Back to Journals » Advances in Medical Education and Practice » Volume 7
Physicians’ attitudes toward, use of, and perceived barriers to clinical guidelines: a survey among Swiss physicians
Authors Birrenbach T, Kraehenmann S, Perrig M, Berendonk C, Huwendiek S
Received 16 June 2016
Accepted for publication 6 October 2016
Published 13 December 2016 Volume 2016:7 Pages 673—680
DOI https://doi.org/10.2147/AMEP.S115149
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Tanja Birrenbach,1 Simone Kraehenmann,1 Martin Perrig,1 Christoph Berendonk,2 Soeren Huwendiek2
1Department of General Internal Medicine, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland; 2Department of Assessment and Evaluation, Institute of Medical Education, Medical Faculty Bern, Bern, Switzerland
Background: Little is known about the attitudes toward, use of, and perceived barriers to clinical guidelines in Switzerland, a country with no national guideline agency. Moreover, there is no available data on the objective assessment of guideline knowledge in Switzerland. Therefore, we conducted a study at a large university’s Department of General Internal Medicine in Switzerland to assess physicians’ attitudes toward, use of, perceived barriers to, and knowledge of clinical guidelines.
Participants and methods: Ninety-six physicians (residents, n=78, and attendings, n=18) were invited to take part in a survey. Attitudes toward, self-reported use of, and barriers hindering adherence to the clinical guidelines were assessed using established scales and frameworks. Knowledge of the guidelines was objectively tested in a written assessment comprising of 14 multiple-choice and 3 short answer case-based questions.
Results: Fifty-five participants completed the survey (residents, n=42, and attendings, n=13; overall response rate 57%). Of these, 50 took part in the knowledge assessment (residents, n=37, and attendings, n=13; overall response rate 52%). Attitudes toward guidelines were favorable. They were considered to be a convenient source of advice (94% agreement), good educational tools (89% agreement), and likely to improve patient quality of care (91% agreement). Self-reported use of guidelines was limited, with only one-third reporting using guidelines often or very often. The main barriers to guideline adherence were identified as lack of guideline awareness and familiarity, applicability of existing guidelines to multimorbid patients, unfavorable guideline factors, and lack of time as well as inertia toward changing previous practice. In the assessment of guideline knowledge, the scores were rather modest (mean ± standard deviation: 60.5%±12.7% correct answers).
Conclusion: In general, this study found favorable physician attitudes toward clinical guidelines. However, several barriers hindering guideline implementation were identified. The importance of improving guideline implementation was supported by modest results in a guideline knowledge test.
Keywords: clinical guidelines, attitudes, barriers, knowledge, survey, physicians
Background
Clinical practice guidelines (hereinafter referred to as guidelines) are “statements that include recommendations intended to optimize patient care that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options”.1 Properly developed guidelines can change clinical practice and may lead to positive changes in patient outcomes while decreasing health care costs.2–5 A recent Cochrane review including 27 studies, noted that length of stay was the most commonly employed outcome measure with most studies reporting significant reductions by applying clinical guidelines. A reduction in in-hospital complications and a decrease in hospital costs/charges favoring clinical guidelines were also noted.3,4 However, successful guideline implementation depends on several factors. Relevant factors are physicians’ attitudes toward guidelines and possible perceived barriers. In 1994, Tunis et al conducted one of the largest studies on physicians’ attitudes toward guidelines, involving over 1,500 internists of the American College of Physicians.6 Although most of them recognized the potential benefits of clinical guidelines, many were concerned about possible effects on their autonomy, on health care costs, and on satisfaction with clinical practice. More favorable attitudes were held by those who had recently graduated.6 A systematic review of surveys on clinicians’ attitude toward clinical practice guidelines conducted in 2002, which included over 11,000 international responses, also found generally favorable opinions on guidelines (eg, good source of advice and educational tools, intended to improve patient quality of care).7 However, clinicians often considered them to be impractical, too rigid to apply to individual patients, oversimplified, and a possible threat to physician autonomy.7
Despite the generally favorable attitudes toward guidelines, evidence shows that their implementation in clinical practice is insufficient.8,9 Adoption of and physician adherence to guidelines may be hindered by a variety of barriers, as studied by Cabana et al in 1999.10 Their comprehensive review of 76 studies yielded 3 general categories of barriers, affecting physician knowledge (lack of awareness and lack of familiarity), attitudes (lack of agreement, lack of self-efficacy, lack of outcome expectancy, and inertia of previous practice), or behavioral/external barriers (patient factors, guideline factors, and environmental factors). Barriers varied according to local setting; thus, implementation strategies need to focus on specific local barriers.10
Unlike many other countries (eg, UK, Germany, and Scotland), there is no national guideline agency in Switzerland, and no formal national guideline program exists other than the general recommendation of the Swiss Medical Association for medical specialties to develop high-quality guidelines.11,12 So far, only very few Swiss guidelines exist (eg, for chronic obstructive pulmonary disease).13 Very little is known in Switzerland about physicians’ attitudes toward clinical guidelines. To date, only one study has examined attitudes toward guidelines and their impact on clinical care in Switzerland.14 This study, conducted in 2002 by Bochud et al at the Department of Medicine, University Hospital of Lausanne in the French-speaking part of Switzerland, found favorable attitudes toward guidelines overall, especially among less experienced physicians. However, familiarity with the guidelines was noted to be low, and only half of the participants reported that clinical practice guidelines had changed their medical practice during the last year.14 Furthermore, there are only a few studies objectively assessing the knowledge of guidelines.8
In summary, there is only one study on the attitudes toward, use of, and perceived barriers to clinical guidelines, and this study was conducted back in 2002. Moreover, there are no available data on the objective assessment of guideline knowledge in Switzerland, and Switzerland constitutes a special case, as it has no national guideline agency. Therefore, we conducted a study at a large university’s Department of General Internal Medicine in Switzerland to assess physicians’ attitudes toward, use of, perceived barriers to, and knowledge of clinical guidelines, in order to better understand guideline usage in Switzerland and to get ideas on how to optimize guideline development, dissemination, and implementation, and therefore ultimately patient outcomes. Furthermore, we wanted to investigate possible differences between residents and attendings regarding attitudes toward guidelines, use and knowledge, and explore, if our results on attitudes toward clinical guidelines differ from international findings.
Participants and methods
Participants and settings
Residents (n=78) and attendings (n=18) of the Department of General Internal Medicine at the University Hospital of Bern, Switzerland were asked to participate in a survey and knowledge test. Demographic and professional characteristics of the physicians were obtained. By law, working hours for hospital physicians in Switzerland are generally restricted to 50 hours per week and thus were not separately registered. Participants were informed about the goal of the survey (medical education research) orally and/or in writing. By voluntarily participating in the survey after adequate information of its aim informed consent was implied, but not formally obtained in writing. No remuneration was provided. We confirm that participation was voluntary, participants could not be identified from the material presented, and no plausible harm to participating individuals could arise from the study. Information disclosed by the participants was only discussed within the research team where confidentiality was maintained. At the time of the planning of the study and the data collection there was no relevant institutional review board for medical educational studies and the University of Bern institutional review board ruled this type of research ‘exempt from formal ethical approval’.
Measurement instruments
Survey
In May 2013, a paper-based survey comprising of 28 closed-ended questions and 1 open-ended question was conducted during a lunchtime lecture session. The survey was additionally conducted online.
Attitudes
The first part of the survey consisted of 10 closed-ended questions regarding attitudes toward guidelines. The statements used were adapted from previous publications and were assessed using a 5-point ordinal Likert scale (1= “strongly disagree” to 5= “strongly agree”).6,7,14 Answers were compared with international study results.
Use
Physicians were asked how often and who explicitly informed them about guidelines and whether they knew where to find information about guidelines. Physicians were asked to state guidelines with which they were familiar with. Frequency of guideline use was self-assessed. Since there is no validated framework on how to define regular use, we purposely decided against using an extended definition (eg, often being considered once a week) but chose to apply a 5-point Likert scale (1= “never”; 2= “seldom”; 3= “sometimes”; 4= “often”; and 5= “very often”).
Barriers
Assessment of barriers was based on a 14-item questionnaire developed by Kunz,15 using the barriers identified in the review by Cabana et al.10 The response format was a 5-point ordinal Likert scale (1= “I see no problem at all” to 5= “I see a very big problem”).
The attitudes and barriers components were evaluated according to the work of Tunis et al:6 For the questions about attitudes and barriers using the 5-point ordinal Likert scale, the 5-point-scale was reduced to a 3-point-scale for analysis (agreement = percent of respondents marking 4 or 5; neutral = percent of respondents marking 3; disagreement = percent of respondents marking 1 or 2).
Furthermore, an overall score was calculated using an adapted attitude scale according to Tunis et al.6 The scale sums up the ratings for 3 descriptions reflecting positive views on guidelines (good educational tools, convenient source of advice, and likely to improve quality of care) and the inverted ratings for each of the 3 descriptions reflecting negative views on guidelines (oversimplified or too “cookbook” medicine, a challenge to physician autonomy, too rigid to apply to individual patients) divided by 6. The values on the scale range from 1 to 5, with lower values representing negative attitudes toward guidelines and vice versa. Comparisons of the adapted attitude scale between the group of residents and attendings as well as according to sex were tested for statistical significance using 2-sided t-tests. Reliability of the adapted attitude scale was evaluated by determining the Cronbach’s alpha.
Knowledge test
Furthermore, a knowledge test was administered, comprising of 14 multiple-choice and 3 short answer case-based questions adapted from the Medical Knowledge Self-Assessment Program of the American College of Physicians. These questions were used to test knowledge of guideline-compliant therapy regarding the following 4 topics: venous thromboembolic disease, heart failure, chronic obstructive pulmonary disease, and community-acquired pneumonia. These were chosen because they resolve around important and frequent causes of “dyspnea” and well-established international guidelines commonly applied at the Bern University Hospital are available on these topics (guidelines for venous thromboembolic disease edited by the American College of Chest Physicians, guidelines for heart failure edited by the European Society of Cardiology, guidelines for chronic obstructive pulmonary disease edited by the Global Initiative for Obstructive Lung Disease, and guidelines for community-acquired pneumonia edited by the European Respiratory Society, the European Society for Clinical Microbiology and Infectious Diseases as well as British Thoracic Society).16–20
The participants were randomly assigned to two sets of tests consisting of similar yet different questions (eg, 2 different scenarios for outpatient treatment of community-acquired pneumonia). Since the questions were chosen from the Medical Knowledge Self-Assessment Program of the American College of Physicians, the answering key was given, and again checked for local appropriateness by authors TB and MP, who are internal medicine specialists. Randomization was carried out by listing the participants alphabetically and allocating even and odd numbers to the two subsets of questions (each subset consisting of 48 participants: residents, n=39, and attendings, n=9).
Analysis
Data were entered and analyzed using Excel 2013 and SPSS Version 21 (IBM Corporation, Armonk, NY, USA). Quantitative outcomes were described using mean values and their corresponding standard deviations (SD). For the knowledge test, comparisons between the group of residents and attendings as well as the 2 sets of tests were tested for statistical significance using 2-sided t-tests. The customary 5% level of significance (α =0.05) was used. Reliability of the adapted attitude scale and knowledge tests was evaluated by determining the Cronbach’s alpha.
Results
Participants
Fifty-five physicians completed the survey (residents, n=42, and attendings, n=13; response rate 57%); 5 of these residents did not complete the knowledge test (response rate knowledge test 52%). Of the physicians who completed the survey, 60% were female and 81% of the residents had >2 years professional experience in general internal medicine.
The nonresponders to the knowledge test consisted of 41 residents and 5 attendings (50% female).
Attitudes
Generally, attitudes toward guidelines were favorable (Table 1). They were considered to be a convenient source of advice (94% agreement), good educational tools (89% agreement), and likely to improve patient quality of care (91% agreement). Only 13% perceived guidelines in general as an oversimplified tool and 4% viewed them as a challenge to physician’s autonomy. Guidelines were not generally considered to be too rigid to apply to individual patients (7% agreement).
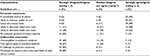  | Table 1 Physicians’ attitude toward guidelines |
The generally positive attitude was reflected in the adapted attitude scale (mean: 4.10 SD: 0.44). The results of this scale did not differ significantly between residents and attendings (p=0.169), or according to sex (p=0.171). The internal consistency coefficient (Cronbach’s alpha) for this scale was 0.6.
A comparison of international studies with our results on attitudes toward clinical guidelines is presented in Table 2.
Use
The majority of the physicians used clinical guidelines sometimes (56%) or often (26%). Only 6% reported never using guidelines (Table 3). Familiar guidelines included a variety of national guideline agency recommendations and mainly international specialist society recommendations (eg, cardiovascular topics originating from the European Society of Cardiology, the American Heart Association, the National Institute of Health and Clinical Excellence, pneumology recommendations originating from the Global Initiative for Chronic Obstructive Lung Disease and for Asthma, infectious diseases recommendations from the Swiss Society of Infectious Diseases as well as the Infectious Diseases Society of America and the Bundesamt für Gesundheit (Federal Office of Public Health). The physicians were only seldom (38%) or sometimes (43%) explicitly informed about clinical guidelines, usually by senior staff, self-study, the internet, other residents, or conferences. However, 30% of the physicians did not know where to find information about clinical guidelines.
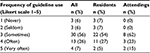  | Table 3 Self-reported frequency of guideline use on a Likert scale from 1 to 5 |
Barriers
Several barriers to guideline adherence were explored and identified (Table 4): Lack of awareness and lack of familiarity emerged as the main barriers (70% and 57% agreement, respectively). Patient factors (eg, inability to reconcile patient preferences with guideline recommendations and applicability to practice population, both 30% agreement) and lack of time (33% agreement) also proved to be obstacles. Furthermore, guideline attributes, such as their low usability (36% agreement), guideline accessibility (43% agreement), and the presence of contradictory guidelines (30% agreement) were seen as problematic. Additionally, the inertia toward changing previous practice hindered guideline implementation (32% agreement). Only 10% of all physicians cited disagreement with guideline content as a barrier to their adherence. There was general confidence in the guideline developers (only 11% considered this to be a problem). Guidelines were not generally considered to be too rigid to apply to individual patients (only 7% agreement), yet there was concern about the applicability to practice population (30% agreement). Neither lack of outcome expectancy nor lack of self-efficacy was considered to be a large problem (10% and 19% agreement, respectively).
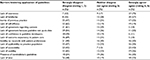  | Table 4 Barriers to guideline application |
Knowledge test
Fifty physicians (residents, n=37, and attendings, n=13) completed the knowledge test (17 multiple-choice and short answer questions (response rate 52%). The mean score was 60.5% correct answers (SD: 12.7%) and did not differ significantly between the sets of tests (61.9% [SD: 15.1% vs 59.6% [SD: 11.2%], p=0.522) (Table 5). Residents’ scores were significantly lower than those of attendings (mean 58.6% [SD: 12.9%] vs mean 66.0% [SD 11.0%]; p=0.035).
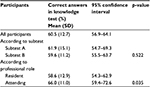  | Table 5 Results of the knowledge test Abbreviation: SD, standard deviation. |
The internal consistency coefficient (Cronbach’s alpha) was 0.53 and 0.12 for subtests A and B, respectively.
Discussion
We sought to assess physicians’ attitudes toward, use of, perceived barriers to adherence to, and knowledge of clinical guidelines at a large university’s Department of General Internal Medicine in Switzerland. We found favorable physician attitudes toward clinical guidelines and support for the use of guidelines to improve clinical care. Self-reported use of guidelines was limited. Several barriers hindering guideline implementation were identified. The knowledge test showed only modest knowledge of guidelines.
In our survey, we found a favorable attitude toward guidelines. Three unambiguously positive statements (guidelines are considered to be a convenient source of advice, good educational tools, and are likely to improve quality of care) elicited around 90% agreement. This is only the second report on Swiss internists’ attitudes toward guidelines. Bochud et al found similarly positive attitudes in the French-speaking part of Switzerland, especially among junior and less experienced physicians.14 In our study, we found no significant difference between the attitudes of residents and attendings or according to sex. International findings and reviews also support these favorable attitudes.6,7,21,22 Compared to both international and Swiss studies and reviews, we found even more favorable attitudes (Table 2).6,7,9,14,15,23 Particularly striking in this regard was the disagreement with statements about guidelines being oversimplified, too rigid to apply to individual patients, and a challenge to physician autonomy: these beliefs were shared by less than 15% of the participants. This result may be due to fewer medico-legal and regulatory concerns regarding guidelines threatening physician autonomy in Switzerland than in other countries (eg, US).
Only one-third of the participants in our study reported using guidelines often or very often, which is comparable to findings among German and international physicians.15,21,22 Kunz reported that only 40% of German family physicians had used clinical guidelines during the last 6 months.15 In a large sample of Canadian physicians, 52% reported using guidelines at least monthly.21
The results of the objective knowledge test further support this self-reported statement regarding limited use. Participants’ scores were modest, with only 60% correct answers, confirming the rather low knowledge of clinical guidelines when applying them to case-based questions. Thus, despite favorable attitudes, guideline use and knowledge were limited. To our knowledge, only a small number of studies on guideline implementation have incorporated an objective knowledge test, and these used few questions.8
We identified a low level of awareness of and familiarity with existing guideline recommendations as the main barriers hindering use and implementation of clinical guidelines. Additionally, applicability of existing guidelines to a multimorbid patient population, guideline factors (eg, lack of user-friendliness, poor accessibility, and presence of contradictory guidelines), and lack of time were found to be important barriers. These correspond well to commonly encountered barriers by physicians, including residents in other settings.10,15,23–26 Awareness of and familiarity with existing guideline recommendations emerged as the most common barriers in our study (70% and 57% agreement, respectively), comparable to the results of the review by Cabana et al.10 Applicability of guideline recommendations to a multimorbid practice population was stated as an important barrier in our study, and is now also being recognized internationally as a major problem; several studies have demonstrated that age and multimorbidity are not fully addressed in some national guidelines.27,28 There is a general wish for guidelines for people rather than for diseases.28–30 However, the evidence for comorbidity-related recommendations is limited, since this population is generally not included in controlled-randomized trials. Finding out more about pattern of diseases, including these populations in clinical trials and then specifically addressing these common comorbidities and their therapeutic co-implications in the guidelines is required. However, there still remain uncertainties as to how these interactions should be interpreted, weighed, and finally, illustrated.
There are several strengths of our study. This is only the second report on Swiss internal medicine specialists who were questioned about their attitudes toward and perceived barriers to guidelines. The evaluation of attitudes and barriers was carried out according to established frameworks and a previously developed questionnaire.6,10 Besides self-reported measures, knowledge of guidelines was objectively assessed in a case-based multiple-choice test. This has not been previously reported for Switzerland and, to our knowledge, has also not been addressed in larger international studies. The combination of the documentation of attitudes, self-reported use, barriers, as well as an objective measure of knowledge allowed for an important insight into guideline usage and implementation in a large internal medicine department in Switzerland.
Limitations
Nevertheless, some limitations of our study should be noted. The sample size of the study is limited and the study took place in a single university hospital setting, albeit the largest of its kind in Switzerland. Therefore, the generalizability to other settings and countries is questionable. With a response rate of 57%, there is a possibility of selection bias. Participants may possibly be more motivated and might express more positive attitudes compared to nonparticipants. As information is based on self-report (apart from the knowledge test), a bias due to social desirability cannot be excluded. Additionally, a bias toward over-reporting adherence to guidelines has been noted elsewhere.24 Furthermore, there is a certain overlap between the concepts of attitude and barriers, since attitude (eg, lack of agreement, lack of self-efficacy, lack of outcome expectancy, and inertia of previous practice) is one of the 3 general categories of barriers, as reported by Cabana et al.10 Although the evaluation of attitudes and barriers was carried out in accordance with other studies, a formal validation of these measures has not been done.6,7,10,15,21–23,26 Furthermore, reliability of one knowledge subtest was limited.
Conclusion
This study found that internal medicine residents and specialists had positive attitudes toward guidelines. However, only one-third used them often or very often. The knowledge test supported the limited application of guideline recommendations when solving case-based questions. Several barriers hindering guideline implementation were identified in our setting, the most important of which was awareness of and familiarity with guidelines. Applicability of existing guidelines to our multimorbid patient population, guideline factors (eg, lack of user-friendliness, poor accessibility, and presence of contradictory guidelines) as well as lack of time proved to be further obstacles that need to be considered in the endeavor to improve adherence. These findings can help to provide a better understanding of guideline usage in Switzerland (and possibly other countries with no formal guideline agency) and to optimize guideline development, dissemination, and implementation, and therefore ultimately patient outcomes.
Disclosure
The authors report no conflicts of interest in this work.
References
Graham R, Mancher M, Wolman DM, Greenfield S, Steinberg E, editors. Clinical practice guidelines we can trust. Washington, DC: The National Academies Press; 2011. | ||
Grimshaw J, Freemantle N, Wallance S, et al. Developing and implementing clinical practice guidelines. Qual Health Care. 1995;4(1):55–64. | ||
Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):CD006632. | ||
Rotter T, Kinsman L, James E, Machotta A, Willis J, Snow P, Kugler J. The effects of clinical pathways on professional practice, patient outcomes, length of stay, and hospital costs: Cochrane systematic review and meta-analysis. Eval Health Prof. 2012;35(1):3–27. | ||
Lugtenberg M, Burgers JS, Westert GP. Effect of evidence-based clinical practice guidelines on quality of care: a systematic review. Qual Saf Health Care. 2009;18(5):385–392. | ||
Tunis SR, Hayward RS, Wilson MC, Rubin HR, Bass EB, Johnston M, Steinberg EP. Internists’ attitudes about clinical practice guidelines. Ann Intern Med. 1994;120(11):956–963. | ||
Farquhar CM, Kofa EW, Slutzsky JR. Clinicians’ attitudes to clinical practice guidelines: a systematic review. Med J Aust. 2002;177(9):502–506. | ||
Echlin PS, Upshur RE, Markova TP. Lack of chart reminder effectiveness on family medicine resident JNC-VI and NCEP III guideline knowledge and attitudes. BMC Fam Pract. 2004;5:14. | ||
Heidrich J, Behrens T, Raspe F, Keil U. Knowledge and perception of guidelines and secondary prevention of coronary heart disease among general practitioners and internists. Results from a physician survey in Germany. Eur J Cardiovasc Prev Rehabil. 2005;12(6):521–529. | ||
Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PC, Rubin HR. Why don’t physicians follow clinical practice guidelines? JAMA. 1999;282(15):1458–1465. | ||
Eicher E. Guideline fuer Guidelines [Guideline for Guidelines]. Schweiz Aerztezeitung. 1999;80(10):581–584. German. | ||
Hostettler S, Kraft E, Bosshard C. Guidelines – Qualitaetsmerkmale erkennen [Recognize the quality features]. Schweizerische Aerztezeitung. 2014;95(3):45–51. German. | ||
Russi EW, Karrer W, Brutsche M, Eich C, Fitting JW, Frey M, et al. Diagnosis and management of chronic obstructive pulmonary disease: the Swiss guidelines. Respiration. 2013;85(2):160–174. | ||
Bochud M, Cornuz J, Vader JP, Kamm W, Burnand B. Are internists in a non-prescriptive setting favourable to guidelines? Swiss Med Wkly. 2002;132(15–16):201–206. | ||
Kunz A. Leitlinien in der Medizin: Anwendung, Einstellungen und Barrieren – Eine Befragung Berliner Hausaerzte [Clinical practice guidelines: application, attitudes and barriers – a survey of general practitioners in Berlin]. Master thesis MPH. Freie Universitaet, Berlin. 2005. [cited 2015 March 22]. Available from: http://www.ewi-psy.fu-berlin.de/einrichtungen/arbeitsbereiche/ppg/media/projekte/hausaerzte/kunz_2005.pdf?1286350984. German. Accessed March 22, 2015. | ||
Kearon C1, Akl EA, Comerota AJ et al. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S–94S. | ||
McMurray JJ1, Adamopoulos S, Anker SD et al; ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33(14):1787–1847. | ||
COPD Reports. Available from: http://goldcopd.org/gold-reports/. Accessed March 15, 2015. | ||
Levy ML1, Le Jeune I, Woodhead MA, Macfarlaned JT, Lim WS. Primary care summary of the British Thoracic Society Guidelines for the management of community acquired pneumonia in adults: 2009 update. Endorsed by the Royal College of General Practitioners and the Primary Care Respiratory Society UK. Prim Care Respir J. 2010;19(1):21–27. | ||
Woodhead M1, Blasi F, Ewig Set al; Joint Taskforce of the European Respiratory Society and European Society for Clinical Microbiology and Infectious Diseases. Clin Microbiol Infect. 2011;17 Suppl 6:E1–E59. | ||
Hayward RS, Guyatt GH, Moore KA, McKibbon KA, Carter AO. Canadian physicians’ attitudes about and preferences regarding clinical practice guidelines. CMAJ. 1997;156(12):1715–1723. | ||
Graham ID, Evans WK, Logan D, et al. Canadian Oncologists and clinical practice guidelines: a national survey of attitudes and reported use. Provincial Lung Disease Site Group of Cancer Care Ontario. Oncology. 2000;59(4):283–290. | ||
Larisch A, Oertel WH, Eggert K. Attitudes and barriers to clinical practice guidelines in general and to the guideline on Parkinson’s disease. A national survey of German neurologists in private practice. J Neurol. 2009:256(10):1681–1688. | ||
Carlsen B, Glenton C, Pope C. Thou shalt versus thou shalt not: a meta-synthesis of GPs’ attitudes to clinical practice guidelines. Br J Gen Pract. 2007;57(545):971–978. | ||
Van Dijk N, Hooft L, Wieringa-de Waard M. What are the barriers to residents’ practicing evidence-based medicine? A systematic review. Acad Med. 2010;85(7):1163–1170. | ||
Helwig A, Bower D, Wolff M, Guse C. Residents find clinical practice guidelines valuable as educational and clinical tools. Fam Med. 1998;30(6):431–435. | ||
Boyd CM Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716–724. | ||
Hughes LD, McMurdo ME, Guthrie B. Guidelines for people not for diseases: the challenges of applying UK clinical guidelines to people with multimorbidity. Age Aging. 2013;42(1):62–69. | ||
Mercuri M, Sherbino J, Sedran RJ, Frank JR, Gafni A, Norman G. When guidelines don’t guide: the effect of patient context on management decisions based on clinical practice guidelines. Acad Med. 2015;90(2):191–196. | ||
Lugtenberg M, Burgers JS, Clancy C, Westert GP, Schneider EC. Current guidelines have limited applicability to patients with comorbid conditions: A systematic analysis of evidence-based guidelines. PloS One. 2011;6(10):e25987. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

