Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Positive correlation of the serum angiopoietin-like protein 3 levels with the aortic augmentation index in patients with coronary artery disease
Authors Fu YS, Wang JH , Lee CJ , Hsu BG
Received 31 August 2017
Accepted for publication 12 December 2017
Published 5 February 2018 Volume 2018:14 Pages 231—236
DOI https://doi.org/10.2147/TCRM.S150476
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Yu-Shan Fu,1,* Ji-Hung Wang,1,2,* Chung-Jen Lee,3 Bang-Gee Hsu1,4
1School of Medicine, Tzu Chi University, Hualien, 2Division of Cardiology, Buddhist Tzu Chi General Hospital, Hualien, 3Department of Nursing, Tzu Chi University of Science and Technology, Hualien, 4Division of Nephrology, Buddhist Tzu Chi General Hospital, Hualien, Taiwan
*These authors contributed equally to this work
Purpose: Angiopoietin-like protein 3 (ANGPTL3) plays an important role in lipid metabolism and angiogenesis and is elevated in familial hypercholesterolemia, metabolic syndrome, and insulin resistance. This study aims to evaluate the relationship between the fasting serum ANGPTL3 levels and the aortic augmentation index (AIx) in patients with coronary artery disease (CAD).
Materials and methods: Fasting blood samples were obtained from 100 patients with CAD. The AIx was measured using a validated tonometry system (SphygmoCor). The serum ANGPTL3 levels were assessed using a commercial enzyme-linked immunosorbent assay kit.
Results: The aortic AIx values were higher in female patients with CAD (P=0.003) than those in male patients with CAD. The univariate linear analysis of the aortic AIx values reveals that the height (r=-0.363; P<0.001) and body weight (r=-0.350; P<0.001) were negatively correlated, whereas the age (r=0.202; P=0.044) and logarithmically transformed ANGPTL3 (log-ANGPTL3, r=0.357; P<0.001) were positively correlated with the aortic AIx values in patients with CAD. The multivariate forward stepwise linear regression analysis of the factors significantly associated with the aortic AIx revealed that the height (β=-0.269; adjusted R2 change=0.123; P=0.007) and serum log-ANGPTL3 level (β=0.259; adjusted R2 change=0.051; P=0.010) were independent predictors of the aortic AIx values in patients with CAD.
Conclusion: The fasting serum ANGPTL3 level positively correlated with the aortic AIx values among patients with CAD.
Keywords: ANGPTL3, ischemic heart disease, arterial stiffness, height, aortic augmentation index, SphygmoCor
Introduction
Angiopoietin-like proteins (ANGPTL) are a family of proteins that have similar structures as angiopoietin proteins that are reportedly involved in the regulation of lipid metabolism.1 Angiopoietin-like protein 3 (ANGPTL3) is a secretory protein regulating plasma lipid levels by affecting lipoprotein lipase- and endothelial lipase-mediated hydrolysis of phospholipids and triglycerides (TG).2 In humans, participants with heterozygous loss-of-function variants in ANGPTL3 had significantly lower serum levels of TG, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) than participants without these variants.3
Arterial stiffness results from a degenerative process affecting mainly the extracellular matrix of elastic arteries under the effect of aging and atherosclerosis, changes in the elastic elements of the arterial wall, endothelial dysfunction, and inflammation.4 Moreover, arterial stiffness and dyslipidemia are crucial determinants of cardiovascular risk.5 The aortic augmentation index (AIx) is a measure of pulse wave reflection that calculates the central pulse pressure accounted for by the reflected pulse wave and is often referred to as a marker of arterial stiffness.6 Some studies have suggested that the aortic AIx is significantly related to the degree of coronary artery disease (CAD).7,8 Therefore, this study aimed to examine the aortic stiffness by assessing the aortic AIx and serum ANGPTL3 in patients with CAD.
Materials and methods
Patients
Between March and December 2012, 115 patients with CAD (CAD was defined as >50% stenosis in any segment by coronary angiography by medical record) in a medical center in Hualien, eastern Taiwan were enrolled; 15 participants were excluded because of acute infection (n=2); pulmonary edema (n=1); use of calcium, active vitamin D metabolites, bisphosphonates, teriparatide, or estrogens medication (n=5); and refusal to provide informed consent (n=7). Finally, a total of 100 CAD patients (74 males and 26 females) were enrolled in this study. The Protection of the Human Subjects Institutional Review Board of Tzu Chi University and Hospital (Hualien, Taiwan) approved this study. Informed written consent was obtained from all patients before their enrollment in this study. Trained staff members measured the blood pressure (BP) of all participants in the morning, using standard mercury sphygmomanometers with appropriate cuff sizes after the participants had been sitting for at least 10 min. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were taken at the points of appearance and disappearance, respectively. Hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg or prescription of antihypertensive medication in the past 2 weeks. A person was regarded as diabetic if the fasting plasma glucose was either 126 mg/dL or more or if he/she was using diabetes medication (oral or insulin).9
Anthropometric analysis
Patient’s weight was measured in light clothing and without shoes to the nearest 0.5 kg, and the height was assessed to the nearest 0.5 cm. The body mass index was calculated as the weight in kilograms divided by the height in meters squared.10–12
Biochemical investigations
After 8–12 h overnight fasting, blood (~5 mL) of all participants was sampled in the morning, of which ~0.5 mL was used to determine hemoglobin and white blood cells count (Sysmex K-1000; Sysmex America, Mundelein, IL, USA); the remainder was immediately centrifuged at 3,000× g for 10 min. The serum levels of blood urea nitrogen (BUN), creatinine (Cre), fasting glucose, total cholesterol, TG, HDL-C, LDL-C, total calcium, and phosphorus were measured using an autoanalyzer (COBAS Integra 800; Roche Diagnostics, Basel, Switzerland).10–12 The serum ANGPTL3 (R&D Systems, Inc., Minneapolis, MN, USA) and intact parathyroid hormone (iPTH; Diagnostic Systems Laboratories, Webster, TX, USA) concentrations were quantified using commercial enzyme-linked immunosorbent assay.11–13 The estimated glomerular filtration rate (eGFR) was calculated by the Chronic Kidney Disease Epidemiology Collaboration equation.
Pulse wave analysis and AIx assessment
The pulse wave analysis and AIx assessment were arranged on the same day after blood sampling and not necessarily in fasting status. Patients were positioned supine and allowed to rest for 10 min before the test was performed. Although the consumption of food, drink, alcohol, or tobacco was not restricted, patients were not allowed to sleep or talk during the testing procedure. The pulse wave analysis by applanation tonometry was performed on the right radial artery and analyzed by the SphygmoCor software (SphygmoCor system; AtCor Medical, Australia), which also calculates a number of major indices including the aortic AIx.6,11,12
Statistical analysis
Normally distributed data were expressed as the mean ± SD and comparisons between patients were performed using the Student’s independent t-test (two-tailed). Data not normally distributed were expressed as medians and interquartile ranges. The TG, glucose, BUN, Cre, and ANGPTL3 data sets revealed skewed non-normal distributions and therefore were recalculated by transformation to the logarithm to the base 10; after this transformation, the log-TG, -glucose, -BUN, -Cre, and -ANGPTL3 exhibited a normal distribution. The clinical variables that correlated with the aortic AIx values in patients with CAD were evaluated using the univariate linear regression analysis first. However, the variables that were significantly associated with the aortic AIx in patients with CAD were tested for independence by the multivariate forward stepwise regression analysis (adapted factors: age, sex, height, body weight, and log-ANGPTL3). All data were analyzed using the SPSS for Windows (version 19.0; SPSS Inc., Chicago, IL, USA). P<0.05 was considered statistically significant.
Results
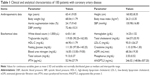
The demographic, biochemical, and clinical characteristics of 100 patients with CAD are shown in Tables 1 and 2. Patients’ medical histories included diabetes mellitus (n=47; 47.0%) and hypertension (n=77; 77.0%). The use of drugs included angiotensin-converting enzyme inhibitor (ACEI; n=30; 30.0%), angiotensin-receptor blocker (ARB; n=39; 39.0%), calcium-channel blocker (CCB; n=32; 32.0%), β blocker (n=57; 57.0%), statins (n=66; 66.0%), and fibrate (n=14; 14.0%). The aortic AIx values in female patients with CAD (P=0.003) were higher that than in male patients with CAD. No statistically significant difference based on ACEI, ARB, β blocker, CCB, statins, or fibrate use in the aortic AIx values was noted.
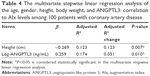
Table 3 shows the univariate linear regression analysis of the aortic AIx values for patients with CAD. In participants of this study, the height (r=−0.363; P<0.001) and body weight (r=−0.350; P<0.001) were negatively correlated with the aortic AIx, whereas the age (r=0.202; P=0.044) and logarithmically transformed ANGPTL3 (log-ANGPTL3, r=0.357; P<0.001) were positively correlated with the aortic AIx. The variables that were significantly associated with the aortic AIx values (adapted factors: age, sex, height, body weight, and log-ANGPTL3) were analyzed using the multivariate forward stepwise linear regression analysis, which revealed that the height (β=−0.269; adjusted R2 change=0.123; P=0.007) and serum log-ANGPTL3 level (β=0.259; adjusted R2 change=0.051; P=0.010) were independent factors that were associated with the aortic AIx in our patients with CAD (Table 4).
Discussion
This study suggests that the age, female sex, and fasting serum ANGPTL3 level positively correlated with the aortic AIx values among patients with CAD. Conversely, the height and body weight were negatively correlated with the aortic AIx values. The height and serum log-ANGPTL3 level were independent factors associated with the aortic AIx values in our patients with CAD after adjustment for the age, sex, and body weight.
Several studies have suggested that the aortic AIx values were inversely correlated with height and were higher in females.14–17 Reportedly, arterial wave reflections occur later in taller individuals because the distance from the heart to the reflection point is longer, causing greater time of reflection in taller people.7 This assertion could explain the reason why the AIx value was consistently higher in women than that in men.14–17 The aortic AIx value is also higher in girls than that in boys at 14 years and is closely associated with the change in the height between 8 and 14 years in adolescents.18 Reeve et al noted that taller individuals had more favorable central hemodynamics and reduced evidence of CAD compared with those of shorter individuals.19 The results of our study revealed that female patients with CAD had higher aortic AIx values, and height is negatively associated with the aortic AIx values in patients with CAD. After the adjustment of other factors, such as gender, the multivariate forward stepwise linear regression analysis showed that the height was negatively associated with the aortic AIx values in patients with CAD.
With aging, the vasculature undergoes structural and functional changes characterized by vascular fibrosis and arterial stiffening.20 The aortic AIx values were significantly and independently associated with the age.17,21 Our results also noted that the age is positively associated with the aortic AIx values in patients with CAD. In patients with chronic kidney disease, body weight is inversely associated with the aortic AIx values.22 Furthermore, weight loss was significantly and independently associated with each reduction in the aortic AIx values after a 12-week training program among Japanese elderly persons.23 However, weight loss induced by energy restriction did not improve the aortic AIx values in a systematic review and meta-analysis of clinical trials involving adult subjects.24 Another study identified that changes in the AIx values were related to changes in the abdominal fat and total body fat percent when adjusted for gender and relevant baseline confounders.25 Although this study noted that body weight is negatively associated with the aortic AIx values in patients with CAD, future research is required to prove this finding.
Hyperlipidemia is associated with reduced nitric oxide bioavailability and endothelial dysfunction, which may lead to the increase in the aortic AIx values and arterial stiffness.26 The aortic AIx value was significantly higher in patients in the hypercholesterolemia group.27 Moreover, patients with hypercholesterolemia have stiffer blood vessels than matched controls, and the hemodynamic change might contribute to the increased risk of cardiovascular disease.4 ANGPTL3 regulates the TG metabolism by reversibly inhibiting the lipoprotein lipase activity.1 ANGPTL3 deficiency causes enhanced activity of lipoprotein lipase in the muscle and adipose tissue and accelerates the clearance of TG-rich lipoproteins. The decreased lipolysis in adipose tissue results in a scarcity of free fatty acid substrates for hepatic de novo synthesis of TG and cholesterol, and, consequently, decreased lipidation of very low-density lipoprotein cholesterol.2 In an animal study, ANGPTL3 deficiency and the resulting hypolipidemia were protective against the development of atherosclerosis.2 In human studies, ANGPTL3 deficiency is associated with the protection from CAD.3,28 Therapeutic antagonism of ANGPTL3 (evinacumab) in humans caused a dose-dependent placebo-adjusted reduction in fasting TG levels of up to 76% and LDL-C levels of up to 23%.3 In contrast, the aortic AIx value was shown to be significantly correlated with cardiovascular risk.29,30 The results of our study further confirmed that the serum ANGPTL3 level was also positively associated with the aortic AIx values in patients with CAD after the adjustment of other confounders.
Limitations
There are limitations of this study that need to be highlighted. First, the sample size is small. Perhaps, larger study groups of patients with CAD could increase the accuracy of results. Second, this study was an observational study; therefore, further longitudinal studies are needed before a cause–effect relationship between the serum ANGPTL3 level and the aortic AIx value can be established in patients with CAD. In addition, the use of medication for hypertension may affect the AIx values. Studies have noted that the use of ACEIs or statins has a beneficial effect on the aortic AIx value, which is independent of BP reduction or LDL-C changes.31,32 The results of this study did not demonstrate a correlation between antihypertensive drugs, statins, or fibrates used with the aortic AIx values in patients with CAD. Finally, current smoking33 and smoking pack years34 may affect aortic AIx values. Further studies are required to elucidate the relationship between aortic AIx values and smoking and serum ANGPTL3 level in CAD patients.
Conclusion
Our study reveals that the fasting serum ANGPTL3 level positively correlated with the aortic AIx values, whereas the height negatively correlated with the aortic AIx values among patients with CAD. Further prospective studies are needed to confirm the mechanisms underlying this association.
Acknowledgment
This study was supported by a grant from the Buddhist Tzu Chi General Hospital, Hualien, Taiwan (TCRD101-03).
Author contributions
YSF, BGH, and JHW conceived and designed the experiments. CJL and JHW performed the experiments. BGH and CJL analyzed the data. YSF, BGH, and JHW wrote the manuscript. All of the authors reviewed and approved the final version of this paper. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Li Y, Teng C. Angiopoietin-like proteins 3, 4 and 8: regulating lipid metabolism and providing new hope for metabolic syndrome. J Drug Target. 2014;22:679–687. | ||
Tikka A, Jauhiainen M. The role of ANGPTL3 in controlling lipoprotein metabolism. Endocrine. 2016;52:187–193. | ||
Dewey FE, Gusarova V, Dunbar RL, et al. Genetic and pharmacologic inactivation of ANGPTL3 and cardiovascular disease. N Engl J Med. 2017;377:211–221. | ||
Palombo C, Kozakova M. Arterial stiffness, atherosclerosis and cardiovascular risk: pathophysiologic mechanisms and emerging clinical indications. Vascul Pharmacol. 2016;77:1–7. | ||
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–2219. | ||
Butlin M, Qasem A. Large artery stiffness assessment using sphygmocor technology. Pulse. 2017;4:180–192. | ||
Janner JH, Godtfredsen NS, Ladelund S, et al. Aortic augmentation index: reference values in a large unselected population by means of the SphygmoCor device. Am J Hypertens. 2010;23:180–185. | ||
Choi J, Kim SY, Joo SJ, Kim KS. Augmentation index is associated with coronary revascularization in patients with high Framingham risk scores: a hospital-based observational study. BMC Cardiovasc Disord. 2015;15:131. | ||
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. I. Diagnosis and classification of diabetes mellitus: provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. | ||
Hsu BG, Chen YC, Lee RP, Lee CC, Lee CJ, Wang JH. Fasting serum level of fatty-acid-binding protein 4 positively correlates with metabolic syndrome in patients with coronary artery disease. Circ J. 2010;74:327–331. | ||
Hsu BG, Lee CJ, Chen YC, Ho GJ, Lin TY, Lee MC. Serum osteoprotegerin levels associated with aortic augmentation index in renal transplant recipients. Tzu Chi Medical Journal. 2016;28:20–23. | ||
Tsai JP, Wang JH, Chen ML, Yang CF, Chen YC, Hsu BG. Association of serum leptin levels with central arterial stiffness in coronary artery disease patients. BMC Cardiovasc Disord. 2016;16:80. | ||
Chung HS, Lee MJ, Hwang SY, et al. Circulating angiopoietin-like protein 8 (ANGPTL8) and ANGPTL3 concentrations in relation to anthropometric and metabolic profiles in Korean children: a prospective cohort study. Cardiovasc Diabetol. 2016;15:1. | ||
Ayer JG, Harmer JA, Marks GB, Avolio A, Celermajer DS. Central arterial pulse wave augmentation is greater in girls than boys, independent of height. J Hypertens. 2010;28:306–313. | ||
Hughes AD, Park C, Davies J, et al. Limitations of augmentation index in the assessment of wave reflection in normotensive healthy individuals. PLoS One. 2013;8:e59371. | ||
Torjesen AA, Wang N, Larson MG, et al. Forward and backward wave morphology and central pressure augmentation in men and women in the Framingham Heart Study. Hypertension. 2014;64:259–265. | ||
Wilenius M, Tikkakoski AJ, Tahvanainen AM, et al. Central wave reflection is associated with peripheral arterial resistance in addition to arterial stiffness in subjects without antihypertensive medication. BMC Cardiovasc Disord. 2016;16:131. | ||
Barraclough JY, Garden FL, Toelle B, et al. Sex differences in aortic augmentation index in adolescents. J Hypertens. 2017;35:2016–2024. | ||
Reeve JC, Abhayaratna WP, Davies JE, Sharman, JE. Central hemodynamics could explain the inverse association between height and cardiovascular mortality. Am J Hypertens. 2014;27:392–400. | ||
Harvey A, Montezano AC, Lopes RA, Rios F, Touyz RM. Vascular fibrosis in aging and hypertension: molecular mechanisms and clinical implications. Can J Cardiol. 2016;32:659–668. | ||
Tsuru T, Adachi H, Enomoto M, et al. Augmentation index (AI) in a dose-response relationship with smoking habits in males: the Tanushimaru study. Medicine. 2016;95:e5368. | ||
Afsar B, Elsurer R, Soypacaci Z, Kanbay M. The relationship between weight, height and body mass index with hemodynamic parameters is not same in patients with and without chronic kidney disease. Clin Exp Nephrol. 2016;20:77–86. | ||
Kawamoto R, Kohara K, Katoh T, et al. Effect of weight loss on central systolic blood pressure in elderly community-dwelling persons. Hypertens Res. 2014;37:933–938. | ||
Petersen KS, Clifton PM, Lister N, Keogh JB. Effect of weight loss induced by energy restriction on measures of arterial compliance: a systematic review and meta-analysis. Atherosclerosis. 2016;247:7–20. | ||
Hvidt KN, Olsen MH, Ibsen H, Holm JC. Weight reduction and aortic stiffness in obese children and adolescents: a 1-year follow-up study. J Hum Hypertens. 2015;29:535–540. | ||
Chung JW, Lee YS, Kim JH, et al. Reference values for the augmentation index and pulse pressure in apparently healthy Korean subjects. Korean Circ J. 2010;40:165–171. | ||
Wilkinson IB, Prasad K, Hall IR, et al. Increased central pulse pressure and augmentation index in subjects with hypercholesterolemia. J Am Coll Cardiol. 2002;39:1005–1011. | ||
Stitziel NO, Khera AV, Wang X, et al. ANGPTL3 deficiency and protection against coronary artery disease. J Am Coll Cardiol. 2017;69:2054–2063. | ||
Nürnberger J, Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schafers RF. Augmentation index is associated with cardiovascular risk. J Hypertens. 2002;20:2407–2414. | ||
Patvardhan E, Heffernan KS, Ruan J, et al. Augmentation index derived from peripheral arterial tonometry correlates with cardiovascular risk factors. Cardiol Res Pract. 2011;2011:253758. | ||
Mallareddy M, Parikh CR, Peixoto AJ. Effect of angiotensin-converting enzyme inhibitors on arterial stiffness inhypertension: systematic review and meta-analysis. J Clin Hypertens. 2006;8:398–403. | ||
Sahebkar A, Pećin I, Tedeschi-Reiner E, Derosa G, Mafioli P, Reiner Ž. Effects of statin therapy on augmentation index as a measure of arterial stiffness: a systematic review and meta-analysis. Int J Cardiol. 2016;212:160–168. | ||
Sluyter JD, Hughes AD, Thom SA, et al. Arterial waveform parameters in a large, population-based sample of adults: relationships with ethnicity and lifestyle factors. J Hum Hypertens. 2017;31:305–312. | ||
Mozos I, Maidana JP, Stoian D, Stehlik, M. Gender differences of arterial stiffness and arterial age in smokers. Int J Environ Res Public Health. 2017;14:E565. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.