Back to Journals » Breast Cancer: Targets and Therapy » Volume 11
Positive margins (R1) risk factors in breast cancer conservative surgery
Authors Lombardi A , Pastore E , Maggi S , Stanzani G, Vitale V, Romano C , Bersigotti L, Vecchione A , Amanti C
Received 28 April 2019
Accepted for publication 12 June 2019
Published 26 July 2019 Volume 2019:11 Pages 243—248
DOI https://doi.org/10.2147/BCTT.S210788
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pranela Rameshwar
Augusto Lombardi,1 Elena Pastore,1 Stefano Maggi,1 Gianluca Stanzani,2 Valeria Vitale,2 Camilla Romano,1 Laura Bersigotti,1 Andrea Vecchione,3 Claudio Amanti1
1Breast Surgery, Università La Sapienza, Ospedale Sant’Andrea, Rome, Italy; 2Breast Surgery, Ospedale Sant’Andrea, Rome, Italy; 3Department of Pathology, Università La Sapienza, Ospedale Sant’Andrea, Rome, Italy
Background: The primary goal in conservative breast cancer surgery is the complete excision of the tumor, but at the same time attempting to obtain a satisfactory postoperative esthetic result. The notion of “No Ink on Tumor” that indicates exclusively the presence of tumor cells on the inked surface of the surgical specimen is now the gold standard; however, the problem of the free margin is still a fundamental topic of debate that has not yet found a definitive solution.
Methods: Our retrospective analysis takes into account 1440 patients undergoing breast conservative surgery, from October 2004 to November 2018, all treated at the breast unit of our institution.
Results: Positive margins (R1) rate was 10.2% (147 cases out of 1440). Overall survival was 95% at 5 years and 89% at 10 years. No differences in mortality and local recurrence rate between R0 and R1 patients were found. Half of the R1 patients underwent secondary surgery with enlargement of margins, while in the other half we performed direct mastectomy. Among the analyzed variables, age, histological size, histological type, grading, multifocality, lympho-vascular invasion and lymph node status were significantly correlated with the R1 status. The multivariate analysis shows the association of age and surgical technique (oncoplastic) with R1 status.
Conclusion: Further studies will allow the creation of a statistical model, for better pre-operative prediction of patients with higher risk of R1 and better selection of patients to be candidates for conservative surgery.
Keywords: breast-conserving therapy, margin status, age, oncoplastic surgery
Introduction
In the last 40 years, the trend in management of breast cancer has followed less invasive policies of treatment than mastectomy.1 Nevertheless, the recent increase in mastectomies disregards the cultural approach to date.
Multiple large-scale studies have confirmed that, in terms of survival, the conservative surgery followed by radiation therapy is as effective as mastectomy.2,3
The primary goal of conservative surgery is the complete excision of the tumor, maintaining the oncological radicality but at the same time attempting to a satisfactory postoperative esthetic result.4
On this concern, the “resection margins” are a fundamental issue for the conservative surgery. By “surgical resection margin”, we mean the distance between the tumor and the edge of the surrounding tissue, which is to be removed completely.
The old prevailing historical concept claimed that a wider margin of resection would lower the risk of recurrence of neoplastic cells in the residual mammary tissue.5
Although this theory is not improper in terms of common sense, various meta-analyses carried out in more recent years have shown that wider margins are not associated with a lower risk of recurrence.6–9
For many years, the precise size of “adequacy” of the resection margins has been a controversial subject.7,10,11 Morrow’s work asserted the notion of “NO INK on Tumor”, after the publication of her paper, a multidisciplinary consensus panel examining a meta-analysis of 33 studies conducted on 28,126 patients. The term “positive margin“ (R1 in TNM stadiation) indicates exclusively the presence of tumor cells on the inked surface of the surgical specimen. This condition is associated with an increase in local recurrence of approximately two-fold. This risk is not reduced in the case of favorable biology, endocrine therapy and radiological boosting.12
In this era of multidisciplinary therapy, “no ink on tumor” is now becoming a standard policy to grasp the appropriateness of the margins in surgery operations. In fact, it is associated with low rates of ipsilateral true breast tumor recurrence and has the potential to decrease re-excision rates, improve cosmetic outcomes and decrease health care cost.13,14
However, the problem of the free margin size is still a fundamental topic of debate that has not yet found a definitive solution.15
While waiting to find an “adequate” surgical margin, our present aim is to identify the factors influencing the R1 in breast conservative surgery.
Patients and methods
Our analysis takes into account 1440 patients undergoing breast conservative surgery, from October 2004 to November 2018, treated at the Breast Unit of our institution, Azienda Ospedaliaera Sant’Andrea, Università di Roma, La Sapienza.
The present retrospective case study includes patients with early breast cancer clinically N0, submitted to primary resection surgery and sentinel lymph node biopsy. The inclusion criteria adopted acknowledged patients of any age with breast conservative surgery. The exclusion criteria did not allow patients undergoing mastectomy, patients with in situ neoplasia and patients undergoing neoadjuvant therapy.
Six hundred and eighteen patients (43%) were submitted to quadrantectomy with classical technique, according to Veronesi, with removal of the skin overlying the lesion, while the remaining 882 (57%) underwent an oncoplastic surgery technique (Periareolar, Central, lateral sulcus or real “J mammoplasty”).
All surgical specimens were marked by suture threads and metal clips in order to identify the margins of resection and to allow a correct spatial orientation.
In all surgical procedures, we performed the “Cavity Shaving” by enlarging the lateral, medial, areolar margin and the band below the lesion.
For all the surgeries carried out before 2015, performed after the Stereotassic ROLL (Radioguideded Occult Lesion Localization)16 centering of the lesion, a mammographic check of the surgical part was carried out in radiology to verify the presence of the metal clip in the excised tissue.
Since 2015, we introduced at our institution, the portable Mammographer Kubtecxpert Imager 40 Milford, allowing the performance of intraoperative radiographic control of the piece, directly in the operating room.
This has allowed us to directly assess the presence of the lesion, in the surgical piece, to evaluate its position in relation to the resection margins and to locate the side for further enlargements in case of lesion too close to a margin and to identify the metal clip in case of lesions previously subjected to Stereotassic ROLL centering.
We sent all the surgical pieces to our department of pathology for the definitive histological examination.
After surgical treatment, we subjected all patients to adjuvant therapy according to current protocols of radiation therapy, hormone therapy, chemotherapy and biological therapy.
The clinical and instrumental follow-up held in collaboration with the oncologists and radiation oncologists had a response of 1010 (70%).
Statistical analysis was performed by SPSS package (IBM®, Release 20.0.0). We considered a P<0.05 as a significant value and P<0.01 as a highly significant value.
Results
The average age of the patients examined is 58.76 (±12.24) with a minimum value of 26 years and a maximum of 89 years at the time of diagnosis. In 764 patients (53% of the total sample), the lesion was borne by the left breast. In 39.94% of the cases, the lesion was localized to Upper-Outer Quadrant, in 24.31% to Upper-Inner, in 18.33% to Lower-Outer Quadrant, in 12.08% to Lower-Inner Quadrant and the remaining 5.2% in the Central Portion (Nipple Areola Complex, NAC).
We have recorded 147 cases of “R1” in the definitive histological report (10.2%).
The evaluation of the Overall Survival in the test sample is 95% at 5 years, while at 10 years, this value drops to 89%. Comparing the Overall Survival of the R0 and R1 patients, using the Kaplan Maier method, we see that there is no statistically significant difference between the two populations measured. The R1 seem to have an earlier mortality rate than the R0, but this figure stabilizes subsequently, about 4 years after surgery, since the R1s underwent a further treatment (Figure 1).
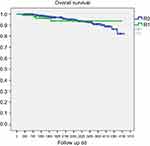 |
Figure 1 Overall survival by margins (R0= free margins, R1= positive margins) (n. s.).Abbreviations: dd, days; ns, not significant. |
If we evaluate the local recurrence rate, we see no significant statistic that differentiates the treatment of R1, with enlargement of the previous excision from mastectomy. It is evident that local recurrences are less among R1 patients, because this population of patients includes those who have undergone a secondary mastectomy.
We subjected half of the 147 R1 patients to surgery with enlargement of margins, while the other half to mastectomy. In one case, no further surgical procedures were carried out, due to the patient’s clinical condition. The condition of enlargement and subsequent mastectomy occurred very rarely and affected only 2% of the cases.
Table 1 shows the variables examined
 |
Table 1 Characteristics of the sample |
In Table 2, results of multivariate analysis are shown.
 |
Table 2 Multivariate analysis |
Conclusions
Our analysis points out age as a very significant variable in the probability of R1. This risk is greater in younger patients.
This datum can be related to a denser glandular structure, which is associated with a difficulty in diagnosing the lesion and of its extension, in addition to the higher incidence of more aggressive tumors compared to those occurring at a later age.
The location of the tumor site does not represent a statistically significant variable in the assessment of the R1.
Not even the surgical technique represents a statistically significant variable, despite the fact that we detected a higher incidence of R1 in patients undergoing oncoplastic surgery. These data probably related to the fact that we tend to use this technique more in younger patients and, as already pointed out, in these patients, the risk of R1 is higher. Moreover, we should probably relate this datum to the fact that for esthetic reasons, younger patients are generally undergoing smaller excisions.17
The histologic diameter of the lesion represents a very significant variable: greater is the lesion greater is the probability of R1.
The histologic type represents a very significant variable, confirming that the Lobular cancer has a higher probability of R1. The clinical and radiologic features of this type of lesion can explain this result. We know this from the literature, confirmed also by our case studies.18,19
Grading is a significant variable. In fact, our analysis has shown that R1 concentrates more in G2 tumors.
This result riddles us, as we would expect that the greater probability of having positive margins should occur in G3 tumors.
We can explain the prevalence of R1 in G2 tumors assuming that G3 tumors are less likely to spread locally, or have a lower intraductal component. We can also assume this category of lesions concentrate more tumors with greater systemic aggressiveness than local aggressiveness and, therefore, have a lower risk of margin positivity.
Multifocality is no doubt one of the main factors of R1. Multifocal lesions may present additional microscopic localizations, which in turn, we can identify only by histologic examination of the surgical piece.20
The molecular subtype does not represent a statistically significant variable. It is important to point out that the incidence of R1 in the Triple Negative variant is still low. We can consider this datum in the same optic of the low probability of R1 inG3 tumors. Also in this case, we are dealing with lesions that more rarely present microscopic diffusion outbreaks and a rarer intraductal component.
Lymph vascular Invasion (ex LVI, now LV1) has a significant value. Being a local way of spreading as well as lymph node, it increases the probability of R1.
The Lymph node positivity (N+) is associated with an increased risk of incurring R1, due to the more advanced state of the disease.
The multivariate data analysis with a linear statistical model confirm that there is a significant relation between young age associated to oncoplastic surgical technique and the occurrence of R1.
The datum that we did not examine but that would be interesting to assess is the risk of R1 connected to the volume of the breast affected by neoplasia. Surgery carried out with oncoplastic technique, despite the same oncological radicality, compared to the other risk factors mentioned above, could have a higher risk of R1 on a smaller breast.
By correlating the variables taken into consideration, our future aim is to create a statistical model that can assess the preoperative risk of R1. But, the variable that has the most impact is the histologic multifocality. The limit is that we can obtain this datum only after surgery, with the final histological examination of the piece.
An interesting goal could be the creation of a statistical model, correlating the magnetic resonance imaging data with the histologic multifocality, allowing a better pre-operative prediction of patients with higher risk of R1 and better selection of patients to be candidates for conservative surgery, excluding those at high risk of R1.
Ethics and consent statement
The authors declare that this is a retrospective study and it does not require approval by the Ethics Committee, but rather, only required approval by the Breast Unit Core Team Institutional Review Board (Professor Claudio Amanti, breast surgery, Professor Mattia Falchetto Osti, radiation oncology, and Professor Patrizia Pellegrini, oncology). Patient consent to review their medical records was not required by the board because all patients included in the study signed, at admission, a standard form about privacy and processing of personal data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Jobsen JJ, Riemersma S, van der Palen J, Ong F, Jonkman A, Struikmans H. The impact of margin status in breast-conserving therapy for lobular carcinoma is age related. Breast. 2018;42:3–9. Epub 2018 Jul 18. doi:10.1016/j.breast.2018.07.007
2. Darby S, McGale P, Correa C, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378:1707–1716. doi:10.1016/S0140-6736(11)60984-7
3. Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–1241. doi:10.1056/NEJMoa022152
4. Povoski SP, Jimenez RE, Wang WP, Xu RX. Standardized and reproducible methodology for the comprehensive and systematic assessment of surgical resection margins during breast-conserving surgery for invasive breast cancer. BMC Cancer. 2009;9:254. doi:10.1186/1471-2407-9-254
5. Dixon JM, Thomas J, Kerr GR, et al. A study of margin width and local recurrence in breast conserving therapy for invasive breast cancer. EJ Eur J Surg Oncol. 2016;42(5):657–664. Epub 2016 Feb 18. doi:10.1016/j.ejso.2016.02.008
6. Bland KI. Surgical margins in breast cancer: how wide? How accurate? How big? Does it make a difference? Curr Surg. 2001;58:248–253.
7. Taghian A, Mohiuddin M, Jagsi R, Goldberg S, Ceilley E, Powell S. Current perceptions regarding surgical margin status after breast-conserving therapy: results of a survey. Ann Surg. 2005;241:629–639. doi:10.1097/01.sla.0000157272.04803.1b
8. Jacobs L. Positive margins: the challenge continues for breast surgeons. Ann Surg Oncol. 2008;15:1271–1272. doi:10.1245/s10434-007-9766-0
9. Luini A, Rososchansky J, Gatti G, et al. The surgical margin status after breast-conserving surgery: discussion of an open issue. Breast Cancer Res Treat. 2009;113:397–402. doi:10.1007/s10549-008-9929-0
10. Morrow M. Margins in breast-conserving therapy: have we lost sight of the big picture? Expert Rev Anticancer Ther. 2008;8:1193–1196. doi:10.1586/14737140.8.8.1193
11. Azu M, Abrahamse P, Katz SJ, et al. What is an adequate margin for breast-conserving surgery? Surgeon attitudes and correlates. Ann Surg Oncol. 2010;17:558–563. doi:10.1245/s10434-010-1022-3
12. Moran MS, Schnitt SJ, Giuliano AE, et al. Society of surgical oncology – American Society for Radiation Oncology Consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Ann Surg Oncol. 2014;21(3):704–716. Epub 2014 Feb 10. doi:10.1245/s10434-014-3481-4
13. Chung A, Gangi A, Amersi F, Bose S, Zhang X, Giuliano A. Impact of consensus guidelines by the society of surgical oncology and the American Society for Radiation Oncology on margins for breast-conserving surgery in stages 1 and 2 invasive breast cancer. Ann Surg Oncol. 2015;22(Suppl3):S422–S427. Epub 2015 Aug 27. doi:10.1245/s10434-015-4829-0
14. Yu J, Elmore LC, Cyr AE, Aft RL, Gillanders WE, Margenthaler JA. Cost analysis of a surgical consensus guideline in breast-conserving surgery. J Am Coll Surg. 2017;225(2):294–301. Epub 2017 Apr 14. doi:10.1016/j.jamcollsurg.2017.03.020
15. Merrill AL, Coopey SB, Tang R, et al. Implications of new lumpectomy margin guidelines for breast-conserving surgery: changes in reexcision rates and predicted rates of residual tumor. Ann Surg Oncol. 2016;23(3):729–734. Epub 2015 Oct 14. doi:10.1245/s10434-015-4916-2
16. De Cicco C, Pizzamiglio M, Trifirò G, et al. Radioguided Occult Lesion Localization (ROLL) and surgical biopsy in breast cancer. Technical Aspects. QJNucl Med. 2002;46(2):145–151.
17. Mazeh H, Sagiv I, Katz D, Freund HR, Peretz T, Allweis TM. Association between patient age, volume of breast tissue excised, and local recurrence. J Surg Res. 2013;181(2):187–192. Epub 2012 Jul 4. doi:10.1016/j.jss.2012.06.043
18. Christgen M, Steinemann D, Kühnle E, et al. Lobular breast cancer: clinical, molecular and morphological characteristics. Pathol Res Pract. 2016;212(7):583–597. doi:10.1016/j.prp.2016.05.002
19. Mukhtar RA
20. Vera-Badillo FE
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
