diagnosis to ensure adequate resection. All surgeries were completed by the same surgical team to assure comparability.
Histological Analysis
Pathological data were extracted from pathological reports and original pathology slides were re-examined by two pathologists who were blinded to the clinical outcomes. Lymphovascular invasion was defined as the presence of carcinoma cells in an endothelial-lined space.
Radiotherapy
All patients in the study started to receive PORT within 6 weeks after surgical resection. In brief, patients who underwent PORT received a total of 60–66 Gy in 30–33 fractions in regions at high risk for malignant dissemination.
Chemotherapy
The POCRT regimen comprised mainly a combination of identical PORT plus concurrent cisplatin administrated every 3 weeks at 100 mg/m2. Two to three cycles of chemotherapy were used depending on the radiation fractionation scheme. If needed, the dose was modified at the physician’s discretion. Few patients were given 30 to 50 mg/m2 of cisplatin weekly because of adverse effects.
Patient Follow-Up
After surgery, patients were evaluated every 3 months over the first 3 years and every 6 months thereafter by physical examination and CT/MRI scans. All patients were followed up for at least 2 years or until death. Patients were regarded as recurrence-free if cancer absence was recorded on the last visit. Recurrences were diagnosed by biopsy, PET, bone scan or CT/MRI.
Overall survival (OS) was assigned as the primary end-point, which was the time from the beginning of therapy to the date of death due to any cause or last follow-up. The secondary end-points were recurrence-free survival (RFS) and disease-specific survival (DSS). DSS was the time from the beginning of treatment to the date of death from LSCC or the last follow-up. RFS was the time from starting treatment to the date of recurrence or last follow-up. Toxicities related to chemotherapy and radiotherapy were graded using Common Terminology Criteria for Adverse Events (CTCAE) v4.0.14
Statistical Analysis
The results are presented as the number of cases and percentages. Baseline characteristics between the POCRT group and the PORT group were compared with the Pearson χ2 test. PSM was applied because several significant differences were found in the baseline data between the two groups. Nearest neighbor 1:1 matching was applied in the matching for the POCRT and PORT group. Matching covariates included age, gender, adult comorbidity score, tumor site, clinical stage, differentiation grade, HPV status, and tobacco and alcohol consumption. Survival analyses comparing the two groups were performed using Kaplan–Meier methodology and the Log-rank test. The unadjusted Cox proportional hazards model was applied in the univariate and multivariate analyses to estimate the hazard ratio (HR). All statistical tests were two-sided, and P-values <0.05 were considered statistically significant. Statistical analyses were conducted using SPSS version 23.0 (IBM Corporation, Armonk, NY, USA).
Results
Baseline Characteristics
From January 2007 to December 2017, 388 eligible patients were enrolled in this study. Most patients were between 56 and 70 years old (61.3%). The male:female ratio was 23.2:1 (372 males:16 females). Most patients (51.5%) were diagnosed with stage III–IV diseases. Two hundred and seventy-eight patients were treated with POCRT and 110 with PORT.
The baseline characteristics of the two groups before and after PSM are presented in Table 1. Before PSM, no significant differences were found between the two groups regarding age, gender, alcohol consumption, clinical stage and tumor site. Compared with the PORT group, the POCRT group had a significantly higher proportion of smokers (P=0.033), HPV-negative patients (P=0.041), patients with poorly differentiated LSCC (P=0.043), and patients with none to mild morbidity score (P=0.015). We selected all the characteristics in Table 1 as independent variables for the propensity score calculation. Using PSM (1:1), 110 patients who received POCRT were paired with 110 patients who received PORT. After PSM, the baseline characteristics between the two groups were well balanced as shown in Table 1.
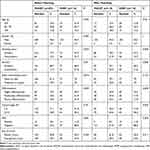 |
Table 1 Baseline Characteristics of LSCC Patients Before and After Propensity-Score Matching Between POCRT and PORT Groups |
Treatment Exposure
The median cumulative radiation dose in the whole cohort was 65 Gy. Nine patients (5 patients in the PORT group and 4 in the POCRT group) received <60 Gy. The median cumulative radiation dose was the same in both groups (65 Gy), and there was no significant difference in the radiation dose between the two groups. In the POCRT group, 19 patients stopped chemotherapy within two courses.
Treatment Outcomes
The median OS, DSS, and RFS time for the entire cohort were 48, 48, and 43 months, respectively. At the end of the study, 173 patients were alive. A total of 167 patients (POCRT, n=108; PORT, n=59) expired due to LSCC. Forty-eight patients expired due to intercurrent diseases. The 3- and 5-year OS rates for the whole cohort were 76.0% and 48.7%, respectively. The 3- and 5-year DSS rates for the whole cohort were 77.2% and 58.2%, respectively.
Recurrences were observed in 176 patients. The 3- and 5-year RFS rates for the whole cohort were 70.7% and 56.0%, respectively. Despite recurrence, the patients could still survive for several months after the diagnosis of relapse. The median survival time of patients with recurrence was 9.0 months (range: 0–26 months). However, most patients with recurrence experienced related symptoms, including dyspnea, tissue infections requiring antibiotics, dysphagia, and bucking.
As shown in Figure 1, before PSM, the POCRT group was associated with better OS (P=0.045) and RFS (P=0.040). After PSM, the 5-year OS was 50.5% in the POCRT group compared with 42.4% in the PORT group. The 5-year DSS was 61.6% in the POCRT group compared with 52.4% in the PORT group. The 5-year RFS was 58.1% and 48.0% in the POCRT and PORT group, respectively. A significant difference in RFS was found between the two groups (P=0.040).
Univariate and Multivariate Analyses
As shown in Table 2, before PSM, the treatment group (PORT vs POCRT) was associated with OS (P=0.048) and RFS (P=0.042) in the univariate analysis. After adjustment for age, gender, smoking status, alcohol, adult comorbidity score, differentiation, clinical stage, tumor site, and HPV status, patients in the POCRT group were associated with a better RFS (HR=1.441; 95% CI 1.052–1.975; P=0.023).
 |
Table 2 Univariate and Multivariate Cox Regression Analyses in Patients Received POCRT or PORT |
After PSM, the treatment group (PORT vs POCRT) was associated with RFS (HR=1.494; 95% CI 1.013–2.202; P=0.043) in the univariate analysis. In the multivariate analysis, the treatment group (PORT vs POCRT) was a significant predictive factor for OS (HR=1.432; 95% CI 1.002–2.407; P=0.049), DSS (HR=1.607; 95% CI 1.065–2.424; P=0.024) and RFS (HR=1.667; 95% CI 1.123–2.474; P=0.011).
Treatment-Related Complications
The incidences of treatment toxicities were recorded for the POCRT group and PORT group and are shown in Table 3. Patients receiving POCRT had significantly higher incidences of grade 1–3 acute hematologic toxicities (25% vs 0.9%, P<0.001) and mucositis (35.0% vs 19.1%, P=0.002). There was no significant difference in dermatitis (9.7% vs 8.2%, P=0.636) between the two groups. Regarding late toxicities, no significant differences were found in the incidence of xerostomia (19.8% vs 23.6%, P=0.398) or dysphagia (6.2% vs 9.1%, P=0.322) between the two groups. There were no grade 4 toxicities in either group.
 |
Table 3 Incidence of Toxicities During Postoperative Treatment Between POCRT and PORT Groups |
Discussion
Lymphovascular invasion is a significant pathological diagnosis for HNSCC patients. Several studies have explored the correlation of lymphovascular invasion with clinicopathological factors and prognosis in HNSCC. Studies have shown that lymphovascular invasion may be related to lymph node metastasis and a poor prognosis in HNSCC, including larynx carcinoma, tongue carcinoma, oral carcinoma, and hypopharyngeal carcinoma.15–20 However, NCCN guidelines for head and neck cancer mostly recommend “radiotherapy or consider chemoradiotherapy” for postoperative patients with lymphovascular invasion, and to our knowledge, no studies in the literature focus specifically on ideal postoperative treatments for HNSCC patients with lymphovascular invasion.
In the 1990s, two significant trials, EORTC22931 and ETOG95-01, were conducted to further compare POCRT with PORT as adjuvant treatment for high-risk head and neck cancer.11,21 Combining these two trials, it was indicated that POCRT with cisplatin was superior to PORT alone for patients with either of the common risk factors in the two studies: positive margins and extracapsular nodal extension from neck nodes.22 Although patients with lymphovascular invasion were also included in the EORTC trial, and a possible advantage of POCRT was observed in these patients, no conclusion could be drawn due to the aggregation of all risk factors in the study.
In the current study, we evaluated the prognosis of LSCC patients with lymphovascular invasion receiving either POCRT or PORT. In addition to completing a review of all pathological specimens, a PSM method was applied to adjust confounding factors between the two groups. The present study showed significantly better RFS of patients in the POCRT group than the PORT group (3 and 5 years: 73.5% and 58.1% versus 66.0% and 48.0%). These results revealed that concurrent chemotherapy using cisplatin might generate substantial radiosensitization of LSCC, as demonstrated in prior studies.9,23–27 The results could also be explained by the observed synergistic effects between cisplatin and radiation, which might also improve locoregional control of the primary tumor in patients who have received POCRT.28 No significant differences in OS and DSS were found between the two groups in Kaplan–Meier analysis, which could be explained by the median survival time of 9.0 months (0–26 months) of patients with LSCC recurrence. Thus, the RFS benefit due to POCRT did not convert into a survival advantage. Regarding the health care of patients with malignancy, the aims are not only to extend overall survival but also to improve quality of life. Thus, the significant reduction of the recurrence rate in these LSCC patients receiving POCRT is believed to be clinically important. In the multivariate analysis of the propensity matched cohort, POCRT was the significant variable related to RFS (P=0.011), DSS (P=0.024) and OS (P=0.049), which indicated that the addition of chemotherapy was associated with higher RFS as well as higher DSS and OS.
In terms of treatment toxicity, the proportion of grade 1–3 late toxicities was similar between the two groups, whereas patients who received POCRT had more acute hematological toxicities (25% vs 0.9%, P<0.001) and mucositis (35.0% vs 19.1%, P=0.002). Life-threatening toxicities were not observed in either group. Our results are in line with other studies in the literature. Several randomized clinical trials have shown that POCRT increases grade 3–4 acute toxicities in comparison with PORT alone (RTOG 9501: 77% vs 34%, P<0.001; EORTC 22931: 41% vs 2%, P=0.001)11,21 in patients with head and neck cancers, while the incidences of grade 3–4 late complications between the two groups are comparable (long-term report of RTOG 9501: 24.9% vs 20.5%, P=0.34).29 The higher occurrence of acute toxicities in the POCRT group might delay postoperative treatments, lead to more unplanned hospitalizations and impact the quality of life in these patients. Therefore, acute toxicities should be noted and the dose of chemotherapy should be modified at the physician’s discretion.
To our knowledge, few studies have explored whether HNSCC patients with lymphovascular invasion should receive concurrent chemoradiotherapy. The intention of our study was not to assess a new therapy, but to identify the optimal treatment effect and fewer treatment-related toxicities for these patients. Several unavoidable limitations inherent in this study should be acknowledged. First, this was a retrospective study conducted in a single institution and therefore involved possible selection bias. The patients enrolled in our study tended to have larynx cancer of more adverse clinical stage. Therefore, the PSM method was applied to ensure the compatibility between the two groups to draw the conclusion. Second, the relatively small sample size in this study and other unmeasured factors (such as underestimation of undocumented treatment-induced side effects in patients and subjective treatment decisions) might bias our results. Medical history of patients and telephone follow-up were applied to ensure the sufficient records of side effects in Form CTCAE, and further studies conducted with more patients will be performed to verify our conclusion.
Conclusions
In conclusion, our PSM study demonstrated that adding concomitant chemotherapy to PORT was associated with higher RFS rates in LSCC patients with lymphovascular invasion. In addition to RFS, POCRT also had a significant impact on OS and DFS in these patients in the multivariate analysis. However, the addition of concurrent chemotherapy to PORT also led to more treatment-induced acute toxicities, which were not life-threatening.
Abbreviations
LSCC, larynx squamous cell carcinoma; PORT, postoperative radiotherapy; POCRT, postoperative chemoradiotherapy; PSM, propensity score matching; OS, overall survival; DSS, disease-specific survival; RFS, recurrence-free survival; HNSCC, head and neck squamous cell carcinoma.
Data Sharing Statement
The analyzed data in this study could be acquired from the corresponding author on reasonable claim.
Ethics Approval and Informed Consent
The current study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China. A signed informed consent was obtained from each patient in this study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
The present study was supported by the National Natural Science Foundation of China (grant number 81273173).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lin HW, Bhattacharyya N. Staging and survival analysis for nonsquamous cell carcinomas of the larynx. Laryngoscope. 2008;118(6):1003–1013. doi:10.1097/MLG.0b013e3181671b3d
2. Hoffman HT, Porter K, Karnell LH, et al. Laryngeal cancer in the United States: changes in demographics, patterns of care, and survival. Laryngoscope. 2006;116(9Pt 2 Suppl 111):1–13.
3. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107
4. Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–E386. doi:10.1002/ijc.29210
5. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi:10.3322/caac.21338
6. Groome PA, O’Sullivan B, Irish JC. Management and outcome differences in supraglottic cancer between Ontario, Canada, and the Surveillance, Epidemiology, and End Results areas of the United States. Journal of Clin Oncol. 2003;21(3):496–505. doi:10.1200/JCO.2003.10.106
7. Marur S, Forastiere AA. Head and neck cancer: changing epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2008;83(4):489–501. doi:10.4065/83.4.489
8. Cooper JS, Pajak TF, Forastiere A, et al. Precisely defining high-risk operable head and neck tumors based on RTOG #85-03 and #88-24: targets for postoperative radiochemotherapy? Head Neck. 1998;20(7):588–594. doi:10.1002/(SICI)1097-0347(199810)20:7<588::AID-HED2>3.0.CO;2-F
9. Bachaud JM, David JM, Boussin G, Daly N. Combined postoperative radiotherapy and weekly cisplatin infusion for locally advanced squamous cell carcinoma of the head and neck: preliminary report of a randomized trial. Int J Radiat Oncol Biol Phys. 1991;20(2):243–246. doi:10.1016/0360-3016(91)90098-O
10. Haffty BG, Son YH, Sasaki CT, et al. Mitomycin C as an adjunct to postoperative radiation therapy in squamous cell carcinoma of the head and neck: results from two randomized clinical trials. Int J Radiat Oncol Biol Phys. 1993;27(2):241–250. doi:10.1016/0360-3016(93)90234-M
11. Bernier J, Domenge C, Ozsahin M, et al. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004;350(19):1945–1952. doi:10.1056/NEJMoa032641
12. Zhu Y, Xia X, Gross N, et al. Prognostic implications of human papillomavirus status and p16 expression in laryngeal squamous cell carcinoma. Head Neck. 2019;41(12):4151–4163. doi:10.1002/hed.25961
13. Nesic VS, Petrovic ZM, Sipetic SB, Jesic SD, Soldatovic IA, Kastratovic DA. Comparison of the Adult Comorbidity Evaluation 27 and the Charlson Comorbidity indices in patients with laryngeal squamous cell carcinoma. J Laryngol Otol. 2012;126(5):516–524. doi:10.1017/S0022215112000254
14. National Cancer Institute (US). Common Terminology Criteria for Adverse Events (CTCAE).
15. Michikawa C, Uzawa N, Kayamori K, et al. Clinical significance of lymphatic and blood vessel invasion in oral tongue squamous cell carcinomas. Oral Oncol. 2012;48(4):320–324. doi:10.1016/j.oraloncology.2011.11.014
16. Fives C, Feeley L, O’Leary G, Sheahan P. Importance of lymphovascular invasion and invasive front on survival in floor of mouth cancer. Head Neck. 2016;38(Suppl 1):E1528–E1534. doi:10.1002/hed.24273
17. Saito Y, Omura G, Yasuhara K, et al. Prognostic value of lymphovascular invasion of the primary tumor in hypopharyngeal carcinoma after total laryngopharyngectomy. Head Neck. 2017;39(8):1535–1543. doi:10.1002/hed.24705
18. Close LG, Brown PM, Vuitch MF, Reisch J, Schaefer SD. Microvascular invasion and survival in cancer of the oral cavity and oropharynx. Arch Otolaryngol Head Neck Surg. 1989;115(11):1304–1309. doi:10.1001/archotol.1989.01860350038011
19. Clark JR, de Almeida J, Gilbert R, et al. Primary and salvage (hypo)pharyngectomy: analysis and outcome. Head Neck. 2006;28(8):671–677. doi:10.1002/hed.20428
20. Yilmaz T, Hosal AS, Gedikoglu G, Onerci M, Gursel B. Prognostic significance of vascular and perineural invasion in cancer of the larynx. Am J Otolaryngol. 1998;19(2):83–88. doi:10.1016/S0196-0709(98)90100-4
21. Cooper JS, Pajak TF, Forastiere AA, et al. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004;350(19):1937–1944. doi:10.1056/NEJMoa032646
22. Bernier J, Cooper JS, Pajak TF, et al. Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (# 9501). Head Neck. 2005;27(10):843–850. doi:10.1002/hed.20279
23. Al-Sarraf M, Pajak TF, Marcial VA, et al. Concurrent radiotherapy and chemotherapy with cisplatin in inoperable squamous cell carcinoma of the head and neck. An RTOG Study. Cancer. 1987;59(2):259–265. doi:10.1002/1097-0142(19870115)59:2<259::AID-CNCR2820590214>3.0.CO;2-1
24. Merlano M, Benasso M, Corvo R, et al. Five-year update of a randomized trial of alternating radiotherapy and chemotherapy compared with radiotherapy alone in treatment of unresectable squamous cell carcinoma of the head and neck. J Natl Cancer Inst. 1996;88(9):583–589. doi:10.1093/jnci/88.9.583
25. Brizel DM, Albers ME, Fisher SR, et al. Hyperfractionated irradiation with or without concurrent chemotherapy for locally advanced head and neck cancer. N Engl J Med. 1998;338(25):1798–1804. doi:10.1056/NEJM199806183382503
26. Wendt TG, Grabenbauer GG, Rodel CM, et al. Simultaneous radiochemotherapy versus radiotherapy alone in advanced head and neck cancer: a randomized multicenter study. Journal of Clin Oncol. 1998;16(4):1318–1324. doi:10.1200/JCO.1998.16.4.1318
27. Pignon JP, Bourhis J, Domenge C, Designe L. Chemotherapy added to locoregional treatment for head and neck squamous-cell carcinoma: three meta-analyses of updated individual data. MACH-NC Collaborative Group. Meta-Analysis of Chemotherapy on Head and Neck Cancer. Lancet. 2000;355(9208):949–955. doi:10.1016/S0140-6736(00)90011-4
28. Seiwert TY, Salama JK, Vokes EE. The concurrent chemoradiation paradigm–general principles. Nat Clin Pract Oncol. 2007;4(2):86–100. doi:10.1038/ncponc0714
29. Cooper JS, Zhang Q, Pajak TF, et al. Long-term Follow-up of the RTOG 9501/Intergroup Phase III Trial: postoperative Concurrent Radiation Therapy and Chemotherapy in High-Risk Squamous Cell Carcinoma of the Head and Neck. Int J Radiat Oncol Biol Phys. 2012;84(5):1198–1205. doi:10.1016/j.ijrobp.2012.05.008
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

