Back to Journals » Journal of Blood Medicine » Volume 14
Platelet Parameters and Their Correlation with Parasitemia Levels Among Malaria Infected Adult Patients at Jinella Health Center, Harar, Eastern Ethiopia: Comparative Cross-Sectional Study
Authors Asmerom H , Gemechu K , Bete T, Sileshi B, Gebremichael B, walle M , Arkew M
Received 24 October 2022
Accepted for publication 12 January 2023
Published 19 January 2023 Volume 2023:14 Pages 25—36
DOI https://doi.org/10.2147/JBM.S394704
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Haftu Asmerom,1 Kabtamu Gemechu,1 Tilahun Bete,2 Beza Sileshi,1 Berhe Gebremichael,3 Muluken walle,4 Mesay Arkew1
1School of Medical Laboratory Sciences, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 2School of Nursing and Midwifery, Department of Psychiatry, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 3School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 4Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, Jigjiga University, Jigjiga, Ethiopia
Correspondence: Haftu Asmerom, School of Medical Laboratory Sciences, College of Health and Medical Sciences, Haramaya University, P.O. Box 235, Harar, Ethiopia, Tel +251913889039, Email [email protected]
Background: Malaria is a major public health problem with the highest morbidity and mortality in developing countries. Hematological changes play a great role in malaria pathogenesis through platelets and platelet parameters. However, the changes in platelet parameters are not clearly described in Ethiopia. Therefore, this study aimed to compare platelet parameters and their correlation with parasitemia among malaria-infected adult patients and healthy adults.
Methods: An institutional-based comparative cross-sectional study was conducted involving 186 (93 malaria-infected patients and 93 healthy adults) study participants using a convenient sampling technique at Jinella health center, Harar, Eastern Ethiopia, from July 10–August 10, 2022. Five milliliters of venous blood were collected from each study participant, and platelet parameters were analyzed using a Unicel (DxH 800) automated hematologic analyzer. A drop of blood was taken from malaria-suspected patients for blood film preparation. Results between two groups were compared using the Mann–Whitney U-test. Spearman’s rank correlation coefficient was used to evaluate the relationships between two continuous variables. A P-value of < 0.05 was considered statistically significant.
Results: Platelet, plateletcrit, and mean platelet volume of malaria-infected patients were significantly lower as compared with healthy adults (103 x103cells/μL vs 268 x103cells/μL, 0.13 fl vs 0.23 fl, and 9.6 fl vs 15.3 fl), respectively). Conversely, platelet distribution width and platelet large cell ratio were higher in malaria-infected patients than healthy adults (19.2% vs 15.3% and 0.35% vs 0.29%), respectively). Parasitemia levels had a moderately inverse correlation with platelet count (r= − 0.419) and a weakly positive correlation with mean platelet volume (r=0.278).
Conclusion: The platelet, plateletcrit, and mean platelet volume of malaria-infected patients were significantly lower as compared with healthy adults. Malaria parasitemia had a moderate inverse correlation with platelet count and a weak positive correlation with mean platelet volume. Thrombocytopenia and alteration of platelet parameters should be considered in malaria patients.
Keywords: adults, malaria, parasitemia level, platelet parameters
Introduction
According to the World Health Organization (WHO), malaria is a potentially fatal condition brought on by parasites that are spread to humans through the bites of infected female Anopheles mosquitoes.1 The two parasite species that represent the greatest threat globally are Plasmodium falciparum (P. falciparum) and Plasmodium vivax (P.vivax), which are known to be infectious to humans.2 Hematological alterations are among the most frequent malarial consequences, and they have a significant impact on diseases of pathophysiology. Platelets are among the key cell types affected by these frequent malarial consequences.3–5 Furthermore, the pathophysiology of malarial complications can be greatly influenced by the alteration of platelets.6,7
Additionally, the platelet activation changes the shape of platelets, as well as their mean platelet volume (MPV), platelet distribution width (PDW), platelet large cell ratio (P-LCR), and platelet crit (PCT), which are good indicators of their biomass.8,9 In 2020, an estimated 241 million malaria cases and 627,000 deaths will have been reported worldwide. Africa bore a disproportionate share of the world’s malaria burden.1 Patients with malaria typically have significantly fewer platelets.10
The most frequent malaria infection complication is thrombocytopenia, defined as a decreased quantity of platelets,4,11,12 and low platelet counts (<150 × 103cells/μL) are its defining feature.13 People with platelet counts below 150,000 cells/μL had a 12–15-fold higher risk of contracting malaria than people with platelet levels above 150,000 cells/μL.14 However, the extent of these changes varies with the degree of malaria endemicity, preexisting hemoglobinopathies, dietary state, demographic variables, and malaria immunity.10
Peripheral destruction, excessive platelet sequestration in the spleen, and excessive platelet consumption related to the disseminated intravascular coagulation process are the fundamental mechanisms of thrombocytopenia in malaria.15 Increased secretion of inflammatory cytokines (tumor necrosis factor Alpha (TNFα), Interleukin-1, and Interleukin-10), endothelial cell activation caused by overexpression of cell adhesion molecules like (ICAM-1 and vascular adhesion molecule-1), initiation of the coagulation pathways as a result of platelet consumption, and endothelial damage are all common factors in the entry of the malaria parasite.16
Additionally, the activation of host immune factors, such as cytokines like TNFα and pro-inflammatory interleukins, oxygen free radicals, and nitric oxide (NO), as well as the production of several toxins, causes damage to the host endothelium and tissues.17 Previous studies have demonstrated a relationship between parasite density and the seriousness of malarial infection complications.18 The platelets were also found to be much lower at high parasitemia, and it was reported that increasing P. falciparum parasite loads cause a decline in platelet count.19 Uncertainty exists regarding the degree of platelet parameter alterations that occur during a malarial infection and their underlying biological mechanisms in relation to the level of parasitemia. Little is known about the changes in platelet parameters that occur during malaria infection. Therefore, this study aimed to compare platelet parameters and their correlations with parasitemia among malaria-infected adult patients and apparently healthy adults at Jinella Health Center, Harar, Eastern Ethiopia.
Materials and Methods
Study Design, Area, and Period
A comparative cross-sectional study was conducted in Harar Town, which is one of the regional states of the Federal Democratic Republic of Ethiopia and is located in the eastern part of the country with an elevation of 1885 meters above sea level at latitude 90°12′N and longitude 42°07′E. It is 526 kilometers east of Addis Ababa, Ethiopia’s capital city. According to the Harari Regional Health Bureau’s 2018 annual report, there were 4 hospitals, 10 health centers, and 20 health posts. Among those ten health centers, the study was conducted at Jinella Health Center from July 10, 2022, to August 10, 2022.
Study Participants
The study population for the malaria-infected group consisted of all adult patients who had been diagnosed with the disease and gave their consent to take part in the study. On the other hand, participants who tested positive for Human Immunodeficiency Viruses (HIV), Hepatitis B Surface Antigen (HBsAg), and Hepatitis C Virus (HCV), pregnant and lactating women, and adults with a history of chronic diseases like hypertension, cardiac disease, and diabetes mellitus were excluded from the malaria-infected group. Additionally, during the study period, adults who were age- and gender-matched and appeared healthy were used as the study population for the comparative group. Healthy adults, including Jinella Health Center employees, volunteers, non-paid blood donors, and patient attendants, were included in the comparison group. Human immunodeficiency viruses, HBsAg and HCV, syphilis, and malaria were screened for, and the health of the comparative group was evaluated using the National Blood Bank Service blood donor questionnaire. Blood donors with a history of chronic conditions and those who were unwilling to participate in the study were excluded from the comparative group.
Sample Size Determination and Sampling Technique
According to VanVoorhis and Morgan’s recommendations, 30 subjects per group are required to find meaningful changes, which might give the study 80% power.20 Then, a total of 186 study participants (93 malaria-infected adults and 93 apparently healthy adults) were recruited using a convenience sampling technique.
Operational Definition
Platelet parameters: platelets and platelet indices (platelet, MPV, PDW, PC, T, and P-LCR).19
Apparently healthy adults: adult individuals who are in good health and are not suffering from any illness.21
Thrombocytopenia: a platelet count of less than 150 × 103cells /μL.22
Levels of malarial parasitemia: high parasitemia (>10 parasites per field), moderate parasitemia (1–10 parasites per field), and low parasitemia (1–100 parasites per 100 fields).23
Data Collection Procedure and Sampling Processing
Data were collected using a structured questionnaire, which was prepared first in the English language and translated into local languages (Afan Oromo and Amharic) and then back to the English language. Before data collection, data collectors selected patients who qualified for the inclusion criteria and obtained informed consent. Socio-demographics and the history of the patient were collected by administering the questionnaire under the supervision of the principal investigator. Five milliliters of venous blood were collected from both groups by venipuncture according to WHO guidelines24 under aseptic conditions. A drop of blood was taken from the syringe of malaria- susceptible patients for thick and thin blood film (BF) preparation. Then thick and thin BF were prepared according to the WHO guidelines and labeled. The thin films were fixed with absolute methanol, and both thick and thin smears were stained using the 10% Giemsa stain. After the slides were well-dries, malaria infection diagnosis was conducted by detecting and identifying malaria parasites in BF using light microscopy (100x magnification).24
Parasitemia level was determined with thick BF, and species differentiation (confirmation of Plasmodium species) was determined with thin BF if doubtful on thick films. The level of asexual parasitemia was calculated using the formula (number of parasites counted/white blood cell counted (WBC)) WBC count/L of blood.25 The smears were reported as negative for malaria only if two consecutive smears were assessed and confirmed negative. The remaining blood sample from malaria-suspected patients and the collected blood from the comparative group were transferred into an ethylene diamine tetraacetic acid (EDTA) tube and gently mixed by inverting the tube 5–6 times to prevent clotting. Then, the samples were analyzed for platelet parameters (platelet count, MPV, PDW, PCT, and P-LCR) using an automated hematology analyzer (UniCel DxH 800).
Statistical Analysis of the Data
After the collection of all the necessary data, it was checked for completeness before entering the Epi-Data software for analysis. Data were entered into Epi-Data version 4.4.2.1, and all data were edited, organized, coded, exported, and analyzed using Statistical Package for Social Sciences (SPSS) version 26 statistical software. The results were presented in graphs and tables. Data for the different continuous platelet parameters were expressed as medians (IQR). The Kolmogorov–Smirnov test was used to check the normal distribution of continuous data. Data between malaria-infected and comparative groups were compared by the Mann–Whitney U-test. The Kruskal–Wallis test was applied to compare platelet parameters and levels of parasitemia among malaria-infected adult patients. Spearman’s rank correlation coefficient was used to evaluate the relationships between two continuous variables. Categorical variables were compared using the chi-square test. A p-value of <0.05 was considered statistically significant.
Data Quality Control
The suitability of the test materials, specimen inspection, and request form review were completed. All laboratory activities were performed with strict adherence to standard operating procedures (SOP). The quality and expiration date of the methanol used for thin blood fixation and Giemsa stain were checked. Giemsa was used to stain positive malaria slides to ensure the product’s quality. The reporting took place following inspections of at least 100 fields following the normal blood film examination technique.
An expert laboratory technologist double-checked any disagreement in blood film results between two laboratory personnel. Strict adherence to the manufacturer’s instructions was observed. Quality checks were carried out daily using low, normal, and high control levels to track an instrument’s performance over time before beginning sample analysis. The reagent containers were also checked daily for correct connections between the instrument and the reagent containers, sufficient quantity, expiration date, precipitates, turbidity, and particulate matter.
Ethical Consideration
The study was conducted after ethical approval was obtained from the Institutional Health Research Ethics Review Committee (IHRERC), College of Health and Medical Sciences, Haramaya University, with reference number (IHRERC-125-2022). A permission letter was taken from the Jinella Health Center. All study participants gave informed, voluntary, written, and signed consent before data collection. The test results were kept confidential. Additionally, Patients who experienced platelet alterations were also linked to physicians for better management and care. The study was conducted according to the Declaration of Helsinki.
Results
Socio-Demographic Characteristics of Study Participants
A total of 186 study participants (93 malaria-infected adult patients and 93 apparently healthy adults) participated in this study. Among the study participants, the majority of 37 (39.8%) malaria-infected adult patients and 43 (46.2%) apparently healthy adults were aged between 18 and 27 years. In both groups, the fewest number 4 (4.3%) study participants were found between the ages of 58 and 65. In terms of gender, in malaria-infected adult patients and apparently healthy adults, 61 (65.6%) and 59 (63.4%) of the participants were male, respectively. Regarding marital status, most of the study participants—40 (43.0%) malaria-infected adult patients and 53 (57.0%) apparently healthy adults were married. The majority of 53 (57.0%) malaria-infected adult patients were rural residents; however, the majority of 69 (74.2%) apparently healthy individuals were urban residents. Regarding their educational status, 36 (38.7%) of malaria-infected adult patients were able to read and write, and 51 (54.8%) of apparently healthy adult were in college or higher. About 29 (31.2%) of malaria-infected patients were farmers, but 51 (54.8%) of apparently healthy adults were government employees (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Study Participants at Jinella Health Center, Harar, Eastern Ethiopia from July-August, 2022(n=93) |
Distribution of Plasmodium Species and Parasitemia Levels
In the current study, P. falciparum 49 (52.7%), P. vivax 34 (36.5%), and dual infection 10 (10.8%) were the two plasmodium species identified. In terms of parasitemia levels, 34 (36.6%) had low parasitemia, 30 (32.3%) had moderate parasitemia, and 29 (31.2%) had high parasitemia.
Comparisons of Platelet Parameters Among Study Participants
Platelet parameters of malaria-infected adult patients were compared with those of apparently healthy adults using the Mann–Whitney U-test. The median values of platelet count and PCT of malaria-infected patients were significantly lower as compared with apparently healthy adults (103 x 103cells/μL vs 268 x 103cells/μL; p<0.001) and (0.13 fl vs 0.23 fl; p<0.001), respectively. The MPV was also observed to be lower in malaria-infected adult patients (9.6 fl) than in those of apparently healthy adults (15.3 fl), with a statistically significant difference between the two groups (p<0.001). Conversely, the median values of PDW and P-LCR were observed to be higher in malaria-infected adult patients as compared with apparently healthy adults (19.2% vs 15.3%) and (0.35% vs 0.29%), respectively, with a statistically significant difference between the two groups (p<0.001) (Table 2).
 |
Table 2 Comparison of Platelet Parameters Among Malaria-Infected Adult Patients and Apparently Healthy Adults at Jinella Health Center, Harar, Eastern Ethiopia, 2022 (n=93) (Mann–Whitney U-Test) |
Comparison of Platelet Parameters with Parasitemia Levels
The median platelet count was significantly lower in patients with high parasitemia compared to the low and moderate parasitemia groups (p<0.001). However, the median value of MPV was significantly higher in patients with high parasitemia compared to those with low and moderate parasitemia (p= 0.001) (Table 3).
 |
Table 3 Platelet Parameters at Different Parasitemia Levels Among Malaria-Infected Adult Patients at Jinella Health Center, Harar, Eastern Ethiopia, 2022 (n=93) (P-value by Kruskal Wallis Test) |
Correlation of Platelet Parameters with Parasitemia Levels
There was a moderate inverse correlation between platelet counts and parasitemia levels (r = −0.419, p < 0.001) (Figure 1). But there was a weak positive correlation between parasitemia and mean platelet volume (r = 0.278, p = 0.007). There was a weak inverse correlation between platelet counts and mean platelet volume in malaria-infected adult patients (r = −0.275, p = 0.007) (Figure 2). However, mean platelet volume had a weakly positive correlation with PDW (r = 0.275, p = 0.008) and PCT (r = 0.235, p = 0.023), and a moderately positive correlation with P-LCR among malaria-infected adult patients (r = 0.532, p < 0.001). In addition to this, PDW had a moderate correlation with PLCR (r = 0.688, p < 0.001) and a weakly negative correlation with PCT (r = −0.288, p = 0.005) (Figure 3). A positive correlation was found between platelet count and plateletcrit (r= 0.4; p-value <0.001). Platelet count and platelet distribution width had a negative correlation (r= −0.5; p < 0.001). No significant correlation was found between platelet count and platelet distribution width.
 |
Figure 2 Relationship between platelet count and MPV among malaria-infected adult patients at Jinella Health Center, Harar, Eastern Ethiopia, 2022 (n=93). |
 |
Figure 3 Relationship between PDW and PCT among malaria-infected adult patients at Jinella Health Center, Harar, Eastern Ethiopia, 2022 (n=93). |
Prevalence of Thrombocytopenia Among Parasitemia Levels
The overall prevalence of thrombocytopenia in the current study was 77.4 (95% CI: 68.9–85.9). Thrombocytopenia was defined as platelet count <150 x 103cells/μL and further defined as severe if the platelet count was <50 x 103cells/μL, moderate if the platelet count was between 51–100×103 cells/μL, mild if the platelet count was between101-150x103cells/μL. Platelet count showed a significant difference among different parasitemia levels (P=0.009) (Table 4).
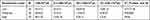 |
Table 4 Cross Tabulation of Chi-Square Analysis of Platelet Counts Among Parasitemia Levels of Malaria-Infected Adult Patients at Jinella Health Center, Harar, Eastern Ethiopia, 2022 (n=93) |
Discussion
Changes in platelet parameters are considered a hallmark of malaria infection. Most of the time, these changes in malaria infection may be a result of higher levels of parasitemia.26 In this study, the median platelet count was significantly reduced in malaria-infected adult patients as compared to apparently healthy individuals (P <0.001). This result was similar to the finds reported in Thailand,8 Colombia,27 Nigeria,28 and Ethiopia.29 The decrease in platelet counts with malaria might be attributed to platelet degranulation, which ends with the release of platelet factor 4 to kill malaria parasites.30,31
The median value of MPV was significantly lower in malaria-infected adult patients than in apparently healthy adults, in agreement with a study conducted in Ghana32 but in contrast with studies conducted in Brazil,15 Sudan,33 and Uganda.34 This inconsistency and variation in malaria infection can be explained by the fast splenic and medullary release of huge volumes of platelets in response to the increased demand for these cells.35 The median value of PCT was significantly decreased in malaria-infected adult patients, which was corroborated with previous studies conducted in Thailand,8 Ghana,32 and Nigeria.36 Low PCT in malaria may be due to the sensitization of platelets by parasitized red blood cells, resulting in increased platelet sensitivity to adenosine diphosphate (ADP) and better dense-granule secretion. This finding is also explained by concomitant thrombocytopenia.37
The median value of PDW during this study was found to be significantly higher in malaria-infected adult patients, which was in agreement with studies conducted in Colombia,27 Thailand,8 and Sudan.33,38 The higher PDW values in malaria can be explained by the bone marrow formation of megakaryocytes to make amends for the low absolute platelet count during acute malaria infection.39 However, this finding was in contrast with a study conducted in Ghana.32 This discordant result was attributed to several factors that will result in changes in PDW, like the recruitment of multiple ploidy classes of megakaryocytes.40
Regarding P-LCR, the median significantly increased in malaria-infected adult patients, which was compatible with the study conducted in Nigeria36 and Sudan.38 This could be because larger platelets are typically younger and contain more intracellular granules, resulting in a higher thrombogenic potential.41 In contrast to this study, a study conducted in Ghana32 showed that the P-LCR was statistically lower than that of a comparative group. Previously, variations in the P-LCR value could be attributed to thrombopoietin suppression by TNF-a, which can inhibit thrombopoiesis and, in fact, reduce the number of juvenile thrombocytes. Thus, elevation of TNF-a in malaria infections is thought to down-regulate Interleukin-10, which inhibits erythropoietin and possibly thrombopoietin biosynthesis and its activity.42
There were significant differences in platelet count and MPV between malaria parasitemia levels (P value <0.001 and 0.007, respectively). The platelet count was notably reduced in patients with high parasitemia compared to those in the low and moderate parasitemia groups. Malaria parasitemia also had a moderately negative correlation with platelet count (r = −0.419, p < 0.001) (Table 5). Many previous studies reported similar correlational statistics between platelet count and malaria parasitemia,29,43,44 but this finding was in contrast to the study conducted in Brazil.26 The decrement of platelets may be due to the role of von Willebrand factor (VWF) multimers in promoting platelet-mediated IE (infected erythrocyte) cytoadherence, and it was proposed that this mechanism may be particularly important during the first stages of malaria infection.45 Additionally, platelets in patients with malaria infection express Toll-like receptors (TLRs), which release prepackaged inflammatory mediators like NO, a key mediator of platelet homeostasis. Then, a decreased bioavailability of NO in patients with severe malaria may contribute to increased platelet activation and consumption as parasitemia increases.19
 |
Table 5 Correlation of Platelet Parameters Among Malaria-Infected Adult Patients at Jinella Health Center, Harar, Eastern Ethiopia, 2022 (n=93) (Spearman’s Rank-Order Correlation) |
The MPV value was found to be higher in patients with high parasitemia compared to those in the low and moderate parasitemia groups. There was also a weak direct correlation between parasitemia levels (r = 0.278, p = 0.007) in contrast with a study conducted in Sudan.44 This variability could be due to the platelet size being larger than average as parasitemia increases, which is typically an indication that the patient’s body is producing too many immature platelets.46
In the present study, there was a moderately weak inverse correlation between platelet count and MPV (r = −0.257; p = 0.007) which was in accordance with other studies.43,47,48 When platelets decrease in number, an early release of platelets from the bone marrow occurs. These early released platelets are larger in size, and the stimulation of megakaryocytes within the marrow by thrombopoietin in response to low platelets produces larger platelets as their nucleus becomes hyper-lobulated with the next polymer.27 The MPV had a weak positive correlation with PDW (r = 0.275; p = 0.008) and PCT (r = 0.235; p = 0.023) which was in accordance with the study conducted in Mangalore.43 Mean platelet volume reflects platelet size, whereas PDW reflects variability in platelet size and is taken into account as a marker of platelet function and activation. So, a high PDW means platelet size varies greatly, which is a clue that there’s platelet activation and has been related to vascular diseases.49 This convergence of MPV and PDW changes may be useful for detecting malaria infection during the first stage of gametocyte sequestration in bone marrow.50
In addition to this, there was a moderate correlation between MPV and P-LCR (r = 0.532; p = 0.001) which was agreed with in a study conducted in Nigeria.36 Since P-LCR is an indicator of circulating larger platelets (> 12 fL), as MPV becomes higher, there’s a tendency for P-LCR to be increased.51 Platelet distribution width had a weak negative correlation with PCT (r = −0.288; p = 0.005), which is the product of MPV and platelet count and represents the percentage of space platelets occupy within the blood.52 On the other hand, PDW had a moderately positive correlation with P-LCR (r = 0.688; P < 0.001). A high P-LCR or PDW may indicate peripheral immune destruction of platelets.53
In the current study, the prevalence of thrombocytopenia was 77.4 (95% CI: 68.9–85.9). Comparable results were found in studies conducted in India (71%),54 Pakistan (70%),55 and Gujarat, India (82%).56 But the prevalence of thrombocytopenia was found to be higher than in similar studies conducted in Saudi Arabia (67.5%),57 Indonesia (33%),58 Aden (42.9%),5 and Turkey (47%),59 and Ghana (47%).60
On the contrary, the prevalence of thrombocytopenia in this study was lower than in the studies conducted in Karnataka, India (89.0%),48 and Karamsad, India (90%).61 This discrepancy might be due to the study designs used, sample size variation between different studies, malaria distribution across different countries, or the type of study participants. Another possible cause for this discrepancy might be due to splenic pooling of platelets and antibody-mediated platelet destruction.33,36,37
Conclusion and Recommendation
It is evident from the results of our current study that the median values of platelet count, MPV, and PCT of adult malaria-infected patients were significantly lower as compared with apparently healthy adults. Besides, malaria parasitemia level had a moderate inverse correlation with platelet count and a weak positive correlation with MPV. In addition, the documented low levels of platelet count and variation in platelet parameters in malaria-positive cases have significant value in supporting the clinical diagnosis of malaria. The causes of thrombocytopenia and alteration of platelet indices should be taken into consideration when comparing findings in malaria patients. Whether or not our findings may be utilized in monitoring the effect of malaria treatment, more work is required to relate these findings to the presence of any parasite component that may be useful to realize the mechanism of platelet parameter alterations.
Abbreviations
BF, Blood Film; EDTA, Ethylene Diamine Tetra Acetic Acid; Hgb, Hemoglobin; ICAM-1, Intravascular cell adhesion molecule-1; MPV, Mean Platelet Volume; NO, Nitric Oxide; PCT, Plateletcrit; PDW, Platelet Distribution Width; P-LCR, Platelet Large Cell Ratio; PF, Plasmodium Falciparum; PV, Plasmodium Vivax; TNFa, Tumor Necrosis Factor-alpha; VWF, Von Willebrand factor; WHO, World Health Organization.
Acknowledgments
We would like to express our heartfelt gratitude to the laboratory technicians and all staff members of Jinella Health Center for their unreserved support in blood sample collection, processing, and use of their laboratory facilities. In addition, we would also like to acknowledge the study participants and data collectors.
Author Contributions
All authors made a significant contribution to the work reported in the conception, study design, execution, acquisition, analysis, and interpretation of data; and took part in drafting, revising, and critically reviewing the manuscript. All authors have agreed on the approval of the final manuscript to be published in the current journal and to be accountable for all aspects of the work.
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
1. World Health Organization. World Malarai Report 2021. Geneva, swizerland: World health organization; 2021.
2. World Health Organization. Eliminating Malaria. World Health Organization; 2016.
3. van Wolfswinkel M, Vliegenthart-Jongbloed K, de Mendonça Melo M, et al. Predictive value of lymphocytopenia and the neutrophil-lymphocyte count ratio for severe imported malaria. Malar J. 2013;12(1):1–8. doi:10.1186/1475-2875-12-101
4. Khan S, Abbass Y, Marwat M. Thrombocytopenia as an indicator of malaria in adult population. Malar Res Treat. 2012;2012:1–4. doi:10.1155/2012/405981
5. Bakhubaira S. Hematological parameters in severe complicated Plasmodium falciparum malaria among adults in Aden. Turkish J Hematol. 2013;30(4):394. doi:10.4274/Tjh.2012.0086
6. Mohandas N, An X. Malaria and human red blood cells. Med Microbiol Immunol. 2012;201(4):593–598. doi:10.1007/s00430-012-0272-z
7. Cox D, McConkey S. The role of platelets in the pathogenesis of cerebral malaria. Cell Mol Life Sci. 2010;67(4):557–568. doi:10.1007/s00018-009-0211-3
8. Tangvarasittichai O, Srikong M, Tangvarasittichai S. Platelet count and platelet indices used as potential markers for first malaria infection diagnosis. Int J. 2016;8(10):1454–1458.
9. Akpinar I, Sayin M, Gursoy Y, et al. Plateletcrit. Herz. 2014;39(1):142–148. doi:10.1007/s00059-013-3798-y
10. Kotepui M, Phunphuech B, Phiwklam N, Chupeerach C, Duangmano S. Effect of malarial infection on haematological parameters in population near Thailand-Myanmar border. Malar J. 2014;13(1):1–7. doi:10.1186/1475-2875-13-218
11. Moulin F, Lesage F, Legros A, et al. Thrombocytopenia and Plasmodium falciparum malaria in children with different exposures. Arch Dis Child. 2003;88(6):540–541. doi:10.1136/adc.88.6.540
12. Abid M, Muhammad Y. Thrombocytopenia: a predictor of malaria among febrile patients in Liberia. 2005.
13. Bayleyegn B, Asrie F, Yalew A, Woldu B. Role of platelet indices as a potential marker for malaria severity. J Parasitol Res. 2021;2021. doi:10.1155/2021/5531091
14. Erhart L, Yingyuen K, Chuanak N, et al. Hematologic and clinical indices of malaria in a semi-immune population of western Thailand. Am J Trop Med Hyg. 2004;70(1):8–14. doi:10.4269/ajtmh.2004.70.8
15. Leal-Santos F, Silva S, Crepaldi N, et al. Altered platelet indices as potential markers of severe and complicated malaria caused by Plasmodium vivax: a cross-sectional descriptive study. Malar J. 2013;12(1):1–6. doi:10.1186/1475-2875-12-462
16. D’souza J, Jayaprakash C, D’souza P, Abraham S, Suresh S, Shrinath M. Comparative hematological changes in malarial infection by P. vivax and P. falciparum: observations from the endemic region of Mangalore, India. Int J Appl Res. 2017;3(6):179–183.
17. Luzzatto L. Genetics of red cells and susceptibility to malaria; 1979.
18. Tangpukdee N, Krudsood S, Kano S, Wilairatana P. Falciparum malaria parasitemia index for predicting severe malaria. Int J Lab Hematol. 2012;34(3):320–327. doi:10.1111/j.1751-553X.2011.01398.x
19. Kotepui M, Piwkham D, PhunPhuech B, Phiwklam N, Chupeerach C, Duangmano S. Effects of malaria parasite density on blood cell parameters. PLoS One. 2015;10(3):e0121057. doi:10.1371/journal.pone.0121057
20. VanVoorhis CW, Morgan BL. Understanding power and rules of thumb for determining sample sizes. Tutor Quant Methods Psychol. 2007;3(2):43–50. doi:10.20982/tqmp.03.2.p043
21. Awulachew E, Diriba K, Anberbir S. Hematological and Immunological parameters in apparently healthy people in Ethiopia: systematic review and meta-analysis; 2020.
22. Roberts I, Stanworth S, Murray N. Thrombocytopenia in the neonate. Blood Rev. 2008;22(4):173–186. doi:10.1016/j.blre.2008.03.004
23. Al-Salahy M, Shnawa B, Abed G, Mandour A, Al-Ezzi A. Parasitaemia and its relation to hematological parameters and liver function among patients malaria in Abs, Hajjah, Northwest Yemen. Interdiscip Perspect Infect Dis. 2016;2016:1–5. doi:10.1155/2016/5954394
24. World Health Organization. Guidelines on Drawing Blood: Best Practices in Phlebotomy. World Health Organization; 2010.
25. Cserti M, Dzik H. The ABO blood group system and Plasmodium falciparum malaria. Blood. 2007;110(7):2250–2258.
26. Dos-Santos JCK, Silva-Filho JL, Judice CC, et al. Platelet disturbances correlate with endothelial cell activation in uncomplicated Plasmodium vivax malaria. PLoS Negl Trop Dis. 2020;14(7):e0007656. doi:10.1371/journal.pntd.0007656
27. Martínez-Salazar EL, Tobón-Castaño A. Platelet profile is associated with clinical complications in patients with vivax and falciparum malaria in Colombia. Rev Soc Bras Med Trop. 2014;47:341–349. doi:10.1590/0037-8682-0078-2014
28. Adias TC, Bariweni M, Dick PD, et al. Effects of plasmodium falciparum on haematological parameters on patients treated with artesunate in the Niger delta of Nigeria. Int J Med Sci Public Health. 2013;1(12):12.
29. Awoke N, Arota A. Profiles of hematological parameters in Plasmodium falciparum and Plasmodium vivax malaria patients attending Tercha General Hospital, Dawuro Zone, South Ethiopia. Infect Drug Resist. 2019;12:521. doi:10.2147/IDR.S184489
30. Kho S, Barber BE, Johar E, et al. Platelets kill circulating parasites of all major Plasmodium species in human malaria. Blood. 2018;132(12):1332–1344.
31. Peprah S, Ogwang MD, Kerchan P, et al. Mean platelet counts are relatively decreased with malaria but relatively increased with endemic Burkitt Lymphoma in Uganda, Tanzania, and Kenya. Br J Haematol. 2020;190(5):772–782. doi:10.1111/bjh.16700
32. Aninagyei E, Adu P, Rufai T, et al. Effect of asymptomatic Plasmodium falciparum parasitaemia on platelets thrombogenicity in blood donors. Indian J Hematol Blood Transfus. 2021;37(4):632–639. doi:10.1007/s12288-020-01390-w
33. Ali EA, Abdalla TM, Adam I. Platelet distribution width, mean platelet volume and haematological parameters in patients with uncomplicated Plasmodium falciparum and P. vivax malaria. F1000Research. 2017;6:865.
34. Muwonge H, Kikomeko S, Sembajjwe LF, Seguya A, Namugwanya C. How reliable are hematological parameters in predicting uncomplicated Plasmodium falciparum malaria in an endemic region? Int Sch Res Notices. 2013:2013:9.
35. Becchi C, Al Malyan M, Fabbri L, Marsili M, Boddi V, Boncinelli S. Mean platelet volume trend in sepsis: is it a useful parameter? Minerva Anestesiol. 2006;72(9):749–756.
36. Yusuf AA, Abdullahi SA, Idris IM, Jobbi YDA. Platelet count and indices in acute uncomplicated Malaria in Kano, Nigeria. Niger J Clin Sci. 2019;16(1):46. doi:10.4103/njbcs.njbcs_21_18
37. Prasad R, Das B, Pengoria R, Mishra OP, Shukla J, Singh TB. Coagulation status and platelet functions in children with severe falciparum malaria and their correlation of outcome. J Trop Pediatr. 2009;55(6):374–378. doi:10.1093/tropej/fmp028
38. Elsayid M, Elbasheer M, Othman AA, Belal RH, Elfaki T. Estimation of complete blood count and platelets indices in Sudanese patients with malaria. Am J Res Commun. 2017;5(1):29–38.
39. Chandra S, Chandra H. Role of haematological parameters as an indicator of acute malarial infection in Uttarakhand state of India. Mediterr J Hematol Infect Dis. 2013;5(1):e2013009. doi:10.4084/mjhid.2013.009
40. Hamid T, Eldin FA, Elnasri HA. Effect of Malaria Parasite Infection on Platelet Parameters (Platelets count, mean platelets volume and platelets distribution width) among Malaria Patients in Khartoum State. Ann Biol Res. 2016;7(5):18–23.
41. Desai K, Patel K, Shah M, et al. A study of platelet volume indices (PVI) in patients of coronary artery disease and acute myocardial infarction in tertiary care hospital. Int J Adv Res. 2013;1:185–191.
42. Othoro C, Lal AA, Nahlen B, Koech D, Orago AS, Udhayakumar V. A low interleukin-10 tumor necrosis factor-α ratio is associated with malaria anemia in children residing in a holoendemic malaria region in western Kenya. J Infect Dis. 1999;179(1):279–282. doi:10.1086/314548
43. Kumar N. Correlation of type of species and parasite density in malaria with platelet count, mean platelet volume and platelet distribution width. J Evol Med Dent Sci. 2016;5(89):6622–6625. doi:10.14260/Jemds/2016/1498
44. Mohamedahmed KA, Ahmed ZA, Nour BYM, Abakar AD, Babker AM. Impact of sever Plasmodium falciparum infection on platelets parameters among Sudanese children living in Al-Jazira state. Int J Clin Biomed Res. 2020;5–9. doi:10.31878/ijcbr.2020.62.02
45. Pain A, Ferguson DJ, Kai O, et al. Platelet-mediated clumping of Plasmodium falciparum-infected erythrocytes is a common adhesive phenotype and is associated with severe malaria. Proc Natl Acad Sci USA. 2001;98(4):1805–1810. doi:10.1073/pnas.98.4.1805
46. Korniluk A, Koper-Lenkiewicz OM, Kamińska J, Kemona H, Dymicka-Piekarska V. Mean Platelet Volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions. Mediators Inflamm. 2019;2019:9213074. doi:10.1155/2019/9213074
47. Coelho HCC, Lopes SC, Pimentel JPD, et al. Thrombocytopenia in Plasmodium vivax malaria is related to platelets phagocytosis. PLoS One. 2013;8(5):e63410. doi:10.1371/journal.pone.0063410
48. Gupta P, Guddattu V, Saravu K. Characterization of platelet count and platelet indices and their potential role to predict severity in malaria. Pathog Glob Health. 2019;113(2):86–93. doi:10.1080/20477724.2019.1600855
49. Vagdatli E, Gounari E, Lazaridou E, Katsibourlia E, Tsikopoulou F, Labrianou I. Platelet distribution width: a simple, practical and specific marker of activation of coagulation. Hippokratia. 2010;14(1):28.
50. Helvacioglu C, Baghaki S, Bibata BB, Yıldırım Karaca S, Doğan K. Can platelet indices be of value in pregnant women with malaria? J Obstet Gynaecol. 2022;42:1–5.
51. Budak YU, Polat M, Huysal K. The use of platelet indices, plateletcrit, mean platelet volume and platelet distribution width in emergency non-traumatic abdominal surgery: a systematic review. Biochemia medica. 2016;26(2):178–193. doi:10.11613/BM.2016.020
52. Chandrashekar V. Plateletcrit as a screening tool for detection of platelet quantitative disorders. J Hematol. 2013;2(1):22–26.
53. Bain BJ, Bates I, Laffan MA, Lewis SM. Dacie and Lewis Practical Haematology: Expert Consult: Online and Print. Elsevier Health Sciences; 2016.
54. Surve KM, Kulkarni AS, Rathod SG, Bindu RS. Study of haematological parameters in malaria. Int J Res Med Sci. 2017;5(6):2552–2557. doi:10.18203/2320-6012.ijrms20172446
55. Memon AR, Afsar S. Thrombocytopenia in hospitalized malaria patients. Pak J Med Sci Q. 2006;22(2):141.
56. Patel A, Jain S, Patel B, Modi B. Hematological changes in P. falciparum & P. vivax malaria. NJMR. 2013;3(02):130–133.
57. Bashawri LA, Mandil AA, Bahnassy AA, Ahmed MA. Malaria: hematological aspects. Ann Saudi Med. 2002;22(5–6):372–376. doi:10.5144/0256-4947.2002.372
58. Aundhakar S, Prajapati P, Prajapati S, et al. Study of clinical and hematological profile of Plasmodium vivax malaria in a tertiary care hospital in Western Maharashtra. Int J Sci Study. 2017;5(3):257–260.
59. Mert A, Ozaras R, Tabak F, Bilir M, Ozturk R, Aktuglu Y. Malaria in Turkey: a review of 33 cases. Eur J Epidemiol. 2003;18(6):579–582. doi:10.1023/A:1024648902848
60. Sakzabre D, Asiamah EA, Akorsu EE, et al. Haematological profile of adults with malaria parasitaemia visiting the Volta Regional Hospital, Ghana. Adv Hematol. 2020;2020:1–6. doi:10.1155/2020/9369758
61. Rajani D, Khatri D, Vaishnav D. Malaria: recent trends manifested as thrombocytopenia. Int J Med Sci Educ. 2016;3(1):7–10.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

