Back to Journals » Drug Design, Development and Therapy » Volume 16
Population Pharmacokinetics of Tigecycline: A Systematic Review
Authors Zhou CC, Huang F, Zhang JM, Zhuang YG
Received 11 March 2022
Accepted for publication 4 June 2022
Published 17 June 2022 Volume 2022:16 Pages 1885—1896
DOI https://doi.org/10.2147/DDDT.S365512
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Tuo Deng
Can-Can Zhou,1,* Fang Huang,1,* Jing-Ming Zhang,1 Yu-Gang Zhuang2
1Department of Pharmacy, Shanghai Tenth People’s Hospital, School of Medicine, Tongji University, Shanghai, 200072, People’s Republic of China; 2Department of Emergency Medicine, Shanghai Tenth People’s Hospital, School of Medicine, Tongji University, Shanghai, 200072, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yu-Gang Zhuang, Email [email protected]
Abstract: Although tigecycline is widely used in clinical practice, its efficiency and optimal dosage regimens remain controversial. The purpose of this article was to help guide tigecycline dosing in different patient subpopulations through comparing the published population pharmacokinetic models of tigecycline, as well as summarizing and determining the potential covariates that markedly influence tigecycline pharmacokinetics. In this review, literature was systematically searched from the PubMed database from inception to March 2022. The articles focusing on population pharmacokinetics for tigecycline in healthy volunteers or patients were included; finally, a total of eight studies were included in this review. NONMEM methods were used in five studies to generate the population pharmacokinetic models. Tigecycline pharmacokinetics were mostly described by a two-compartment model in these included studies. Estimated clearance and volumes of distribution of tigecycline at steady state (Vss) varied widely in different target patient populations, with a range of 7.5– 23.1 L/h and 212.7– 1087.7 L, respectively. Body-weight and creatinine clearance were the most important predictors of clearance in these studies, while other predictors include age, gender, bilirubin and aspartate aminotransferase. In conclusion, this review showed the large variability of tigecycline population pharmacokinetics, which can provide guide dosing in different target populations. For clinicians, the individual dosing adjustment should be based not only on the indication and pathogen susceptibility but also on the potential important predictors. However, more studies were needed to confirm the necessity of modified dosage regimens in different patient subpopulations.
Keywords: tigecycline, population pharmacokinetics, modelling, NONMEM
Introduction
Tigecycline, an antimicrobial agent of glycylcycline class, is approved to treat complicated skin and skin structure infections, complicated intra-abdominal infections, and community-acquired pneumonia by the Food and Drug Administration in America since June 2005.1 The primary mechanism of tigecycline is to bind to a helical region (H34) on the 30S subunit of bacterial ribosomes and inhibit bacterial protein translation.2 Hence, tigecycline possesses high activities against gram-positive, almost all the gram-negative and anaerobic microorganisms.3,4 Due to its broad-spectrum antibacterial activities, tigecycline has been considered as one of the most important agents for treating complicated multi-drug resistant pathogen infections.
The recommended standard dose of tigecycline is a 100 mg starting dose, followed by 50 mg twice daily. Tigecycline has an extensive tissue distribution in the body, as its distribution volume ranges from 7 to 10 L/kg. Systemic clearance and the elimination half-life for tigecycline range from 0.2 to 0.3 L/h/kg and 37 to 67 hours, respectively.3 Tigecycline can highly combine with plasma proteins and exhibit atypical non-linear protein binding. AUC/MIC is considered as the most optimal parameter for pharmacokinetic/pharmacodynamic (PK/PD) to predict the efficacy of tigecycline.5 In vitro, it was suggested that tigecycline exhibits excellent activities against most Gram-positive and Gram-negative pathogens. Yaghoubi et al reported that tigecycline showed a prolonged postantibiotic effect and displayed a time-dependent bactericidal activity in a 3 mg/kg dose.6 Compared with tetracycline, tigecycline was more effective for the Enterococcus faecalis ATCC47077 (a tetracycline-susceptible pathogen).7 However, the efficacy of standard dose tigecycline in clinical application is still controversial. Several studies recently reported that the recommended standard dose of tigecycline exerted insufficient antimicrobial activities in different target patient populations.8,9 A higher dosage of tigecycline (100 mg twice daily) was related to better outcomes in HAP patients.10 A higher dosage of tigecycline could also achieve a better cure rate and be associated with better outcomes in critically ill patients with multidrug-resistant bacteria infection.11 Therefore, optimizing the dosage of tigecycline to improve its efficacy in different target patient population is still need to be clarified.
Recently, the FDA issued a black boxed warning and illustrated that treatment with tigecycline increased the risk of death in FDA-approved and non-approved diseases.12 Several clinical studies have shown that the use of tigecycline was related to higher mortality than other comparator antibiotics.13–15 A meta-analysis also demonstrated that compared with the control groups, the clinical response and mortality in the tigecycline-treated group showed no difference. Tigecycline could not induce better outcomes when compared with other antibiotics in treating complicated multi-drug-resistant pathogen infections, and the mortality in the tigecycline-treated group was even higher than others. Therefore, Ni et al concluded that the use of tigecycline might not be the best choice.16 However, the potential reason for this higher mortality is still unknown. Freire et al attributed the increased risk of death to suboptimal tigecycline dosing.17 Therefore, the FDA advised that tigecycline should be used only in situations when other treating methods are not suitable.10,11 However, due to its strong antimicrobial activities and lack of other effective antimicrobials, tigecycline is still used in complicated multi-drug-resistant pathogen infections as the antibiotic of last resort.
Population pharmacokinetics provided clinicians a useful method to investigate pharmacokinetic variability in different patient subpopulations and to determine covariates that influence drug pharmacokinetics. To decrease the potential adverse reactions of the tigecycline and maintain its efficacy, the population pharmacokinetics of tigecycline has been studied in different target patient populations, including intensively sampled volunteers and sparsely sampled patients. This review aims to comprehensively summarize all population pharmacokinetics analyses of tigecycline (from inception to March 2022). In this review, we systemically compared the population pharmacokinetic models of tigecycline and explored the potential covariates that might influence the pharmacokinetic models.
Materials and Methods
Search Strategy
Literature collected for the review was systematically searched from the PubMed database from inception to March 2022. The following search terms were employed: tigecycline AND (population pharmacokinetic OR pharmacokinetic analysis OR pharmacokinetic model OR NONMEM OR non-linear mixed effect model). All articles were reviewed and double-checked.
Inclusion and Exclusion Criteria
The articles focusing on population pharmacokinetic for tigecycline in healthy or patients could be included as it met the following criteria: (1) Study population in literatures should be human; (2) The administration of tigecycline should be intravenous injection; (3) The analysis method used in the study should be population pharmacokinetic analysis; (4) Original data were used; and (5) The language of the study should be published in English.
Excluded criteria used in this review were as follows: (1) The articles were in vitro or animal studies; (2) The articles were meta-analysis, methodology, and review articles; and (3) The population PK modeling approach was not used.
Data Extraction
All the literature that met the inclusion criteria was collected and the relevant information was extracted. For example, the first authors, the publication year, the country of the study, the characteristics of the population (including the number of patients (male/female), type of the special population, age, body-weight, creatinine clearance, and the levels of albumin), study clinical protocol (including the type of study (retrospective/prospective), the dosage of tigecycline supplementation, the time point, the frequency of sampling, the quantification methods of tigecycline, lower limit of quantification, the instrument used, the population pharmacokinetic modeling methods and techniques (including software used in the studies, the methods of evaluation, and covariate selection strategies), as well as the PopPK models and covariates analysis (including the final formula of PopPK structural and the values of related parameters, the covariates were tested and preserved).
Results
Literature Collection
A total of 169 potentially relevant articles were obtained when the search strategies were performed, of which 30 remained after scanning abstract and title. After the full-text assessment, eight of them met the inclusion criteria and were included in this review (Figure 1).18–25 The characteristics of the relevant eight articles are summarized in Table 1. The patients included in this review were from five countries. Specifically, the patients in two studies were from China, the patients in two studies were from the USA, while the patients in one study were from Poland, Germany, and Spain, respectively. The year of publication range from 2007 to 2022. The number of patients included in these eight studies varied widely, and ranged from 11 patients (Broeker et al) to 410 patients (Rubino et al). Furthermore, the type of population recruited in these studies included healthy volunteers, the patients with intra-abdominal infections, the patients with community or hospital-acquired pneumonia, the patients with sepsis or septic shock, the patients with complicated intra-abdominal or skin and skin structure infections, and the patients with cirrhosis.
 |
Table 1 Summary of Patients’ Demographics for All Population-Pharmacokinetic Studies Included in This Review |
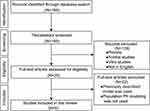 |
Figure 1 The selection process of the studies included in the systematic review. |
Study Designs and Analysis Methods
These studies collected in the present review contain five prospective studies (Broeker et al, Agnieszka et al, Xie et al, Zhou et al, and Bastida et al) and three retrospective studies (Rubino et al, Van Wart et al and Van Wart et al). Although the recommended standard dose of tigecycline is a 100 mg starting dose, followed by 50 mg twice daily; however, the dosage of tigecycline in these studies included in the review varied. The tigecycline administration route in five of the studies was by an intravenous infusion in standard dosage (100 mg loading, 50 mg q12h) or lower (50 mg loading, 25 mg q12h), and the tigecycline in one study conducted by Van Wart et al was administered by intravenous infusion in a single (12.5–300 mg) or multiple (25–100 mg, q12h) dosages. The only exception was conducted by Agnieszka et al who showed that the tigecycline was administered by intravenous infusion in higher dosage (200 mg loading, 100 mg q12h).24 Besides, in Bastida’s study, the dosage of tigecycline administration was not provided.25 The time of samples collection in patients in these eight studies varied widely, for example, in Broeker’s study, arterial blood samples were collected as follows: 0 (before the start of infusion), after the end of infusion (1, 1.25, 1.5, 1.75, 2, 4, 6, 8, and 12 h), while Zhou et al reported that the blood samples were obtained before the ninth dose of tigecycline and at 0, 3, and 8 h after the end of infusion.18,23 To quantify tigecycline concentrations in these samples, the high-performance liquid chromatography and liquid chromatography method with tandem mass spectrometer detection systems were used in these studies. The general characteristics of the clinical protocols for studies are summarized in Table 2.
 |
Table 2 Summary of the Clinical Protocols for Studies Included in This Review |
Population Pharmacokinetic Analysis
As shown in Table 3, NONMEM methods were used in five of these studies to analyze data and generate the population pharmacokinetic models.20,21,23–25 Phoenix NLME, ADAPT, and R software were also used in the study of Zhou et al, Rubino et al, and Xie et al, respectively.18,19,22 Bootstrapping analysis, an internal evaluation method was used in five studies, external evaluations were used in two studies, and one study reported no information on the validations. The best way for modeling population pharmacokinetics of tigecycline was the two-compartmental model in seven analyses; however, three-compartment models were found to be more suitable to describe the subjects obtained single or multiple doses of tigecycline in the study of Van Wart et al20
 |
Table 3 Population Pharmacokinetic Modeling Methods, Tested and Retained Covariates by the Studies Included in the Review |
Several covariates were tested in the models including age, sex, race, body-weight, etc in different subpopulations (Table 3). In our review, the model evaluation in these studies was conducted through basic internal approaches such as goodness of fit, and advanced internal approaches such as bootstrap and visual predictive check. Age was tested as a covariate in all the studies included in our review, and only one study showed that age could affect tigecycline clearance.18 The influence of sex as a covariate on tigecycline clearance was tested in five studies; however, it was only included in the final model in one study.20 Body-weight is also one of the significant covariates on tigecycline clearance, and six of the studies tested it. In two of these studies, the tigecycline clearance is increased with increasing body-weight.18,20 However, no significant effect of body-weight has been found in other four studies. Furthermore, although the covariate creatinine clearance was only included in five population pharmacokinetic models, two studies showed a significant effect of creatinine clearance on tigecycline.20,22 Interestingly, Bastida et al recently reported that Model for End-stage Liver Disease (MELD) score and total serum proteins significantly influenced the clearance of tigecycline in critically ill patients with decompensated cirrhosis and severe infections.25 In addition, other significant covariates on tigecycline clearance included BMI, body surface area, bilirubin, and aspartate aminotransferase.
Clearance and Volume of Distribution
In the final population pharmacokinetic models of these studies included in the review, the clearance of tigecycline ranged from 7.50 to 23.1 L/h. The clearance of tigecycline and between-subjects variability of the included studies is presented in Figure 2. High tigecycline clearance was observed in the following subpopulations: patients with hospital-acquired pneumonia in China, patients with sepsis or septic shock in Poland, patients with community or hospital-acquired pneumonia in the USA, and patients with intra-abdominal infections receiving either continuous veno-venous hemodialysis or hemodiafiltration in Germany. However, the clearance of tigecycline in the lower spectrum was also observed in one study in critically ill patients with severe infections in China.19
 |
Figure 2 Tigecycline clearance and between-subjects variability of the included studies. |
In the studies included in the review, the estimated volumes of distribution varied widely. When detecting the total volume of distribution, the lowest was 212.7 L, which was estimated in patients with intra-abdominal infections receiving either continuous veno-venous hemodialysis or hemodiafiltration in the study of Broeker et al23 Among the estimated total volume of distribution (Vss), the two highest were 1087.7 L and 759 L in healthy volunteers administering as multiple doses and patients with complicated intra-abdominal or skin and skin structure infections in the studies of Van Wart et al and Van Wart et al, respectively20,21 (Table 4).
 |
Table 4 A Summary of Final Models, Fixed and Random Effect Models Described in the Included Studies |
Discussion
Tigecycline, a crucial antibiotic, has been widely used as one of the agents for the treatment of complicated multi-drug-resistant pathogen infections. In clinical studies, the dosage of tigecycline should be carefully adjusted. The recommended standard dose of tigecycline is a 100 mg loading dose, followed by 50 mg twice daily; however, it is widely defined that the recommended dosing regimen is insufficient to treat MDR bacteria infections.6 Meanwhile, the adverse drug reactions of tigecycline also need to be carefully monitored.26 Thus, numerous studies on tigecycline PK have been conducted and several population pharmacokinetic models have also been investigated since 2006 to ascertain the appropriate dosing in different target patient populations. To the best of our knowledge, this is the first review to summarize the literature knowledge on population pharmacokinetics of tigecycline.
The present review included eight different population pharmacokinetic analyses, which were conducted in four countries from 2006 to 2022. NONMEM is one of the softwares widely used in population pharmacokinetic modeling.27 In the studies included in this review, NONMEM was used in five of the studies to identify relevant covariates and optimize the dosage of tigecycline in the respective subpopulation and almost all the studies showed that tigecycline PK with two-compartment models were more precise and adequate. The trends of PK estimates (clearance and volumes of distribution) between different target patient populations were not observed. The estimated clearance and volumes of distribution (V1) of tigecycline varied widely in different target patient populations, with a range of 7.5–23.1 L/h and 23.9–162 L, respectively. However, in view of the difference between respective subpopulations, the study designs, the sample sizes, sampling time, and methods of covariates modeling, the interpretation of such ranges should be cautious and more investigation is required.
Most of the studies collected in the present review were conducted as prospective studies in special subpopulations, including critically ill patients with intra-abdominal infections, sepsis or septic shock, critically ill patients with severe infections and hospital-acquired pneumonia, as well as critically ill patients with decompensated cirrhosis and severe infections. Furthermore, according to the purpose of these studies, many aimed at investigating the relationships between tigecycline treatment and the clinical response as well as optimizing tigecycline dosage in the respective subpopulation. Insufficient sample size and representativity of samples might be limitations for these studies; therefore, the capability to evaluate parameters and detect significant covariates might be confined. Besides, the studies include in this review mostly measured the levels of tigecycline in plasma, which may not necessarily reflect concentrations at the target site. Stepwise covariates selection was the most commonly reported method. A large of different covariates were evaluated and age, sex, body-weight as well as creatinine clearance were identified as the most significant covariates in these studies.
With regard to the covariates, the age of the patients was tested as a covariate in all of the studies included in our review, and only one study showed that the age was associated with the PK parameters of tigecycline in patients (age range: 18–89 years) with HAP. Besides, the influence of age on the tigecycline has also been demonstrated in previous studies. Muralidharan et al reported that there were no significant differences in tigecycline pharmacokinetic parameters in different age groups (age: 18–50 vs 65–75 vs >75 years) in healthy subjects.28 However, higher potential adverse events would be observed in older age groups (age range: >65 years).29 Meanwhile, Liu et al also found that elderly patients (age range: 77.09 ± 15.11 years) were more prone to developing hypofibrinogenemia after the administration of tigecycline.30 The reason for the differences among these studies may be due to the different health status and age distribution of the subjects selected in these studies. In clinical practice, tigecycline is usually used to treat life-threatening infections in elderly patients. This might also be explained by decreased liver blood flow, the changed metabolism of drug binding, and distribution with advanced age.
The associations between sex and tigecycline PK parameters were investigated in five studies. In Van Wart et al’s study, the clearance of tigecycline was significantly related to sex in patients with complicated intra-abdominal or skin and skin structure infections and they found that males had a higher clearance of tigecycline as compared to females.20 It is well known that tigecycline is extensively distributed to the bone, and bone mass in males was significantly higher than in females; therefore, higher bone mass in males may influence the redistribution of tigecycline. Consistently, the AUC0–24 in young women was approximately 21% higher than that in young men after a single dose of tigecycline exposure.28 Interestingly, in the recent study, Fan et al also reported that females had a higher risk due to their greater accumulation of tigecycline than males.31 However, they did not observe a difference in another study in healthy volunteers.28 Meanwhile, no correlation with sex was found in the other four studies included in this review. The potential reason for these contradictory results may be due to insufficient sample sizes and the diversity of patients.
The effects of body-weight as a covariate in patients on the pharmacokinetic parameters of tigecycline have been studied. Zhou et al reported that the weight of the patients with hospital-acquired pneumonia was related to the increased central volume of distribution and tigecycline clearance.18 Van Wart et al observed that the clearance of tigecycline in patients with cIAI or cSSSI was significantly influenced by body-weight.20 Consistent with these studies, Xie et al also found that a larger BMI was associated with increased clearance of tigecycline in critically ill patients, while the final model was not provided and no obese subjects with PK data available for inclusion in their analysis.19 Furthermore, Rubino et al demonstrated that the body surface area was one of the significant predictors of interindividual variability on clearance.22 In contrast, no significant difference was obtained in another four studies. Meanwhile, the study of Pai et al reported that there was no difference in the clearance and volume of distribution between the obese and normal-weight healthy adults.32 Therefore, the importance of body-weight, body size, and BMI in the pharmacokinetics of tigecycline still needs to be investigated.
The parameters associated with liver functions, such as MELD score, bilirubin, aspartate aminotransferase, alkaline phosphatase, and/or alanine aminotransferase were also considered as covariates in some studies. In one study, the impact of bilirubin on tigecycline clearance was demonstrated.23 Another study also recognized bilirubin as a crucial covariate, even though it was not included in the final model.20 In addition, in Zhou et al’s study, they tested the association between total bilirubin, direct bilirubin, and tigecycline clearance, while no significant differences were detected.18 However, they observed that the levels of aspartate aminotransferase, but not alkaline phosphatase and alanine aminotransferase were associated with decreased clearance in patients. Recently, the effects of liver functions on the pharmacokinetics of tigecycline were also investigated. Alraish et al found that compared with the patients with normal liver functions, the levels of tigecycline in plasma were remarkably higher in patients with severe liver failure.33 In Van Wart et al study, there was no association between parameters associated with liver functions (bilirubin, aspartate aminotransferase, alkaline phosphatase and/or alanine aminotransferase) and the pharmacokinetics of tigecycline.20 However, due to the complication of liver functions, which might be influenced by many factors. The effects of liver functions parameters on the pharmacokinetics of tigecycline still need to investigate with a larger sampling.
The renal function such as creatinine clearance and/or serum creatinine concentration also influenced the pharmacokinetic parameters of tigecycline in patients. Therefore, in some studies, these renal function indexes were also analyzed as covariates. In one study, creatinine concentrations were found to be able to influence tigecycline clearance.18 Moreover, another two studies found a close correlation between creatinine clearance and tigecycline clearance.20,22 Contrastly, Xie et al reported that there was no significant association between creatinine clearance, serum creatinine concentration and tigecycline clearance.19 Korth-Bradley et al also reported that tigecycline requires no dosage adjustment in patients with renal impairment.34 In clinical practice, tigecycline clearance is usually calculated to change dosage recommendations, which is based on the body-height and serum creatinine concentration. Therefore, compared with serum creatinine concentration, creatinine clearance is a more reliable renal function index and importantly associated with tigecycline clearance. Therefore, when analyzing the tigecycline PK, it is important to detect the renal function, especially creatinine clearance.
Conclusion
In conclusion, this review included eight studies, which to develop special population pharmacokinetic models on tigecycline in different patient subpopulations including healthy volunteers or patients. Two-compartments models were mostly used to describe tigecycline population pharmacokinetics. The covariates reported in the studies included in this review varied widely in special subpopulations. Body-weight, and creatinine clearance were the most important predictors of clearance in these studies. However, other factors, such as metabolism, drug–drug interactions, and genetic polymorphisms might also influence the tigecycline PK considerably. Therefore, a more stringent sampling strategy and a larger sample size were needed to assess these factors efficiently. In addition, more accurate descriptions of the pharmacokinetic models are needed in the previously reported models and the future models.
Acknowledgments
This work was supported by the grants from Shanghai Sailing Program (No. 20YF1437600) and PangDeng Program of Shanghai Tenth People’s Hospital (2021SYPDRC037).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Pankey GA. Tigecycline. J Antimicrob Chemother. 2005;56(3):470–480. doi:10.1093/jac/dki248
2. Bauer G, Berens C, Projan SJ, Hillen W. Comparison of tetracycline and tigecycline binding to ribosomes mapped by dimethylsulphate and drug-directed Fe2+ cleavage of 16S rRNA. J Antimicrob Chemother. 2004;53(4):592–599. doi:10.1093/jac/dkh125
3. Muralidharan G, Micalizzi M, Speth J, Raible D, Troy S. Pharmacokinetics of tigecycline after single and multiple doses in healthy subjects. Antimicrob Agents Chemother. 2005;49(1):220–229. doi:10.1128/AAC.49.1.220-229.2005
4. Gales AC, Jones RN. Antimicrobial activity and spectrum of the new glycylcycline, GAR-936 tested against 1203 recent clinical bacterial isolates. Diagn Microbiol Infect Dis. 2000;36(1):19–36. doi:10.1016/S0732-8893(99)00092-9
5. Singh RSP, Mukker JK, Drescher SK, Deitchman AN, Derendorf H. A need to revisit clinical breakpoints of tigecycline: effect of atypical non-linear plasma protein binding. Int J Antimicrob Agents. 2017;49(4):449–455. doi:10.1016/j.ijantimicag.2016.12.008
6. Sajad Y, Angelina OZ, Marcela K, et al. Tigecycline antibacterial activity, clinical effectiveness, and mechanisms and epidemiology of resistance: narrative review. Eur J Clin Microbiol Infect Dis. 2021;3:1–20.
7. Barbour A, Schmidt S, Ma B, et al. Clinical pharmacokinetics and pharmacodynamics of tigecycline. Clin Pharmacokinet. 2009;48(9):575–584. doi:10.2165/11317100-000000000-00000
8. Roberts JA, Joynt GM, Choi GY, Gomersall CD, Lipman J. How to optimise antimicrobial prescriptions in the Intensive Care Unit: principles of individualised dosing using pharmacokinetics and pharmacodynamics. Int J Antimicrob Agents. 2012;39(3):187–192. doi:10.1016/j.ijantimicag.2011.11.002
9. Burkhardt O, Rauch K, Kaever V, Hadem J, Kielstein JT, Welte T. Tigecycline possibly underdosed for the treatment of pneumonia: a pharmacokinetic viewpoint. Int J Antimicrob Agents. 2009;34(1):101–102. doi:10.1016/j.ijantimicag.2009.01.015
10. Ramirez J, Dartois N, Gandjini H, Yan JL, Korth-Bradley J, McGovern PC. Randomized Phase 2 trial to evaluate the clinical efficacy of two high-dosage tigecycline regimens versus imipenem-cilastatin for treatment of hospital-acquired pneumonia. Antimicrob Agents Chemother. 2013;57(4):1756–1762. doi:10.1128/AAC.01232-12
11. De Pascale G, Montini L, Pennisi M, et al. High dose tigecycline in critically ill patients with severe infections due to multidrug-resistant bacteria. Crit Care. 2014;18(3):R90. doi:10.1186/cc13858
12. Dixit D, Madduri RP, Sharma R. The role of tigecycline in the treatment of infections in light of the new black box warning. Expert Rev Anti Infect Ther. 2014;12(4):397–400. doi:10.1586/14787210.2014.894882
13. Wang J, Pan Y, Shen J, Xu Y. The efficacy and safety of tigecycline for the treatment of bloodstream infections: a systematic review and meta-analysis. Ann Clin Microbiol Antimicrob. 2017;16(1):24. doi:10.1186/s12941-017-0199-8
14. Vardakas KZ, Rafailidis PI, Falagas ME. Effectiveness and safety of tigecycline: focus on use for approved indications. Clin Infect Dis. 2012;54(11):1672–1674. doi:10.1093/cid/cis239
15. Prasad P, Sun J, Danner RL, Natanson C. Excess deaths associated with tigecycline after approval based on noninferiority trials. Clin Infect Dis. 2012;54(12):1699–1709. doi:10.1093/cid/cis270
16. Ni W, Han Y, Zhao J, et al. Tigecycline treatment experience against multidrug-resistant Acinetobacter baumannii infections: a systematic review and meta-analysis. Int J Antimicrob Agents. 2016;47(2):107–116. doi:10.1016/j.ijantimicag.2015.11.011
17. Freire AT, Melnyk V, Kim MJ, et al. Comparison of tigecycline with imipenem/cilastatin for the treatment of hospital-acquired pneumonia. Diagn Microbiol Infect Dis. 2010;68(2):140–151. doi:10.1016/j.diagmicrobio.2010.05.012
18. Zhou Y, Xu P, Li H, et al. Population pharmacokinetics and exposure-response analysis of tigecycline in patients with hospital-acquired pneumonia. Br J Clin Pharmacol. 2021;87(7):2838–2846. doi:10.1111/bcp.14692
19. Xie J, Roberts JA, Alobaid AS, et al. Population pharmacokinetics of tigecycline in critically Ill patients with severe infections. Antimicrob Agents Chemother. 2017;61(8). doi:10.1128/AAC.00345-17
20. Van Wart SA, Owen JS, Ludwig EA, Meagher AK, Korth-Bradley JM, Cirincione BB. Population pharmacokinetics of tigecycline in patients with complicated intra-abdominal or skin and skin structure infections. Antimicrob Agents Chemother. 2006;50(11):3701–3707. doi:10.1128/AAC.01636-05
21. Van Wart SA, Cirincione BB, Ludwig EA, Meagher AK, Korth-Bradley JM, Owen JS. Population pharmacokinetics of tigecycline in healthy volunteers. J Clin Pharmacol. 2007;47(6):727–737. doi:10.1177/0091270007300263
22. Rubino CM, Forrest A, Bhavnani SM, et al. Tigecycline population pharmacokinetics in patients with community- or hospital-acquired pneumonia. Antimicrob Agents Chemother. 2010;54(12):5180–5186. doi:10.1128/AAC.01414-09
23. Broeker A, Wicha SG, Dorn C, et al. Tigecycline in critically ill patients on continuous renal replacement therapy: a population pharmacokinetic study. Crit Care. 2018;22(1):341. doi:10.1186/s13054-018-2278-4
24. Borsuk-De Moor A, Rypulak E, Potrec B, et al. Population pharmacokinetics of high-dose tigecycline in patients with sepsis or septic shock. Antimicrob Agents Chemother. 2018;62(4). doi:10.1128/AAC.02273-17
25. Bastida C, Hernandez-Tejero M, Cariqueo M, et al. Tigecycline population pharmacokinetics in critically ill patients with decompensated cirrhosis and severe infections. J Antimicrob Chemother. 2022;77(5):1365–1371. doi:10.1093/jac/dkac036
26. Chi W, Lee HJ, Chong YP. Comparison of prospective and retrospective methods of a tigecycline post-marketing surveillance study in the safety outcomes of patients with complicated skin structure infection, complicated intraabdominal infection and community-acquired pneumonia. Infect Dis Ther. 2021;10(1):411–420. doi:10.1007/s40121-021-00398-7
27. Aljutayli A, Marsot A, Nekka F. An update on population pharmacokinetic analyses of vancomycin, part I: in adults. Clin Pharmacokinet. 2020;59(6):671–698. doi:10.1007/s40262-020-00866-2
28. Muralidharan G, Fruncillo RJ, Micalizzi M, Raible DG, Troy SM. Effects of age and sex on single-dose pharmacokinetics of tigecycline in healthy subjects. Antimicrob Agents Chemother. 2005;49(4):1656–1659. doi:10.1128/AAC.49.4.1656-1659.2005
29. Bassetti M, Guirao X, Montravers P, et al. Influence of age on the clinical efficacy of tigecycline in severely ill patients. J Glob Antimicrob Resist. 2019;18:199–206. doi:10.1016/j.jgar.2019.03.018
30. Liu J, Yan Y, Zhang F. Risk factors for tigecycline-associated hypofibrinogenemia. Ther Clin Risk Manag. 2021;17:325–332. doi:10.2147/TCRM.S302850
31. Fan G, Jin L, Bai H, Jiang K, Xie J, Dong Y. Safety and efficacy of tigecycline in intensive care unit patients based on therapeutic drug monitoring. Ther Drug Monit. 2020;42(6):835–840. doi:10.1097/FTD.0000000000000784
32. Pai MP. Serum and urine pharmacokinetics of tigecycline in obese class III and normal weight adults. J Antimicrob Chemother. 2014;69(1):190–199. doi:10.1093/jac/dkt299
33. Alraish R, Wicha SG, Frey OR, et al. Pharmacokinetics of tigecycline in critically ill patients with liver failure defined by maximal liver function capacity test (LiMAx). Ann Intensive Care. 2020;10(1):106. doi:10.1186/s13613-020-00707-2
34. Korth-Bradley JM, Troy SM, Matschke K, et al. Tigecycline pharmacokinetics in subjects with various degrees of renal function. J Clin Pharmacol. 2012;52(9):1379–1387. doi:10.1177/0091270011416938
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
