Back to Journals » Clinical Audit » Volume 9
Physical exam in mental health: implementation of a form to guide medical assessment of acute psychiatric inpatients
Authors Munshi T, Asmer MS, Penfold S, Pikard J, Mauer-Vakil D , Banwell E
Received 4 December 2016
Accepted for publication 16 February 2017
Published 24 May 2017 Volume 2017:9 Pages 1—7
DOI https://doi.org/10.2147/CA.S129425
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marietta Stanton
Tariq Munshi,1,2 M Selim Asmer,1,2 Sarah Penfold,1,2 Jennifer Pikard,1,2 Dane Mauer-Vakil,1 Emma Banwell1
1School of Medicine, Queen’s University, 2Department of Psychiatry, Queen’s University, Kingston, ON, Canada
Abstract: The physical health of individuals suffering from mental illness is known to be diminished compared to the general population, with worse health outcomes and shortened life expectancy. This places a great burden on health care systems around the world. Due to stigma and clinician attitudes, it may be difficult for physicians to engage with mentally ill patients to screen for physical disease and implement physical health interventions. Engaging with these patients during acute inpatient admission is an ideal time to identify any specific problems that may be the focus of medical attention. The Canadian Government mandates that all patients admitted to hospital receive routine physical assessment as part of their care. Our study aimed to implement a form to guide physical screening for all psychiatric patients admitted to an acute inpatient Psychiatric Unit in Kingston, ON, Canada; the patients underwent two cycles of clinical audit between 2014 and 2015 to measure completion of forms. Although the completion rate decreased, the frequency of consultation with the hospitalist increased significantly between the two cycles. There was no relationship found between patient age, psychiatric diagnosis, and day of admission during the week did not affect completion of physical health screening. Further education and advocacy is needed to ensure appropriate screening of physical problems in patients admitted for psychiatric reasons. Future studies are needed to study the effectiveness of these forms and whether or not they are effective in improving health outcomes in the long term.
Keywords: physical examination, audit, health form
Introduction
The physical health of individuals with mental illness is an area of growing concern worldwide.1 As early as several decades ago, the British Medical Journal reported a strong association between poor physical health and mental illness.2 Age-adjusted death rates were found to be two to four times higher than those of the general population, along with 13–30 years of shortened life expectancy. Obesity, cardiovascular diseases, viral diseases, and respiratory tract diseases were found to be of higher prevalence in psychiatric patients compared to those who did not suffer from mental illness.2
Pharmacological interventions for schizophrenia, bipolar disorder, schizoaffective disorder, and major depressive disorder3,4 may contribute toward decreasing the physical health of these patients due to metabolic, endocrine, gastrointestinal, and cardiac side effects of many medications. Previous studies have established a clear relationship between metabolic syndrome and related health complications in psychiatric patients using atypical antipsychotics, requiring regular monitoring for primary and secondary prevention.4–6 Furthermore, the use of selective serotonin reuptake inhibitors has been associated with an increased risk of osteoporosis and fractures.2 In addition to the physical burden of illness, the increased use of medical services also places a great burden on the health care system.
Environmental factors such as poor housing, financial constraints, and unemployment may also contribute to physical morbidity in individuals with psychiatric illness. Having a severe mental illness may influence patient’s adherence and/or seeking out of medical services, which may also contribute toward this declined physical health status. In this regard, a complete and comprehensive physical examination of a patient with psychiatric illness is imperative.7 This would give a more complete picture of a patient’s complete overall general health and have multiple benefits on patient outcomes including discovering and documenting medical comorbidities, which may impact psychiatric treatment plan and outcome, due to adverse effects of many psychotropic medications.7 However, resource constraints, such as short consultations in an acute hospital setting, and clinical challenges, such as severe agitation, may pose barriers for physicians to comprehensively assess both the mental and physical health status of patients. Physicians who do not feel comfortable engaging with patients with serious mental illness may also pose a barrier in ensuring that appropriate medical care is delivered.7 The goal of our study was to explore how frequently patients admitted to an acute psychiatric inpatient ward are assessed with regard to screening for medical issues.
The Department of Health (United Kingdom) defines clinical audit as “the systematic, critical analysis of the quality of medical care, including the procedures used for diagnosis and treatment, the use of resources, and the resulting outcome and quality of life for the patient”.8 An audit can provide a review of current practices and compare this to legal or predefined standards; more specifically at our hospital, a medical history and physical exam must be completed within 72 hours of admission. With clinical auditing, organizations are better able to identify specific areas where practice and knowledge can be improved, in an attempt to provide better services.9
The Ontario Hospitals Act requires that all patients admitted to inpatient hospital services must receive a medical history review and undergo a physical examination.10 The current study is a quality improvement initiative to assess the completion of physical examination in patients admitted to an acute mental health ward. Furthermore, we aimed to assess whether patients’ demographics, diagnosis, and length of stay would have an effect on the likelihood of physical assessment completion. We hypothesized that patients who were admitted for shorter periods of time and those who had a diagnosis of schizophrenia and were more likely to be agitated would be less likely to have a physical assessment completed.
Methods
We conducted an audit of physical health assessment and physical examination practices in a 40-bed mental health inpatient unit at Kingston General Hospital, a university-affiliated, tertiary care hospital in Southeastern Ontario, Canada. This study underwent review for ethical compliance by the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (PSIY-471-15), which was approved. The patient consent requirement was waived as it was a retrospective chart review and there was no identifiable information collected for patients.
Physical health assessment and physical examination form
Prior to the initial audit cycle, a standardized template was designed and implemented to assist residents and medical students in the completion, and documentation, of general health assessments and physical examinations of patients admitted to the mental health unit. The form was created with input from psychiatry residents, inpatient psychiatrists, and a hospitalist who provides medical consultation and care in the unit, and approved by a hospital committee, which oversees the design of medical documentation forms. The following headings/sections were included in the form: history of presenting illness/problems; past medical history; medications and allergies; family history; reproductive history; substance use; physical examination findings; laboratory investigation findings; and imaging/other investigation findings. The form also included a section for physician’s overall assessment and treatment plan, as well as a section where an individual completing the assessment can request a consultation from the hospitalist for a suspected or identified general medical issue (Figure 1). Psychiatry residents and attending physicians working on the inpatient unit were instructed to complete a screening history for physical health problems and a focused physical examination of all patients admitted to their team within 72 hours of admission. If patients were deemed to be too agitated or unable to be examined, physicians were asked to defer the examination and document the reason for deferral. For each audit cycle, charts were sampled over a 3-month period to allow for a short audit and re-audit cycle and to allow relatively rapid implementation of an intervention if needed.
  | Figure 1 General medical assessment form. |
Initial audit cycle
Following implementation of the physical health assessment and examination tool, an initial audit was conducted by way of a retrospective chart review, sampling all admissions (lasting 72 hours or more) from July 1, 2014 to September 30, 2014, inclusive. In total, 168 admitted patients’ charts were reviewed to determine whether the form, and therefore physical health assessment and examination, had been completed. Chi-square analysis was used to calculate the proportion of audited charts meeting specified criteria, where the number of charts meeting criteria was the nominator and the total number of audited charts was the denominator. Identifying patient information was removed, and the following information was collected on each admission:
Form completion status (“complete” or “incomplete”)
For completed forms, the role of the individual who had completed the form (i.e., medical student, resident, staff)
For deferred or incomplete physical assessments, the reason for non-completion
Age of patient
Psychiatric diagnosis
Day of the week that the patient was admitted
Whether or not a consultation to the hospitalist was requested.
We hypothesized that patients who were older would be more likely to present with acute physical symptoms, requiring urgent medical attention, which would trigger the completion of a screening medical assessment and consultation with the hospitalist. Similarly, we hypothesized that individuals with longer length of stay would generally be those with more severe mental illness, which would similarly correlate with a higher number of physical comorbidities and need for physical health assessment by the hospitalist.
Interventions
After completing the initial audit cycle, we implemented a number of interventions in an effort to increase the number of completed physical health assessments and examinations in the ward. A grand rounds presentation (by one of the co-authors of this present study) on the importance of physical health assessment and examination of psychiatric patients was presented to the Department of Psychiatry of Queen’s University. The forms were discussed at multiple resident meetings, and residents received reminders via email communications and in the form of posters that were posted in the inpatient ward and in resident meeting areas.
Second audit cycle
A second audit cycle was conducted, using the same protocol as the initial audit, sampling charts of patients admitted (for 3 days or more) between July 1, 2015 and September 30, 2015, inclusive. This time, 91 patient charts were reviewed to determine the following: the rate of physical health assessment and physical examination completion and whether the rate had changed following implementation of the aforementioned interventions. Chi-square analysis was used once again as described in the initial audit cycle.
Results
The percentage of patients receiving a screening physical assessment during the initial audit cycle was 54%. The rate of completion decreased during the second audit cycle to 33%. However, there were significantly more hospitalist consultations requested during the second audit cycle, with consultations increasing from 31% to 53% of patients for whom an assessment was completed. There was no significant difference in documentation of reasons for exam deferral between the two audit cycles (Table 1).
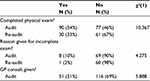  | Table 1 Physical exams audit vs re-audit Abbreviation: GP, general practitioner. |
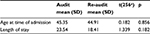
Assessments were found to be completed almost exclusively by residents, with medical students completing a small percentage of assessments. Attending physicians did not participate in completion of physical assessments, and only one assessment in the second audit cycle was completed but not signed. There were no significant differences found between the two time points in terms of team members who completed the assessment (Table 2).
  | Table 2 Staff members completing assessment |
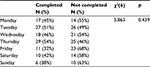
The mean age of patients who were admitted to the inpatient ward during the first and second audit cycles was 45.35 and 44.91 years, respectively. The mean length of admission during the first and second admission cycles was 23.54 and 18.41 days, respectively. The differences in both measures between the two audit cycles were not statistically significant (Table 3).
  | Table 3 Mean age and length of stay Notes: atotal number of patients. Abbreviation: SD, standard deviation. |
We also measured whether the rates of completing exams differed based on the day of the week or diagnosis. Our hypothesis was that patients admitted on Fridays would be less likely to have a physical exam completed by the weekend team. Some diagnoses, for example, dementia and delirium, were combined as these were relatively uncommon diagnoses in our sample. Patients in acute substance withdrawal did not appear in our study as this diagnosis would have been resolved by the time they would have been admitted to the unit. While the percentage of completed exams was slightly lower for patients admitted on Fridays and weekends, there was no significant difference found (Table 4). There were also no significant differences found in terms of completion rate depending on the patients’ diagnosis (Table 5).
  | Table 4 Completed exam by days of the week |
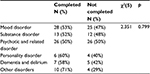  | Table 5 Completed exam by diagnosis |
Discussion
Physical comorbidities in patients with serious mental illness remain high, and several barriers pose challenges in assessing and managing these conditions in this population. Use of systematic physical evaluations has been suggested to improve morbidity and mortality.6 Our study designed and implemented a systematic physical screening tool for all patients admitted to an acute inpatient psychiatric ward in Canada. The results of our study suggest that the completion of physical health screening for psychiatric inpatients in our acute inpatient ward remains low despite continued education and advocacy. Although a standardized protocol was implemented and education was provided to the staff in the inpatient psychiatric unit, the completion of physical assessment decreased between the two audit cycles. Reasons for this may include fluctuations in number of house staff, overall workload,11 and perception that physical assessment is of lower priority in the admission process.12
Our results are generalizable to an inpatient acute psychiatric facility in a small to medium-sized center. These results point to a need for improved education for staff working with mentally ill individuals on the importance of advocacy for patients with serious mental illness. Much of the time, the patients only contact with health care providers may be through the mental health care team whose members are less capable of interpreting physical signs and symptoms. This may be due to decreased ability to correctly identify and address physical health issues due to ongoing psychiatric symptoms. Mental care workers are placed in a position of increased responsibility to screen for possible underlying medical disorders, and to advocate for appropriate referral to medical care.11 Thus, physical assessment should play a more prominent role in the admission process.
Furthermore, the reason for deferring physical examination was not documented in a majority of cases. The main reason reported by house staff in informal discussions was that the form was too lengthy and an additional documentation on top of the required admission assessment. Aggressive or agitated behavior of a patient to accept an examination was another reason for deferral of the physical examination. In a psychiatric population where patients might be psychotic, paranoid, or experience traumas, for example, the deferral of a physical examination may be appropriate. There was also uncertainty and disagreement about who should take responsibility for physical screening: the psychiatry staff or the hospitalist. A recent audit of physical health screening in psychiatric patients in the UK identified consistent barriers. The authors noted the following as some of the barriers identified during their first audit: physical health screening not being perceived as a priority, screening being unsystematic and erratic, poor recording of screening tests, and patients’ lack of interest and motivation in the screening process.12
Despite all these, the proportion of admitted patients being referred to the hospitalist for assessment of specific medical issues increased. This was thought to be due to improved engagement with the hospitalist and increased informal physical health screening during admission. In fact, between audit cycles, focus groups with staff identified that there was concern over the length and onerousness of the implemented form. One reason for the declining completion of the physical assessment form may have been an increased rate of informal screening during emergency department psychiatric assessments and appropriate referral to emergency room physicians or other specialists prior to admission, to address these issues. Unfortunately, this could not be captured in our audit process.
Examining the staff members completing the form showed that the majority of physical health assessments were completed by postgraduate residents and medical students. This could be for a variety of reasons. Firstly, attending physicians have multiple roles, are usually present in the inpatient unit for shorter periods of time, and are less involved in direct patient care. Furthermore, as many attending psychiatrists had been in practice for many years, their confidence with screening for physical health problems and conducting a physical examination may be a barrier. A previous survey revealed that many psychiatrists did not feel competent performing physical exams, did not like performing physical exams, and/or avoided performing physical exams to avoid any transference/countertransference issues.13,14 Many attending psychiatrists may have not used a stethoscope or performed a physical examination in many years, and this may affect their confidence to do so. Belief that the physical examination should be performed by a physician other than a psychiatrist may also be a contributing factors.15 Future interventions may involve further training to refresh these skills and improve comfort level.
Variables such as age at the time of admission, length of stay, and day of the week that the patient was admitted did not have a statistically significant association with physical assessment completion rate. Patient diagnosis was similarly not associated with physical assessment completion. This was significant in that our hypothesis was disproven: patients with more serious mental illnesses were not less likely to be screened.
Considerable challenges are faced in the implementation of a new practice within an establishment. With a multi-disciplinary team as found in a hospital setting and a diverse set of patients and providers, it can be challenging to invoke a new procedure that all can accept. The purpose of this intervention was to establish a physical health assessment form that can remind health care professionals of the importance of physical examination of a mental health patient while providing a template to do so. Regardless of such efforts, there are many barriers that prevent a higher rate of completion than hoped, from the time of its implementation. Future interventions are planned to improve our screening process so that patients may have physical assessments that are brief and focused so as to become a routine part of the psychiatric assessment form instead of a separate form. This may help improve physical health outcomes for patients within this vulnerable population by providing education and treating medical conditions at an opportune point in time. Education and advocacy is needed to improve completion of physical screening in our hospital. Future studies should also examine the effectiveness of this process in improving health outcomes in the long term. An evaluation of how comorbidities may affect the number and impact of physical illness in this population, and whether this has an effect on screening rates and potential for long-term improvement with adequate screening and treatment, should be explored.
Conclusion
Monitoring the physical health of patients with mental illness is an important area of advocacy for psychiatrists and other staff working in mental health care. The results of our study suggest that further education, advocacy, and quality improvement are needed to improve the screening and detection of physical health problems in patients admitted to hospital for psychiatric reasons. Although the completion rate of physical screening decreased during the second audit cycle, the proportion of patients being referred to appropriate medical care for acute issues did improve significantly. Future studies are required to explore the effectiveness of standardized screening in improving overall health outcomes in patients with psychiatric illness.
Disclosure
The authors report no conflicts of interest in this work.
References
Hall RC, Popkin MK, Devaul RA, Faillace LA, Stickney SK. Physical illness presenting as psychiatric disease. Arch Gen Psychiatry. 1978;35(11):1315–1320. | ||
Phillips RJ. Physical disorder in 164 consecutive admissions to a mental hospital. Br Med J. 1937;2(3998):363–366. | ||
Roshanaei-Moghaddam B, Katon W. Premature mortality from general medical illnesses among persons with bipolar disorder: a review. Psychiatr Serv. 2009;60(2):147–156. | ||
Rössler W, Salize HJ, van Os J, Riecher-Rössler A. Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol. 2005;15(4):399–409. | ||
DE Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52–77. | ||
Jeste DV, Gladsjo JA, Lindamer LA, Lacro JP. Medical comorbidity in schizophrenia. Schizophr Bull. 1996;22(3):413–430. | ||
Phelan M, Stradins L, Morrison S. Physical health of people with severe mental illness. BMJ. 2001;322:443. | ||
Ellis BW, Sensky T. A clinician’s guide to setting up audit. BMJ. 1991;302(6778):704–707. | ||
Tsaloglidou A. Does audit improve the quality of care? Int J Caring Sci. 2009;2(2):65. | ||
Ontario. Public Hospitals Act, R.S.O. 1990, c. P.40. Available from: https://www.ontario.ca/laws/statute/90p40. Accessed October 14, 2016. | ||
De Hert M, Cohen D, Bobes J, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011;10(2):138–151. | ||
Latoo J, Omodunbi O, Hindley D, Derbyshire A, Kane R. Physical health of people with severe mental illness: Don’t just screen… intervene! Br J Med Pract. 2015;8(3):a821. | ||
Patterson CW. Psychiatrists and physical examinations: a survey. Am J Psychiatry. 1978;135(8):967–968. | ||
Singh GP, Chavan BS, Kaur P, Bhatia S. Physical illnesses among psychiatric outpatients in a tertiary care health institution: a prospective study. Indian J Psychiatry. 2006;48(1):52–55. | ||
Garden G. Physical examination in psychiatric practice. Adv Psychiatr Treat. 2005;11(2):142–149. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
