Back to Journals » Journal of Pain Research » Volume 13
Popliteal Artery Entrapment Syndrome in a Young Baseball Pitcher: A Case Report
Authors Huang WC, Tsai MM, Chang TL, Lai CL
Received 28 October 2019
Accepted for publication 19 February 2020
Published 21 April 2020 Volume 2020:13 Pages 777—781
DOI https://doi.org/10.2147/JPR.S236306
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Wei-Ching Huang,1,* Ming-Miau Tsai,1,* Tzu-Ling Chang,1 Chung-Liang Lai1,2
1Department of Physical Medicine and Rehabilitation, Taichung Hospital, Ministry of Health and Welfare, Taichung, Taiwan; 2Department of Occupational Therapy, Asia University, Taichung, Taiwan
*These authors contributed equally to this work
Correspondence: Chung-Liang Lai
Department of Physical Medicine and Rehabilitation, Taichung Hospital, Ministry of Health and Welfare, 199 San Min Road, Sec. 1, Taichung, Taiwan 403, Taiwan
Email [email protected]
Background: Popliteal artery entrapment syndrome (PAES) is a rare disease in young adults and is thought to be under-diagnosed, and its main cause is the abnormal structure between the popliteal artery and gastrocnemius muscle. The patients experience symptoms after the blood vessels are compressed. Failure to diagnose and treat PAES can cause serious sequelae.
Case: A 19-year-old male baseball pitcher with PAES type 2 suffered from left calf muscle tension and foot numbness and was mis-diagnosed for nearly a year. Finally, the lesion was detected by ultrasonography and confirmed by magnetic resonance imaging. After surgical intervention, he quickly returned to sport.
Discussion/Conclusion: PAES has 6 types. Type 2 (25%) and type 3 (30%) are the most common. Patients with this syndrome suffer from aching pain, numbness, and cramping in the calf area when they exercise. It is necessary to include this disease in differential diagnosis to implement early diagnosis, and ultrasonography is a more cheap and simple method for early detection.
Keywords: popliteal artery entrapment syndrome, intermittent claudication
Background
Popliteal artery entrapment syndrome (PAES) is an uncommon disease that is seldom diagnosed in young adults.1 Compared with atherosclerotic issues experienced by the elderly, the lower limb pain or intermittent claudication experienced in young adults is seldom regarded as vascular disease.2 PAES is mainly caused by the popliteal artery being compressed by the abnormal muscles and tendons around it, which further leads to vascular claudication.3 This case report investigated a young baseball pitcher experiencing the symptom of lower limbs numbness who was diagnosed with PAES. The lesion was finally detected by ultrasonography after a long period of medical attention at different clinics and confirmed by magnetic resonance imaging (MRI). After surgical intervention, the patient quickly returned to sport.
Case Report
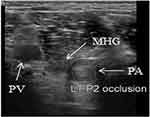
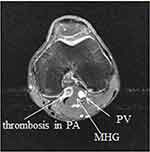
A 19-year-old male baseball pitcher repeatedly sought medical attention due to left calf muscle tension and foot numbness for nearly a year. His symptoms were especially aggravated after exercising and with left knee joint extension. Although the patient repeatedly visited the clinic, none of the symptoms were improved. Therefore, the patient was referred from the clinic to our hospital. The physical examination revealed no limitation on left knee joint mobility, no specific discomfort, no weakness in the left lower extremity, and no atrophy or hypertrophy of the muscles. However, paresthesia was reported in the left calf and foot. There was tenderness in the left knee popliteal fossa and medial gastrocnemius muscle. For the appearance, there was no swelling or redness or local heat, but the left toes were colder than the right ones. The imaging studies showed no abnormality in the knee X-ray. However, further musculoskeletal ultrasonography’s transverse view of popliteal space of the posterior knee discovered the left popliteal artery was compressed by popliteus muscle and medial gastrocnemius muscle and an occlusion at the popliteal artery (as shown in Figure 1). Therefore, the patient was scheduled for knee MRI. The result showed that the origin of the medial head of gastrocnemius muscle was abnormally inclined to the lateral side, and the popliteal artery was located in the medial side of the medial head of the gastrocnemius muscle (which is rarely observed) and formed an aneurysm (as shown in Figures 2–4). As a symptom and result of imaging studies, the patient was diagnosed with popliteal artery entrapment syndrome, type 2.
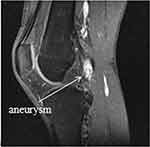 |
Figure 3 The left knee sagittal T1 with contrast MRI; aneurysm formation caused by the compressed popliteal artery can be observed at the popliteal artery. |
Due to the worsening symptoms, the patient was referred to the division of Vascular Surgery for surgical treatment. The pre-operative ultrasonography revealed a persistent occlusion at the P2 segment of the popliteal artery. During the surgery, it was found that the medial head of the gastrocnemius muscle was not located at the normal anatomical location, and the origin was inclined to the lateral side to compress the popliteal artery, which formed an aneurysm. Therefore, a decompression surgery was performed to surgically remove the partial tendon of the medial head of the gastrocnemius muscle and abnormal left popliteal artery. The left small saphenous vein transplantation surgery was further performed to replace the removed abnormal left popliteal artery. After the operation, the symptoms were completely relieved. Although the muscle strength of the left lower leg was slightly weakened, the patient quickly returned to the stadium to pitch baseball. The patient had signed a written informed consent form to have the case details and any accompanying images published and the manuscript was approved by the Ethics committee of Taichung Hospital, Ministry of Health and Welfare (Taichung, Taiwan) to have the case details published.
Discussion
The earliest case data of the disease PAES were published by Anderson Stuart due to anatomical structural abnormality in 1879. However, it was not until 1969 that Love and Whelan named this disease caused by structural abnormality as popliteal entrapment syndrome.4,5
PAES is one of the causes of the rare symptoms of lower extremity, intermittent claudication, which can be clearly diagnosed. The prevalence is between 0.165% and 3.5%, the male to female ratio is 15:1, and the prevalence of bilateral symptoms is 27–67%.6,8
In the beginning, PAES was divided into four types according to the differences in anatomical structural abnormalities (relative positions of popliteal artery, medial head of gastrocnemius muscle, and popliteus muscle).5 Afterwards, two types were added: compression of popliteal vein type and functional type where the anatomical structural position is normal.1,9,11 These 6 types are: (1) type 1: medial head of gastrocnemius muscle position is normal, but popliteal artery abnormally surrounds the medial side of medial head of gastrocnemius muscle; (2) type 2: medial head of gastrocnemius muscle position is abnormal, and its origin is inclined to the lateral side to make the popliteal artery locate at its medial side; (3) type 3: popliteal artery position is normal, but an accessory slip of the medial head of the gastrocnemius muscle abnormally surrounds the two sides of the popliteal artery to compress the popliteal artery; (4) type 4: popliteal artery position is deeper and is compressed by fibrous band or popliteus muscle; (5) type 5: popliteal vein is compressed and its structural abnormality conforms to any type of the four types of compressed popliteal artery; (6) type 6 is functional type, the anatomical positions of the popliteal artery and medial head of the gastrocnemius muscle are normal, but the medial head of the gastrocnemius muscle compresses the popliteal artery due to hypertrophy. According to the statistics, type 2 (25%) and type 3 (30%) are the most common.12
The symptoms and signs include intermittent claudication, cramping pain, paresthesia, tingling, and coldness in the foot and limb weakness. In particular, these symptoms and signs are developed after exercise and are relieved at the time of rest.13 In terms of physical examination: there is a tender point in the medial head of the gastrocnemius muscle. Whether the popliteal artery is compressed can be tested by the contraction of the gastrocnemius muscle. Moreover, passive dorsiflexion and forced plantar flexion of the ankle cause compression, resulting in popliteal and pedal pulses decreased or absent pulses.14,15 Imaging examinations include Doppler ultrasonography, MRI/magnetic resonance angiography (MRA), computed tomography angiography (CTA), and catheter-based angiography.16 Doppler ultrasonography is a useful and non-invasive test that is non-radiative and inexpensive . It can be used to perform a preliminary assessment to check if there is peripheral stenosis or occlusion. The changes that have occurred after the popliteal artery has been compressed (eg, thrombosis, aneurysm) can be observed. Doppler can also be used to detect changes in blood flow rate at the proximal and distal ends, and blood flow rate increases over the stenotic section. Generally, when examining the popliteal space of the posterior knee with musculoskeletal ultrasound, most physicians pay attention to the abnormality of the structures such as muscle or tendon, ligament, meniscus and nerve, and pay less attention to the relative position of each structure. Under normal circumstances, the popliteal fossa’s transverse view should show that the popliteal artery, popliteal vein, and tibial nerve are located in the middle of the two heads of the gastrocnemius muscle, that is, the popliteal artery and vein are located on the lateral side of the medial head together. So, we should pay attention to the following conditions: the popliteal artery is located on the medial side of the medical head of the gastrocnemius muscle (type 2 PAES), the popliteal artery and vein are located on the medial side of the medial head of the gastrocnemius muscle (type 5 PAES), or the slip of the medical head of gastrocnemius muscle is located between the popliteal artery and vein, separating the two (type 3 PAES). Regarding other abnormalities, we should also pay attention to whether there is stenosis or aneurysm of the artery lumen. In longitudinal view, we should also carefully trace the direction of the muscle and artery and check if there are abnormal turns or structural abnormalities. MRI/MRA, including axial and coronal images, is a good tool for diagnosing anatomical abnormalities to determine whether the anatomical structure between the medial gastrocnemius muscle and popliteal artery at the popliteal fossa causes vascular compression.8 In addition, MRI/MRA can also be used to identify other issues, such as trauma and cystic adventitial disease.17,19 CTA and catheter-based angiography are also commonly used for diagnosis. Moreover, stress angiography is a good way to diagnose PAES. It is a dynamic test for achieving a preliminary diagnosis to calf claudication with symptoms such as cold, numbness or cyanosis. It allows the patients’ lower limb to maintain the ankle’s neutral position during the test. When compared with ankle active dorsiflexion and active plantar flexion, it is often observed that the blood flow is significantly weakened.20 This method can also be applied to ultrasonography, CTA and MRA. However, it is more difficult to apply it to MRA because the examination time is longer and it is difficult for the patient to maintain ankle flexion until the examination is completed.
The treatments depend on the level of vascular compression and the level of damage of the blood vessels. The non-operative treatment includes time-limited restriction of physical activity for functional type PAES and endoluminal revascularization by catheter-directed thrombolysis for thrombosis. However, thrombolysis does not seem to decrease the need for subsequent surgery.21 The main treatment is surgical treatment, and the method is to remove the muscles or tendons of the compressed blood vessels so that the blood flow can be restored.22 However, if there is marked thickening, occlusion or aneurysm formation of the vessel walls, it is necessary to consider vascular bypass or transplantation, and the vessel frequently used for transplantation is the saphenous vein. It is generally not recommended to perform a single intravascular repair, because the root cause of vascular compression is not resolved and it is easy to cause re-occlusion. The removal of the muscle or tendon of the compressed vessel is required.23,24 Type 6 of the PAES is functional type. The surgical effect on type 6 is worse than that on the other types, because the anatomy itself is normal. In recent years, botulinum toxin has been injected into the gastrocnemius muscle to reduce the compression of the gastrocnemius muscle and the therapeutic effect has been good. Besides, the training effect will be increased in athletes. This result may be related to the situation that athletes are unable to engage in training due to limb discomfort caused by PAES not being resolved.25
Clinical Implications
Although PAES is not common and has often been under-diagnosed, it is a very important differential diagnosis of lower limb numbness and pain, especially when young people develop symptoms after exercising and experience intermittent claudication. It is necessary to include this disease in differential diagnosis to implement early diagnosis and ultrasonography is a more cheap and simple method for early detection. In this case, after the diagnosis was confirmed using medical history and imaging examinations, the patient quickly returned to sport after undergoing the surgery.
Acknowledgments
This research was supported by the PMR team of the Taichung Hospital, Ministry of Health and Welfare.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gourgiotis S, Aggelakas J, Salemis N, Elias C, Georgiou C. Diagnosis and surgical approach of popliteal artery entrapment syndrome: a retrospective study. Vasc Health Risk Manag. 2008;4(1):83–88. doi:10.2147/VHRM.S1938
2. Radonic V, Koplic S, Giunio L, Bozic I, Maskovic J, Buca A. Popliteal artery entrapment syndrome: diagnosis and management, with report of three cases. Tex Heart Inst J. 2000;27(1):3–13.
3. Skeik N, Thomas TM, Engstrom BI, Alexander JQ. Case report and literature review of popliteal artery entrapment syndrome. Int J Gen Med. 2015;8:221–225. doi:10.2147/IJGM.S82067
4. Stuart TP. Note on a variation in the course of the popliteal artery. J Anat Physiol. 1879;13(Pt 2):162.
5. Love JW, Whelan TJ. Popliteal artery entrapment syndrome. Am J Surg. 1965;109:620–624. doi:10.1016/S0002-9610(65)80016-2
6. Bouhoutsos J, Daskalakis E. Muscular abnormalities affecting the popliteal vessels. Br J Surg. 1981;68(7):501–506. doi:10.1002/bjs.1800680720
7. Gibson MH, Mills JG, Johnson GE, Downs AR. Popliteal entrapment syndrome. Ann Surg. 1977;185(3):341–348. doi:10.1097/00000658-197703000-00016
8. Kim HK, Shin MJ, Kim SM, Lee SH, Hong HJ. Popliteal artery entrapment syndrome: morphological classification utilizing MR imaging. Skeletal Radiol. 2006;35(9):648–658. doi:10.1007/s00256-006-0158-5
9. Rich NM, Hughes CW. Popliteal artery and vein entrapment. Am J Surg. 1967;113(5):696–698. doi:10.1016/0002-9610(67)90323-6
10. Levien LJ, Veller MG. Popliteal artery entrapment syndrome: more common than previously recognized. J Vasc Surg. 1999;30(4):587–598. doi:10.1016/S0741-5214(99)70098-4
11. Roche-nagle G, Wong KT, Oreopoulos G. Vascular claudication in a young patient: popliteal entrapment syndrome. Hong Kong Med J. 2009;15(5):388–390.
12. Rosset E, Hartung O, Brunet C, et al. Popliteal artery entrapment syndrome. Anatomic and embryologic bases, diagnostic and therapeutic considerations following a series of 15 cases with a review of the literature. Surg Radiol Anat. 1995;17(2):
13. Almeida MJ, Yoshida WB, Melo NR. [Popliteal artery entrapment syndrome]. Rev Port Cir Cardiotorac Vasc. 2003;10(4):199–206.[Article in English, Portuguese]
14. Gokkus K, Sagtas E, Bakalim T, Taskaya E, Aydin AT. Popliteal entrapment syndrome. A systematic review of the literature and case presentation. Muscles Ligaments Tendons J. 2014;4(2):141–148. doi:10.32098/mltj.02.2014.09
15. Politano AD, Bhamidipati CM, Tracci MC, Upchurch GR
16. Simsek E, Bugra O, Teber MA, Katircioglu SF. What should be the first treatment of popliteal artery entrapment syndrome. Ann Thorac Cardiovasc Surg. 2014;20(2):169–172. doi:10.5761/atcs.cr.12.02007
17. Chun JY, Yella R, Gonzalez-Junyent C, et al. Popliteal artery entrapment syndrome: anatomy, imaging techniques and findings.
18. Wright LB, Matchett WJ, Cruz CP, et al. Popliteal artery disease: diagnosis and treatment. Radiographics. 2004;24(2):467–479. doi:10.1148/rg.242035117
19. Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997;26(3):517–538. doi:10.1016/S0741-5214(97)70045-4
20. McCrory P, Bell S, Bradshaw C. Nerve entrapments of the lower leg, ankle and foot in sport. Sports Med. 2002;32(6):371–391. doi:10.2165/00007256-200232060-00003
21. Sinha S, Houghton J, Holt PJ, Thompson MM, Loftus IM, Hinchliffe RJ. Popliteal entrapment syndrome. J Vasc Surg. 2012;55(1):252–262. doi:10.1016/j.jvs.2011.08.050
22. Sutcliffe JB
23. Kim SY, Min SK, Ahn S, Min SI, Ha J, Kim SJ. Long-term outcomes after revascularization for advanced popliteal artery entrapment syndrome with segmental arterial occlusion. J Vasc Surg. 2012;55(1):90–97. doi:10.1016/j.jvs.2011.06.107
24. Levien LJ. Popliteal artery entrapment syndrome. Semin Vasc Surg. 2003;16(3):223–231. doi:10.1016/S0895-7967(03)00028-0
25. Hislop M, Kennedy D, Cramp B, Dhupelia S. Functional popliteal artery entrapment syndrome: poorly understood and frequently missed? A review of clinical features, appropriate investigations, and treatment options. J Sports Med (Hindawi Publ Corp). 2014;2014:105953. doi:10.1155/2014/105953
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.